SUMMARY
Preterm birth affects 12.5% of all births in the USA. Infants of Black mothers are disproportionately affected, with 1.5 times the risk of preterm birth and 3.4 times the risk of preterm-related mortality. The preterm birth rate has increased by 33% in the last 25 years, almost entirely due to the rise in late preterm births (34–36 weeks’ gestation). Recently attention has been given to uncovering the often subtle morbidity and mortality risks associated with moderate (32–33 weeks’ gestation) and late preterm delivery, including respiratory, infectious, and neurocognitive complications and infant mortality. This section summarizes the epidemiology of moderate and late preterm birth, case definitions, risk factors, recent trends, and the emerging body of knowledge of morbidity and mortality associated with moderate and late preterm birth.
Keywords: Epidemiology, Obstetrics standards, Pregnancy outcome, Premature birth, Prenatal care, Risk factors
1. Introduction
Preterm birth (<37 weeks gestation) affects approximately one in eight (12.5% in 2008) of all births in the USA each year.1 Preterm birth is the most frequent cause of infant mortality, as well as the leading cause of long term neurologic disabilities in children, including cerebral palsy and developmental delays. It is estimated that preterm birth costs the US healthcare system more than $26 billion each year.2 Black infants are disproportionately affected; infants of non-Hispanic Black women have >1.5 times the risk of preterm birth and 3.4 times the risk of preterm-related mortality compared with infants of White mothers.3 Reducing the high burden of preterm birth, and its associated morbidity, mortality, and racial disparities, has thus been identified as a public health priority, as reflected by the 2006 PREEMIE Act,4 the 2007 Institute of Medicine Report on preterm birth,2 the 2006 Surgeon General’s conference,5 the 2007 US Department of Health and Human Services’ public awareness campaign,6 and Healthy People 2010 and 2020 objectives.7
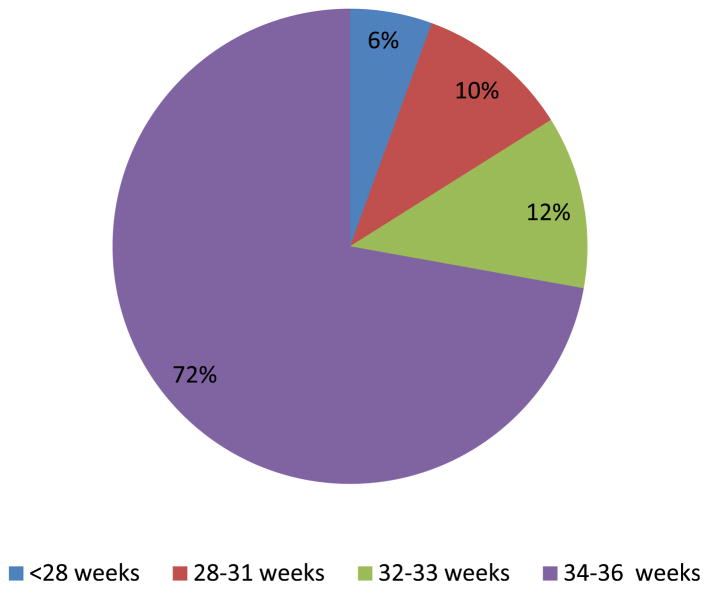
The survival of preterm infants improved greatly in recent decades, primarily due to advances in clinical management including neonatal intensive care units (NICUs), paediatric ventilators, and use of surfactant and antenatal steroids. Concomitant with improvements in preterm survival, the preterm birth rate increased by 33% from 1981 to 2006, almost exclusively due to a rise in late preterm births (34–36 weeks’ gestation).1,8 Currently, ~72% of all preterm births are due to infants born late preterm and 84% are due to late and moderate (32–33 weeks) preterm combined (Fig. 1). Although the majority of preterm-related deaths occur among very preterm infants (<32 weeks’ gestation), increased attention has recently been given to better understanding the reasons for the high rate of late and moderate preterm birth, its causes, short and long term sequelae, and opportunities for prevention. Research is uncovering significant, though often subtle, increased risks for late preterm infants compared with those born at term (i.e. 39–41 weeks’ gestation) for complications at birth and long term neurodevelopmental problems. Increased knowledge about the epidemiology of these moderate and late preterm births is critical for informing practices and guidelines related to the prevention of preterm-related morbidity and mortality.
Fig. 1.
Distribution of preterm births by gestational age: United States, 2008. Source: Centers for Disease Control and Prevention. National Center for Health Statistics. VitalStats. http://www.cdc.gov/nchs/vitalstats.htm. [August 26, 2011].
