Abstract
Background and objective
In the USA, the prevalence of hypertension has been high and increasing in recent decades. Even so, little is known about the changes over time in hospitalizations and the economic burden associated with this epidemic. We examined hypertension-associated hospitalizations and costs from 1979 to 2006.
Methods
Using the National Hospital Discharge Survey and the costs of community hospitals in the USA, we analyzed the changes in hypertension-associated hospitalizations and costs over time. We included those hospitalizations with a primary or secondary diagnosis of hypertension among patients aged 25 years and above. We examined changes in costs by adjusting them into year 2008 dollars. The costs included hospital expenses of payroll, employee benefits, professional fees and supplies.
Results
From 1979–1982 to 2003–2006, the proportion of hospitalizations that were associated with hypertension (primary or secondary diagnosis) increased from 1.9% to 5.4%. Among all hypertension-associated hospitalizations, the proportion with a secondary diagnosis of hypertension increased from 81.8% to 95.1%. In 2008 dollars, annual costs for hypertension-related hospitalizations increased from US$ 40 billion (5.1% of total hospital costs) during 1979–1982 to US$ 113 billion (15.1% of total hospital costs) during 2003–2006.
Conclusions
Both the proportions of hospitalizations that were associated with hypertension and the adjusted annual costs of such hospitalizations nearly tripled over the past 28 years. The increases were in substantial measure due to the greatly increasing proportion of hospitalizations in which hypertension was listed as a secondary diagnosis. Interventions for the management of hypertension as a secondary diagnosis might be potentially cost-effective.
Keywords: Economic cost, hospitalization, hypertension, trends, United States
Introduction
One in three adults in the USA has hypertension (1,2), and this disorder is a major contributor to stroke, heart attack and chronic renal disease. Fortunately, early identification and systematic management of hypertension have been shown to reduce its long-term complications (3–6). Yet, while hypertension has been extensively studied in outpatient populations (7–9), to date there have been few reports on hospitalized hypertensive patients and their associated costs. Hypertension itself does not usually lead to hospitalization, but other conditions, such as coronary heart disease (CHD) (10), heart failure (HF) (11) and stroke, could cause admissions among patients with hypertension, in which case it would be considered a secondary diagnosis. In addition, given that one-third of US adults have hypertension, it is important to provide policy makers with information on the economic costs of hypertension-associated hospitalizations as one step toward reducing the high costs of the US healthcare system.
Beyond the issue of a lack of research on hospitalized hypertension patients and their associated costs, there has been very little study on trends over time in hypertension-associated hospitalizations and their costs, even though many researchers have demonstrated a high, and increasing, trend in the prevalence of hypertension (1,12–14) and the enormous economic burden associated with this problem and its related complications (15–19). Using National Hospital Discharge Survey (NHDS) data, we comprehensively examined US trends in hospitalizations with a primary or secondary diagnosis of hypertension. Because for the vast majority (over 95% in both the 2003–2006 NHDS and 2005 MarketScan data (15)) of hospitalized hypertensive inpatients the hypertension was a secondary diagnosis, we extended our trend analysis to hospitalizations involving hypertension where the primary diagnosis was CHD, stroke, HF, other cardiovascular disease (CVD), diabetes or renal disease. In addition to analyzing trends in hypertension-related hospitalizations, we examined the odds ratio for in-hospital death among patients with hypertension. Finally, by combining the number of hospitalizations from the NHDS and the unit cost of hospitalizations obtained from the US Census Bureau, we derived the costs of hypertension-associated hospitalizations during 1979–1982 and 2003–2006.
Methods
Data
The NHDS collects data from the inpatient records of a national sample of hospitals. In 1979–2006, hospitals were eligible for the NHDS if their average length of stay was shorter than 30 days and if they were general hospitals. They were excluded if they were federal, military or Department of Veterans Affairs hospitals or were hospital units of institutions. Hospitals with fewer than six beds were also excluded.
Before 1988, the NHDS relied on a two-stage sample design; from 1988 onward, the survey used a modified, three-stage sample design. Although there were some differences between the original and the new designs, these changes did not affect the ability to conduct a trend analysis over the years of interest (20). Throughout the study period, the survey used systematic random sampling to select discharge records from the sampled hospitals. Because discharges rather than patients were used for selection, individual patients could have been selected more than once if they had multiple hospitalizations.
