Abstract
Background
To guide resource allocation, policy makers need evidence of the cost-effectiveness of interventions. We summarized such evidence on selected interventions to reduce sodium intake that would be intended as population-wide approaches to control hypertension.
Methods
We conducted a comprehensive literature review of journal articles published in English from January 2000 to May 2010 by searching the databases of PubMed, EMBASE, MEDLINE, and EconLit. We selected original research articles for abstracting the evidence on cost-effectiveness of interventions, cost savings and the costs of intervention implementation.
Results
From the 53 references obtained from the literature search, we identified 11 original research articles that provided relevant information on the medical cost savings, implementation costs, or cost-effectiveness of interventions to reduce sodium intake. The interventions were low in cost, e. g., one study showed that the cost ranged from US$ 0.03 to 0.32 per person per year for awareness campaign through mass media outlets and government regulations on food products in low and middle-income countries. Population-wide interventions for salt reduction are very cost-effective such as only ARS$ 151 per disability-adjusted life-year (DALY) saved in Argentina, whereas statin therapy to lower high cholesterol was $ 70 994 per DALY saved. Another study showed that sodium reduction could save US$ 18 billion in annual US healthcare costs by reducing sodium intake to 2300 mg/day.
Conclusion
The literature provided economic evidence that was in favor of population-wide interventions designed to reduce sodium intake. Reducing the intake of sodium through such initiatives might be one of the best buys in public health. However, the small body of literature and hypothetical scenarios in most studies might limit policy implications of the findings.
Keywords: cost-effectiveness, hypertension, salt consumption
Introduction
High blood pressure, the leading risk factor for mortality worldwide, contributes to a substantial number of premature deaths and acts to increase the incidence of a variety of cardiovascular and renal diseases, including stroke, coronary heart disease, heart failure, and kidney failure [1–4]. A high intake of sodium increases blood pressure and the risk of cardiovascular disease [5]. It has been shown that significant population-based reductions in sodium consumption could lower the blood pressure of enough people to yield a very large public health benefit in both developed and developing countries. Indeed, even a modest reduction in the population intake of sodium worldwide could produce a major improvement in public health [3,6]. Accordingly, population reductions in dietary sodium are recommended by a variety of major scientific and public health organizations [2,7–12]. In addition, some studies have shown the cost-effectiveness of interventions for sodium reduction. However, a comprehensive review of the evidence on cost-effectiveness has not been available. Such a review may facilitate the use of such evidence by policy makers in promoting activities to reduce sodium intake.
Because resources are limited, not all potentially beneficial interventions can be funded, that is, choices must be made in allocating scarce resources. Correspondingly, whether healthcare resources are used efficiently is an important factor for policy makers to consider in making such decisions. Specifically, which interventions are possibly effective and, more important, which interventions are economically justifiable, that is, their costs are lower than their benefits? But even if the costs are lower than the benefits, there is still a need to compare these costs and benefits with those of other programs to judge whether the investment in the interventions is the best use of the resources [13–16]. Economic evaluations can help inform decisions regarding the allocation of resources by comparing the costs and consequences of various interventions, and thus such evaluations can have considerable utility. For this study, we investigated which of the interventions designed to reduce sodium intake have been scientifically evaluated from an economic perspective, and we examined the evidence that these interventions are or are not cost-effective. To do this, we summarized the scientific evidence for the cost-effectiveness of interventions described in peer-reviewed articles published in the past decade. Our results will potentially assist policy makers in allocating scarce resources, and the findings should facilitate the process of implementing population-wide interventions to reduce sodium intake and control hypertension.
Methods
We searched the databases of PubMed, EMBASE, and EconLit using the key terms costs, cost-effectiveness, cost-benefit, cost-utility, and medical expenditures, and we combined the key terms sodium and salt with reduction, intake, and consumption. We limited the search to English-language publications from January 2000 to May 2010. In addition to searching the four databases, we performed some searches through Google Scholar and searched the bibliographies of the articles obtained from the electronic searches for further relevant articles. We included cost analyses in this review even though they are not cost-effectiveness analyses by strict definition, because the evidence about costs is a key element in evaluating cost-effectiveness, and policy makers and interventionists can benefit from such information if cost-effectiveness is not readily available.
