Abstract
Background
Studies have identified correlates of intimate partner violence (IPV) during pregnancy at the individual and neighborhood levels, but have used inconsistent definitions of IPV. We aimed to compare correlates based on two IPV definitions: broad (physical, sexual, or psychological violence) and narrow (physical or sexual violence only).
Methods
Our analysis included 12,358 women in 2,110 census tracts (weighted to represent 269,671 women) who recently gave birth and responded to the Los Angeles Mommy and Baby (LAMB) survey. We linked 2007 and 2010 LAMB data to American Community Survey 2006-2010 census tract data, and conducted separate logistic multilevel analyses to identify correlates of IPV based on each definition.
Results
Prevalence of IPV during pregnancy was much higher by the broad (18.3%) than the narrow definition (3.9%). No independent neighborhood-level correlates were identified. Some individual-level correlates were associated with both IPV definitions, including substance abuse (OR 3.15, 95%CI 2.47-4.00 for broad definition; OR 3.60, 95%CI 2.30-5.64 for narrow definition) and medical problems (OR for ≥3 vs. 0 medical problems 2.03, 95%CI 1.61-2.55 for broad definition, OR 2.40, 95%CI 1.54-3.74 for narrow definition). Other correlates associated only with the broad definition, such as car accidents (OR 1.44, 95%CI 1.04-2.00) and moving during pregnancy (OR 1.35, 95%CI 1.12-1.62).
Conclusions
Differences in correlates of IPV during pregnancy for a broad vs. narrow IPV definition may illustrate the situations or mechanisms by which different types of IPV arise. Individual-level characteristics may outweigh neighborhood influences in a diverse population.
Keywords: Intimate partner violence, pregnancy, neighborhood risk factors, psychological violence, Los Angeles County
Introduction
Intimate partner violence (IPV) is a major public health problem in the United States, where 36% of women experience rape, physical violence, or stalking by an intimate partner during their lifetime.1 IPV toward pregnant women is particularly dangerous as it increases risk of adverse birth outcomes including low birth weight,2 preterm birth,3 and perinatal death among infants,4, 5 in addition to delayed prenatal care seeking6 and depression7, 8 among women.
The Centers for Disease Control and Prevention defines IPV broadly as “physical, sexual, or psychological harm by a current or former partner or spouse.”9 However, the public health literature has typically used a narrow definition excluding psychological violence,10 producing an inconsistency noted by some researchers.11 Arguably, the narrow definition is inconsistent with the World Health Organization definition of health as “a state of complete physical, mental, and social well-being.”12 Further, many pregnancy-related adverse effects of IPV likely occur through stress-related mediators, such as substance abuse and poor weight gain.5, 10, 13-15 These mediators may relate directly to the psychological form of IPV; thus, the narrow IPV definition is particularly limiting in the context of pregnancy.
Several studies have identified individual-level social, structural, and behavioral factors associated with risk of narrowly-defined IPV (i.e., physical or sexual IPV) during pregnancy. Sociodemographic correlates include young age, low income, single marital status or non-cohabitation, and lower levels of education.4, 16 Social/behavioral correlates include proxies for low partner involvement, low mastery (i.e., the perception of oneself as an effective person), anxiety, depression, and substance use.4, 17-20 Stressful life events may increase IPV risk, and medical problems such as preeclampsia are associated with IPV during pregnancy.3, 21, 22
Neighborhood-level correlates of IPV during pregnancy have also been identified using multilevel analysis. These correlates include low per capita income, high unemployment, and high residential stability.18, 23 However, because these studies used clinic-based recruitment, homogenous study populations, and the narrow IPV definition their results may not be generalizable or broadly applicable to the general population of women.
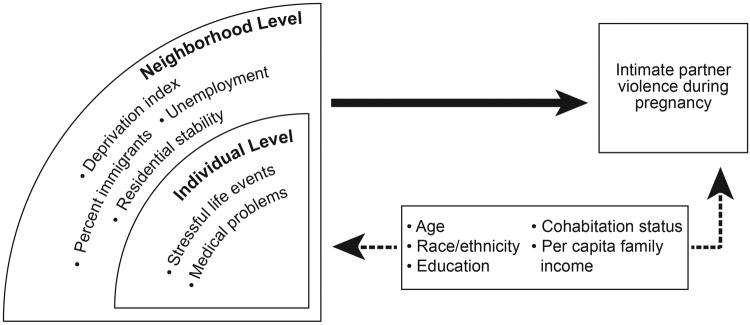
In this study, we aimed to assess whether correlates of IPV differ based on a broad vs. narrow IPV definition, and to identify whether neighborhood-level influences on IPV exist after detailed control for individual-level characteristics. Figure 1 shows the conceptual framework motivating our study, including neighborhood- and individual-level characteristics of interest (a deprivation index,24 unemployment, percent immigrants, and residential stability at the neighborhood level, and stressful life events and medical problems at the individual level). We further considered the established correlates and confounders listed in Figure 1.
