Abstract
The eye is a small and enclosed organ which makes it an ideal target for gene therapy. Recently various strategies have been applied to gene therapy in retinopathies using non-viral and viral gene delivery to the retina and retinal pigment epithelium (RPE). Subretinal injection is the best approach to deliver viral vectors directly to RPE cells. Before the clinical trial of a gene therapy, it is inevitable to validate the efficacy of the therapy in animal models of various retinopathies. Thus, subretinal injection in mice becomes a fundamental technique for an ocular gene therapy. In this protocol, we provide the easy and replicable technique for subretinal injection of viral vectors to experimental mice. This technique is modified from the intravitreal injection, which is widely used technique in ophthalmology clinics. The representative results of RPE/choroid/scleral complex flat-mount will help to understand the efficacy of this technique and adjust the volume and titer of viral vectors for the extent of gene transduction.
Keywords: Neuroscience, Issue 102, Subretinal injection, Retinal pigment epithelium, Gene therapy, Virus, Ophthalmology, Eye, Mice
Introduction
In ophthalmology, gene therapy has emerged as the treatment modality in monogenic inherited retinopathies. There are inherited retinopathies associated with genes in retinal pigment epithelium (RPE) including Leber congenital amurosis1,2, retinitis pigmentosa3, and choroideremia4. The research field of gene therapy is expanding in both preclinical studies and clinical trials using viral vectors such as adeno-associated virus (AAV), lentivirus (LV) and adenovirus (Ad)5. Different viral vectors have different tropism in the retina. For a safe and effective gene therapy, viral vectors should be carefully selected according to target cells and target genes.
The route of gene delivery is also important for effective gene delivery to target cells, thus, it should be carefully chosen as well. The two most common methods for intraocular delivery of viral vectors are subretinal injection and intravitreal injection6. The latter, intravitreal injection, has been widely used for drug delivery to treat choroidal neovascularization in wet age-related macular degeneration (AMD) and macular edema in diabetic retinopathy7. Intravitreal route provides exposure of viral vectors to vitreous and inner retina, but the diffusion of the vectors to outer retina is limited. On the other hand, the subretinal route provides direct delivery of viral vectors to the potential space between retina and RPE, inducing a localized bleb. Therefore, subretinal injection is currently considered a more efficient route for targeting photoreceptor cells and RPE. In terms of surgical approach, pars plana is chosen as a safe area for intravitreal injection to avoid retinal damage in human patients. By simply modifying this approach to mice, we could inject viral vectors subretinally or intravireally via limbal approach.
In this video article, we demonstrate an easy and convenient method of subretinal injection of viral vectors into mice RPE. After single puncture at posterior to limbus with a 30 G 1/2 needle, a 33 G blunt needle equipped microliter syringe is inserted into the subretinal space via the limbal puncture site. The viral vectors of 1.5 - 2 µl volume are injected to the potential space between retina and RPE inducing subretinal blebs. This procedure can be performed under direct visualization using surgical microscope. Repeated practice will guarantee replicable results even without direct visualization of the bleb formation. This will help the researchers to perform accurate and timesaving experiments for subretinal gene delivery in mice RPE.
Protocol
All experiments on animals were performed in accordance with the Association for Research in Vision and Ophthalmology Statement for the Use of Animals in Ophthalmic and Vision Research, and the guidelines and regulations set forth by the Seoul National University Institutional Animal Care and Use Committee and Seoul National University Hospital Biosafety Committee.
1. Preparing Injection Kit and Viral Vectors
Prepare the microliter syringe equipped with a 33 G blunt needle sterilized using ethylene oxide gas. Dilute the viral vectors in PBS for the adequate titer in the micro tube (i.e., 1 x 106 TU/µl). Flush the syringe several times with viral vectors to remove any dead space in the syringe.
