Abstract
Excess intake of sodium, a common problem worldwide, is associated with hypertension and cardiovascular disease (CVD), while hypertension is a major risk factor for CVD. Population-wide efforts to reduce sodium intake have been identified as a promising strategy for preventing hypertension and CVD, and such initiatives are currently recommended by a variety of scientific and public health organizations. By reviewing the literature published from January 2011 to March 2013, we summarized recent economic evidence on interventions to reduce sodium intake. The evidence supports population-wide interventions for reducing sodium intake worldwide. Both lowering the salt content in manufactured foods and conducting mass media campaigns at national level are cost-effective in preventing CVD. Although better data on the cost of interventions is needed for rigorous economic evaluations, population-wide sodium reduction can be a promising approach for containing the growing health and economic burden associated with hypertension and its sequelae.
Keywords: Salt intake, sodium, cardiovascular disease, costs, hypertension, interventions
Introduction
In 2008, cardiovascular disease (CVD), the number one cause of death in the world, accounted for an estimated 17.3 million deaths, or 30% of all deaths in that year [1]. Furthermore, CVD is projected to remain the leading cause of death worldwide in the next several decades [2]. All told, low- and middle-income countries experienced over 80% of all CVD deaths in 2008 [1], while the economic burden of CVD in developed countries continues to be staggering. Indeed, the annual cost of CVD in the United States (US) was conservatively estimated for 2009 at $312.6 billion [3]. In the European Union, an analysis found that CVD cost 169 billion euros in 2003, with 62% of these costs for health care, 21% for loss of productivity, and 17% for informal care [4]. In the United Kingdom (UK) alone, CVD cost 29.1 billion pounds (about $53.0 billion) in 2004, 29% of which was for coronary heart disease and 27% for cerebrovascular disease [5]. Globally, the most important risk factor for CVD is hypertension while suboptimal blood pressure (systolic blood pressure ≥ 115 mmHg) is responsible for an estimated 62% of strokes and 49% of coronary heart diseases worldwide [6]. The economic burden of hypertension ranged 5−15% of the gross domestic product (GDP) in developed countries and 2.5−8.0% of GDP in developing countries [7]. These alarming statistics, combined with ageing population and the growth in major risk factors such as obesity and physical inactivity, have caught the attention of global leaders, and in 2011 the United Nations called for setting a new international agenda on noncommunicable diseases, like heart disease and stroke, and a focus on major risk factors like high intake of salt and the use of tobacco [8].
Reducing sodium intake has repeatedly been documented effective in lowering risk of CVD and hypertension [9–22] although some literature still questioned the validity of universal reduction of sodium intake [23, 24]. In fact, initiatives promoting a reduction in sodium intake began as early as the 1970s, and there are success stories in Finland and the UK [18, 25, 26]. In the US, efforts to reduce sodium started as early as 1969, when at the White House Conference on Food, Nutrition and Health, excess sodium intake was linked to hypertension [27], and since the 1980s, advice has been consistent that the public should reduce salt intake [18]. Recently actions in North America have accelerated. In April 2010, the Institute of Medicine released a report on strategies to reduce sodium intake in the US [28], and in May 2013 released sodium intake in population: assessment of evidence [24]; in Canada, in 2010, the federal and provincial governments agreed to an interim target of 5.75 g/day salt by 2016 [29]. Similarly, in developing countries, sodium reduction has been on the public health priority agenda. In February 2010, the Pan American Health Organization−World Health Organization (WHO) regional expert group on preventing CVD through the reduction of dietary salt outlined its recommendations for a population-based approach. In September 2011, South Africa set a target to reduce salt intake to <5 g/person/day (~2000 mg sodium/person/day) by the year 2020 through a public health campaign and by regulating the food industry [14]. Irrespective of the initiatives already under way, economic analysis can help inform selection of intervention strategies for reducing salt intake. This summary of the current status of economic evaluation of sodium reduction to prevent CVD can be helpful in informing current initiatives, and revising current interventions or developing new ones to improve cost-effectiveness. Appropriately designed interventions to reduce sodium intake should improve public health by reducing the growing burden of hypertension and CVD worldwide.
Major types of economic evaluations of preventing CVD by reducing sodium intake
The presence of a public health problem is not a sufficient justification for public intervention. First, the societal costs of the intervention should be less than its expected social benefits. Second, because resources are limited, even if the costs are lower than the benefits, there is still often a need to compare these costs and benefits with those of other interventions to judge whether the possible investment in the intervention being considered is the best use of resources [30–32]. Accordingly, not all potentially beneficial interventions can be funded and/or implemented, i.e., choices must be made in allocating scarce resources.