2. Preterm birth definitions and subcategories
Fetal growth and maturation occur along a continuum throughout pregnancy. As such, case definitions based on discrete categories of gestational age may appear somewhat arbitrary. However, standard categorization of preterm infants based on gestational age is valuable for assessments of morbidity and mortality risk, comparisons across populations and research studies, generating health policy guidelines, and guiding patient care.9 Generally, preterm birth is defined as birth of an infant at <37 weeks’ completed gestation. However, there has traditionally been a lack of consensus on standard gestational age categories for infants born in the period near to term, i.e. from 32 to <37 weeks’ gestation. These infants have been grouped by different gestational categories and identified by different names, such as ‘near term’, ‘late preterm’, ‘marginally preterm’, ‘moderate preterm’, and ‘borderline preterm’. Unfortunately, these terms have not adequately captured the important implications that these infants are still premature and vulnerable.9,10 Lack of recognition of prematurity, and its important physical and neurocognitive sequelae, could lead to increased comfort with early elective deliveries, less rigorous newborn assessment, early discharge, or inadequate monitoring. The 2005 National Institutes of Health workshop recommended that infants born at 34 0/7 through 36 6/7 weeks’ gestation after the onset of the mother’s last menstrual period (LMP) be referred to as ‘late preterm’.10 We will use this definition to define late preterm births in this review and define infants born at 32 0/7 to 33 6/7 weeks’ gestation as ‘moderate preterm’.
3. Estimating gestational age
Ensuring accurate and standardized estimation and reporting of gestational age may often be challenging. Gestational age is routinely estimated according to the number of weeks’ gestation after the onset of the mother’s LMP. However, this estimate may be unreliable and prone to error in maternal recall. The gold standard for accurate determination of gestational age is first trimester ultrasound.11 Nevertheless, early ultrasound is currently not recommended for routine gestational age dating and, in the USA, is often not reimbursed by public and private payers unless there is uncertainty about dates. In addition, women who seek prenatal care late may be less likely to have accurate dating. Inaccurate determination of gestational age can affect multiple downstream factors, including estimation of fetal maturity before elective delivery, clinical and epidemiologic investigations, and program evaluation.
US birth certificate records are the only source of national data for surveillance and epidemiologic studies about preterm birth. Typically, reported gestational age is based on the interval between the first day of the mother’s LMP and the date of birth.1 When information on the date of LMP is missing or when the birth weight is incongruent with the gestational age, the clinical or obstetric estimate of gestation is used in place of the LMP gestational age (~5% of all births). This reliance on LMP results in a high percentage of deliveries in which gestational age is misclassified. Basso and Wilcox12 reported that preterm births are more likely to be misclassified than term births. Qin et al.13 found that US preterm birth rates were lower when gestational age was based on the clinical estimate or on an LMP/clinical estimate composite measurement than when it was based on the LMP alone. When Qin et al.13 applied different data editing methods in an attempt to correct for misclassification, they found that the increase in preterm delivery rates from 1990 through 2002 persisted, but was attenuated.
4. Causes of late and moderate preterm birth
Preterm birth is not a single entity, but a common final outcome of a heterogeneous collection of underlying maternal and fetal factors. Approximately two-thirds of all singleton preterm births are spontaneous, often with no known cause, and approximately one-third are the result of medical intervention (i.e. medically indicated) to protect the health of the mother or infant.14 Complications of pregnancy that lead to both spontaneous and indicated preterm birth are multiple, complex, and vary according to gestational age. Although the rates of indicated deliveries remain similar throughout pregnancy, the medical reasons for intervention vary according to the changing biological processes and complications that occur at different periods of gestation. For example, placental insufficiency becomes increasingly important later in pregnancy due to the increased demands for oxygen and nutrients during a crucial period of fetal growth. The risks of some maternal complications also increase later in pregnancy, such as hypertension, pre-eclampsia, diabetes, and placenta praevia. Decisions regarding obstetric intervention must weigh the risks of continuing the pregnancy in a suboptimal uterine environment compared with the risks of early delivery. Thus, understanding the risks of moderate and late preterm birth is critical to informing optimal clinical decision-making.15,16
5. Epidemiology of preterm birth
Surveillance of preterm birth is essential for informing and evaluating clinical practices, research, programs, and policies aimed at reducing infant morbidity and mortality. Surveillance and epidemiologic analyses can measure the contribution of preterm birth to infant morbidity and mortality, identify populations at highest risk, detect changes in obstetric practices, and guide the development, implementation, and evaluation of programs.17
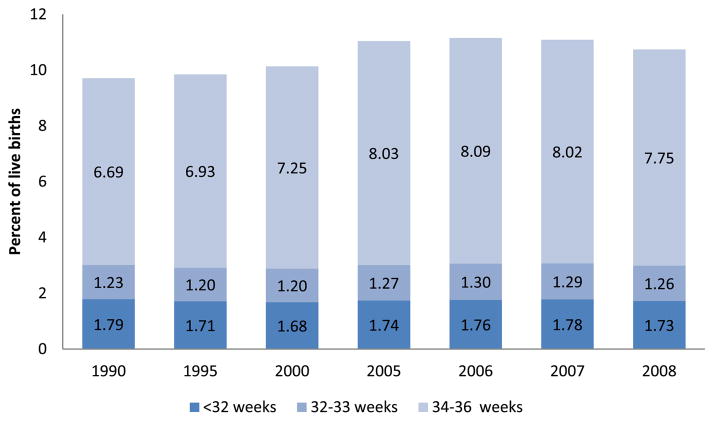
Increases in the singleton preterm birth rate since 1990 have been almost entirely due to infants born late preterm (Fig. 2). During 1990–2006, the late preterm birth rate for singleton births increased 20.9%, from 6.7% to 8.1%. This rate declined slightly in 2007 and 2008 to 8.0% and 7.8%, respectively. Preliminary data from 2009, the latest year available, suggest that this decline is continuing.18
Fig. 2.