Figure 1. Conceptual framework explaining individual and neighborhood influences on intimate partner violence during pregnancy.
Methods
The Los Angeles Mommy and Baby Project
The Los Angeles Mommy and Baby Project (LAMB, www.lalamb.org)has been described elsewhere.25 Briefly, LAMB is a population-based survey conducted approximately every two years by the Los Angeles County Department of Public Health. In each survey year, a stratified random sample of women who gave birth in the previous 2-6 months is drawn using birth records. Selected women are mailed a survey about events that may have occurred before, during, and after pregnancy. Using birth records, respondents are statistically weighted to represent all eligible women, with weights based on the woman's race/ethnicity, age, Service Planning Area (i.e., geographical area), and the infant's birth weight (low birth weight, yes/no).
For this analysis, we combined 2007 and 2010 LAMB data. Adjusted response rates were 56% and 57% respectively, based on calculations proposed by the American Association for Public Opinion Research (AAPOR) to adjust for faulty addresses, language issues, maternal deaths, and loss to follow-up due to inability to locate the respondent. Unadjusted response rates were 36% and 42%. Approximately 2% of respondents completed the survey by phone during intensive follow-up in geographic areas with historically low response rates.
Broad and Narrow Definitions of IPV
We constructed broadly and narrowly-defined IPV outcomes from individual outcomes of physical, sexual, and/or psychological violence perpetrated by an intimate partner of a woman during pregnancy, which were captured using a modified Abuse Assessment Screen.26 In the 2010 LAMB survey, women were asked, “During your last pregnancy, did the baby's father or your partner do any of the following?” followed by the sub-questions “a) hit or slapped me when he was angry; b) insulted or criticized me or my ideas; c) the baby's father threatened me or made me feel unsafe in some way; d) I was frightened for my safety or the safety of my family because of his anger or threats; e) he tried to control my daily activities, for example, telling me who I could talk to or where I could go; f) he forced me to take part in any sexual activity when I did not want to (including touch that made me feel uncomfortable).”
Physical abuse was defined using sub-question a), sexual abuse using sub-question f), and psychological abuse using sub-questions b)-e). In the 2007 survey, the phrase “or your partner” was not included in the base question, and the sub-questions were worded in second person. For broadly-defined IPV, we defined an affirmative answer to any of the six questions as “yes” and a negative answer to all six questions as “no.” We classified women who omitted a question and did not answer any others affirmatively as missing. We similarly constructed the narrow IPV outcome using sub-questions a) and f) only.
Individual-Level Covariates
Data describing age, race/ethnicity, and education of the woman were obtained from birth certificates. Marital/cohabitation status was asked on the LAMB survey. We classified women who responded “married” or “never married but living together” as cohabiting, and women who responded “separated or divorced,” “widowed,” or “never married and living apart” as not cohabiting. Total pre-tax family income in the year prior to the survey was asked in categories on the LAMB survey. An option for “I don't know” was available only on the 2010 survey, and we coded these responses as missing. We divided medians of income categories by the reported number of household members to give approximate per capita family income.
Occurrence of stressful life events during pregnancy was assessed by the LAMB survey and included hospitalization of family members, moving, homelessness, loss of employment, loss of employment by partner, financial difficulties, incarceration, substance abuse, death of a loved one, and car accidents. These events apply to the woman except where noted, and each was a binary variable (yes/no). The survey also assessed occurrence of 13 medical problems during pregnancy, including hypertension, gestational diabetes, premature labor, premature rupture of membranes, fetal growth restriction, incompetent cervix, placental problems (e.g. abruption placentae and placenta previa), bacterial vaginosis, sexually transmitted infection, influenza, severe nausea/vomiting/dehydration, teeth or gum problems, and bed rest. We considered that bed rest, while not a direct medical problem, might capture pregnancy complications not specified by the survey. For analysis, we created categories of 0, 1, 2, or ≥3 medical problems.
Neighborhood-Level Covariates
As a proxy for neighborhoods, we geocoded women to census tracts, which are designed by the U.S. Census Bureau to be relatively stable geographical units containing approximately 4,000 residents.27 We then linked LAMB data with five-year (2006-2010) estimates from the American Community Survey (ACS),27 an ongoing survey administered by the U.S. Census Bureau that provides data annually. Using ACS data, we examined 4 neighborhood-level variables. One was a modified neighborhood deprivation index24, which is a measure that combines correlated neighborhood-level variables. We used principal component analysis of 6 census tract variables recommended by Messer et al.:24 percentage in management occupations, in crowded housing (≥1 person per room), below the poverty line, in single-parent female-headed homes, receiving public assistance, and aged ≥25 with less than a high school education. Correlations of these variables with the final index, which was normalized to a z- score, ranged from 0.76 (public assistance) to 0.92 (education). The principal component accounted for 71.8% of the total variance.