Figure 1 depicts the linkages between the 5 major types of economic evaluation and the impact of interventions to reduce sodium intake for the purpose of preventing CVD. For any kind of intervention, the most basic economic evaluation is a cost analysis, although researchers often start with a cost-of-illness study. As the evaluation of interventions become more detailed, however, the need to consider the cost of the intervention will become more apparent. In fact, cost analysis is an important component of all economic evaluations and often serves as the foundation for all other kinds of economic evaluations [33].
Fig 1.
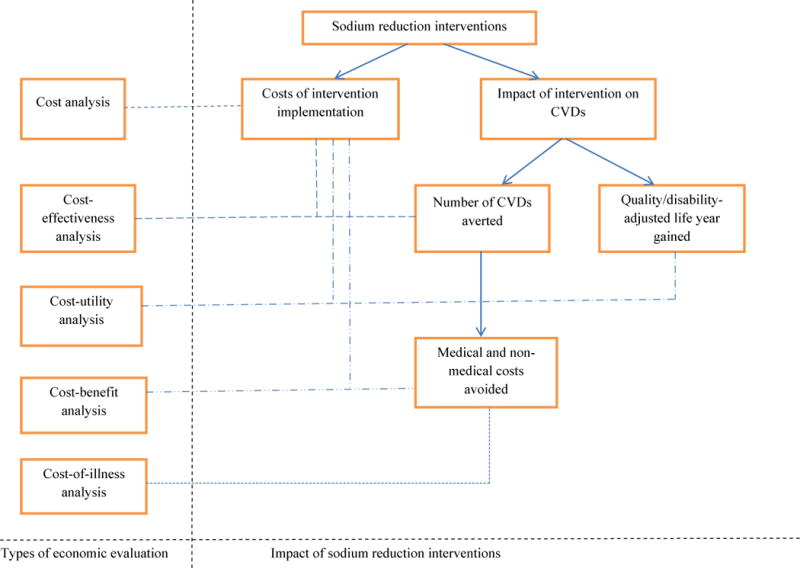
Types of economic evaluation of initiatives to prevent cardiovascular disease (CVD) by sodium reduction
The 3 other types of economic evaluation shown in Figure 1 link the costs (either of the intervention, the illness, or both) with health outcomes from interventions. Because health outcomes are often measured by the number of diseases or deaths averted (CVD’s averted in Figure 1), one natural way of linking the costs of intervention with the health outcomes is the cost per case averted or per death avoided. This is done in a typical cost-effectiveness analysis, and it is often measured by a cost-effectiveness ratio derived by dividing the costs of the intervention by the incremental health outcomes associated with that intervention. Another type of analysis, called cost-utility analysis, links the cost of intervention to the number of life years gained from the intervention. Here, the number of life years gained is often measured by quality-adjusted life years (QALYs) or disability-adjusted life years (DALYs) to produce standardized measures. The validity of both QALYs and DALYs is debatable, however, and their use in economic evaluations should be approached with caution [34].
If the number of cases of the disease in question or the deaths averted can be measured or converted to monetary terms, the linkage between the costs of the intervention and health outcomes can be expressed as a cost-benefit analysis. The cost-benefit ratio is derived by dividing the costs of the intervention by the incremental monetized health outcomes. Alternatively, researchers can look at the net benefit, which simply is the difference between total benefits from the intervention and its costs. In the cost-benefit analysis, because there are no natural prices for health and human life, artificial prices must be created by methods such as willingness to pay. More often than not, however, valuing human life and health in monetary terms is a challenging issue to researchers as well as to the public [35].
Recent economic evaluations of interventions to prevent cardiovascular disease through sodium reduction
Identifying the literature
Using the search terms sodium, salt, dietary, and sodium chloride combined with the terms economics, costs, health care expenditure, health care costs, cost analysis, cost-effectiveness, cost-benefit, cost-utility, and economic aspects of illness, we searched 6 databases and found 91 potentially relevant articles published in English during the period of January 2011 to March 2013: PubMed, n=24; ABI Inform, n=17; EconLit, n=10; Cinahl, n=21; Embase, n=10; and WOS, n=9. After screening them to remove obviously irrelevant articles, reviews, commentary, duplicates, and articles not related to CVD, we identified 5 original research articles for the present review. In addition, we identified a publication of apparent relevance that was written in Spanish but had an English abstract. With that abstract and a Google translation (Google, Mountain View, CA) of the text and tables, we were able to obtain sufficient economic information and thus included it in our review. In all, the 6 publications came from 6 different countries: the US [36], the UK [37], Finland [38], Vietnam [39], Australia [40], and Argentina [41]. Although all but 2 were cost-effectiveness studies (1 was a cost-of-illness study and 1 a cost-utility analysis), they all included at least 2 types of economic evaluation (Table 1).
Table 1.