We first reviewed the titles and abstracts of the collected literature to select potentially relevant studies, and then we carefully reviewed the abstracts and entire studies to decide on the final set of literature for synthesizing the evidence on cost-effectiveness. We required that either the costs of intervention or savings in medical costs be presented. We also required that the study be original research and contain a study design and its own data analysis, and thus editorials and letters, review articles, commentary, and publications reviewing research highlights were not included.
We analyzed the literature for developed (high income) and developing (low and middle income) countries separately. The low-income and middle-income economies were defined by the World Bank [17]. In addition to the differences between such countries in socioeconomic status, in most developed countries, dietary sodium mainly comes from the addition of salt to processed foods while they are being manufactured, whereas in developing countries most dietary salt comes from salt added during cooking or from sauce [6]. Such differences may indicate a need for different strategies or policy-making processes in efforts to reduce sodium intake.
Results
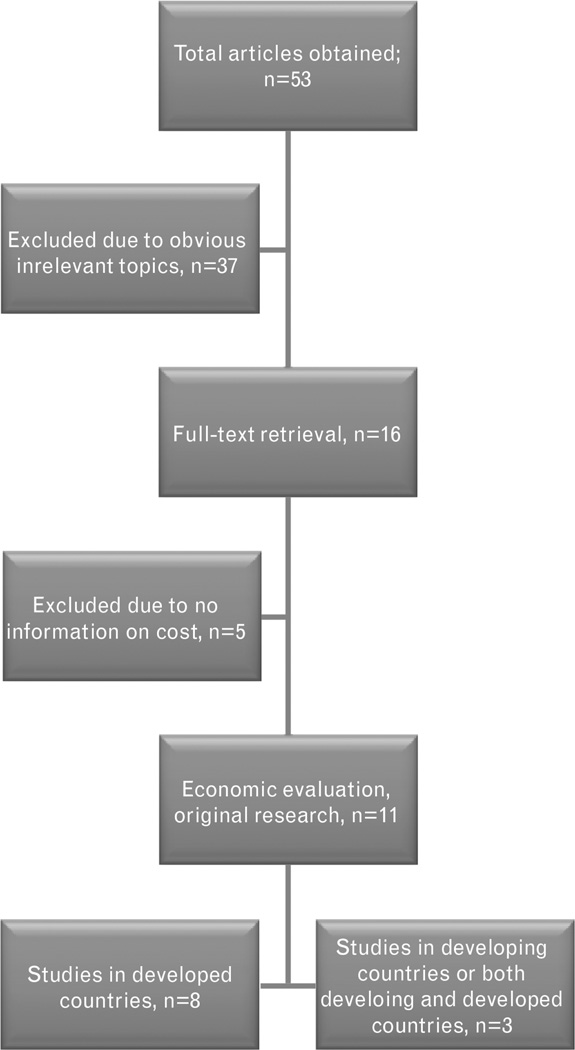
The literature search provided 53 references; after screening their titles and abstracts, we selected 16 for a critical review. From this group, we identified 11 original research articles that evaluated interventions from an economic perspective and provided relevant evidence on cost-effectiveness (Fig. 1). Of these 11 studies, eight evaluated interventions in developed countries, two in developing countries, and one in both kinds of countries (Table 1). Nine of the 11 studies were published in 2006 or later. In conducting the analysis, some studies only considered medical cost saving from sodium-reduction interventions, whereas others investigated the costs of intervention implementation.
Fig. 1.
Diagram for selecting the studies on the cost-effectiveness of interventions to reduce sodium intake.
Table 1.