Trends in singleton preterm birth rates: United States, final 1990, 1995, 2000, and 2005–2008. Source: Centers for Disease Control and Prevention. National Center for Health Statistics. VitalStats. http://www.cdc.gov/nchs/vitalstats.htm. [August 26, 2011].
Although the reasons for the increasing rates of moderate preterm and late preterm birth during the last two decades are not well understood, several theories have been postulated. These include improved risk assessment and timing for maternal and fetal disorders, more elective inductions and caesarean sections to reduce adverse fetal outcomes, increasing maternal age (>35 years), and increasing rates of multiple gestations.10,19,20 Growing concerns have been raised about more invasive medical management without clear indication, driving late preterm and early term rates due to providers’ concerns about medical malpractice, patient requests, or even convenience of the family or obstetrician. The actual prevalence of these practices is unknown. One recent study reviewed medical records and estimated that more than half of all late preterm infants delivered by obstetric intervention could be ‘non-evidence based iatrogenic preterm birth’.21 However, cautious interpretation of this study is warranted, as information on the indication for the delivery was often missing in the medical record.22
Concern about the practice of elective induction or caesarean delivery without medical indication prompted the March of Dimes to launch a national campaign, ‘Healthy Babies are Worth the Wait’,23 to raise awareness among patients and providers on the importance of preventing non-indicated intervention. Also, several large health insurance groups have moved to limit elective inductions and caesarean sections without medical indication before 39 weeks.24,25 Preliminary results of these programs appear promising, demonstrating rapid declines in elective inductions and caesarean section without indication prior to 39 weeks’ gestation, as well as cost savings due to NICU and hospital stays.25 More information is needed to determine the extent of changes that have occurred in clinical practice, or just changes in reporting of indications. The reduction in US preterm birth rates in 2007–2009, the reversal of a long term trend in increasing rates, may indicate that these programs are having a positive impact (Fig. 2).
5.1. Risk factors for moderate and late preterm birth
Multiple maternal and infant characteristics are associated with spontaneous preterm births, such as multiple gestations, birth defects, maternal age, and race and ethnicity. Although many of these variables are not modifiable, knowledge of these risk factors is important for targeting interventions to those at highest risk.
5.1.1. Multiple gestations
Twins and higher order multiples have elevated rates of late and moderate preterm birth compared with singletons. Between 1990 and 2008, the rate of singleton infants born late preterm increased by 14.7%, whereas among multiples the rate increased by 27.4%.26 Much of the increase in multiples is thought to be attributable to delayed childbirth and increased use of assisted reproductive technologies (ART).1 The proportion of multiples due to ART is quite high (~48%),27 but the overall contribution of ART to the national preterm birth rate is more limited; only about 1% of all US births in 2006 were attributable to ART.27 ART is also associated with increased risk of preterm birth among singleton births, but it is not known whether ART or the underlying biological reasons for infertility increase the risk of preterm birth.28
5.1.2. Congenital malformations
Congenital malformations are associated with increased preterm birth rates. A US multi-state study from 1995 to 2000 showed that infants born at 32–36 weeks’ gestation had more than a two-fold risk of having congenital malformations than their term counterparts.29 The risk was five times higher for those born at earlier gestations.