Types and elements of economic evaluations for preventing cardiovascular disease by reducing sodium intake published during the period of January 2011 to March 2013
| Lead author/country | Cost analysis | Cost-effectiveness analysis | Cost-utility analysis | Cost of illness |
|---|---|---|---|---|
| Gase/US [36] | √ | √ X | ||
| Barton/UK [37] | √ X | √ | ||
| Martikainen/Finland [38] | √ | √ X | √ | √ |
| Ha/Vietnam [39] | √ | √ X | ||
| Cobiac/Auatralia [40] | √ | √ X | √ | |
| Ferrante/Argentina [41] | √ | √ X | √ |
√ denotes that this type of economic evaluation was included in the study.
X denotes the main type of economic evaluation in the study.
No studies used cost-benefit analysis.
The selected studies (Table 2)
Table 2.
Summary information on economic evaluations of initiatives to prevent cardiovascular disease by sodium reduction: from the literature published in January 2011−March 2013
| Lead author/country | Interventions/population/methods | Intervention costs | Economic benefits | Conclusions | Key shortcomings |
|---|---|---|---|---|---|
| Gase/US [36] | Postulated a county government food-procurement policy to reduce sodium consumption/Adults and children were potentially affected by the policy/Included a health impact assessment and simulation | Costs of implementing the policy, including staffing, training, tracking, oversight, promotion, food, and start-up. | Direct health care costs of hypertension could be decreased by $629,724 per year in the intervention county. | A food-procurement policy aimed at reducing sodium intake in various food-service settings could achieve substantial positive health and economic effects. | Used too many key assumptions due to lack of data |
| Barton/UK [37] | Population-wide reduction of salt intake by 3g/day in a modeling study/Whole population of England and Wales (approximately 50 million)/Spreadsheet model | Not specified. | Prevent 4,450 deaths with savings of 347 million pounds over a decade, or annual savings of 40 million pounds. | Any salt-reduction intervention costing up to 40 million pounds a year would be cost saving. | No particular program was proposed |
| Martikainen/Finland [38] | Markov model/Focus on population-wide modest salt reduction, and quality improvement of fat in food among Finnish adults aged 30−74 years in 2007 | Costs, from a societal perspective, included direct costs of prevention, morbidity, rehabilitation, and loss of production. | Over 20 years, the intervention could prevent 8,000–13,000 CVD cases, yield an additional 26,000–45,000 QALYs, and save 150–225 million euros. | Even a modest reduction of dietary salt with quality improvement of fat can substantially reduce CVD burden, with large cost saving from a societal perspective. | Used too many restrictions and assumptions; No particular intervention was specified. |
| Ha/Vietnam [39] | Mass media education program on reducing salt intake and tobacco use/National populations (not specifically specified/WHO-CHOICE methods and analytical models | Program costs of training, administration and mass media; patient costs of diagnostic and laboratory tests, consultation, drugs, and hospital and clinic visits. | A mass media education program to reduce salt intake is the most cost-effective (US$118/DALY averted). | A health education program to reduce salt intake and a combined mass media program on salt/tobacco/cholesterol are the best use of government budget. | Heavily depend on expert opinions and data from other countries. |
| Cobiac/Australia [40] | A governmentally imposed mandatory reduction of salt in breads, margarine, and cereals/Australian adults aged 35–84 years/WHO’s generalized cost-effectiveness analysis. | Costs of legislative changes and enforcement for the mandatory program are derived from WHO unit costs. | Mandatory salt limits led to 80,000 DALYs gained and cost saving. | Mandating the use of less salt in breads, margarines, and cereals is easily the most effective and cost-effective strategy for primary prevention of CVD. | Implementation cost of government policy on mandatory salt reduction was hardly quantified. |
| Ferrante/Argentina [41] | Assuming reduction in salt content of food by 5% to 25%/Argentine adults aged 35–84 years/A simulation model. | Cost of human resources, biochemical analysis of food, transportation, mass media campaign. | A net saving ranging from US $2.080 billion to $3.765 billion. | Implementing this strategy to reduce salt intake would lead to both QALY gains and savings in economic resources. | No specific intervention program for salt reduction was specified |
United States
A study [36] conducted in the county of Los Angeles, California, examined the impact on blood pressure and health care costs of a local policy to reduce sodium intake. The intervention was a food-procurement policy implemented by the county to reduce the intake of sodium in various settings. The study presented 2 policy scenarios to reduce the sodium content of foods: 1) reducing the sodium content of all foods in the settings of child care, senior meal programs, cafeterias, and mobile trucks; and 2) reducing sodium content by labeling foods and by promoting, subsidizing, and providing low-sodium food options in hospitals and in county government cafeterias. Using health impact assessment methods and considering the best available empirical evidence as well as the opinions, experience, and expectations of those who would be affected by the proposed policy, the authors found that if the sodium-reduction strategies were implemented, adults in the county would consume 233 fewer mg of sodium per day, on average, in 2010. This would correspond to an average decrease of 0.71 mmHg in systolic blood pressure (SBP) among adults with hypertension, 388 fewer cases of uncontrolled hypertension, and a decrease per year of $629,724 in direct health care costs.