Characteristics of cost-effectiveness studies on interventions to reduce sodium intake
| Type of countries | Study type | Perspective | |||||
|---|---|---|---|---|---|---|---|
| Time frame | Developed | Developing | Both | Advanced modeling |
Empirical investigation |
Savings in medical costs |
Costs of implementing the intervention |
| January 2000–December 2005 | 1 | 0 | 1 | 1 | 1 | 0 | 2 |
| January 2006–May 2010 | 7 | 2 | 0 | 5 | 4 | 6 | 3 |
| Total | 8 | 2 | 1 | 6 | 5 | 6 | 5 |
Developed countries
Smith-Spangler et al. [18] (US) assessed the cost-effectiveness of two different population strategies that were intended to reduce intake of sodium: collaboration of the government with food manufacturers to voluntarily reduce sodium in processed foods, and a tax on sodium (Table 2). For US adults aged 40–85 years, collaboration with industry that decreased mean intake of sodium by 9.5% was estimated to avert 513 885 strokes and 480 358 myocardial infarctions over their lifetimes and to save US$ 32.1 billion in annual medical costs. Over the same period, a tax on sodium that decreased the population’s intake of sodium by 6% was projected to save US$ 22.4 billion in such costs. The authors concluded that population-based strategies for salt reduction in the US would reduce substantially the incidence of both stroke and myocardial infarction, thereby saving billions of dollars in expenses for medical care. They also demonstrated that collaboration with industry to establish voluntary sodium targets in processed food would be more cost-effective than a tax on sodium and would be an appropriate first step toward reducing population intake of sodium and the burden of cardiovascular disease.
Table 2.
Cost-effectiveness of interventions in developed countries to reduce sodium intake
| 1st author, year/analysis type/country | Populations /interventions | Study design and methods | Main results |
|---|---|---|---|
| Smith-Spangler 2010/cost-effectiveness/US | Adults aged 40–85 years/population-based: government collaboration with food industry versus sodium tax | Markov model constructed with four health states: well, AMI, acute stroke, history of AMI or stroke | Government collaboration with food manufacturers is more effective than a tax on sodium, although both programs would improve health and save billions of dollars. |
| Bibbins-Domingo 2010/cost-effectiveness/US | US residents aged 35 years of age or older/population-based program | Markov modeling (computer simulation, state-transition model) | Reduction in salt intake of 3 g/day saves US$10 to $24 billion in annual medical costs. It would be more cost-effective than using drugs to control hypertension for everyone with that disorder. |
| Palar 2009/medical cost savings, QALYs gained/US | Noninstitutionalized US adults aged 18 and older/population-based program | Cross-sectional simulation/health outcomes: cases of hypertension and QALYs | Reducing sodium intake to 2300 mg/day may result in 11 million fewer cases of hypertension, reduce medical costs by US$18 billion, and gain 312 000 QALYs (valued at US$32 billion) annually. |
| Dall 2009/savings in medical costs/US | 225 million adults aged 18 and older/population-based program | Simulation model/hypothetical dietary change | Reduction in sodium intake of 400 mg/day in hypertensive persons would result in 1.5 million fewer cases annually, saving US$2.3 billion. |
| Dall 2009/national productivity gain/US | 225 million adults aged 18 and older/population-based program | Simulation model/hypothetical dietary change | Reductions in sodium intake of 400 mg/day in hypertensive persons would increase annual productivity by US$ 2.5 billion. |
| Joffres 2007/medical costs savings/Canada | 23 129 individuals from the Canadian Heart Health Surveys/population-based program | Obtaining information from various data sources. No specific cost-effectiveness methods used | Sodium reduction reduced prevalence of hypertension and saved substantial medical costs (US$430 million in direct costs; physician visits and laboratory costs decreased by 6.5%). |
| Kristiansen 2006/willingness to pay/Denmark | Random sample of Danish adults (n = 924) aged 20–74 years/population-based program | Contingent valuation through computer-assisted personal interviewing | The annual net program cost was US$148 million, less than the aggregate willingness to pay of US$ 468 million. The program is economically justifiable. |
| Selmer 2000/cost of interventions versus medical cost savings/Norway | Aged 40 and older/population-based program | Dynamic simulation model | The costs of the population interventions will be offset by cost savings from fewer strokes and heart attacks. |
AMI, acute myocardial infarction; CVD, cardiovascular disease; QALY, quality-adjusted life-year.