2. Subretinal Injection of Viral Vectors
Anesthetize the adult mice (i.e., 6 - 8 weeks old) with an intraperitoneal injection of the mixture of tiletamine and zolazepam (1:1, 2.25 mg/kg body weight) and xylazine hydrochloride (0.7 mg/kg body weight) or an alternative suitable anesthesia regime.
Dilate pupils with an eye drop of phenylephrine 0.5% and tropicamide 0.5%.
Prepare the microliter syringe by loading with 1.5 - 2 µl of viral vectors.
Open the eyelid and protrude the eye to expose the equator for convenient injection and focus on under the operating microscope. Maintain the protruded eye position until finishing the injection, or displacement of the needle can occur during the injection. To hold the eyeball firmly, place the fingers outside the orbital rim.
Apply a drop of ophthalmic viscoelastic solution to the corneal surface.
Place a small round cover slide on the top of the cornea to visualize the retina.
Puncture a small hole at slight posterior to the limbus using a sterile 30 G 1/2 needle for the further subretinal injection. Make the hole inferior for the right eye, and superior for the left eye for the convenience. NOTE: If the hole is made at temporal or nasal, it’s hard to be covered by the eyelid after the injection. Initial puncture should be made slightly posterior to the limbus to avoid the limbal vessels which run along the limbus and can be easily recognized. Be careful to avoid hitting the lens with needle while making the initial puncture. Do not insert the entire bevel of the needle to avoid lens puncture.
Place the 33 G blunt needle of microliter syringe through the pre-punctured hole and approach the needle into the subretinal space until the point when mild resistance is felt. NOTE: For the subretinal injection, the best approach angle of the needle is about 45 degrees against iris plane, and the blunt needle should be pushed posteriorly toward peripapillary area. Dotted square indicated the suggested needle pathway across the vitreous cavity for the subretinal injection in Figure 1. NOTE: There will be no resistance felt when piercing (or passing) the retinal layers as they are very soft. Thus, the first feeling of mild resistance indicates that the needle has already touched the RPE layer and the insertion of the needle should be stopped. Be careful not to penetrate scleral tissue with excessive pressure because the needle should be placed in the potential subretinal space. If the needle punctures the scleral tissue by excessive power, it enters into the extraocular orbital spaces without resistance. (This step is critical)
 Figure 1. Schematic Diagram of the Subretinal Injection. H&E stained cross section of the mouse eye depicting the structures with a needle pathway for the subretinal injection marked (a dotted square). Magnification:40X, Scale bar: 500 µm. Please click here to view a larger version of this figure.
Figure 1. Schematic Diagram of the Subretinal Injection. H&E stained cross section of the mouse eye depicting the structures with a needle pathway for the subretinal injection marked (a dotted square). Magnification:40X, Scale bar: 500 µm. Please click here to view a larger version of this figure.
Inject the viral vectors (i.e., 1 x 106 TU/µl) gently into the subretinal space without tremor to avoid unwanted tissue damage and withdraw the needle gently. Hold the eyeball firmly during the injection as described in 2.4.
Observe the formation of subretinal bleb after the injection under operating microscope to make sure there is no retinal bleeding.
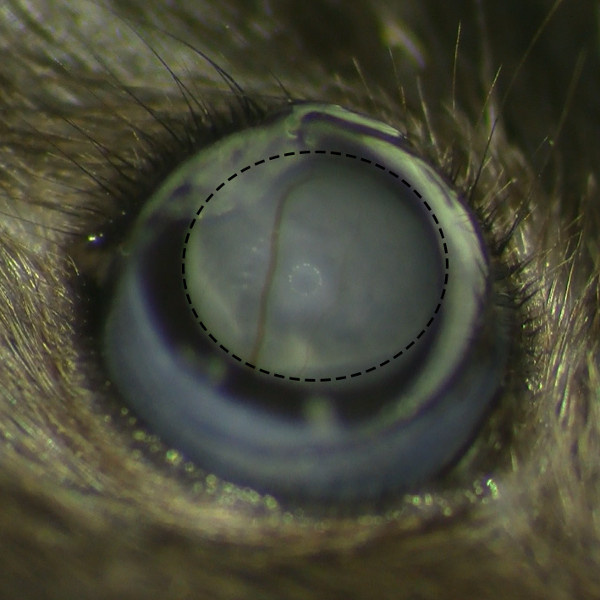 Figure 2. Subretinal Belb Formation without Retinal Hemorrhage. Microscopic view of subretinal belb after the subretinal injection under operating microscope shows successful bleb formation without retinal hemorrhage. Please click here to view a larger version of this figure.
