Abstract
Myiasis is a general term for infection by fly larvae feeding on the host's necrotic or living tissue. Although infestation by fly larvae is much more prevalent in animals, it is a relatively frequent in occurrence. Oral myiasis is a rare pathology in humans and is associated with poor oral hygiene. Larvae cause itching and irritation due to their crawling movements and can destroy vital tissues, inducing serious or even life-threatening haemorrhage. The treatment is a mechanical removal of the maggots one by one; however, a systemic treatment with macrolide antibiotics, have been recently used for treatment. We present a case report of a 70-year-old man indigent, alcohol-dependent with an extensive necrotic wound in mandible and fetid odour. The prevention of human myiasis is by education, but unfortunately in the developing countries some people live in low social condition, predisposing the occurrence of the infestation.
Background
Poor oral hygiene, which is a primary cause for growth of maggots leading to the development of myiasis. Present case shows a unique association of oral squamous cell carcinoma (OSCC) with oral myiasis.
Case presentation
The term myiasis is derived from the Latin word ‘muia’ which means fly and ‘iasis’ means disease.1 It is a pathology caused by the larvae in human and animal tissue that evolve to a parasite.1–3 The flies deposit their eggs, which then hatch into larvae, which in turn infiltrate the tissue and destroy it.4 Clinical manifestations depend on the tissue involved and the larval population is directly proportional to the number of eggs deposited and the period of time that elapsed between infestation and diagnosis and treatment of the disease.5 The oral cavity is rarely affected by this infestation. It has been associated with poor oral hygiene, alcoholism, senility, suppurating lesions, severe halitosis and others conditions.3
The aim of this paper is to report an extensive case of myiasis associated with OSCC.
Case report
A 75-year-old male patient presented to the department of Oral & Maxillofacial Pathology, Modern Dental College & Research Center, Indore (Madhya Pradesh), India; with a chief complaint of worms coming out from the oral cavity, since 4 days. Extraoral examination showed a well-defined ulcerative lesion with central necrotic tissue and multiple live maggots crawling over it, present below the chin (figure 1). A thorough history of the patient was taken. Patient appeared to be irritated and uncooperative on interaction. He gave a history of pain and mobility with his lower-left mandibular premolars for which he underwent extraction, more than a month ago. After a week patient realised that the wound was unhealed. Later due to his carelessness and poor oral-hygiene maintenance, the wound became chronic and turned to the present size as an ulcerative lesion. Few days back patient noticed flies and worms crawling over and coming out from his mouth. On taking personal history it was known that the patient belonged to a very low-socioeconomic status. He was chronic alcoholic and had a very poor oral hygiene. On extraoral examination, a single well-defined ulcerative lesion was present below the chin region which extended from right parasymphisis region which crossed the midline to involve one-third of the left body of mandible. The borders appeared nodular and rolled. Centrally the floor of the ulcerative lesion showed brown necrosed tissue with many live maggots coming out. Single left-submandibular lymph node was palpable. Intraoral examination showed an ulceroproliferative lesion in relation to left anterior teeth with displacement of anterior teeth. Lesion extended posteriorly till 35 region. On palpation the associated teeth showed mobility. Intraorally too the worms appeared crawling. The surrounding skin was inflamed. On palpation the borders were indurated with the base of the lesion fixed to the underlying structures. Accordingly primary symptomatic treatment was done. Wound was cleaned and disinfected using turpentine oil. Maggots were removed manually with the help of forceps (figure 2). Antihelminthic and analgesic drugs with other antibiotics were prescribed.
Figure 1.

Photograph showing larvae crawling over the lesion.
Figure 2.

Photograph showing removal of larvae from the ulcerative lesion.
Treatment
Accordingly primary symptomatic treatment was done. Wound was cleaned and disinfected using turpentine oil. Maggots were removed manually with the help of forceps. Antihelminthic and analgesic drugs with other antibiotics were prescribed. Later biopsy procedure was conducted. Histopathological examination revealed nests and islands of neoplastic epithelial cells invading the connective tissue stroma. Invaded epithelial cells predominantly showed keratin pearl formation. A final diagnosis of well-differentiated OSCC with secondary oral myiasis was given (figure 3).