Bibbins-Domingo et al. [19] (US) employed Markov modeling applied to US residents aged 35 years or older to assess the impact of reducing dietary salt by 3 g per day on the annual number of new cases of coronary heart disease, stroke, and myocardial infarction and on reducing annual deaths from any cause. These researchers found that a regulatory intervention targeting a daily reduction of 3 g of salt would save, on an annual basis, 194 000 to 392 000 quality-adjusted life-years (QALYs) and US$ 10–24 billion in healthcare costs. Such an intervention would save costs even if the reduction was just 1 g per day, achieved on a gradual basis between 2010 and 2019, and it would be more cost-effective than a program of using drugs to lower blood pressure in the entire hypertensive population. The expected decreases in cardiovascular events from a reduction in dietary salt of 3 g per day would be either similar in magnitude or greater than those projected for interventions targeting tobacco or obesity, interventions involving primary prevention with statins, and the pharmacologic treatment of hypertension.
Palar and Sturm [20] (US) calculated the potential savings to society from reducing the rates of hypertension and related cardiovascular disease by lowering the population’s sodium intake; this study used a cross-sectional simulation approach to model various scenarios. The authors found that reducing average sodium intake to 2300 mg/day might eliminate 11 million cases of hypertension, save US$ 18 billion in healthcare costs, and gain 312 000 QALYs valued at US$ 32 billion on an annual basis. The authors concluded that society may gain large benefits from efforts to lower the consumption of salt over time.
In two studies, Dall et al. [21,22] (US) used a simulation model to predict the health benefits (saving in medical costs) or gains in productivity under hypothetical scenarios for dietary change among US adults that included reduced intake of sodium. The authors found that long-term reductions in sodium intake of 400 mg/day in those with uncontrolled hypertension would eliminate about 1.5 million hypertension cases, which per year would save US$ 2.3 billion and potentially increase productivity by US$ 2.5 billion.
Joffres et al. [23] (Canada) estimated the impact of dietary sodium reduction on the prevalence of hypertension and medical cost savings. The authors found that the sodium reduction of 1840 mg/day might decrease the prevalence of hypertension by 30%, which in Canada would mean a reduction of 1 million hypertensive patients, and it would almost double the rates of treatment and control for hypertensive persons. The authors estimated direct cost savings from fewer physician visits and laboratory tests and less use of drugs to be about US$ 430 million annually. They also estimated that the total costs of physician visits and laboratory services would decrease by 6.5% and predicted that among patients receiving treatment for hypertension, 23% fewer would need drugs to control their blood pressure.
Kristiansen et al. [24] (Demark) conducted a face-to-face interview survey in 2000 on a random sample (n = 924) of Danish people aged 20–74 years in which they asked participants how much they would be willing to pay as an additional tax for a population program that would cut the intake of salt in half. The aggregated willingness to pay was $ 468 million (in US dollars), more than three times the annual program cost (net) of $ 148 million. Although only 57% of the population was willing to pay, the authors found that such a program was warranted from an economic perspective.
Selmer et al. [25] (Norway) estimated the economic and health consequences (reduced risk of myocardial infarction and stroke because of lowered blood pressure) of interventions designed to reduce individual daily sodium intake in the Norwegian population by 6 g. Health promotion (informational campaigns), the development by industry of new recipes for foods, reporting the salt content of foods, and levying taxes on salty food/providing subsidies for products with less salt were the possible interventions. The net cost of the interventions (discounted at 5%) was minus US$ 118 million (i.e. they were cost saving). Thus, the costs of population interventions were lower than the cost savings from fewer strokes and heart attacks.