Figure 2. Subretinal Belb Formation without Retinal Hemorrhage. Microscopic view of subretinal belb after the subretinal injection under operating microscope shows successful bleb formation without retinal hemorrhage. Please click here to view a larger version of this figure.
Gently close the eyelid to cover the injection site for self-sealing. Return the mice to home cage and keep alive until the evaluation. NOTE: After the researchers get used to the procedures, they can get the repeatable results with rapid procedures by skipping these steps (2.5, 6, and 10)
3. Evaluation of the Efficacy of Gene Delivery in Retinal Pigment Epithelium
Sacrifice the mice in the CO2 chamber. Enucleate the eyes using scissors.
Fix the eyes in the 4% paraformaldehyde solution at 4 °C for a minimum 1 hr to few days.
Grab the cornea with fine forceps and puncture the cornea with micro-scissors. Remove the cornea after scissoring along the limbus. Remove the lens with forceps.
Trim the ciliary body with micro-scissors allowing retinal detachment. Gently pull the whole retina from the RPE/choroid/sclera complex. Cut the RPE/choroid/scleral complex radially from the periphery to the center near optic nerve several times to make 4 to 8 leaves for flat mounting.
Flip the RPE/choroid/scleral complex to make RPE side down, and trim all the remaining tissues at the scleral side including muscles, conjunctiva and optic nerve. This step is important to make a flat RPE/choroid/scleral complex because any remaining tissue makes the complex uneven.
Incubate the complex with primary and secondary antibody for your specific research purposes (optional, see the references for detailed methods). Flat-mount the RPE/choroid/scleral complexes on the glass slide and absorb the PBS with an absorbent sponge.
Add 30 µl of mounting solution and place the cover slide. Observe the sample for the efficacy of vector delivery under fluorescein microscope. Keep the samples in the refrigerator for further observation.
Representative Results
To evaluate the efficacy of the subretinal injection on viral gene transduction by this protocol, we used commercially available LV vectors with CMV promoter expressing both GFP and RFP for the indicator. Eyes were enucleated after the appropriate time period according to the research purpose. For the representative results, eyes were enucleated 10 weeks and 20 weeks after subretinal injection. After complete removal of the retina using the method described above, the flat mount of RPE/choroid/sclera complex was evaluated under fluorescence microscope. The representative results were shown in Figure 3A (good example with complete removal of the retina) and Figure 3B (poor example with intact retina). Although the existence of remnant neural retina (especially photoreceptor outer segment) over RPE layer did not interfere to analyze the area of gene delivery in RPE, it blocked the fluorescence of GFP/RFP and inhibited direct visualization of RPE layer for further analyses. Therefore, complete removal of neural retina from the RPE/choroid/sclera complex would provide better results.