Figure 3.
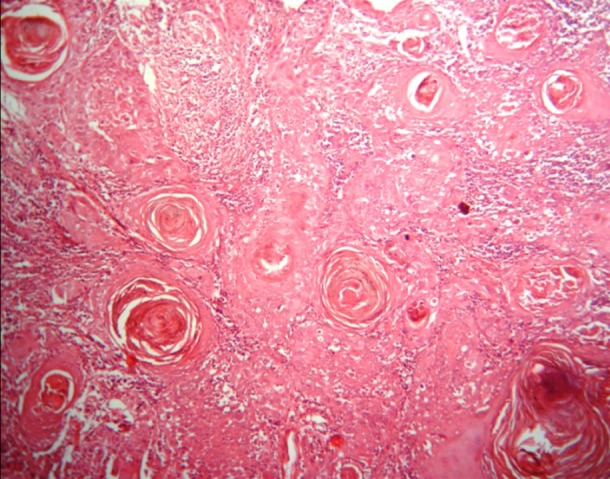
Photomicrograph showing invaded dysplastic epithelial cells in sheets and forming Keratin pearls ( H&E satin, ×100).
Outcome and follow-up
A 3-day follow-up was done till complete removal of the maggots as a primary treatment. Further the patient was referred to cancer hospital.
Discussion
Myiasis, is also known as hultukko by the Oromos of Southwestern Ethiopia and as yebissana til by the Amharas.6 German entomologist Fritz Zumpt describes myiasis as7 ‘the infestation of live human and vertebrate animals with dipterous larvae, which at least for a period, feed on the host's dead or living tissue, liquid body substances, or ingested food’.6–8 The Reverend Frederick William Hope coined the term myiasis in 1840 to refer to diseases resulting from dipterous larvae as opposed to those caused by other insect larvae.8 The flies responsible for this condition prefer a warm and humid environment, therefore myiasis is restricted to the summer months in temperate zones while it is all year round in the tropics.9 They lay over 500 eggs at a time onto foodstuffs, onto necrotic tissue in wounds or directly onto undamaged skin. The eggs hatch to become maggots in less than a week. The life cycle is completed in about 2 weeks when the maggots turn into flies.10 As soon as they mature, they wriggle out and fall to the ground to pupate.6 The developmental transition via the larval stage requires an intermediate host and the number of developing larvae depends on the number of viable eggs deposited.3 In the oral cavity, larvae burrow deeper into the soft tissues by making tunnels, separating the gingival and mucoperiosteum from the bone and obtain their nutrition from the surrounding tissues. They have a brown-black tip anteriorly, a greyish with colour and a cork-screw appearance.11
Myiasis affects mostly the uncovered body areas where oviposition is easily carried out. It frequently affects low socioeconomic level individuals with poor hygiene habits and unhealthy patients with psychiatric disorders, diabetics and immunocompromised patients.12 It is classified as specific, semispecific or accidental depending on their feed which being the host organs, body fluids or ingested food.8 Clinically, they can be classified as primary and secondary. Primary myiasis is caused by biophagous larvae (feed on living tissue), which are common in cattle (called bicheiras) and are rare in humans. Secondary myiasis is caused by the necrobiophagous flies (feed on dead tissue). This is a more common type and attacks patients with necrotic cavity lesions.13
Out of various options for treating this lesion, the simplest is the mechanical removal of the larvae with tweezers, usually under local anaesthesia. But, this is not possible because of the larva's hooks that it uses to grip the tissue cavity.14 Application of ether to the wound has been suggested in order to compel the maggots wiggle out of the host tissue. The wounds can be debrided by irrigating with normal saline or antiseptic medicaments such as 0.2% aqueous chlorhexidine, iodoform, ethyl chloride, mercuric chloride, creosote or turpentine oil. Whitehead varnish pack, which contains ether, can be applied to the raw wound for protection during the healing phase 3.10 Recently, Ivermectin, a semisynthetic macrolide antibiotic used in veterinary medicine, has been applied to the treatment of oral myiasis. This medication activates the release of γ-aminobutyric acid which induces the death of the larvae and their spontaneous elimination.5
Oral myiasis is a rare condition. Since first described by Laurence in 1909, only about two dozen cases of oral myiasis have been reported.15 Our case was among the cases where patient got secondarily infected by this infestation of fly on a pre-existing ulcerative lesion. The conditions being in favour are the history of previous unhealed extraction. Further his disturbed mental status, poor-economical status along with his poor status of oral hygiene maintenance favour the condition. Similar cases of oral myiasis in association with epidermoid carcinoma have also been reported by Gabriel et al12 and Carvalho et al.4 The present case and its consequences show that educational measures, basic sanitation and medical care close to home should be implemented especially in developing countries to improve the quality of life of the population.