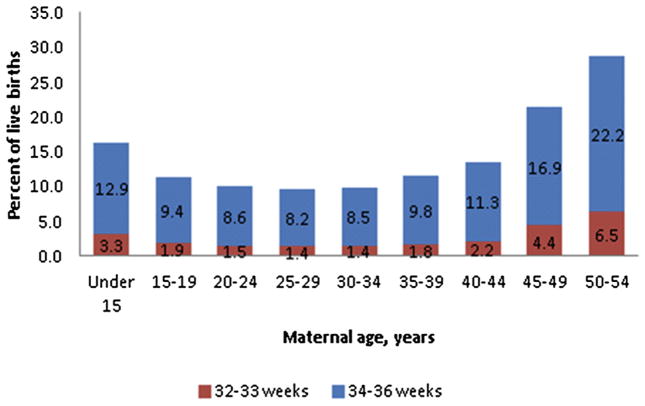
5.1.3. Maternal age
A U-shaped distribution is observed between maternal age and late preterm birth (Fig. 3). In 2008, late preterm birth rates were highest among women of <20 and >35 years of age; women of 20–34 years of age had the lowest preterm rates. A similar pattern is observed for those born moderately preterm (Fig. 3). Increased preterm risk among older women may be due to an increased prevalence of co-morbid conditions such as diabetes and hypertension, as well as higher multiple birth rates and use of ART.27 Among teens, increased preterm risk may be due to biologic immaturity, lower socioeconomic status, and behavioral risk factors such as tobacco use.30 The increase in the preterm birth rate since 1990 has been greater for older mothers and less so for teens.8
Fig. 3.
Percent of live births born moderate and late preterm by maternal age: United States, 2008. Source: Centers for Disease Control and Prevention. National Center for Health Statistics. VitalStats. http://www.cdc.gov/nchs/vitalstats.htm. [August 26, 2011].
5.1.4. Race and ethnicity
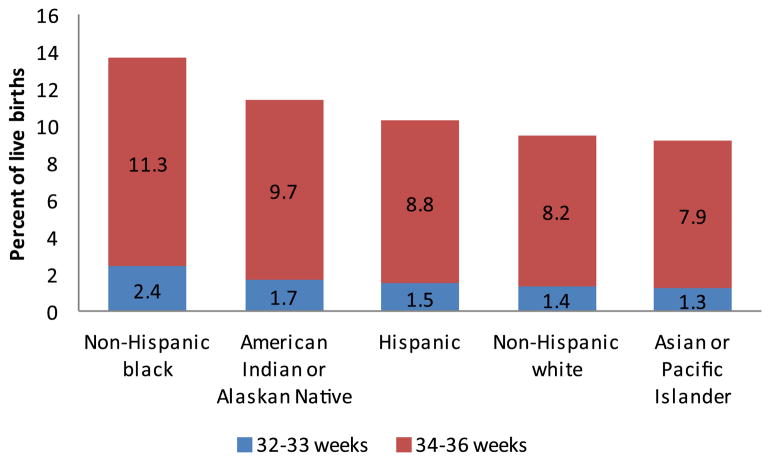
Preterm birth rates vary for different racial and ethnic groups. In 2008, late preterm birth rates were highest for infants of non-Hispanic black mothers (11.3%), followed by American Indian or Alaskan Natives (9.7%), Hispanics (8.8%), non-Hispanic whites (8.2%) and Asian or Pacific Islanders (7.9%) (Fig. 4). A similar pattern is observed for moderate preterm births. The reasons for these racial and ethnic disparities remain poorly understood. Possible explanations include differences in access to care and quality of care, social determinants of health including the effects of psychosocial stress, poverty, and the environment; prevalence of co-morbidities; and genetic factors.3 Although preterm birth risk declines with increasing level of maternal education and income, Black women with a college education still have higher preterm birth rates than White women with a college education.31 Despite social and economic disadvantages, Hispanic women tend to have a lower risk of preterm birth compared with Black women, often termed the ‘Hispanic paradox’.32 Reasons for disparities in late preterm birth and preterm-related mortality for non-Hispanic blacks, American Indian or Alaskan Natives, adolescent, and older mothers have not been fully elucidated and represent a critical area for research.
Fig. 4.
Percent of live births born moderate and late preterm by maternal race and Hispanic origin: United States, 2008. Source: Centers for Disease Control and Prevention. National Center for Health Statistics. VitalStats. http://www.cdc.gov/nchs/vitalstats.htm. [August 26, 2011].