However, the study did not provide robust data on most cost components of implementing the intervention, and thus there were no cost-effectiveness measures presented. Because of the variety of assumptions used and the intervention strategies postulated, the health benefits and savings in health care costs that were postulated should be considered potential at best.
United Kingdom
Using a spreadsheet model to quantify the reduction in CVD over a decade that would proceed from a population-wide risk-reduction program, this study [37] estimated the potential cost-effectiveness of such a program. Major outcomes were the number of cardiovascular events avoided, QALYs gained, and savings achieved in health care costs for a given level of effectiveness; the study also produced estimates of how much it would be worth spending to achieve a specific outcome.
The authors found that legislation or other measures to reduce the intake of salt by 3 g/day/person (in a population where current mean intake was about 8.5g/day) would reduce mean population SBP by approximately 2.5 mmHg, prevent about 30,000 cardiovascular events and approximately 4,450 deaths, and produce discounted savings overall of approximately 347 million pounds (about $684 million) over a decade, which would be equivalent to annual savings of approximately 40 million pounds. Thus, salt-reduction interventions that cost less than 40 million pounds a year that achieved the proposed sodium reduction would be cost saving. Further, any intervention that achieved even a modest population-wide reduction in the incidence of any major cardiovascular risk factor would produce a net cost saving to the National Health Service of the UK while also improving health. Unfortunately, this paper did not detail the specific costs of particular programs.
Finland
In this study [38], a Markov model with a dynamic population structure was developed to present the natural history of CVD based on the most current information on the age- and sex-specific risk factors for CVD, dietary habits, and nutrient intake of the Finnish population aged 30−74 years. The authors applied the model to predict the health economic consequences of modest reductions in the daily intake of salt and the replacement of saturated fat with polyunsaturated fat in the population of interest. For the 20 years beginning in 2007, the model predicted that this intervention could potentially prevented 8,000−13,000 CVD cases, and meanwhile added 26,000 to 45,000 QALYs and saved 150−225 million euros (about $203–204 million). Thus a modest reduction in salt intake and replacing saturated fat with polyunsaturated fat in foods can significantly reduce the adult Finnish population’s burden of CVD.
In this study, costs were estimated from a societal perspective and included the direct cost of prevention, morbidity, rehabilitation, and production losses due to nonfatal CVD events. Age- and sex-specific estimates of quality of life (QoL) were used to represent the average QoL in the Finnish population. The dietary reduction of 1 g of salt per day was assumed to lower SBP by approximately 1.185 mmHg among hypertensive subjects and by 0.595 mmHg among normotensive subjects. One shortcoming of the study is that it did not specify any particular intervention aimed at reducing dietary salt and intake of saturated fat, thus the cost of specific activities was unclear.
Vietnam
This study [39] was performed to assess the costs, health effects, and the cost-effectiveness of a group of personal and non-personal (i.e., at the individual and population level) strategies to reduce CVD in Vietnam. The interventions, 23 in total, included a mass media campaign that advocated reduced consumption of salt and tobacco, the use of drugs for lowering blood pressure or cholesterol, and employing combined drug therapy for people at varying absolute risk of a cardiovascular event. A health education program to reduce salt intake was the most cost-effective measure at the population level, and treating people who had an SBP above 160 mmHg was the most cost-effective measure at the individual level. The authors asserted that a mass media education program on salt intake and a combination mass media program that focused on salt intake, cholesterol level, and tobacco use should be selected first. Among the 23 interventions considered in this study, the least costly was a health education program using the mass media to reduce salt intake, with a total cost per year of VND (Viet Nam Dong) 89 billion (equals US $0.06/person). It was also the most cost-effective at VND 1.9 million (US $118) per DALY averted.
In this study, costs were comprised of program and patient-related costs. Program costs were those incurred at the national, provincial, and district administrative levels, including training, program administration, and mass media, while patient costs were incurred at the point of delivery and consisted of diagnostic and laboratory tests, consultation, drugs, and hospital and health center visits. However, the very low cost of the health education program merits further investigation to ensure the validity of the data.
Australia
Using a Markov simulation model, the authors of this study [40] evaluated the cost-effectiveness of interventions to prevent CVD in the Australia population of men and women aged 35−84 years. The study examined 2 interventions targeting the whole population: (a) a community heart health program, and (b) mandatory reduction of salt in the manufacture of breads, margarines, and cereals; it also examined 6 other interventions aimed at high-risk populations.
The authors concluded that reduction of salt in breads, margarines, and cereals is clearly the more effective and cost-effective strategy for the primary prevention of CVD; it produces larger improvements in population health, and between the two interventions considered, it can save the most money for the health sector. The authors asserted that to achieve best value for money in the primary prevention of CVD, the Australian government must take a tougher approach in mandating limits on salt in processed foods. One drawback to the study is that although it considered or included a variety of cost items from a number of sources, it is not clear whether these data were valid inputs into the model, especially the cost of mandatory salt reduction. For example, the authors did not mention the costs to government of implementing the policy or describe the costs to the manufacturers. These should have been included as intervention costs.