We examined 3 additional neighborhood-level variables individually: unemployment, percent immigrants, and residential stability (percentage of homes with a householder of ≥5 years).27
Statistical Analysis
The combined 2007 and 2010 data contain 12,847 women (weighted N=284,716). Exclusion of 88 women who could not be geocoded, 1 living in a census tract with missing neighborhood-level information, and 410 missing the broadly-defined IPV yielded a sample of 12,358 (weighted N=269,671) for the broad definition analysis. Further exclusion of 21 women with missing data for narrowly-defined IPV gave a sample of 12,337 (weighted N=269,104) for the narrow definition analysis.
Missing data were treated by multiple imputation (N=5 imputations).28 Age, education, cohabitation status, approximate per capita family income, each stressful life event, and each medical problem were imputed individually. Medical problem categories were created after imputation.
We assessed crude relationships between IPV and covariates in the weighted sample using Wald chi-square and t statistics for individual and neighborhood variables, respectively. We next fit a series of weighted logistic multilevel models with random intercepts based on the systematic approach described by Singer.29 First, using the outcome of broadly-defined IPV, we estimated a model with no covariates to confirm that IPV varied by census tract (unconditional model). We added all individual-level covariates to this model and performed backward stepwise selection until all variables were statistically significant. Then, we added each neighborhood-level variable one at a time, maintaining variables with statistical significance. We repeated this process using the narrowly-defined IPV outcome.
We used a two-sided significance level of α=0.05 for all statistical tests. Analyses were conducted in SAS version 9.3 (SAS Institute Inc., Cary, NC), using the MI, GLIMMIX, and MIANALYZE procedures for multiple imputation, multilevel modeling, and synthesis of imputation-specific estimates, respectively. To estimate global p-values for categorical variables, we used the command metap in Stata version 12 (StataCorp, College Station, TX). Our study was approved by the California Committee for the Protection of Human Subjects and the Los Angeles County Public Health Institutional Review Board.
Results
Our weighted study population represented 2,110 census tracts and was majority Hispanic, with most women aged 25-34 (Table 1). Women who experienced broadly-defined IPV during pregnancy differed significantly from women who did not based on age, race, education, per capita family income, and cohabitation status, and were more likely to experience medical problems and stressful life events during pregnancy.
Table 1. Characteristics of the 2007 and 2010 Los Angeles Mommy and Baby Project, stratified by outcome of broadly-defined intimate partner violence during pregnancy.
| IPV Weighted N (%) | No IPV Weighted N (%) | p-value | Missing (N)a | |
|---|---|---|---|---|
|
| ||||
| Individual-Level Variables | ||||
|
| ||||
| Woman's age (years) | < 0.001 | 0 | ||
| <20 | 7,277 (14.8) | 17,365 (7.9) | ||
| 20-24 | 12,508 (25.4) | 43,263 (19.6) | ||
| 25-34 | 21,903 (44.5) | 115,322 (52.3) | ||
| >35 | 7,537 (15.3) | 44,496 (20.2) | ||
| Woman's race | < 0.001 | 0 | ||
| White | 6,760 (13.7) | 41,318 (18.7) | ||
| Hispanic | 32,035 (65.1) | 132,547 (60.1) | ||
| African-American | 5,328 (10.8) | 16,325 (7.4) | ||
| Asian/Pacific Islander | 4,320 (8.8) | 27,815 (12.6) | ||
| Other/unknown | 783 (1.6) | 2,441 (1.1) | ||
| Woman's education | < 0.001 | 363 | ||
| >12 years | 19,577 (40.7) | 105,958 (49.1) | ||
| =12 years | 12,981 (27.0) | 53,602 (24.8) | ||
| <12 years | 15,515 (32.3) | 56,146 (26.0) | ||
| Per capita family incomeb | ||||
| >$34,995 | 3,425 (8.3) | 35,047 (19.0) | < 0.001 | 2,040 |
| >$ 16,666-$34,995 | 5,056 (12.3) | 31,086 (16.9) | ||
| >$9,996-$ 16,666 | 8,636 (21.0) | 37,951 (20.6) | ||
| ≥$5,275-$9,996 | 9,712 (23.7) | 32,576 (17.7) | ||
| <$5,275 | 14,228 (34.7) | 47,343 (25.7) | ||
| Cohabitation status | < 0.0001 | 89 | ||
| Cohabiting | 34,231 (70.6) | 193,507 (88.4) | ||
| Not cohabiting | 14,282 (29.4) | 25,510 (11.6) | ||
| Medical problems | < 0.001 | 657 | ||
| 0 | 9,351 (21.6) | 70,722 (34.1) | ||