5.2. Morbidity and mortality rates
Risk of infant morbidity and mortality declines dramatically with increasing gestational age up until term and then increases again post-term.33 Understanding which infants are at greatest risk for morbidity and mortality can assist providers in anticipating potential complications and with successful management, early intervention, and follow-up.19 During the last decade, studies have shown consistently that late preterm infants are at higher risk than term infants for a number of neonatal complications including respiratory distress requiring ventilation, transient tachypnea of the newborn, intraventricular hemorrhage, bacterial sepsis, apnoea, hypoglycemia, temperature instability, jaundice and hyperbilirubinaemia, feeding problems, neonatal intensive care admission, and even death.34–36 Although moderate and late preterm birth is associated with increased neonatal complications, it is important to note that the direction of causality remains unclear. Preterm delivery may cause adverse infant outcomes, or the medical indications leading to the need for the preterm delivery, such as intrauterine growth restriction or fetal anomalies, may be the cause of the adverse outcomes. A growing body of evidence suggests that infants born late and moderate preterm also have higher risks of later childhood morbidity and disability, including cerebral palsy, poor school performance, early intervention services, special education needs, and asthma.37–41
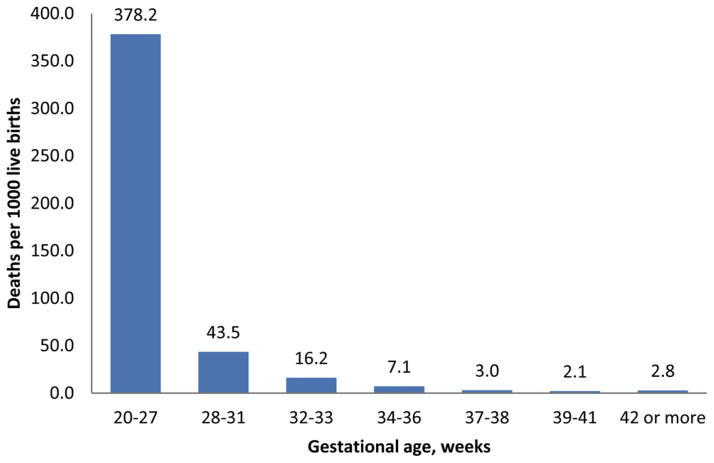
Infant mortality rates are highest among the most preterm infants (Fig. 5). During 2006–2008 infants born <28 weeks’ gestation had by far the highest infant mortality rate (378.2 per 1000 live births), whereas infants born at 39–41 weeks had the lowest mortality rates (2.1 per 1000 live births). It is important to note that mortality risk continues to decline up to 39–41 weeks’ gestation, including those born late preterm (7.1 per 1000 live births) and moderate preterm (16.2 per 1000 live). Infants born at 32–33 and 34–36 weeks’ gestation have, respectively, ~8 and 3 times the rate of infant mortality compared with their term counterparts.
Fig. 5.
Infant mortality rates (per 1000 live births) by gestational age: United States, 2006. Source: United States Department of Health and Human Services (US DHHS), Centers of Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS), Office of Analysis and Epidemiology (OAE), Division of Vital Statistics (DVS), Linked Birth/Infant Death Records 2003–2006 on CDC WONDER Online Database. Accessed at http://wonder.cdc.gov/lbd-current.html on Sep 27, 2011 03:40:20 PM.
Several studies have attempted to examine neonatal complications and mortality by underlying factors resulting in preterm birth. Using 2001 US vital statistics data, Chen et al.15 compared neonatal mortality risk by preterm birth subcategory (i.e. spontaneous preterm birth with intact fetal membranes, preterm premature rupture of membranes before labor onset, and indicated preterm birth). Compared with spontaneous preterm deliveries, late and moderate preterm infants delivered for medical indications had twice the risk of neonatal death. In another study restricted to late preterm births, Reddy et al.16 reported similar findings. Deliveries with recorded obstetric complications (e.g. polyhydramnios, oligohydramnios, incompetent cervix, cord prolapse, fetal distress) had at least twice the risk of neonatal and infant mortality compared with deliveries with no recorded indication.
Another large retrospective cohort study using vital statistics and hospital discharge records in Massachusetts found that morbidity risk during birth hospitalization among late preterm infants decreased with increasing gestational age.42 Morbidity rates were similar among infants born between 39 and 41 weeks’ gestation (ranging from 2.5% to 2.8%). However, morbidity rates approximately doubled for each additional gestational week earlier than 38 weeks, from 5.9% with morbidities if born at 37 weeks’ gestation to 51.7% morbidity at 34 weeks’ gestation. Importantly, this study also found that the risk of neonatal morbidity increased among infants born late preterm if the pregnancy was complicated by an underlying medical condition, especially for antepartum haemorrhage and hypertensive disorders of pregnancy.