The patient information obtained included age; sex; expected primary sources of payment; discharge status, including the patient’s disposition (long-term care facility, in-hospital death, etc.); up to seven discharge diagnoses; and number of days hospitalized. We did not analyze data by race because some hospitals did not collect information on that variable (21). Hypertension-associated hospitalizations were identified as those with an ICD-9-CM (International Classification of Diseases, 9th Revision, Clinical Modification) code of 401–405 for the primary or secondary diagnosis (up to six secondary diagnoses were considered). In our analysis of admissions with hypertension as a secondary diagnosis, we used the following ICD-9-CM codes for the six primary diagnoses listed earlier: 410–414 (CHD), 430–438 (stroke), 428 (HF), 390–459 (other CVD, excluding those conditions mentioned above), 250 (diabetes) and 580–589 (renal disease).
For the present study, the hospitalization costs were based on the unit costs (average cost per stay) of community hospitals as listed in the US Census Bureau’s Statistical Abstract for the years of interest (22–23). These costs were based on total hospital expenses, including payroll, employee benefits, professional fees and supplies; other researchers have used this method to examine healthcare costs (17,24–26). Although the costs were not for hypertension specifically and thus may have substantially overestimated or underestimated the actual costs of treating patients with hypertension, the trends in the costs of hypertension hospitalizations should not have been affected to any great degree unless they were differently affected (versus the costs of other kinds of hospitalizations) by changes in technology over the time period.
Statistical analysis
We included all records of hospital admissions of patients aged 25 years and above with any diagnosis of hypertension during the 28-year period of interest (1979–2006). The number of hospitalizations and characteristics of hospitalized patients were estimated after taking into account the sampling weight to reflect the overall US population. Age-standardized hospitalization rates (using the 2000 US standard population) were calculated for blocks of 4 years (i.e. 1979–1982, 1983–1986, … 2003–2006) by using the total weighted number of hospitalizations as the numerator and the US civilian population in the corresponding years as the denominator. These age-standardized hospitalization rates (per 1000) were calculated by diagnosis status (hypertension as the first diagnosis or a secondary diagnosis), sex and age in years (25–64, 65–74, and ≥75).
We further derived selected patient characteristics for three 4-year periods (1979–1982, 1991–1994 and 2003–2006): age (in years), insurance status (private, public, no insurance), median length of stay (in days), first diagnosis and disposition (including in-hospital death). In addition, we calculated the Charlson Comorbidity Index (CCI), which measures the likelihood of death or serious disability in the subsequent year and was derived from up to 18 co-morbidities and complications (27–29). We estimated relative percent changes (RPC) between 1979–1982 and 2003–2006 by dividing the changes over the two periods by the values in the first period. The ORs for in-hospital death among hypertension-related hospitalization patients were calculated by logistic regression while adjusting for age, sex, insurance status, hospitalization year, the CCI and primary diagnosis.
To quantify and compare the costs of hospitalizations over time, we first estimated the number of hospital stays in the earliest 4-year (1979–1982) and the most recent 4-year (2003–2006) periods by the first and secondary diagnosis, separately. Then, based on the hospital stays, we derived the costs by multiplying the number of hospital stays by the average cost per stay, which was US$2041 in 1979–1982 (22) and US$8480 in 2003–2006 (23). For comparison purposes, we adjusted the hospital costs to 2008 dollars by using the consumer price indices of medical care costs for hospital and related services (23).
Results
During the 28-year period, there were an estimated 127,558,000 hypertension-related hospitalizations. The number of such hospitalizations in 1979 (2,185,000) was only one-fifth of the number in 2006 (11,095,000). Of the total hospitalizations, only 7% were for patients with a primary diagnosis of hypertension, while 93% were for hospitalizations with a secondary diagnosis of that problem. Versus admissions in which hypertension was a secondary diagnosis, admissions with hypertension as a primary diagnosis had, on average, younger patients (62.7 vs 67.8 years), lower CCI (0.91 vs 1.23), a shorter hospital stay (5.3 vs 6.2 days) and lower in-hospital mortality (1.5% vs 2.4%).
Age-standardized hospitalization rates were much higher for hypertension as a secondary diagnosis than for hypertension as the first diagnosis, and the rates for hypertension as the secondary diagnosis increased substantially over the time period (Figure 1). Age-standardized hospitalization rates for hypertension increased for both men and women over time, with women having slightly higher rates than men (Figure 2). Hypertension-related hospitalization rates were highest in the oldest age group (≥ 75 years) and increased faster than in the two other age groups (25–64, 65–74, Figure 3).
Figure 1.