Developing countries
Rubinstein et al. [15] (Argentina) identified the most efficient of a variety of interventions, including reducing the amount of salt in bread, for decreasing cardiovascular disease (Table 3). The average cost-effectiveness ratio [measured in Argentine pesos (ARS $) per DALY saved for the interventions was as follows: reducing salt in bread, $ 151; a mass-media campaign, $ 547; combination pharmacotherapy for participants who had a 20, 10, and 5% global risk of cardiovascular disease, $ 3599, 4113, and 4533, respectively; therapy to lower blood pressure, $ 7716; tobacco cessation using the drug bupropion, $ 33 563; and statin therapy to lower high cholesterol, $ 70 994. Using the average per capita income in Argentina, the two population-based interventions that were chosen for analysis (reducing salt in bread and providing health education through mass-media campaigns) and the pharmacotherapy strategy targeting people with a 20% or greater risk of cardiovascular disease were cost-effective.
Table 3.
Cost-effectiveness of interventions in developing countries to reduce sodium intake
| 1st author, year/analysis type/country | Populations/interventions | Study design and methods | Main results |
|---|---|---|---|
| Rubinstein 2009/generalized cost-effectiveness analysis/Argentina | Over 3 million people in Buenos Aires, Argentina/population and individual-based salt programs | WHO-CHOICE methodology | The population-based reduction in the amount of salt in bread was most cost-effective (ARS$ 151 per DALY saved) among the analyzed interventions. |
| Asaria 2007/deaths averted versus cost of implementation/23 low-income or middle-income countries | General population in 23 low-income and middle-income countries (no specific population mentioned)/population-based program | WHO comparative risk assessment | The population-based salt reduction could be implemented without great cost (US$ 0.04 to 0.32 per person year) or structural change (in the health system) and could greatly reduce the death rate from chronic diseases. |
| Murray 2003/costs of selected interventions, health effects/southeast Asia, Latin America, and Europe | General population (no specifics provided)/population-based program | Methods taken from WHO-CHOICE project | Government action to stimulate a reduction in the amount of salt contained in processed foods is cost-effective for limiting cardiovascular disease. |
ARS $, Argentine pesos; DALY, disability-adjusted life-year, WHO, World Health Organization, WHO-CHOICE, World Health Organization-choosing interventions that are cost-effective.
Asaria et al. [26] (23 low-income to middle-income countries), who investigated how many deaths might be avoided over 10 years by implementing certain population-based interventions, calculated the costs of implementation using methods from the World Health Organization’s Comparative Risk Assessment project. In this analysis, salt intake would be reduced by 15% over 10 years in 23 countries in low and middle-income regions of the world. The main costs of the strategy would be an awareness campaign carried out through mass-media outlets and the regulation of food products by public health officers, with a total cost ranging from US$ 0.04 to 0.32 per person. This intervention could be implemented without great cost or structural change to the health system and could make a major contribution to reducing the death rate from chronic diseases.
Both developed and developing countries
Murray et al. [3] (Southeast Asia, Latin America, and Europe) estimated health effects at the population level and the costs of specific interventions to reduce the risks associated with high cholesterol and elevated blood pressure in areas of the world that had different epidemiological profiles (Table 3). Nonpersonal health interventions – among them action by government to stimulate a lowering of the salt content of processed foods – were found to be cost-effective in limiting cardiovascular disease and could avoid the loss of over 21 million DALYs annually around the world. The combination of personal and non-personal health interventions they evaluated could reduce the incidence of cardiovascular events worldwide by as much as 50%.
Discussion
We found that all 11 of the original research studies published in the past decade provided a significant amount of economic evidence in favor of interventions to reduce sodium intake. Notably, all of the interventions evaluated from an economic perspective were population-based initiatives. The results show that they were either low in cost, provided benefits higher than their costs, or were more cost-effective than other interventions. Among eight studies that dealt with developed countries, six were from the US and Canada, and two were from Europe (Denmark and Norway). Interestingly, all six US and Canadian studies evaluated salt reduction from the point of view of savings in medical costs (some took at least one additional perspective), but no options for implementation or strategies were investigated. In contrast, the two European studies evaluated the costs of implementation. Similarly, of the three studies that included one or more developing countries, two evaluated how much the implementation would cost. Thus, in the US and Canada, information on how to implement interventions and what resources might be required is lacking. Accordingly, future research on how to implement interventions might be important in achieving the goals of sodium reduction in these countries. In this regard we note that one author, Sugarman [11], proposed an innovative strategy in the US that is relevant to salt reduction. He proposed performance-based regulation to require food retailers (supermarkets and restaurants) to reduce the overall amount of salt contained in the foods they sold over time; in Sugarman’s proposal, this would be measured by grams of salt per dollar volume of sales.