Because fetal lung maturation is completed late in gestation, respiratory morbidities are a frequent concern for late and moderate preterm infants.43,44 In a comprehensive review, Colin et al. found that infants born 32–36 weeks’ gestation had a greater risk of respiratory morbidities compared with term infants.43 Rates of infant deaths due to respiratory distress syndrome have been found to increase with each week of decreasing gestational age before 37 weeks (0.06 infant deaths per 1000 live births at 36 weeks, 0.11 at 35 weeks, 0.26 at 34 weeks, 0.44 at 33 weeks, and 3.09 at 28–32 weeks).44
5.3. Late preterm birth and fetal death
Many argue that advances in obstetric practice have led to more intensive monitoring during pregnancy, which has led to increased obstetric interventions. It follows that this increase in medical interventions resulting in early delivery would lead to a decrease in stillbirths. Some evidence exists to support this argument.45–47 Joseph et al.46 examined US vital records from 1988–1999 to evaluate the temporal associations between trends in late preterm births and fetal deaths. The increase in obstetric intervention at 34–36 weeks’ gestation appeared to be temporally associated with a significant decline in late fetal death rates. Others have examined similar data and have shown that increases in preterm birth precipitated by obstetric intervention correlated with a reduction in perinatal mortality.47 Though more direct assessments are needed, these associations suggest that the rise in moderate and late preterm births, perhaps due to increased obstetric intervention, may be conferring some improvement in perinatal outcomes.14
In summary, late preterm birth accounts for the vast majority of preterm births in the USA and for the rise in the national preterm birth rate over the past two decades. Late and moderate preterm infants are both physiologically and developmentally immature and have higher risks for morbidity and mortality compared with infants born at term. Attention to increasing rates of late preterm births during the last decade have led to several campaigns aimed at reducing non-medically indicated preterm births.23,25 It will be important to document the health and economic impact of these initiatives in the years to come. Prospective studies will further strengthen our knowledge about decisions regarding obstetric intervention. We must go beyond crude measures such as race, ethnicity, and age, and explore the complex mediators of disparities to further advance identification of effective prevention strategies.
Practice points.
Among infants born preterm, 72% are born late preterm, i.e. at 34 0/7 through 36 6/7 completed weeks’ gestation.
Although mortality risk declines with increasing gestational age, even infants born close to term are at increased risk for mortality.
Compared with term births, infants born late preterm experience higher rates of infant morbidity and mortality, as well as higher risks of childhood disabilities.
Research directions.
Detailed prospectively collected data would increase knowledge about decisions regarding obstetric intervention.
Racial and ethnic disparities in late preterm birth mortality are complex and remain poorly understood.
Acknowledgments
Funding sources
None.
Footnotes
Conflict of interest statement
None declared. The findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Mathews TJ, Osterman MJ. Births: final data for 2008. Natl Vital Stat Rep. 2010;59:1–72. [PubMed] [Google Scholar]
- 2.Behrman RE, Butler AS, Institute of medicine (U.S.) Preterm birth: causes, consequences, and prevention. Washington, DC: National Academies Press; 2007. Committee on understanding premature birth and assuring healthy outcomes. [PubMed] [Google Scholar]
- 3.MacDorman MF. Race and ethnic disparities in fetal mortality, preterm birth, and infant mortality in the United States: an overview. Semin Perinatol. 2011;35:200–8. doi: 10.1053/j.semperi.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 4.Prematurity Research Expansion and Education for Mothers who deliver Infants Early Act (PREEMIE Act) 2006 [Available from: http://frwebgate.access.gpo.gov/cgi-bin/getdoc.cgi?dbname=109_cong_public_laws&docid=f:publ450.109]
- 5.Surgeon general’s conference on the prevention of preterm birth. 2008 doi: 10.1097/AOG.0b013e31819bdba3. [Available at http://www.surgeongeneral.gov/library/preterm_birth/background.html] [DOI] [PubMed]
- 6.‘A Healthy Baby Begins with You’ Campaign. [Available at http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlID=117]