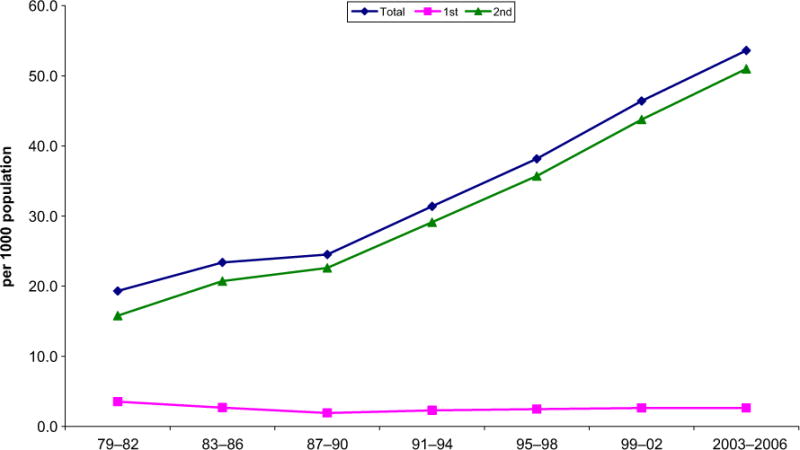
Age-standardized hypertension hospitalization, total and by first and second diagnosis.
Figure 2.
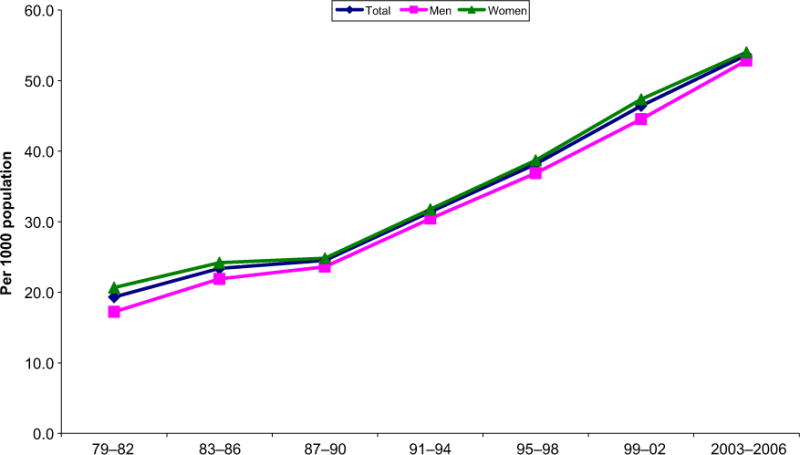
Age-standardized hospitalization rates for hypertension by sex.
Figure 3.
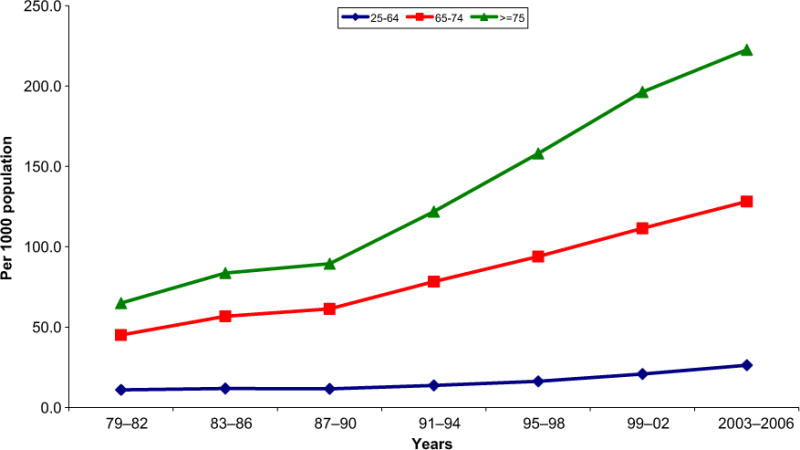
Age-standardized hypertension-related hospitalization by age, 1979 – 2006.
The mean age of patients (in years) increased from 64.5 in 1979–1982 to 67.8 in 2003–2006 (Table I), while the media length of stay decreased from 7 to 3 days during this period. The CCI increased from 1.01 to 1.30, but the rate of in-hospital death dropped from 3.3% to 1.9%. Among hospitalizations with hypertension as the secondary diagnosis, the percentage with a first diagnosis of diabetes or stroke decreased. In contrast, the percentage with a first diagnosis of HF, kidney disease or “all other conditions” increased. The percentage of patients transferred to long-term care facilities rose sharply over time, from 2.8% to 12.5%.
Table I.