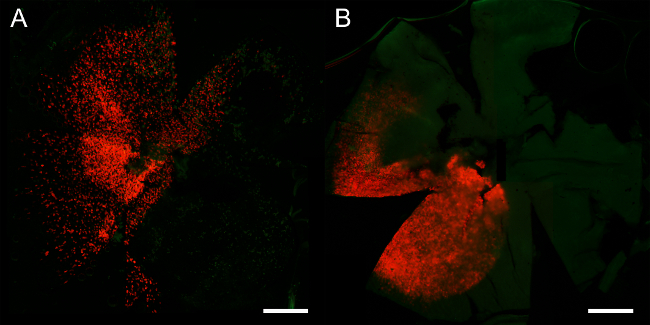 Figure 3. The Example of RPE/Choroid/Scleral Complex Flat-mount according to the Complete Removal of Retina. Twenty Weeks after Subretinal Injection of Lentivirus with GFP/RFP Gene. (A) Good example of RPE flat mount with complete removal of the retina shows clear and discrete expression of GFP/RFP in the RPE cells. (B) Poor example of RPE flat mount due to no removal of the retina shows the area of gene delivery with RFP signals which is inadequate to analyze the RPE pathology. Magnification: 40X, Scale bar: 500 µm. Please click here to view a larger version of this figure.
Figure 3. The Example of RPE/Choroid/Scleral Complex Flat-mount according to the Complete Removal of Retina. Twenty Weeks after Subretinal Injection of Lentivirus with GFP/RFP Gene. (A) Good example of RPE flat mount with complete removal of the retina shows clear and discrete expression of GFP/RFP in the RPE cells. (B) Poor example of RPE flat mount due to no removal of the retina shows the area of gene delivery with RFP signals which is inadequate to analyze the RPE pathology. Magnification: 40X, Scale bar: 500 µm. Please click here to view a larger version of this figure.
It is hard to judge the efficacy by the quantitative analysis because signal intensities of GFP/RFP are variable in the RPE cells of the injected area. In addition, the area of transduction is limited to the area of bleb formation after injection. Thus, it would be more reliable to judge the efficacy by the presence of GFP/RFP expression according to the viral titer per same injected volume (i.e. 2 µl). This helps to adjust appropriate viral titer for the experiment.
The representative results of RPE/choroid/scleral complex flat mount 10 weeks after subretinal injection were shown in various magnification in Figure 4 (40X) and Figure 5 (400X). The images with low magnification are enough to evaluate the area of GFP/RFP expression. On the other hand, the images with high magnification are necessary for other RPE pathology regarding to the researchers’ specific purposes. These images with various magnifications help to understand the viral expression pattern in RPE (Figure 4 and 5). We have also checked the expression of GFP/RFP up to 36 weeks post injection. The expression of GFP/RFP was still observed after 36 weeks post injection (data not shown).
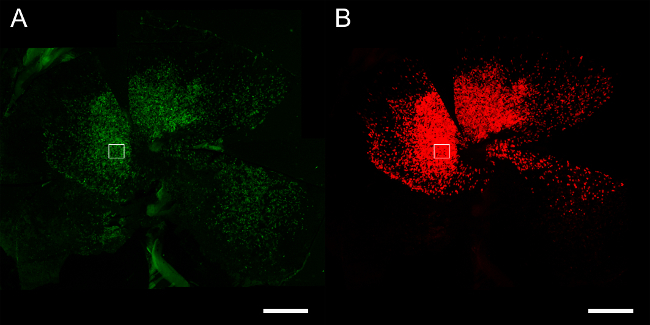 Figure 4. The Example of RPE/Choroid/Scleral Complex Flat-mount 10 Weeks after Subretinal Injection of Lentivirus with GFP/RFP Gene (Magnification: 40X). (A) green channel for GFP (B) red channel for RFP. Scale bar: 500 µm. Please click here to view a larger version of this figure.
Figure 4. The Example of RPE/Choroid/Scleral Complex Flat-mount 10 Weeks after Subretinal Injection of Lentivirus with GFP/RFP Gene (Magnification: 40X). (A) green channel for GFP (B) red channel for RFP. Scale bar: 500 µm. Please click here to view a larger version of this figure.