- 7.Healthy People. [Available at: http://www.healthypeople.gov/2010/default.htm]
- 8.Martin JA, Osterman MJ, Sutton PD. Are preterm births on the decline in the United States? Recent data from the National vital statistics system. NCHS Data Brief. 2010:1–8. [PubMed] [Google Scholar]
- 9.Engle WA. A recommendation for the definition of “late preterm” (near-term) and the birth weight–gestational age classification system. Semin Perinatol. 2006;30:2–7. doi: 10.1053/j.semperi.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 10.Raju TN, Higgins RD, Stark AR, Leveno KJ. Optimizing care and outcome for late-preterm (near-term) infants: a summary of the workshop sponsored by the National Institute of Child Health and Human Development. Pediatrics. 2006;118:1207–14. doi: 10.1542/peds.2006-0018. [DOI] [PubMed] [Google Scholar]
- 11.Kramer MS, McLean FH, Boyd ME, Usher RH. The validity of gestational age estimation by menstrual dating in term, preterm, and postterm gestations. JAMA. 1988;260:3306–8. [PubMed] [Google Scholar]
- 12.Basso O, Wilcox A. Mortality risk among preterm babies: immaturity versus underlying pathology. Epidemiology. 2010;21:521–7. doi: 10.1097/EDE.0b013e3181debe5e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Qin C, Dietz PM, England LJ, Martin JA, Callaghan WM. Effects of different data-editing methods on trends in race-specific preterm delivery rates, United States, 1990–2002. Paediatr Perinat Epidemiol. 2007;21(Suppl 2):41–9. doi: 10.1111/j.1365-3016.2007.00860.x. [DOI] [PubMed] [Google Scholar]
- 14.Ananth CV, Joseph KS, Oyelese Y, Demissie K, Vintzileos AM. Trends in preterm birth and perinatal mortality among singletons: United States, 1989 through 2000. Obstet Gynecol. 2005;105:1084–91. doi: 10.1097/01.AOG.0000158124.96300.c7. [DOI] [PubMed] [Google Scholar]
- 15.Chen A, Feresu SA, Barsoom MJ. Heterogeneity of preterm birth subtypes in relation to neonatal death. Obstet Gynecol. 2009;114:516–22. doi: 10.1097/AOG.0b013e3181b473fc. [DOI] [PubMed] [Google Scholar]
- 16.Reddy UM, Ko CW, Raju TN, Willinger M. Delivery indications at late-preterm gestations and infant mortality rates in the United States. Pediatrics. 2009;124:234–40. doi: 10.1542/peds.2008-3232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.German RR, Lee LM, Horan JM, Milstein RL, Pertowski CA, Waller MN. Updated guidelines for evaluating public health surveillance systems: recommendations from the Guidelines Working Group. MMWR Recomm Rep. 2001;50:1–35. quiz CE1–7. [PubMed] [Google Scholar]
- 18.Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2009. Natl Vital Stat Rep. 2010;59:1–19. [PubMed] [Google Scholar]
- 19.Engle WA, Tomashek KM, Wallman C. “Late-preterm” infants: a population at risk. Pediatrics. 2007;120:1390–401. doi: 10.1542/peds.2007-2952. [DOI] [PubMed] [Google Scholar]
- 20.Davidoff MJ, Dias T, Damus K, et al. Changes in the gestational age distribution among U.S. singleton births: impact on rates of late preterm birth, 1992 to 2002. Semin Perinatol. 2006;30:8–15. doi: 10.1053/j.semperi.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 21.Bannerman CG, Fuchs KM, Young OM, Hoffman MK. Non-spontaneous late preterm birth: etiology and outcomes. Am J Obstet Gynecol. 2011;205:456.e1–6. doi: 10.1016/j.ajog.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 22.Iams JD. Late preterm birth: more and better data needed. Am J Obstet Gynecol. 2011;205:395. doi: 10.1016/j.ajog.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 23.Healthy Babies are Worth the Wait. 2011 [Available at: http://www.marchofdimes.com/professionals/medicalresources_hbww.html] [PubMed]
- 24.Oshiro BT, Henry E, Wilson J, Branch DW, Varner MW. Decreasing elective deliveries before 39 weeks of gestation in an integrated health care system. Obstet Gynecol. 2009;113:804–11. doi: 10.1097/AOG.0b013e31819b5c8c. [DOI] [PubMed] [Google Scholar]
- 25.Clark SL, Frye DR, Meyers JA, et al. Reduction in elective delivery at <39 weeks of gestation: comparative effectiveness of 3 approaches to change and the impact on neonatal intensive care admission and stillbirth. Am J Obstet Gynecol. 2010;203:449 e1–449 e6. doi: 10.1016/j.ajog.2010.05.036. [DOI] [PubMed] [Google Scholar]
- 26.VitalStats. [Available at: http://www.cdc.gov/nchs/vitalstats.htm]
- 27.Sunderam S, Chang J, Flowers L, et al. Assisted reproductive technology surveillance – United States, 2006. MMWR Surveill Summ. 2009;58:1–25. [PubMed] [Google Scholar]