Characteristics of patients hospitalized with a primary or secondary diagnosis of hypertension, National Hospital Discharge Survey, 1979–2006.
| 1979–1982 | 1991–1994 | 2003–2006 | RPC | |
|---|---|---|---|---|
| Age (mean ± SD) | 64.5 ± 14.1 | 67.3 ± 14.2 | 67.8± 15.0 | + 5.1 |
| Insurance (%) | ||||
| Private | 61.7 | 48.7 | 44.4 | − 28.0 |
| Public | 37.7 | 46.5 | 49.8 | + 32.1 |
| No | 0.6 | 4.8 | 5.8 | + 866.7 |
| Median length of stay (day) | 7 | 5 | 3 | − 57.1 |
| First-listed diagnosis (%) | ||||
| Hypertension | 18.2 | 7.2 | 4.9 | − 73.1 |
| Coronary heart disease | 10.5 | 14.7 | 10.1 | − 3.8 |
| Stroke | 7 | 7.5 | 5.3 | − 24.3 |
| Heart failure | 2.1 | 4.8 | 5.1 | + 142.9 |
| Other CVD | 7.5 | 8 | 8.5 | + 13.3 |
| Kidney disease | 3.1 | 2.7 | 4.1 | + 32.3 |
| Diabetes | 5.3 | 2.8 | 2.5 | − 52.8 |
| All others | 46.2 | 52.3 | 59.4 | + 28.6 |
| CCI (mean ± SD) | 1.01 ± 1.37 | 1.19 ± 1.55 | 1.30 ± 1.53 | + 28.7 |
| Discharge status (%) | ||||
| Home | 85.7 | 78.5 | 72.7 | − 15.16 |
| Other short-term facilities | 3.6 | 4.6 | 5.9 | + 63.9 |
| Long-term facilities | 2.8 | 8.3 | 12.5 | + 346.4 |
| Against medical advice | 0.5 | 0.7 | 0.8 | + 60.0 |
| Death | 3.3 | 2.7 | 1.9 | − 42.4 |
| Unknown | 4 | 5.3 | 6.3 | + 57.5 |
RPC, relative percentage change (calculated from changes from 1979–1982 to 2003–2006 and divided by 1979–1982); CVD, cardiovascular disease; CCI, Charlson Comorbidity Index.
Overall, during 1979–2006, 2.4% of the patients with a hypertension-related hospitalization died in the hospital. The likelihood of death was higher among the elderly, men, those admitted with public insurance or no insurance, and those with a higher CCI. The OR for death dropped from 1.00 (reference) for 1979–1982 to 0.45 for 2003–2006; in most cases, the OR for a 4-year period was significantly lower than the immediately preceding OR (Table II). Versus patients hospitalized with hypertension as the first diagnosis, patients with stroke as their first diagnosis and hypertension as a secondary diagnosis had more than three times the risk of death. In addition, those with a first diagnosis of CHD, HF, other CVD or kidney disease who had hypertension as a secondary diagnosis had a higher risk of death than those with hypertension as their first diagnosis, while patients with diabetes as the first diagnosis and hypertension as a secondary diagnosis had a lower risk of death than those with a primary diagnosis of hypertension.
Table II.
Odds ratio of in-hospital death among patients hospitalized with hypertension, National Hospital Discharge Survey, 1979–2006.
| Odds ratio | 95% Confidence interval | p | |
|---|---|---|---|
| Age (years) | |||
| 25–64 | 1.00 | ||
| 65–74 | 1.66 | 1.65–1.67 | < 0.0001 |
| ≥75 | 3.67 | 3.66–3.68 | < 0.0001 |
| Sex | |||
| Male | 1.00 | ||
| Female | 0.83 | 0.82–0.84 | < 0.0001 |
| Insurance | |||
| Private | 1.00 | ||
| Public | 1.26 | 1.25–1.27 | < 0.0001 |
| None | 1.23 | 1.22–1.23 | < 0.0001 |
| Period in which hospitalized | |||
| 1979–1982 | 1.00 | ||
| 1983–1986 | 0.75 | 0.75–0.76 | < 0.0001 |
| 1987–1990 | 0.75 | 0.74–0.75 | < 0.0001 |
| 1991–1994 | 0.67 | 0.66–0.67 | < 0.0001 |
| 1995–1998 | 0.60 | 0.59–0.60 | < 0.0001 |
| 1999–2002 | 0.53 | 0.52–0.53 | < 0.0001 |
| 2003–2006 | 0.45 | 0.44–0.45 | < 0.0001 |
| Charlson Comorbidity Index | 1.28 | 1.27–1.28 | < 0.0001 |
| First diagnosisa | |||
| Hypertension | 1.00 | ||
| Coronary heart disease | 1.67 | 1.66–1.68 | < 0.0001 |
| Stroke | 3.23 | 3.21–3.25 | < 0.0001 |
| Heart failure | 1.46 | 1.45–1.47 | < 0.0001 |
| Other CVD | 1.41 | 1.40–1.42 | < 0.0001 |
| Kidney disease | 1.33 | 1.32–1.34 | < 0.0001 |
| Diabetes | 0.87 | 0.86–0.88 | < 0.0001 |
Odds ratio for each co-morbidity condition expressed as yes vs no. CVD, cardiovascular disease.