Argentina
This study [41] employed a simulation model to measure the impact of policies on heart disease in Argentina in order to predict trends in incidence, prevalence, mortality, and cost for CVD in the population aged 35–84 years. The cost of intervention included the cost of human resources, transportation, and a mass media campaign. The authors estimated the cost-utility ratio of an intervention among people aged ≥35 years that involved reducing the salt content of foods by 5% to 25%; these researchers modeled the impact and costs of a 3-g daily reduction in dietary salt intake by reducing the salt in processed food and the amount of salt that participants added to foods over a 10-year period.
In the high-impact scenario, the intervention generated a net savings of US $3.77 billion and an increase of 656,657 QALYs; in the low-impact scenario these figures were US $2.08 billion and 401,659 QALYs. It was estimated that there would be a 24.1% reduction in the incidence of heart disease, 21.6% in acute myocardial infarction, 20.5% in stroke, 19.9% in mortality from heart disease, and 6.4% in all-cause mortality. Benefits were observed for both genders and for all age groups. Thus, implementing this strategy to reduce salt intake would produce a very positive impact in terms of QALY gains and savings in the use of economic resources. But this study did not present the variations of cost of interventions between high-impact and low-impact scenarios.
Summary and conclusions
Five of the 6 studies that we reviewed listed the cost components of the intervention to at least some extent, but none of them used robust cost data. In the US study, which involved a local food-procurement policy to reduce sodium intake, the cost of implementation was only based on the literature as well as data gathered from interviews with 30 agency representatives and food vendors [36]. In the study from Finland [38], which involved a Markov model and not an actual intervention, the authors used a societal perspective to list the costs of prevention efforts, morbidity, rehabilitation, and loss of production due to nonfatal CVD events. These are not the estimated costs of an intervention to reduce salt intake, however. In the Vietnam study, for mass media campaigns (one of the options), the program costs included training, program administration, and mass media [39]. The cost estimates were based largely on expert opinion. In the Australia study [40], the costs of mandatory salt reduction were the costs of legislative changes and enforcement. Estimates for all these costs came from other studies or various sources. In the Argentina study, the costs of an intervention to reduce sodium intake included human resources, biochemical analysis of food, transportation, and a mass media campaign [41]. However, the study did not vary the cost when health outcome changed from low-impact to high-impact scenarios. In the UK, the study authors pointed out that no detailed specific costs of particular programs were available [37].
Although 5 of the 6 studies listed cost categories for the intervention(s), all of the cost data were incomplete. This shortcoming, in turn, may have limited the robustness of the results for cost-effectiveness, thereby limiting the public health implications of these studies [42]. There might be two major reasons on why the cost data were so inadequate? First, the population-wide interventions were not well defined. When the description of the intervention was not concrete or specific enough, it was hard for the authors to estimate intervention costs. Second, there might have been no economic evaluation component when the interventions were being developed or implemented. Further, all the economic evaluations were conducted after the interventions started. Thus, at best, the authors could only collect data on costs retrospectively.
Health outcomes in the studies we reviewed were measured by the number of CVD cases or deaths averted, QALYs/DALYs gained, blood pressure reduction, and health care costs saved. Five of the 6 studies presented the health care costs saved. This is useful information for advocacy purposes, but not necessary for demonstrating cost-effectiveness. Support for the study conclusions would have been stronger with more robust data on health care costs. In addition, the saving in health care costs is only a proportion of the total cost saving, as indirect costs such as productivity loss and the cost of informal care are often very large when CVD is the primary problem [4, 43]. Although the Finnish study [38] listed the costs of rehabilitation and lost production, it appears that the authors confused health care costs with the costs of intervention.
Except for the US study which was a county level investigation, all other studies claimed a significant health and economic benefit through population-wide sodium reduction. It is interesting that although the body of literature was small, the 6 studies we analyzed in detail included both developed and developing countries and involved the geographic regions of North America, South America, Europe, Australia, and Asia. This suggests that population-wide efforts to reduce sodium intake are of interest globally. This is important because both hypertension and CVD affect all populations around the world. Furthermore, all evaluations claimed the population-wide interventions to be cost-effective or cost-beneficial. Because the body of literature was small and there was only one study conducted in each country, we cannot derive an overall comparative measure of cost-effectiveness across countries. Conducting cost-effectiveness analysis using multi-country level data might be necessary.