- 28.Basso O, Baird DD. Infertility and preterm delivery, birthweight, and Caesarean section: a study within the Danish National Birth Cohort. Hum Reprod. 2003;18:2478–84. doi: 10.1093/humrep/deg444. [DOI] [PubMed] [Google Scholar]
- 29.Honein M, Kirby R, Meyer R, et al. The association between major birth defects and preterm birth. Matern Child Health J. 2009;13:164–75. doi: 10.1007/s10995-008-0348-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Strobino DM, Ensminger ME, Kim YJ, Nanda J. Mechanisms for maternal age differences in birth weight. Am J Epidemiol. 1995;142:504–14. doi: 10.1093/oxfordjournals.aje.a117668. [DOI] [PubMed] [Google Scholar]
- 31.McGrady GA, Sung JF, Rowley DL, Hogue CJ. Preterm delivery and low birth weight among first-born infants of black and white college graduates. Am J Epidemiol. 1992;136:266–76. doi: 10.1093/oxfordjournals.aje.a116492. [DOI] [PubMed] [Google Scholar]
- 32.Brown HL, Chireau MV, Jallah Y, Howard D. The “Hispanic paradox”: an investigation of racial disparity in pregnancy outcomes at a tertiary care medical center. Am J Obstet Gynecol. 2007;197:197 e1–197 e7. doi: 10.1016/j.ajog.2007.04.036. discussion e7–9. [DOI] [PubMed] [Google Scholar]
- 33.Kirby RS, Wingate MS. Late preterm birth and neonatal outcome: is 37 weeks’ gestation a threshold level or a road marker on the highway of perinatal risk? Birth. 2010;37:169–71. doi: 10.1111/j.1523-536X.2010.00399.x. [DOI] [PubMed] [Google Scholar]
- 34.Wang ML, Dorer DJ, Fleming MP, Catlin EA. Clinical outcomes of near-term infants. Pediatrics. 2004;114:372–6. doi: 10.1542/peds.114.2.372. [DOI] [PubMed] [Google Scholar]
- 35.Escobar GJ, Greene JD, Hulac P, et al. Rehospitalisation after birth hospitalisation: patterns among infants of all gestations. Arch Dis Child. 2005;90:125–31. doi: 10.1136/adc.2003.039974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hibbard JU, Wilkins I, Sun L, et al. Respiratory morbidity in late preterm births. JAMA. 2010;304:419–25. doi: 10.1001/jama.2010.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Abe K, Shapiro-Mendoza CK, Hall LR, Satten GA. Late preterm birth and risk of developing asthma. J Pediatr. 2010;157:74–8. doi: 10.1016/j.jpeds.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 38.Chyi LJ, Lee HC, Hintz SR, Gould JB, Sutcliffe TL. School outcomes of late preterm infants: special needs and challenges for infants born at 32 to 36 weeks gestation. J Pediatr. 2008;153:25–31. doi: 10.1016/j.jpeds.2008.01.027. [DOI] [PubMed] [Google Scholar]
- 39.Gurka MJ, LoCasale-Crouch J, Blackman JA. Long-term cognition, achievement, socioemotional, and behavioral development of healthy late-preterm infants. Arch Pediatr Adolesc Med. 2010;164:525–32. doi: 10.1001/archpediatrics.2010.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Petrini JR, Dias T, McCormick MC, Massolo ML, Green NS, Escobar GJ. Increased risk of adverse neurological development for late preterm infants. J Pediatr. 2009;154:169–76. doi: 10.1016/j.jpeds.2008.08.020. [DOI] [PubMed] [Google Scholar]
- 41.Romeo DM, Di Stefano A, Conversano M, et al. Neurodevelopmental outcome at 12 and 18 months in late preterm infants. Eur J Paediatr Neurol. 2010;14:503–7. doi: 10.1016/j.ejpn.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 42.Shapiro-Mendoza CK, Tomashek KM, Kotelchuck M, et al. Effect of late-preterm birth and maternal medical conditions on newborn morbidity risk. Pediatrics. 2008;121:e223–32. doi: 10.1542/peds.2006-3629. [DOI] [PubMed] [Google Scholar]
- 43.Colin AA, McEvoy C, Castile RG. Respiratory morbidity and lung function in preterm infants of 32 to 36 weeks’ gestational age. Pediatrics. 2010;126:115–28. doi: 10.1542/peds.2009-1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Joseph KS, Nette F, Scott H, Vincer MJ. Prenatal corticosteroid prophylaxis for women delivering at late preterm gestation. Pediatrics. 2009;124:e835–43. doi: 10.1542/peds.2009-0905. [DOI] [PubMed] [Google Scholar]
- 45.Ananth CV, Liu S, Joseph KS, Kramer MS. A comparison of foetal and infant mortality in the United States and Canada. Int J Epidemiol. 2009;38:480–9. doi: 10.1093/ije/dyn194. [DOI] [PubMed] [Google Scholar]
- 46.Joseph KS, Demissie K, Kramer MS. Obstetric intervention, stillbirth, and preterm birth. Semin Perinatol. 2002;26:250–9. doi: 10.1053/sper.2002.34769. [DOI] [PubMed] [Google Scholar]
- 47.Lisonkova S, Hutcheon JA, Joseph KS. Temporal trends in neonatal outcomes following iatrogenic preterm delivery. BMC Pregn Childbirth. 2011;11:39. doi: 10.1186/1471-2393-11-39. [DOI] [PMC free article] [PubMed] [Google Scholar]