Based on the number of hospitalizations and the average cost per stay, the annual hospital cost of patients with any diagnosis of hypertension was estimated to be US$5.21 billion for the 4-year period 1979–1982, but this figure rose more than 1600% to US$88.74 billion for 2003–2006 (Table III). In both periods, the main component of the cost was the cost of hospitalizations with hypertension as a secondary diagnosis, which was US$4.26 billion/year (82% of the costs for hospitalizations with any diagnosis of hypertension) in 1979–1982 and US$84.38 billion/year (95% of the total) in 2003–2006. After adjusting for inflation, we found that in 2008 constant dollars the annual hypertension-related hospitalization cost increased from US$40.22 billion in 1979–1982 to US$113.39 billion in 2003–2006, a rise of 182%.
Table III.
Costs of hospitalizations with a hypertension diagnosis during 1979–1982 and 2003–2006, National Hospital Discharge Survey.
| 1979–1982
|
2003–2006
|
|||||
|---|---|---|---|---|---|---|
| 1st diagnosis | 2nd diagnosis | Total | 1st diagnosis | 2nd diagnosis | Total | |
| Number of such hospitalizations (million) | 1.86 | 8.35 | 10.21 | 2.05 | 39.81 | 41.86 |
| 4-year hospital costa (US$ billion) | 3.80 | 17.05 | 20.85 | 17.42 | 337.54 | 354.95 |
| Annual hospital cost (US$ billion) | 0.95 | 4.26 | 5.21 | 4.35 | 84.38 | 88.74 |
| Value of annual hospital cost in 2008 dollarsb (US$ billion) | 7.33 | 32.89 | 40.22 | 5.56 | 107.83 | 113.39 |
Based on the average cost per stay of US$2041 during 1979–1982 (US Census Bureau, Statistical Abstract of the United States, 1990), and US$8480 during 2003–2006 (US Census Bureau, Statistical Abstract of the United States, 2008).
Using the consumer price indices of medical care prices (hospital and related services) to inflate to year 2008 dollars: 1980–2008. US Census Bureau, Statistical Abstract of the United States, 2010.
Discussion
We found a large increase from 1979–2006 in hypertension-related hospitalizations among US adults, a rise that was driven in substantial measure by a great increase in hospitalizations with hypertension as a secondary diagnosis. As would be expected based on trends in hospitalization during the period, length of stay decreased substantially, as did in-hospital case-fatality rates. Regardless, the greatly increased number of hypertension-related hospitalizations led to much higher costs for hypertension-related hospitalization.
The trends we found in this study could be related in part to the better identification and treatment of hypertension in the ambulatory setting (e.g. outpatient clinics and physician offices). Hypertension is one of the ambulatory care-sensitive conditions defined by the Agency for Healthcare Research and Quality (21); these conditions include diseases such as hypertension, diabetes or HF for which hospitalization can be prevented by effective outpatient care and early interventions. The increased hospitalization rates we saw for hypertension as a secondary diagnosis no doubt reflected a situation in which many patients with hypertension had their blood pressure controlled, but were hospitalized due to other conditions, including CHD or stroke, while still having hypertension as a secondary diagnosis. Buttressing this conclusion is a recent report revealing that hypertension control improved from 27.3% in 1988–1994 to 50.1% in 2007–2008 (16,30,31).
In 2010, Wang and coworkers reported that the increasing rates of hospitalization with hypertension as a secondary diagnosis in the US were driving up the total cost for hypertension-related hospitalization (15). With the aging of the US population and the treatment available to improve survival for patients following acute myocardial infarction and stroke (32,33), it is likely that many more people will be living with hypertension in the future. Correspondingly, there seems little doubt that hospitalizations in which hypertension is a secondary diagnosis will continue to increase.