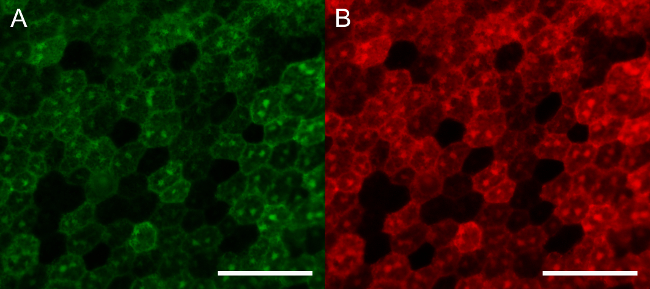 Figure 5. The Example of RPE/Choroid/Scleral Complex Flat-mount 10 Weeks after Subretinal Injection of Lentivirus with GFP/RFP Gene (Magnification: 400X). (A) green channel for GFP (B) red channel for RFP. Scale bar: 50 µm. Please click here to view a larger version of this figure.
Figure 5. The Example of RPE/Choroid/Scleral Complex Flat-mount 10 Weeks after Subretinal Injection of Lentivirus with GFP/RFP Gene (Magnification: 400X). (A) green channel for GFP (B) red channel for RFP. Scale bar: 50 µm. Please click here to view a larger version of this figure.
Discussion
In this video article, we described the limbal-approach subretinal injection technique in detail with representative results of RPE/choroid/scleral flat-mount. This is an easy and convenient technique for subretinal injection of viral vectors into RPE. Direct visualization of bleb formation during the injection is an important step for accurate delivery for the beginners. There are some subretinal injection techniques introduced in Journal of Visualized Experiments8-10. Subretinal space is the potential space between retina and RPE, therefore there are two possible routes to approach the subretinal space. One is an inside approach to the subretinal space via vitreous and retina and the other is an outside approach via RPE and sclera. This limbal-approach subretinal injection technique is the former one via intravitreal space and retina. This technique has an advantage to provide more posterior bleb formation compared to the latter because the latter approach makes a bleb from the peripheral side via scleral tunneling or incision, which should be made over the peripheral retina. In addition, simple limbal puncture is easier than scleral tunneling without retinal penetration. For the neonatal mice, however, it would be more appropriate to use the outside approach9. Because neonatal mouse’s eyeball is very small and full of the lens, limbal-approach technique can cause unwanted cataract formation or even phthisis bulbi.
There are some critical steps in this protocol. First of all, initial puncture should be place slightly posterior to the limbus because too anterior puncture at the cornea makes iris incarceration, or too posterior puncture makes direct hole at the peripheral retina. Secondly, it is recommended to be careful to avoid hitting the lens with needle while making the initial puncture. It is better not to insert the entire bevel of the needle to avoid lens puncture. Thirdly, the best approach angle of the needle is about 45 degrees against iris plane, and the blunt needle should be pushed posteriorly toward peripapillary area. Finally, the needle should be placed in the subretinal space during the injection, resulting in uniform bleb formations, otherwise the displaced needle causes intravitreal injection.
The eye is a small organ with unique features that make it an attractive target for gene therapy11. Specifically, it is a small-enclosed compartment with immune-privilege that enables gene therapy with relatively low toxicity and immune reactions in the eye and adverse systemic effects. Easy visualization and ready accessibility to surgical approaches are other advantages of the eye for gene therapy. The retina has a highly organized laminar structure with 10 distinct layers. Thus, accurate spatial gene delivery can only be achieved by the appropriate methods of intraocular injection. The two most common methods for intraocular delivery of viral vectors are intravitreal injection and subretinal injection6. In general, intravitreal injection is the preferred route for inner retina targeting retinal ganglion cells and Müller cells. Subretinal injection is the preferred route for outer retina targeting photoreceptor cells and RPE cells. For an efficient transduction in RPE, it is necessary to deliver viral vectors subretinally despite the potential for damage to the retina.