While the results of cost-effectiveness analyses are helpful to decision makers in prioritizing public health interventions [44], valid cost-effectiveness evaluations must be based on robust data on the cost of interventions. Without high-quality data, even the best method cannot produce useful results. Conversely, with high-quality data on costs, a cost analysis of the intervention will provide decision makers and program developers a stronger economic argument for implementing or not implementing interventions. We also need rigorous estimates of the economic burden of CVD, kidney disease and other health conditions closely related to hypertension, especially estimates that include their indirect costs.
In conclusion, our review of recent literature allowed us to summarize the most recent economic evidence on reduction of sodium intake as it relates to the prevention of hypertension and CVD. The evidence generally supports population-wide interventions to achieve sodium reduction, although in each country only a single study is available on key intervention strategies such as reducing the salt content in manufactured foods and conducting mass media campaigns. The findings reinforced the findings in the literature [42]. In the US, all previous studies used Markov or other simulation models for their cost-effectiveness evaluation and used medical cost saving as outcomes [45–49]. None of these studies mentioned the costs of intervention. Although the most recent US study [36] did not provide convincing cost of the intervention, authors went to extra efforts in obtaining some of the costs for intervention implementation from the communities. This is one good step toward developing practical intervention programs. In other developed countries, we did not find the similar efforts. In developing countries, the previous literature [50, 51] used too general data and methods and treated a large geographic area as a region for cost-effectiveness evaluation. Overall, although more robust data on the costs of interventions and more empirical data on health outcomes (health outcomes presented in the literature were based on projections and simulations) are needed to conduct rigorous economic evaluations, population-wide sodium reduction is promising in addressing the public health burden of hypertension, atherosclerosis, and their sequelae.
Acknowledgments
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the U.S. Centers for Disease Control and Prevention (CDC).
Footnotes
There is no potential conflict of interest related to any part of this article.
References
- 1.World Health Organization. Global status report on noncommunicable diseases 2010. Geneva: WHO; 2011. [Google Scholar]
- 2.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013:e6–245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leal J, Luengo-Fernández R, Gray A, Petersen S, Rayner M. Economic burden of cardiovascular diseases in the enlarged European Union. Eur Heart J. 2006;27:1610–1619. doi: 10.1093/eurheartj/ehi733. [DOI] [PubMed] [Google Scholar]
- 5.Luengo-Fernández R, Leal J, Gray A, Petersen S, Rayner M. Cost of cardiovascular diseases in the United Kingdom. Heart. 2006;92:1384–1389. doi: 10.1136/hrt.2005.072173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. The world health report 2002 – reducing risks, promoting healthy life. Geneva: WHO; 2002. Available at http://www.who.int/whr/2002/en/whr02_en.pdf. Accessed May 23, 2013. [Google Scholar]
- 7.Pan American Health Organization-World Health Organization. Cardiovascular disease prevention through dietary salt reduction. Washington, DC: PAHO-WHO; 2011. Available at http://new.paho.org/hq/index.php?option=com_content&task=view&id=2015&itemid=1757. Accessed April 5, 2013. [Google Scholar]
- 8.United Nations. Political declaration of the high-level meeting of the general assembly on the prevention and control of non-communicable diseases. 2012 Jan 24; Available at http://www.who.int/nmh/events/un_ncd_summit2011/political_declaration_en.pdf, Accessed April 4, 2013.
- 9.Morrison AC, Ness RB. Sodium intake and cardiovascular disease. Annu Rev Public Health. 2011;32:71–90. doi: 10.1146/annurev-publhealth-031210-101209. [DOI] [PubMed] [Google Scholar]
- 10.He FJ, MacGregor GA. Salt reduction lowers cardiovascular risk: meta-analysis of outcome trials. Lancet. 2011;378:380–382. doi: 10.1016/S0140-6736(11)61174-4. [DOI] [PubMed] [Google Scholar]
- 11.Cook NR, Cutler JA, Obarzanek E, et al. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP) BMJ. 2007;334:885–888. doi: 10.1136/bmj.39147.604896.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Graudal NA, Hubeck-Graudal T, Jürgens G. Effects of low-sodium diet vs. high-sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride (Cochrane Review) Am J Hypertens. 2012;25:1–15. doi: 10.1038/ajh.2011.210. [DOI] [PubMed] [Google Scholar]