The decline in in-hospital mortality observed in the present study is consistent with the overall decline seen over time in age-adjusted mortality from total CVD and cerebrovascular disease (34,35). Yet, a report from Ayala and colleagues (36) revealed an increase in the US hypertension-related death rate from 1980 to 1998. In that period, however, both patient age and CCI were increasing, both of them indicators of greater risk of mortality. Although results of current study indicated that in-hospital mortality for patient with hypertension declined over a period of about two and a half decades, we were unable to measure the overall outcomes for such patients. No doubt some hypertension patients who were alive at discharge died in another setting, including their home, a nursing facility or a chronic rehabilitation center. Indeed, our data revealed that among those with a hypertension hospitalization, the percentage discharged to a long-term care facility increased dramatically over the study period. Unfortunately, the NHDS provided no information on post-discharge mortality.
Although many studies have investigated the economic burden of hypertension (15–19), ours is the first to analyze the trends in economic burden over time based on detailed information about hospitalization. Furthermore, a unique feature of our study was that we estimated costs by the primary and secondary diagnosis, separately. Thus the results shed more light on the drivers of cost in a given time period and on trends over time. Such information should be valuable for developing and evaluating interventions designed to limit the impact of hypertension.
We estimated the annual cost of hospitalizations with a diagnosis of hypertension during 1979–1982 to be US$5.21 billion, 5.1% of total annual hospital costs of US$102.7 billion during that period (22). Annual costs of hypertension hospitalizations increased dramatically to US$88.74 billion during 2003–2006, or 15.1% of total annual hospital costs of US$587.75 billion (23). This large increase in the percentage of total hospital costs, combined with the decreasing in-hospital death rate and increasing rate of transferring patients to long-term care facilities, suggests that the economic burden of hypertension has become enormous in recent years. Even after adjusting for inflation, we found that the annual costs of hospitalizations with hypertension nearly tripled, increasing from US$40.2 billion in 1979–1982 to US$113.4 billion in 2003–2006. The fact that in 2003–2006, 95.1% of the annual cost was for hospitalizations in which the hypertension diagnosis was a secondary rather than primary underscore the great need to reduce the complications and co-morbidities of hypertension.
The NHDS, with its large population, national sample of hospital admissions, and standardized methodology for obtaining data from hospital records, allowed us to thoroughly examine long-term trends in hospitalizations and the associated costs (37). Furthermore, because hypertension is a major independent risk factor for other costly diseases, including heart attack and stroke, and is often listed as a secondary diagnosis, with this data we were able to examine the hospitalization trend by diagnosis status and other major diseases associated with hypertension.
The numerous strengths of our study notwithstanding, it had several limitations. First, the NHDS database provided only limited clinical information to assess the severity of disease, and it provided no information by which to determine the long-term outcome. Second, our results showing a reduction in the in-hospital death-rate and an increasing proportion of patients transferred to long-term care facilities over the years suggest that the cost of outpatient care would increase greatly, but we could not capture the costs incurred in settings out of hospitals. Third, the data were at the discharge level rather than at the patient level. Because a person might have multiple admissions or discharges during a year or a 4-year period (the period we used for the analysis), the hospitalization rates cannot be used to assess disease prevalence. Fourth, the costs estimates cannot be interpreted as the actual costs for hypertension treatment. Especially for hospitalizations in which hypertension was listed as a secondary diagnosis, the costs could be expected to be primarily for treating the disease listed as a primary diagnosis.
Fifth, we used the average cost per hospital stay as the hospital cost for hypertension-associated hospitalizations. This might be a concern if medical technologies developed much faster or slower in CVD treatment than in other disease areas, but this issue was outside of the scope of this study, and we are unaware of any supporting evidence on this matter. Thus, we believe that using the average cost per hospital stay for the trend analysis was acceptable. Further studies on the costs actually attributable to hypertension over the years are needed to provide insights on the impact of hypertension on the costs. Finally, for the great majority of hypertension-associated hospitalizations in our study, hypertension was a secondary diagnosis. It is possible that there was a higher percentage of misdiagnosis or missing codes in these hospitalizations. In any event, we were unable to investigate this issue using the NHDS database, and we consider it to be outside of the scope of this study. Regardless, the fact that a very high percentage of the hospitalizations had hypertension as a secondary diagnosis likely made our estimates of both hospitalization rates and costs to some degree conservative.