Another characteristic of the 11 studies that we examined in detail was their relative recency, with nine published in 2006 or later, even though our time frame began in 2000. Furthermore, six of the 11 studies were based in the US or Canada. These findings may suggest that the high content of sodium in the diets of both Americans and Canadians has become better recognized as an important public health issue in recent years.
At present there is a clear need, especially in developing countries, for information on the cost and cost-effectiveness of initiatives to reduce sodium intake. For example, a study [10] of an intervention in China claimed that it was a low-cost strategy, but there was no information on cost in that study. Another study [12], in New Zealand, suggested that lowering the amount of salt in bread is a cost-effective way to reduce population-wide blood pressure, but again we could find no information on cost in the study. This lack of information on cost may limit the policy implications of these studies. Another concern about the literature we reviewed is that all the studies used adults or the general population as study participants; no studies assessed salt intake in children and adolescents. And yet, interventions targeting children and adolescents have high expected benefits that are generally attributed to ‘early’ prevention [27]. The literature has suggested that a moderate reduction in salt intake in children causes immediate falls in blood pressure and, if continued, may well less the subsequent rise in blood pressure with age [28].
Limitations
In addition to the strengths and weaknesses of the literature summarized in Table 4 and the information we obtained from the 11 studies notwithstanding, some limitations should be considered in interpreting our findings from the literature. First, ‘publication bias’ may have been present; we could review only what has been published. Studies that report favorable results are more likely to get published, and thus there is a tendency to overestimate the efficiency and effectiveness of the interventions in question. Additionally, we searched only four literature databases, and those only from 2000 to May 2010. Thus, we may have missed important evidence (from the grey literature, for example). Second, we did not explore healthcare systems across countries in our study, which was organized by high and low-income countries. This approach may have limited the use of our results for the establishment of health policy and for deciding how to allocate resources, as it may be hard to generalize the health economic data across countries. Finally, we did not formally address the issue of the analytic approaches chosen in terms of their potential value to readers. For example, studies from the US and Canada evaluated the impact of sodium reduction from the perspective of savings in medical costs, but the issues of which intervention strategies were feasible and the associated costs of implementation were not investigated. Additionally, all six US and Canadian studies used simulation models under hypothetical scenarios rather than data on the actual intervention to evaluate the approaches to sodium reduction. Thus, the policy implications of the study findings might be limited.
Table 4.
Strengths and weaknesses of the literature
| Countries | Strengths | Weakness |
|---|---|---|
| United States and Canada (six studies) | Employed advanced mathematical modeling. | Lack of specific intervention strategies. |
| Used high-quality data on health and medical costs. | Lack of costs for implementing interventions. | |
| Rest of the world (five studies) | Evaluated specific interventions. | Lack of data on health and medical costs. |
| Analyzed costs of implementation. | ||
| Overall (11 studies) | All studies evaluated population-wide interventions. | Not a complete cost-effectiveness analysis. |
| All focused on general population. |
Implications for policy
The economic evidence we obtained in this study clearly favors the use of population-wide interventions to reduce sodium intake around the world. Policy makers could use such information in setting their priorities for choosing or funding interventions. The next question is how to inform policy makers about the available evidence. In this regard, we see a need for research to explore the extent to which the available economic evidence informs policy making. In addition, further studies of the cost-effectiveness of various strategies to achieve sodium reduction, and an understanding of what is involved in implementing these strategies, are needed to scale up the population-wide interventions.