| 1 | 11,355 (26.3) | 57,064 (27.5) | ||
| 2 | 9,555 (22.1) | 39,748 (19.2) | ||
| ≥3 | 12,993 (30.0) | 39,767 (19.2) | ||
| Stressful life events | ||||
| Family hospitalized | 0.001 | 338 | ||
| Yes | 9,455 (20.1) | 34,556 (16.1) | ||
| No | 37,578 (79.9) | 179,879 (83.9) | ||
| Moving | < 0.001 | 249 | ||
| Yes | 15,709 (33.0) | 49,124 (22.7) | ||
| No | 31,866 (67.0) | 167,181 (77.3) | ||
| Homelessness | < 0.001 | 429 | ||
| Yes | 4,510 (9.7) | 8,200 (3.9) | ||
| No | 41,850 (90.3) | 204,252 (96.1) | ||
| Woman lost employment | < 0.001 | 384 | ||
| Yes | 9,039 (19.4) | 20,343 (9.5) | ||
| No | 37,600 (80.6) | 193,139 (90.5) | ||
| Partner lost employment | < 0.001 | 379 | ||
| Yes | 11,171 (23.8) | 29,802 (14.0) | ||
| No | 35,682 (76.2) | 183,587 (86.0) | ||
| Financial difficulties | < 0.001 | 340 | ||
| Yes | 19,637 (41.6) | 40,289 (18.8) | ||
| No | 27,565 (58.4) | 173,641 (81.2) | ||
| Incarceration | < 0.001 | 445 | ||
| Yes | 4,744 (10.2) | 5,131 (2.4) | ||
| No | 41,879 (89.8) | 207,206 (97.6) | ||
| Substance abuse | < 0.001 | 379 | ||
| Yes | 10,863 (23.2) | 14,432 (6.8) | ||
| No | 35,884 (76.8) | 199,175 (93.2) | ||
| Death of loved one | 0.002 | 343 | ||
| Yes | 7,427 (15.8) | 26,863 (12.5) | ||
| No | 39,683 (84.2) | 187,422 (87.5) | ||
| Car accident | < 0.001 | 401 | ||
| Yes | 3,852 (8.2) | 9,540 (4.5) | ||
| No | 43,037 (91.8) | 203,426 (95.5) | ||
|
| ||||
| Neighborhood-Level Variables | ||||
|
| ||||
| IPV Weighted mean | No IPV Weighted mean | p-value | Missing (N)a | |
|
| ||||
| Deprivation index | 0.24 | 0.18 | 0.033 | 0 |
| Percent immigrants | 36.82 | 35.93 | 0.024 | 0 |
| Unemployment | 9.59 | 9.29 | 0.016 | 0 |
| Residential stability | 67.27 | 67.01 | 0.419 | 0 |
IPV, intimate partner violence.
Broadly-defined IPV includes physical, sexual, and psychological abuse. N=12,358, weighted N=269,671.
Counts of missing observations are unweighted.
Estimated. See Methods: Individual-Level Covariates for details.
Based on the broad definition, prevalence of IPV during pregnancy was 18.3% (95%CI 17.4%-19.1%). In the unconditional model (i.e., no covariates), variance of the random intercept was 6.82 (p<0.001), indicating that broadly-defined IPV varied significantly by census tract. Individual-level variables were added then removed in the following order: death of a loved one, hospitalization of family member, race/ethnicity, loss of employment by partner. No neighborhood variables were statistically significant when combined with the resulting set of individual variables. Age of ≥20 years and cohabitation (OR 0.38, 95%CI 0.31-0.47)showed a protective association with IPV during pregnancy, while substance abuse showed the strongest adverse association (OR 3.15, 95%CI 2.47-4.00). Other correlates included approximately two-fold increases in odds of IPV for incarceration, financial difficulties, and ≥3 vs. 0 medical problems (all p<0.001), and more modest increases for moving, homelessness, loss of woman's employment, and car accidents (all p≤0.030). The broadly-defined IPV model contained an average of 5.9 women in each of 2,110 census tracts (range 1 to 37).
Based on the narrow definition, prevalence of IPV was much lower at 3.9% (95%CI 3.4%-4.3%). For this model, individual-level variables were removed in the following order: loss of partner's employment, death of a loved one, educational level, car accident, hospitalization of family member, moving, loss of woman's employment, age. No neighborhood variables were statistically significant when combined with the resulting set of individual-level variables, though residential stability was marginally significant (OR=1.15 for a 10% increase in residential stability, p=0.067, data not shown). The strongest adverse correlate for narrowly-defined IPV was also substance abuse (OR 3.60, 95%CI 2.30-5.64, Table 2), followed by low per capita family income (OR for lowest vs. highest quintile 3.52, 95%CI 1.07-11.59). Higher risk of narrowly-defined IPV was also associated with race/ethnicity outside of the 4 most common groups (global p=0.018), increasing number of medical problems, homelessness, financial difficulties, and incarceration (all p≤0.003). Cohabitation was associated with lower odds of narrowly-defined IPV (OR 0.43, 95%CI 0.28-0.64).