In this study, we used LV vectors with GFP and RFP for the visualization. Because viral vectors have tropism for specific cell types of the retina, viral vectors should be chosen according to tropism of AAV, LV, and Ad to target cells5. For example, AAV2/2, AAV2/6 and AAV2/8 are the highest transduction efficiency to RGC and Müller cells. AAV2/5, 2/7, 2/8 and 2/9 efficiently transduce photoreceptor cells and RPE with AAV2/8 being the most efficient serotype in mice5,12. AAV2/1, AAV2/2, AAV2/4, AAV2/6, and AAV2/8 efficiently transduce RPE5. For LV vectors, there is a high-level of expression in RPE cells after subretinal injections, but little or no expression after intravitreal injections13.
For effective gene delivery to RPE, viral promoters should be also considered. Viral promoters, such as cytomegalovirus (CMV) promoter and chimeric chicken beta-actin/CMV enhancer promoter are strong and ubiquitous promoters, thus, they are used in majority of gene therapy studies. In RPE, the CMV promoter is estimated to express ten-fold as much protein compared with the RPE65 promoter14. Of importance, the optimal combination of the promoter and viral vectors including serotype should be achieved for better results as demonstrated by superior expression of RPE65 when the human RPE65 promoter are packaged in serotype rAAV2/4 than rAAV2/215. Focusing on gene delivery to RPE cells, RPE-specific promoters such as the RPE65 or the VMD2 promoter reduces the off-target safety issues16.
AMD is a complex disease that has two phases with a degenerative phase referred to as dry AMD and a phase characterized by choroidal neovascularization referred to as wet AMD. Also, AMD is a disease in which numerous genetic susceptibilities including complement factor H (CFH), complement C3, complement factor I (CFI), Age-related maculopathy susceptibility 2 (ARMS2) and ApoE are combined with environmental risk factors17. Due to the complex nature of genetic risk factors in AMD, there is no single candidate gene for its gene therapy. Thus, the current gene therapy in AMD is focused on gene transfer to express anti-angiogenic proteins targeting choroidal neovascularization in wet AMD18. There is no candidate gene yet for treating dry AMD with a gene therapy. Recently, we suggested that intracellular amyloid beta accumulation could be related to dry AMD features in transgenic mice19. In addition, subretinally injected amyloid beta was taken up by RPE in mice (data not published). We can cleave intracellular amyloid beta with viral protease20. Thus, we have further studied the gene therapy in dry AMD with potential targets.
In conclusion, gene therapy in ocular disease is more promising than in any other organ. In addition, subretinal injection is a fundamental technique for gene therapy in retinal diseases, especially in relation to photoreceptor cells and RPE. Thus, we hope that this technique becomes more widely used and can contribute to the advancement of gene therapy not only in monogenic inherited retinopathy but also in age-related macular degeneration.
Disclosures
The authors have nothing to disclose.
Acknowledgments
This study was supported by the Seoul National University Research Grant (800-20140542), the Pioneer Research Program of NRF/MEST (2012-0009544), and the Bio-Signal Analysis Technology Innovation Program of NRF/MEST (2009-0090895), and the Grant of NRF/MEST (2015M3A9E6028949).