Conclusions
During the past 28 years, the number of US hospitalizations that involved hypertension increased dramatically, and the associated hospital costs increased, particularly among patients with hypertension as a secondary diagnosis. With the aging of the US population, an increasing prevalence of hypertension, and improvement of control for this disorder, it is expected that hospitalizations with hypertension as a secondary diagnosis will continue to increase in the future. Clearly, this will result in a great increase in hypertension-related hospital costs. Accordingly, there is a pressing need to develop effective interventions for preventing hypertension and its sequelae. The detailed information presented in the current report about hypertension-associated hospitalizations, the characteristics of these hospitalizations, and the associated costs should facilitate the development of useful interventions.
Footnotes
Disclosure: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention. The authors declared no conflict of interest.
References
- 1.Fields LE, Burt VL, Cutler JA, Hughes J, Roccella EJ, Sorlie P. The burden of adult hypertension in the United States 1999 to 2000: A rising tide. Hypertension. 2004;44:398–404. doi: 10.1161/01.HYP.0000142248.54761.56. [DOI] [PubMed] [Google Scholar]
- 2.Ostchega Y, Yoon SS, Hughes J, Louis T. Hypertension awareness, treatment, and control – continued disparities in adults : United States, 2005–2006. NCHS Data Brief. 2008:1–8. [PubMed] [Google Scholar]
- 3.Chobanian AV, Bakris GL, Black HR, et al. The Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 4.Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: Principal results of the Hypertension Optimal Treatment (HOT) randomised trial. Lancet. 1998;351:1755–1762. doi: 10.1016/s0140-6736(98)04311-6. [DOI] [PubMed] [Google Scholar]
- 5.Collins R, Peto R, MacMahon S, et al. Blood pressure, stroke, and coronary heart disease. Part 2, Short-term reductions in blood pressure: Overview of randomised drug trials in their epidemiologic context. Lancet. 1990;335:827–838. doi: 10.1016/0140-6736(90)90944-z. [DOI] [PubMed] [Google Scholar]
- 6.Psaty BM, Smith NL, Siscovick DS, et al. Health outcomes associated with antihypertensive therapies used as first-line agents. A systematic review and meta-analysis. JAMA. 1997;277:739–745. [PubMed] [Google Scholar]
- 7.Fang J, Keenan NL, Ayala C. Health care services provided during physician office visits for hypertension–differences by specialty. J Clin Hypertens. 2010;12:89–95. doi: 10.1111/j.1751-7176.2009.00219.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fang J, Alderman MH, Keenan NL, Ayala C, Croft JB. Hypertension control at physicians’ offices in the United States. Am J Hypertens. 2008;21:136–142. doi: 10.1038/ajh.2007.35. [DOI] [PubMed] [Google Scholar]
- 9.Baumann BM, Cienki JJ, Cline DM, Egging D, Lehrmann JF, Tanabe P. Evaluation, management, and referral of elderly emergency department patients with elevated blood pressure. Blood Press Monit. 2009;14:251–256. doi: 10.1097/MBP.0b013e328332fd40. [DOI] [PubMed] [Google Scholar]
- 10.Fang J, Alderman MH, Keenan NL, Ayala C. Acute myocardial infarction hospitalization in the United States, 1979 to 2005. Am J Med. 2010;123:259–266. doi: 10.1016/j.amjmed.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 11.Fang J, Mensah GA, Croft JB, Keenan NL. Heart failure-related hospitalization in the U.S., 1979 to 2004. J Am Coll Cardiol. 2008;52:428–434. doi: 10.1016/j.jacc.2008.03.061. [DOI] [PubMed] [Google Scholar]
- 12.Mohan S, Campbell NR. Hypertension management in Canada: Good news, but important challenges remain. CMAJ. 2008;178:1458–1460. doi: 10.1503/cmaj.080296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global burden of disease study. Lancet. 1997;349:1436–1442. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]
- 14.Wolf-Maier K, Cooper RS, Banegas JR, et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. JAMA. 2003;289:2363–2369. doi: 10.1001/jama.289.18.2363. [DOI] [PubMed] [Google Scholar]
- 15.Wang G, Zhang Z, Ayala C. Hospitalization costs associated with hypertension as a secondary diagnosis among insured patients aged 18–64 years. Am J Hypertens. 2010;23:275–281. doi: 10.1038/ajh.2009.241. [DOI] [PubMed] [Google Scholar]