Table 2. Multilevel logistic regression models of intimate partner violence during pregnancy in the 2007 and 2010 Los Angeles Mommy and Baby Project.
| Broadly-defined IPVa | Narrowly-defined IPVb | |||
|---|---|---|---|---|
|
| ||||
| OR (95% CI) or coefficient (SE) | p-value | OR (95% CI) or coefficient (SE) | p-value | |
|
| ||||
| Fixed Effects | ||||
| Intercept (coefficient) | -2.64 (0.20) | < 0.001 | -7.29 (0.60) | < 0.001 |
| Woman's age (years) | < 0.001 | - | - | |
| <20 | REF | - | - | |
| 20-24 | 0.58 (0.43, 0.78) | - | - | |
| 25-34 | 0.54 (0.42, 0.71) | - | - | |
| >35 | 0.58 (0.42, 0.79) | - | - | - |
| Woman's race | - | - | - | 0.018 |
| White | - | - | REF | |
| Hispanic | - | - | 1.23 (0.67, 2.23) | |
| African-American | - | - | 1.65 (0.86, 3.14) | |
| Asian/Pacific Islander | - | - | 1.64 (0.86, 3.14) | |
| Other/unknown | - | - | 3.22 (1.10, 9.38) | - |
| Woman's education | - | 0.045 | - | - |
| >12 years | REF | - | - | |
| =12 years | 0.82 (0.65, 1.03) | - | - | |
| <12 years | 0.89 (0.69, 1.14) | - | - | |
| Per capita family incomec | < 0.001 | < 0.001 | ||
| >$34,995 | REF | REF | ||
| >$ 16,666-$34,995 | 1.44 (1.05, 1.97) | 1.88 (0.50, 7.15) | ||
| >$9,996-$ 16,666 | 1.39 (1.00, 1.93) | 2.49 (0.77, 8.07) | ||
| ≥$5,275-$9,996 | 1.75 (1.28, 2.40) | 2.55 (0.80, 8.12) | ||
| <$5,275 | 1.79 (1.27, 2.52) | 3.52 (1.07, 11.59) | ||
| Cohabiting | 0.38 (0.31, 0.47) | < 0.001 | 0.43 (0.28, 0.64) | < 0.001 |
| Medical problems | < 0.001 | < 0.001 | ||
| 0 | REF | REF | ||
| 1 | 1.35 (1.08, 1.69) | 1.53 (0.94, 2.51) | ||
| 2 | 1.59 (1.26, 2.00) | 1.76 (1.04, 2.98) | ||
| ≥3 | 2.03 (1.61, 2.55) | 2.40 (1.54, 3.74) | ||
| Stressful life events | ||||
| Moving | 1.35 (1.12, 1.62) | 0.002 | - | - |
| Homelessness | 1.50 (1.05, 2.15) | 0.027 | 2.85 (1.65, 4.93) | < 0.001 |
| Woman lost employment | 1.33 (1.03, 1.72) | 0.027 | - | - |
| Financial difficulties | 2.22 (1.82, 2.70) | < 0.001 | 2.56 (1.82, 3.60) | < 0.001 |
| Incarceration | 1.95 (1.36, 2.79) | < 0.001 | 2.25 (1.33, 3.82) | 0.003 |
| Substance abuse | 3.15 (2.47, 4.00) | < 0.001 | 3.60 (2.30, 5.64) | < 0.001 |
| Car accident | 1.44 (1.04, 2.00) | 0.030 | - | - |
|
| ||||
| Random Effects: Variance Components | ||||
|
| ||||
| Intercept (census tract) | 6.49 (0.25) | < 0.001 | 7.78 (0.34) | < 0.001 |
OR, odds ratio; IPV, intimate partner violence; CI, confidence interval; SE, standard error.
Broad definition of IPV including physical, sexual, and psychological abuse. N=12,358, weighted N=269,671.
Narrow definition of IPV including physical and sexual abuse only. N=12,337, weighted N=269,104.
Estimated. See Methods: Individual-Level Covariates for details.
Discussion
Prior studies that identified correlates of IPV during pregnancy have typically used a narrow definition of IPV including only physical or sexual violence (i.e., excluding psychological violence). This narrow definition may be limiting in the context of maternal health; thus, we compared individual- and neighborhood-level IPV correlates using a broad vs. narrow IPV definition. After detailed control for individual characteristics, we found no independent neighborhood-level correlates of IPV. Some individual-level correlates were consistent across definitions, including a protective effect of cohabitation and higher risk associated with substance abuse. However, others differed between the two definitions, which may illustrate on the situations or mechanisms by which different types of IPV arise.