- 13.O’Donnell MJ, Yusuf S, Mente A, et al. Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA. 2011;306:2229–2238. doi: 10.1001/jama.2011.1729. [DOI] [PubMed] [Google Scholar]
- 14.He FJ, Campbell NR, MacGregor GA. Reducing salt intake to prevent hypertension and cardiovascular disease. Rev Panam Salud Publica. 2012;32:293–300. doi: 10.1590/s1020-49892012001000008. [DOI] [PubMed] [Google Scholar]
- 15.Strazzullo P, D’Elia L, Kandala NB, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ. 2009;339:b4567. doi: 10.1136/bmj.b4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Coxson PG, Cook NR, Joffres M, et al. Mortality benefits from US population-wide reduction in sodium consumption: projections from 3 modeling approaches. Hypertension. 2013;61:564–570. doi: 10.1161/HYPERTENSIONAHA.111.201293. [DOI] [PubMed] [Google Scholar]
- 17.D’Elia L, Barba G, Cappuccio FP, Strazzullo P. Potassium intake, stroke, and cardiovascular disease: a meta-analysis of prospective studies. J Am Coll Cardiol. 2011;57:1210–1219. doi: 10.1016/j.jacc.2010.09.070. [DOI] [PubMed] [Google Scholar]
- 18.Appel LJ, Frohlich ED, Hall JE, et al. The importance of population-wide sodium reduction as a means to prevent cardiovascular disease and stroke: a call to action from the American Heart Association. Circulation. 2011;123:1138–1143. doi: 10.1161/CIR.0b013e31820d0793. [DOI] [PubMed] [Google Scholar]
- 19.Stolarz-Skrzypek K, Kuznetsova T, Thijs L, et al. Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. JAMA. 2011;305:1777–1785. doi: 10.1001/jama.2011.574. [DOI] [PubMed] [Google Scholar]
- 20.Whelton PK, Appel LJ, Sacco RL, et al. Sodium, blood pressure, and cardiovascular disease: further evidence supporting the American Heart Association sodium reduction recommendations. Circulation. 2012;126:2880–2889. doi: 10.1161/CIR.0b013e318279acbf. [DOI] [PubMed] [Google Scholar]
- 21.Tomonari T, Fukuda M, Miura T, et al. Is salt intake an independent risk factor of stroke mortality? Demographic analysis by regions in Japan. J Am Soc Hypertens. 2011;5:456–462. doi: 10.1016/j.jash.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 22.Gardener H, Rundek T, Wright CB, Elkind MS, Sacco RL. Dietary sodium and risk of stroke in the Northern Manhattan study. Stroke. 2012;43:1200–1205. doi: 10.1161/STROKEAHA.111.641043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alderman MH, Cohen HW. Dietary sodium intake and cardiovascular mortality controversy resolved? AJH. 2012 doi: 10.1038/ajh.2012.52. [DOI] [PubMed] [Google Scholar]
- 24.Institute of Medicine. Sodium intake in population: assessment of evidence. Washington, DC: IOM; 2013. Available at http://iom.edu/Reports/2013/Sodium-Intake-in-Populations-Assessment-of-Evidence.aspx. Accessed May 22, 2013. [Google Scholar]
- 25.National Health Service National Institute for Health and Clinical Excellence. Prevention of cardiovascular disease at population level. NICE public health guidance 25. 2010 Available at http://guidance.nice.org.uk/PH25. Accessed April 16, 2013.
- 26.World Health Organization (WHO) Reducing salt intake in populations: report of a WHO forum and technical meeting. Geneva: WHO; 2007. pp. 1–60. [Google Scholar]
- 27.Establishing Guidelines for the Nutrition of Vulnerable Groups (with special reference to the poor) 1969 Conference on Food, Nutrition, and Health. :37–100. Available at http://www.nns.nih.gov/1969/full_report/PDFcontents.htm, Accessed April 16, 2013.
- 28.Institute of Medicine. Strategies to reduce sodium intake in the United States. Washington, DC: IOM; 2010. Available at www.iom.edu/reports/2010/strategies-to-reduce-sodium-intake-in-the-United-States.aspx. Accessed March 30, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sodium Working Group. Sodium reduction strategy for Canada. Ottawa: Health Canada; 2010. Available at http://publications.gc.ca/collections/collection_2010/sc-hc/H164-121-2010-eng.pdf. Accessed March 30, 2013. [Google Scholar]
- 30.Dalziel K, Segal L, Mortimer D. Review of Australia health economic evaluation—245 interventions: what can we say about cost-effectiveness? Cost Eff Resour Alloc. 2008;6:9. doi: 10.1186/1478-7547-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schwappach DLB, Boluarte TA, Suhrcke M. The economics of primary prevention of cardiovascular disease—a systematic review of economic evaluations. Cost Eff Resour Alloc. 2007;5:5. doi: 10.1186/1478-7547-5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rubinstein A, Garcia Marti S, Souto A, Ferrante D, Augustovski F. Generalized cost-effectiveness analysis of a package of interventions to reduce cardiovascular disease in Buenos Aires, Argentina. Cost Eff Resour Alloc. 2009;7:10. doi: 10.1186/1478-7547-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention (CDC) Cost analysis. Available at http://www.cdc.gov/owcd/eet/Cost/1.html. Accessed April 6, 2013.