Acknowledgements
We wish to thank Dr Molly Cogswell, Dr Diane Dunet, and two anonymous referees for their constructive comments.
Abbreviations
- AMI
acute myocardial infarction
- ARS
Argentine pesos
- CVD
cardiovascular disease
- QALY
quality-adjusted life-year
- WHO
World Health Organization
- WHO-CHOICE
World Health Organization-choosing interventions that are cost effective
Footnotes
Partial results of this manuscript were presented at the World Health Organization (WHO) and Food Standards Agency (FSA) of UK Jointly Convened Technical Meeting on Creating an Enabling Environment for Population-based Salt Reduction Strategies, 1–2 July 2010, London, UK; and at the 2011 Annual Scientific Meeting and Exposition of the American Society of Hypertension Inc., 21–24 May 2011, New York.
Conflicts of interest
There is no potential conflict of interest related to any part of this manuscript.
The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention (CDC).
References
- 1.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 2.Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM. Dietary approaches to prevent and treat hypertension: a scientific statement From the American Heart Association. Hypertension. 2006;47:296–308. doi: 10.1161/01.HYP.0000202568.01167.B6. [DOI] [PubMed] [Google Scholar]
- 3.Murray CJ, Lauer JA, Hutubessy RC, Niessen L, Tomijima N, Rodgers A, et al. Effectiveness and costs of interventions to lower systolic blood pressure and cholesterol: a global and regional analysis on reduction of cardiovascular-disease risk. Lancet. 2003;361:717–725. doi: 10.1016/S0140-6736(03)12655-4. [DOI] [PubMed] [Google Scholar]
- 4.Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet. 1997;349:1436–1442. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]
- 5.IOM (Institute of Medicine) Strategies to reduce sodium intake in the United States. Washington, DC: The National Academies Press; 2010. [Google Scholar]
- 6.He FJ, MacGregor GA. Effect of modest salt reduction on blood pressure: a meta-analysis of randomized trials. Implications for public health. J Hum Hypertens. 2002;16:761–770. doi: 10.1038/sj.jhh.1001459. [DOI] [PubMed] [Google Scholar]
- 7.Havas S, Dickinson BD, Wilson M. The urgent need to reduce sodium consumption. JAMA. 2007;298:1439–1441. doi: 10.1001/jama.298.12.1439. [DOI] [PubMed] [Google Scholar]
- 8.Dickinson BD, Havas S. Reducing the population burden of cardiovascular disease by reducing sodium intake: a report of the Council on Science and Public Health. Arch Intern Med. 2007;167:1460–1468. doi: 10.1001/archinte.167.14.1460. [DOI] [PubMed] [Google Scholar]
- 9.He FJ, MacGregor GA. Reducing population salt intake worldwide: from evidence to implementation. Prog Cardiovasc Dis. 2010;52:363–382. doi: 10.1016/j.pcad.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 10.The China Salt Substitute Study Collaborative Group. Salt substitution: a low-cost strategy for blood pressure control among rural Chinese: a randomized, controlled trial. J Hypertens. 2007;25:2011–2108. doi: 10.1097/HJH.0b013e3282b9714b. [DOI] [PubMed] [Google Scholar]
- 11.Sugarman SD. Salt, high blood pressure, and performance-based regulation. Regul Govern. 2009;3:84–102. [Google Scholar]
- 12.Ni Mhurchu C, Young L, Lawes C, Brooks J, Pound C, Duizer L, Rodgers A. Less salt in bread: a cost-effective way to reduce New Zealand population blood pressure levels. N Z Med J. 2003;116:U487. [PubMed] [Google Scholar]