- 16.Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162:2269–2276. doi: 10.1001/archinte.162.20.2269. [DOI] [PubMed] [Google Scholar]
- 17.Hodgson TA, Cai L. Medical care expenditures for hypertension, its complications, and its comorbidities. Med Care. 2001;39:599–615. doi: 10.1097/00005650-200106000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Balu S, Thomas J., 3rd Incremental expenditure of treating hypertension in the United States. Am J Hypertens. 2006;19:810–816. doi: 10.1016/j.amjhyper.2005.12.013. [DOI] [PubMed] [Google Scholar]
- 19.Trogdon JG, Finkelstein EA, Nwaise IA, Tanka FK, Orenstein D. The economic burden of chronic cardiovascular disease for major insurers. Health Promot Pract. 2007;8:234–242. doi: 10.1177/1524839907303794. [DOI] [PubMed] [Google Scholar]
- 20.Dennison C, Pokras R. Design and operation of the National Hospital Discharge Survey: 1988 redesign. Vital Health Stat. 2000;1:1–42. [PubMed] [Google Scholar]
- 21.Kozak LJ. Underreporting of Race in the National Hospital Discharge Survey. Adv Data 1995 (265), National Health Statistics. Vital Health Stat. 1996;16:1–12. [PubMed] [Google Scholar]
- 22.US Census Bureau. Statistical Abstract of the United States: 1990. 110th. Washington, DC: US Census Bureau; 1990. [Google Scholar]
- 23.US Census Bureau. Statistical Abstract of the United States: 2010. 130th. Washington, DC: US Census Bureau; 2010. [Google Scholar]
- 24.Saka O, McGuire A, Wolfe C. Cost of stroke in the United Kingdom. Age Aging. 2009;38:27–32. doi: 10.1093/ageing/afn281. [DOI] [PubMed] [Google Scholar]
- 25.Wang G, Dietz WH. Economic burden of obesity in youths aged 6 to 17 years: 1979–1999. Pediatrics. 2002;109:E81–1. doi: 10.1542/peds.109.5.e81. [DOI] [PubMed] [Google Scholar]
- 26.Linjer E, Jornmark J, Hedner T, Jonsson B, The Stop Hypertension-2 Group Predictors for high costs of hospital care in elderly hypertensive patients. Blood Press. 2006;15:245–250. doi: 10.1080/08037050600912237. [DOI] [PubMed] [Google Scholar]
- 27.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A New method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 28.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 29.D’Hoore W, Bouckaert A, Tilquin C. Practical considerations on the use of the Charlson Comorbidity Index with administrative data bases. J Clin Epidemiol. 1996;49:1429–1433. doi: 10.1016/s0895-4356(96)00271-5. [DOI] [PubMed] [Google Scholar]
- 30.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 31.Caminal J, Starfield B, Sanchez E, Casanova C, Morales M. The role of primary care in preventing ambulatory care sensitive conditions. Eur J Public Health. 2004;14:246–251. doi: 10.1093/eurpub/14.3.246. [DOI] [PubMed] [Google Scholar]
- 32.Tunstall-Pedoe H, Kuulasmaa K, Mähönen M, Tolonen H, Ruokokoski E, Amouyel P. Contribution of trends in survival and coronary-event rates to changes in coronary heart disease mortality: 10-year results from 37 WHO MONICA Project populations. Lancet. 1999;353:1547–1557. doi: 10.1016/s0140-6736(99)04021-0. [DOI] [PubMed] [Google Scholar]
- 33.Lloyd-Jones D, Adams RJ, Brown T, et al. Heart disease and stroke statistics – 2010 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2010;121:e1–e170. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 34.Levi F, Chatenoud L, Bertuccio P, Lucchini F, Negri E, La Vecchia C. Mortality from cardiovascular and cerebrovascular diseases in Europe and other areas of the world: An update. Eur J Cardiovasc Prev Rehabil. 2009;16:333–350. doi: 10.1097/HJR.0b013e328325d67d. [DOI] [PubMed] [Google Scholar]
- 35.Gerber Y, Jacobsen SJ, Frye RL, Weston SA, Killian JM, Roger VL. Secular trends in deaths from cardiovascular diseases: A 25-year community study. Circulation. 2006;113:2285–2292. doi: 10.1161/CIRCULATIONAHA.105.590463. [DOI] [PubMed] [Google Scholar]
- 36.Ayala C, Croft JB, Wattigney WA, Mensah GA. Trends in hypertension-related death in the United States: 1980–1998. J Clin Hypertens (Greenwich) 2004;6:675–681. doi: 10.1111/j.1524-6175.2004.03730.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kozak LJ, DeFrances CJ, Hall MJ. National Hospital Discharge Survey: 2004 annual summary with detailed diagnosis and procedure data. Vital Health Stat. 2006;13:1–209. [PubMed] [Google Scholar]