References
- Maguire AM, et al. Safety and efficacy of gene transfer for Leber's congenital amaurosis. N Engl J Med. 2008;358(21):2240–2248. doi: 10.1056/NEJMoa0802315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson SG, et al. Gene therapy for leber congenital amaurosis caused by RPE65 mutations: safety and efficacy in 15 children and adults followed up to 3 years. Arch Ophthalmol. 2012;130(1):9–24. doi: 10.1001/archophthalmol.2011.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conlon TJ, et al. Preclinical potency and safety studies of an AAV2-mediated gene therapy vector for the treatment of MERTK associated retinitis pigmentosa. Hum Gene Ther Clin Dev. 2013;24(1):23–28. doi: 10.1089/humc.2013.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLaren RE, et al. Retinal gene therapy in patients with choroideremia: initial findings from a phase 1/2 clinical trial. Lancet. 2014;383(9923):1129–1137. doi: 10.1016/S0140-6736(13)62117-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trapani I, Puppo A, Auricchio A. Vector platforms for gene therapy of inherited retinopathies. Prog Retin Eye Res. 2014;43:108–128. doi: 10.1016/j.preteyeres.2014.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang FQ, Anand V, Maguire AM, Bennett J. Intraocular delivery of recombinant virus. Methods Mol Med. 2001;47:125–139. doi: 10.1385/1-59259-085-3:125. [DOI] [PubMed] [Google Scholar]
- Peyman GA, Lad EM, Moshfeghi DM. Intravitreal injection of therapeutic agents. Retina. 2009;29(7):875–912. doi: 10.1097/IAE.0b013e3181a94f01. [DOI] [PubMed] [Google Scholar]
- Matsumoto H, Miller JW, Vavvas DG. Retinal detachment model in rodents by subretinal injection of sodium hyaluronate. J Vis Exp. 2013. [DOI] [PMC free article] [PubMed]
- Wert KJ, Skeie JM, Davis RJ, Tsang SH, Mahajan VB. Subretinal injection of gene therapy vectors and stem cells in the perinatal mouse eye. J Vis Exp. 2012. [DOI] [PMC free article] [PubMed]
- Eberle D, Santos-Ferreira T, Grahl S, Ader M. Subretinal transplantation of MACS purified photoreceptor precursor cells into the adult mouse retina. J Vis Exp. 2014. p. e50932. [DOI] [PMC free article] [PubMed]
- Sahel JA, Roska B. Gene therapy for blindness. Annu Rev Neurosci. 2013;36:467–488. doi: 10.1146/annurev-neuro-062012-170304. [DOI] [PubMed] [Google Scholar]
- Allocca M, et al. Novel adeno-associated virus serotypes efficiently transduce murine photoreceptors. J Virol. 2007;81(20):11372–11380. doi: 10.1128/JVI.01327-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi K, et al. Sustained transduction of ocular cells with a bovine immunodeficiency viral vector. Hum Gene Ther. 2002;13(11):1305–1316. doi: 10.1089/104303402760128531. [DOI] [PubMed] [Google Scholar]
- Rolling F, et al. Gene therapeutic prospects in early onset of severe retinal dystrophy: restoration of vision in RPE65 Briard dogs using an AAV serotype 4 vector that specifically targets the retinal pigmented epithelium. Bull Mem Acad R Med Belg. 2006;161(10-12):497–508. [PubMed] [Google Scholar]
- Le Meur G, et al. Restoration of vision in RPE65-deficient Briard dogs using an AAV serotype 4 vector that specifically targets the retinal pigmented epithelium. Gene Ther. 2007;14(4):292–303. doi: 10.1038/sj.gt.3302861. [DOI] [PubMed] [Google Scholar]
- Alexander JJ, Hauswirth WW. Adeno-associated viral vectors and the retina. Adv Exp Med Biol. 2008;613:121–128. doi: 10.1007/978-0-387-74904-4_13. [DOI] [PubMed] [Google Scholar]
- Puche N, et al. Genetic and environmental factors associated with reticular pseudodrusen in age-related macular degeneration. Retina. 2013;33(5):998–1004. doi: 10.1097/IAE.0b013e31827b6483. [DOI] [PubMed] [Google Scholar]
- Campochiaro PA. Gene transfer for neovascular age-related macular degeneration. Hum Gene Ther. 2011;22(5):523–529. doi: 10.1089/hum.2011.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park SW, et al. Intracellular amyloid beta alters the tight junction of retinal pigment epithelium in 5XFAD mice. Neurobiol Aging. 2014;35(9):2013–2020. doi: 10.1016/j.neurobiolaging.2014.03.008. [DOI] [PubMed] [Google Scholar]
- Shin B, et al. Intracellular cleavage of amyloid beta by a viral protease NIa prevents amyloid beta-mediated cytotoxicity. PLoS One. 2014;9(6):e98650. doi: 10.1371/journal.pone.0098650. [DOI] [PMC free article] [PubMed] [Google Scholar]