In our analysis, sociodemographic factors were differentially associated with broadly and narrowly-defined IPV, though cohabitation was protective based on both definitions. Age <20 years was associated with higher risk of broadly-defined IPV only, perhaps indicating high risk of psychological abuse among teenage mothers. For the broad definition, income below the highest quintile showed a small increase in IPV risk, while risk increased in a strong linear manner across decreasing income quintiles for the narrow IPV definition. This pattern may imply that income increases are protective against physical/sexual IPV, while psychological IPV is prevalent across most income groups. We found few meaningful associations with race/ethnicity, perhaps indicating that race does not independently correlate with IPV after detailed adjustment for other factors (e.g., stressful life events). For the narrow definition, these findings are generally consistent with prior studies.4, 16-18
A summary index of medical problems was associated with IPV for both definitions. The association with the narrow definition was larger and has been shown in previous studies.3, 21, 22 This association may reflect direct harm inflicted by physical and sexual violence, as psychological violence is believed to cause medical problems largely through stress-related mediators.
Three stressful life events – moving, loss of the woman's employment, and car accidents – were correlates of broadly-defined IPV only, and may be associated specifically with psychological abuse. These associations may be explained by reactions to stress by the father, the mother, or both. Among men, stress may lead to feelings of hopelessness, powerlessness, shame, and humiliation, which may in turn lead to violence.30, 31 However, the woman's reaction to stress may also contribute to these associations. For example, if a woman loses her employment, she may become more sensitive to criticism from her partner and thus be more likely to perceive and report psychological abuse.
Some stressful life event correlates, including homelessness, substance abuse, and incarceration, were associated with both outcomes, but more strongly with narrowly-defined IPV. Homeless pregnant women may be more vulnerable to severe forms of abuse due to deprivation, isolation, and lack of respite, and this association could also reflect representation by women who become homeless after fleeing highly violent relationships.32 For substance abuse, studies have cited depression, posttraumatic stress disorder, lack of social support, and lack of mastery as consistent correlates of and contributors to substance use by abused pregnant women.19, 20, 33 For incarceration, our cross-sectional survey is not designed to identify the timing or sequence of incarceration and IPV. Therefore, one cannot know whether these associations reflect abuse during or outside the incarceration period.
Unlike other studies, which identified neighborhood influences on IPV during pregnancy including low per capita income, high unemployment,23 and high residential stability,18 our analysis found no significant neighborhood-level correlates. However, each of these studies was conducted among a homogenous population. If neighborhood environments affect different groups in distinct ways, then the overall effect may be blurred in a population diverse in terms of age, race/ethnicity, and income. Additionally, while we required that neighborhood variables be statistically significant in addition to individual-level variables, we might have found significant associations for neighborhood factors had we not adjusted for individual-level variables. Notably, neighborhood residential stability showed a marginally significant positive association with the narrow definition, corroborating previous findings.18
Strengths of our study include a large and diverse population-based sample, use of multiple imputation instead of model-wise deletion for missing data,34 and use of a mailed survey for IPV outcome ascertainment.35 Limitations include relatively low response rates, lack of longitudinal data, and no eligibility of/representation by women experiencing miscarriage or stillbirth. Additionally, we used weights to adjust for differential response rates across demographic groups. However, this method requires the assumption that respondents in a given group are representative of non-respondents in that group. Finally, census tracts were not designed to represent neighborhoods, which could contribute to the lack of independent neighborhood-level associations in our study.
With further study, our findings could facilitate identification and prevention of the various forms of IPV during pregnancy. For example, one might survey pregnant women about stressful life events and target IPV prevention efforts to women who experience them. Similarly, prenatal care providers might deepen the domestic violence discussion for women experiencing many medical problems. In diverse populations, these individual correlates may warrant focus over neighborhood environments. Future studies might investigate these associations using longitudinal data, or consider creating formal risk prediction models that could be applied in clinical or other settings to estimate the probability that a woman will experience IPV during a current or future pregnancy.
In conclusion, correlates of IPV during pregnancy may differ between broad vs. narrow definitions of IPV, and the broad definition should be more widely applied particularly during pregnancy. Pregnant women experiencing medical problems and certain stressful life events are more likely to also be experiencing IPV. With further characterization and replication, these correlates may strengthen efforts to recognize and prevent all forms of IPV toward pregnant women.
Acknowledgments
The authors gratefully acknowledge the respondents of the 2007 and 2010 Los Angeles Mommy and Baby (LAMB) survey. Funding for the LAMB study was provided by the County of Los Angeles Department of Public Health, Maternal, Child and Adolescent Health. We thank Sai Liu, Cinthiya Kasana, Diana Liu, Yeghishe Nazinyan, Carmen Gutierrez, Suvas Patel, Chandra Higgins, Marian Eldahaby, and Judith Zarate for their efforts in data collection and management for the LAMB project and their feedback on the design and interpretation of this analysis. We acknowledge Dr. Ricardo Basurto-Davila, Dr. Patricia O'Campo, and Dr. Jacky Jennings for their guidance in the early stages of data analysis and manuscript preparation, and we thank Daniel Helfer for his assistance with graphic design. Finally, we thank the de Beaumont Foundation for its support of the Epi Scholars Program, which partially supported H. Robbins in conducting this research.