- 34.Kind P, Lafata JE, Matuszewski K, Raisch D. The use of QALYs in clinical and patient decision-making: issues and prospects. Value Health. 2009;12(suppl 1):S27–S30. doi: 10.1111/j.1524-4733.2009.00519.x. [DOI] [PubMed] [Google Scholar]
- 35.Ackerman F. Pricing the priceless: cost-benefit analysis of environmental protection. Univ Penna Law Rev. 2001;150(5) Available at http://law-journals-books.vlex.com/vid/pricing-priceless-cost-benefit-protection-54504662, Accessed April 6, 2013. [Google Scholar]
- 36.Gase LN, Kuo T, Dunet D, Schmidt SM, Simon PA, Fielding JE. Estimating the potential health impact and costs of implementing a local policy for food procurement to reduce the consumption of sodium in the county of Los Angeles. Am J Public Health. 2011;101:1501–7. doi: 10.2105/AJPH.2011.300138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barton P, Andronis L, Briggs A, McPherson K, Capewell S. Effectiveness and cost effectiveness of cardiovascular disease prevention in whole populations: modelling study. BMJ. 2011;28:343. doi: 10.1136/bmj.d4044. d4044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Martikainen JA, Soini EJ, Laaksonen DE, Niskanen L. Health economic consequences of reducing salt intake and replacing saturated fat with polyunsatuarated fat in the adult Finnish population: estimates based on the FINRISK and FINDIET studies. Eur J Clin Nutr. 2011;65:1148–55. doi: 10.1038/ejcn.2011.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ha DA, Chisholm D. Cost-effectiveness analysis of interventions to prevent cardiovascular disease in Vietnam. Health Policy Plan. 2011;26:210–222. doi: 10.1093/heapol/czq045. [DOI] [PubMed] [Google Scholar]
- 40.Cobiac LJ, Magnus A, Lim S, Barendregt JJ, Carter R, Vos T. Which interventions offer best value for money in primary prevention of cardiovascular disease? PLoS One. 2012;7:e41842. doi: 10.1371/journal.pone.0041842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ferrante D, Konfino J, Mejía R, et al. The cost-utility ratio of reducing salt intake and its impact on the incidence of cardiovascular disease in Argentina [in Spanish] Rev Panam Salud Publica. 2012;32:274–280. doi: 10.1590/s1020-49892012001000005. [DOI] [PubMed] [Google Scholar]
- 42.Wang G, Labarthe D. The cost-effectiveness of interventions designed to reduce sodium intake. J Hypertens. 2011;29:1693–1699. doi: 10.1097/HJH.0b013e328349ba18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Heidenreich PA, Trogdon JG, Khavjou OA. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 44.Appel LJ, Angel SY, Cobb LK, et al. Population-wide sodium reduction: the bumpy road from evidence to policy. Ann Epidemiol. 2012;22:417–425. doi: 10.1016/j.annepidem.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Smith-Spangler CM, Juusola JL, Enns EA, Owens DK, Garber AM. Population strategies to decrease sodium intake and the burden of cardiovascular disease: a cost-effectiveness analysis. Ann Intern Med. 2010;152:481–487. doi: 10.7326/0003-4819-152-8-201004200-00212. [DOI] [PubMed] [Google Scholar]
- 46.Bibbins-Domingo K, Chertow GM, Coxson PG, et al. Projected effect of dietary salt reduction on future cardiovascular disease. N Engl J Med. 2012;362:590–599. doi: 10.1056/NEJMoa0907355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Palar K, Sturm R. Potential societal savings from reduced sodium consumption in the U.S. adult population. Am J Health Promot. 2009;24:49–57. doi: 10.4278/ajhp.080826-QUAN-164. [DOI] [PubMed] [Google Scholar]
- 48.Dall TM, Fulgoni VL, 3rd, Zhang Y, et al. Potential health benefits and medical cost savings from calorie, sodium, and saturated fat reductiuons in the American diet. Am J Health Promot. 2009;23:412–422. doi: 10.4278/ajhp.080930-QUAN-226. [DOI] [PubMed] [Google Scholar]
- 49.Dall TM, Fulgoni VL, 3rd, Zhang Y, et al. Predicted national productivity implications of calorie and sodium reductions in the American diet. Am J Health Promot. 2009;23:423–430. doi: 10.4278/ajhp.081010-QUAN-227. [DOI] [PubMed] [Google Scholar]
- 50.Asaria P, Chisholm D, Mathers C, et al. Chronic disease prevention: health benefits and financial costs of strategies to reduce salt intake and control tobacco use. Lancet. 2007;370:2044–2053. doi: 10.1016/S0140-6736(07)61698-5. [DOI] [PubMed] [Google Scholar]
- 51.Murray CJ, Lauer JA, Hutubessy RC, et al. Effectiveness and costs of interventions to lower systolic blood pressure and cholesterol: a global and regional analysis on reduction of cardiovascular-disease risk. Lancet. 2003;361:717–725. doi: 10.1016/S0140-6736(03)12655-4. [DOI] [PubMed] [Google Scholar]