- 13.Dalziel K, Segal L, Mortimer D. Review of Australian health economic evaluation: 245 interventions: what can we say about cost effectiveness? Cost Eff Resour Alloc. 2008;6:9. doi: 10.1186/1478-7547-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwappach DL, Boluarte TA, Suhrcke M. The economics of primary prevention of cardiovascular disease: a systematic review of economic evaluations. Cost Eff Resour Alloc. 2007;5:5. doi: 10.1186/1478-7547-5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rubinstein A, Garcia Marti S, Souto A, Ferrante D, Augustovski F. Generalized cost-effectiveness analysis of a package of interventions to reduce cardiovascular disease in Buenos Aires, Argentina. Cost Eff Resour Alloc. 2009;7:10. doi: 10.1186/1478-7547-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McMurray J. The health economics of the treatment of hyperlipidemia and hypertension. Am J Hypertens. 1999;12:99S–104S. doi: 10.1016/s0895-7061(99)00161-2. [DOI] [PubMed] [Google Scholar]
- 17.World Bank. 2009 list of developing countries. [Accessed 10 April 2011];2008 Jul; http://web.worldbank.org/. Total of 144 countries. [Google Scholar]
- 18.Smith-Spangler CM, Juusola JL, Enns EA, Owens DK, Garber AM. Population strategies to decrease sodium intake and the burden of cardiovascular disease: a cost-effectiveness analysis. Ann Intern Med. 2010;152:481–487. W170–W173. doi: 10.7326/0003-4819-152-8-201004200-00212. [DOI] [PubMed] [Google Scholar]
- 19.Bibbins-Domingo K, Chertow GM, Coxson PG, Moran A, Lightwood JM, Pletcher MJ, Goldman L. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med. 2010;362:590–599. doi: 10.1056/NEJMoa0907355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Palar K, Sturm R. Potential societal savings from reduced sodium consumption in the U.S. adult population. Am J Health Promot. 2009;24:49–57. doi: 10.4278/ajhp.080826-QUAN-164. [DOI] [PubMed] [Google Scholar]
- 21.Dall TM, Fulgoni VL, 3rd, Zhang Y, Reimers KJ, Packard PT, Astwood JD. Potential health benefits and medical cost savings from calorie, sodium, and saturated fat reductions in the American diet. Am J Health Promot. 2009;23:412–422. doi: 10.4278/ajhp.080930-QUAN-226. [DOI] [PubMed] [Google Scholar]
- 22.Dall TM, Fulgoni VL, 3rd, Zhang Y, Reimers KJ, Packard PT, Astwood JD. Predicted national productivity implications of calorie and sodium reductions in the American diet. Am J Health Promot. 2009;23:423–430. doi: 10.4278/ajhp.081010-QUAN-227. [DOI] [PubMed] [Google Scholar]
- 23.Joffres MR, Campbell NR, Manns B, Tu K. Estimate of the benefits of a population-based reduction in dietary sodium additives on hypertension and its related healthcare costs in Canada. Can J Cardiol. 2007;23:437–443. doi: 10.1016/s0828-282x(07)70780-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kristiansen IS, Gyrd-Hansen D, Nexoe J, Bo Nielsen J. Willingness-to-pay for a population program aimed at reducing dietary salt in Denmark. Prev Med. 2006;43:31–35. doi: 10.1016/j.ypmed.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 25.Selmer RM, Kristiansen IS, Haglerod A, Graff-Iversen S, Larsen HK, Meyer HE, et al. Cost and health consequences of reducing the population intake of salt. J Epidemiol Commun Health. 2000;54:697–702. doi: 10.1136/jech.54.9.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Asaria P, Chisholm D, Mathers C, Ezzati M, Beaglehole R. Chronic disease prevention: health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet. 2007;370:2044–2053. doi: 10.1016/S0140-6736(07)61698-5. [DOI] [PubMed] [Google Scholar]
- 27.RAND Research Brief. Proven benefits of early childhood interventions. [Accessed 28 December 2010];2005 http://www.rand.org/pubs/research_briefs/RB9145/index1.html. [Google Scholar]
- 28.He FJ, MacGregor GA. Importance of salt in determining blood pressure in children: meta-analysis of controlled trials. Hypertension. 2006;48:861–869. doi: 10.1161/01.HYP.0000245672.27270.4a. [DOI] [PubMed] [Google Scholar]