Funding: No funding was sought or obtained to undertake this specific study. H.A. Robbins was supported during a portion of this study's duration by the Cancer Epidemiology, Prevention, and Control Training Grant (NCI T32 CA009314).
Footnotes
Disclosure of Interests: All authors declare no conflict of interest.
Contribution to Authorship: All authors contributed to the design of the study and interpretation of results. HR was responsible for the statistical analysis, and HR and EH were primarily responsible for drafting the article. LL and SC provided guidance and supervision at every stage, and SC also serves as the principal investigator of the Los Angeles Mommy and Baby Project.
Detail of Ethics Approval: This study received ethics approval from the California Committee for the Protection of Human Subjects (project number 12-08-0600, approval date 8/31/2012) and the Los Angeles County Public Health Institutional Review Board (proposal number 2012-08-397, approval date 8/30/2012).
References
- 1.Black MC, Basile KI, Breiding MJ, Smith SG, Walters ML, Merrick MT, et al. Center for Disease Control and Prevention. Atlanta, GA: National Center for Injury Prevention and Control, Division of Violence Prevention and Control; 2011. National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. [Google Scholar]
- 2.Murphy CC. Abuse: a risk factor for low birth weight? A systematic review and meta-analysis. CMAJ. 2001;164(11):1567. [PMC free article] [PubMed] [Google Scholar]
- 3.Silverman JG. Intimate partner violence victimization prior to and during pregnancy among women residing in 26 US states: associations with maternal and neonatal health. Am J Obstet Gynecol. 2006;195(1):140. doi: 10.1016/j.ajog.2005.12.052. [DOI] [PubMed] [Google Scholar]
- 4.Janssen PA. Intimate partner violence and adverse pregnancy outcomes: a population-based study. Am J Obstet Gynecol. 2003;188(5):1341. doi: 10.1067/mob.2003.274. [DOI] [PubMed] [Google Scholar]
- 5.Coker AL. Partner violence during pregnancy and risk of adverse pregnancy outcomes. Paediatr Perinat Epidemiol. 2004;18(4):260. doi: 10.1111/j.1365-3016.2004.00569.x. [DOI] [PubMed] [Google Scholar]
- 6.Curry MA, Perrin N, Wall E. Effects of abuse on maternal complications and birth weight in adult and adolescent women. Obstet Gynecol. 1998;92(4 Pt 1):530–4. doi: 10.1016/s0029-7844(98)00258-0. [DOI] [PubMed] [Google Scholar]
- 7.Tiwari A, Chan KL, Fong D, Leung WC, Brownridge DA, Lam H, et al. The impact of psychological abuse by an intimate partner on the mental health of pregnant women. BJOG. 2008;115(3):377–84. doi: 10.1111/j.1471-0528.2007.01593.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Urquia ML. Experiences of violence before and during pregnancy and adverse pregnancy outcomes: An analysis of the Canadian Maternity Experiences Survey. BMC Pregnancy Childbirth. 2011;11(1):42. doi: 10.1186/1471-2393-11-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Intimate Partner Violence. 2012 [Google Scholar]
- 10.Campbell JC. Health consequences of intimate partner violence. Lancet. 2002;359(9314):1331. doi: 10.1016/S0140-6736(02)08336-8. [DOI] [PubMed] [Google Scholar]
- 11.Ansara DL, Hindin MJ. Exploring gender differences in the patterns of intimate partner violence in Canada: a latent class approach. J Epidemiol Community Health. 2010;64(10):849–54. doi: 10.1136/jech.2009.095208. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. WHO Definition of Health. New York: International Health Conference; 1948. [Google Scholar]
- 13.O'Campo P. Racial inequalities in preterm delivery: Issues in the measurement of psychosocial constructs. Am J Obstet Gynecol. 2005;192(5):S56. doi: 10.1016/j.ajog.2005.01.074. [DOI] [PubMed] [Google Scholar]
- 14.Campbell J. Physical and Nonphysical Partner Abuse and Other Risk Factors for Low Birth Weight among Full Term and Preterm Babies A Multiethnic Case-Control Study. Am J Epidemiol. 1999;150(7):714. doi: 10.1093/oxfordjournals.aje.a010074. [DOI] [PubMed] [Google Scholar]
- 15.McFarlane J. Abuse during pregnancy: associations with maternal health and infant birth weight. Nurs Res. 1996;45(1):37. doi: 10.1097/00006199-199601000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Martin SL, Mackie L, Kupper LL, Buescher PA, Moracco KE. Physical abuse of women before, during, and after pregnancy. JAMA. 2001;285(12):1581–4. doi: 10.1001/jama.285.12.1581. [DOI] [PubMed] [Google Scholar]