Learning points.
Oral myiasis is very common to occur in open and necrotic wound.
Poor oral hygiene plays an important role in occurrence of oral myiasis.
Medical personnel taking care of old or debilitated patients need to bear in mind the possibility of this condition to be able to make a prompt diagnosis and implement relevant intervention to prevent extensive tissue destruction.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Sharma J, Mamatha GP, Acharya R. Primary oral myiasis: a case report. Med Oral Patol Oral Cir Bucal 2008;13:E714–16. [PubMed] [Google Scholar]
- 2.Rossi-Schneider T, Cherubini K, Yurgel LS, et al. Oral myiasis: a case report. J Oral Sci 2007;49:85–8. [DOI] [PubMed] [Google Scholar]
- 3.Abdo EN, Sette-Dias AC, Comunian CR, et al. Oral myiasis: a case report. Med Oral Patol Oral Cir Bucal 2006;11:E130–1. [PubMed] [Google Scholar]
- 4.Carvalho RW, Santos TS, Antunes AA, et al. Oral and maxillofacial myiasis associated with epidermoid carcinoma: a case report. J Oral Sci 2008;50:103–5. [DOI] [PubMed] [Google Scholar]
- 5.Nunes Melo AM, Nunes Alves WJ, Ribeiro Costa CC, et al. Oral myiasis: a case report in a child with cerebral palsy. J Clin Exp Dent 2010;2:e157–9. [Google Scholar]
- 6.Yewhalaw D, Legesse W, Gebre-Selassie S, et al. Human myiasis in an endemic area of Southwestern Ethiopia: prevalence, knowledge, perceptions and practices. Ethiop. J Health Dev 2007;21:166–72. [Google Scholar]
- 7.Wikipedia. Myiasis http://en.wikipedia.org/wiki/Myiasis.
- 8.Yuka K, Caksen H, Sakin Feyyat Y, et al. Aural myiasis in children and literature review. Tohuku J Exp Med 2005;206:125–30. [DOI] [PubMed] [Google Scholar]
- 9.Yucan Can M, Erol B, Balacan F, et al. Myiasis caused by Musca domestica larvae in a child: a case study. J Anim Vet Adv 2011;10:2149–52. [Google Scholar]
- 10.Yeung KH, Leung Chun-Fung A, Tsang Chee-Ching A. Oral myiasis. Hong Kong Dental J 2004;1:35–6. [Google Scholar]
- 11.Marzola C, Capelari Mm, Toledo-Filho J, et al. Human myiasis in Brazil case report. Roteiro completo da revista de odontologia da ato 2007;7:899–906. [Google Scholar]
- 12.Gabriel JG, Marinho SA, Verli FD, et al. Extensive myiasis infestation over a squamous cell carcinoma in the face. Case report. Med Oral Patol Oral Cir Bucal 2008;13:E9–11. [PubMed] [Google Scholar]
- 13.Shinohara Eh, Martini Mz, Neto Oliveira H, et al. Oral myiasis treated with ivermectin: case report. Braz Dent J 2004; 15:79–81. [DOI] [PubMed] [Google Scholar]
- 14.Verma N, Marya J. Oral myiasis in maxillofacial trauma—treated with ivermectin. Int J Dent Clin 2011;3:97–8. [Google Scholar]
- 15.Droma EB, Wilamowski A, Schnur H, et al. Oral myiasis: a case report and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 2007;103:92–6. [DOI] [PubMed] [Google Scholar]