- 17.Campbell JC, Poland ML, Waller JB, Ager J. Correlates of battering during pregnancy. Res Nurs Health. 1992;15(3):219–26. doi: 10.1002/nur.4770150308. [DOI] [PubMed] [Google Scholar]
- 18.Li Q, Kirby RS, Sigler RT, Hwang SS, Lagory ME, Goldenberg RL. A multilevel analysis of individual, household, and neighborhood correlates of intimate partner violence among low-income pregnant women in Jefferson county, Alabama. Am J Public Health. 2010;100(3):531–9. doi: 10.2105/AJPH.2008.151159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martin SL. Violence and substance use among North Carolina pregnant women. Am J Public Health. 1996;86(7):991–8. doi: 10.2105/ajph.86.7.991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amaro H. Violence during pregnancy and substance use. Am J Public Health. 1990;80(5):575–9. doi: 10.2105/ajph.80.5.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leone JM, Lane SD, Koumans EH, DeMott K, Wojtowycz MA, Jensen J, et al. Effects of intimate partner violence on pregnancy trauma and placental abruption. J Womens Health. 2010;19(8):1501–9. doi: 10.1089/jwh.2009.1716. [DOI] [PubMed] [Google Scholar]
- 22.Sanchez SE, Qiu C, Perales MT, Lam N, Garcia P, Williams MA. Intimate partner violence (IPV) and preeclampsia among Peruvian women. Eur J Obstet Gynecol Reprod Biol. 2008;137(1):50–5. doi: 10.1016/j.ejogrb.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 23.O'Campo P, Gielen AC, Faden RR, Xue X, Kass N, Wang MC. Violence by male partners against women during the childbearing year: a contextual analysis. Am J Public Health. 1995;85(8 Pt 1):1092–7. doi: 10.2105/ajph.85.8_pt_1.1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Messer LC, Laraia BA, Kaufman JS, Eyster J, Holzman C, Culhane J, et al. The development of a standardized neighborhood deprivation index. J Urban Health. 2006;83(6):1041–62. doi: 10.1007/s11524-006-9094-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chao SM, Donatoni G, Bemis C, Donovan K, Harding C, Davenport D, et al. Integrated approaches to improve birth outcomes: perinatal periods of risk, infant mortality review, and the Los Angeles Mommy and Baby Project. Matern Child Health J. 2010;14(6):827–37. doi: 10.1007/s10995-010-0627-2. [DOI] [PubMed] [Google Scholar]
- 26.McFarlane J, Parker B, Soeken K, Bullock L. Assessing for abuse during pregnancy. Severity and frequency of injuries and associated entry into prenatal care. JAMA. 1992;267(23):3176–8. doi: 10.1001/jama.267.23.3176. [DOI] [PubMed] [Google Scholar]
- 27.U.S. Census Bureau. http://www.census.gov.
- 28.Schafer JL. Analysis of Incomplete Multivariate Data. London: Chapman & Hall/CRC; 1997. [Google Scholar]
- 29.Singer JD. Using SAS PROC MIXED to Fit Multilevel Models, Hierarchical Models, and Individual Growth Models. J Educ Behav Stat. 1998;23(4):323–55. [Google Scholar]
- 30.Bolland JM, McCallum DM, Lian B, Bailey CJ, Rowan P. Hopelessness and violence among inner-city youths. Matern Child Health J. 2001;5(4):237–44. doi: 10.1023/a:1013028805470. [DOI] [PubMed] [Google Scholar]
- 31.Bolland JM. Hopelessness and risk behaviour among adolescents living in high-poverty inner-city neighbourhoods. J Adolesc. 2003;26(2):145–58. doi: 10.1016/s0140-1971(02)00136-7. [DOI] [PubMed] [Google Scholar]
- 32.Robrecht LC. Interpersonal violence and the pregnant homeless woman. J Obstet Gynecol Neonatal Nurs. 1998;27(6):684. doi: 10.1111/j.1552-6909.1998.tb02639.x. [DOI] [PubMed] [Google Scholar]
- 33.Rodriguez MA, Heilemann MV, Fielder E, Ang A, Nevarez F, Mangione CM. Intimate partner violence, depression, and PTSD among pregnant Latina women. Ann Fam Med. 2008;6(1):44–52. doi: 10.1370/afm.743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Greenland S. A critical look at methods for handling missing covariates in epidemiologic regression analyses. Am J Epidemiol. 1995;142(12):1255. doi: 10.1093/oxfordjournals.aje.a117592. [DOI] [PubMed] [Google Scholar]
- 35.Daoud N, Urquia ML, O'Campo P, Heaman M, Janssen PA, Smylie J, et al. Prevalence of abuse and violence before, during, and after pregnancy in a national sample of Canadian women. Am J Public Health. 2012;102(10):1893–901. doi: 10.2105/AJPH.2012.300843. [DOI] [PMC free article] [PubMed] [Google Scholar]


