Abstract
Electroencephalogram (EEG) has been traditionally used to determine which brain regions are the most likely candidates for resection in patients with focal epilepsy. This methodology relies on the assumption that seizures originate from the same regions of the brain from which interictal epileptiform discharges (IEDs) emerge. Preclinical models are very useful to find correlates between IED locations and the actual regions underlying seizure initiation in focal epilepsy. Rats have been commonly used in preclinical studies of epilepsy1; hence, there exist a large variety of models for focal epilepsy in this particular species. However, it is challenging to record multichannel EEG and to perform brain source imaging in such a small animal. To overcome this issue, we combine a patented-technology to obtain 32-channel EEG recordings from rodents2 and an MRI probabilistic atlas for brain anatomical structures in Wistar rats to perform brain source imaging. In this video, we introduce the procedures to acquire multichannel EEG from Wistar rats with focal cortical dysplasia, and describe the steps both to define the volume conductor model from the MRI atlas and to uniquely determine the IEDs. Finally, we validate the whole methodology by obtaining brain source images of IEDs and compare them with those obtained at different time frames during the seizure onset.
Keywords: Medicine, Issue 100, Neuroscience, electroencephalography (EEG), preclinical model, rodents, brain source imaging, epilepsy.
Introduction
It has been shown that interictal epileptiform discharges (IEDs) observed from EEG constitute useful markers of epileptogenesis in patients with focal epilepsy3. The regions inside the brain from which these IEDs originate, named irritative zones, can in practice be localized based on EEG recordings4. Preclinical models are essential to find correlates between these irritative zones and the actual regions underlying seizure initiation. However, recording EEG from small animals is challenging because of the small surface area of the head compared to the human scalp. Although invasive methods for chronic recording in rats can be used5, 6, techniques are not available at this moment to acquire traditional EEG recordings on rodents under acute conditions without the need of anesthesia.
To solve this problem, we apply a patented EEG mini-cap2, which allows us to record 32-channel EEG data from rodents noninvasively. In this study, we also provide evidence about the need of an analgesic to preserve IED frequency. Therefore, although fixation of EEG mini-cap was performed under isoflurane, EEG recordings were obtained with rats only under sedation (dexdomitor)7. The method proposed in this study can be used in any preclinical rat model of focal epilepsy. To illustrate the capabilities of this methodology, we apply it to understand the correlates between irritative and seizure-onset zones in focal cortical dysplasia (FCD). To that end, we use a “double-hit” model of FCD8 in Wistar rats.
To perform brain source analysis, it is required to: a) accurately extract IEDs from EEG raw data and b) obtain a volume conductor model for the individual animal head. To generate a practical volume conductor model, we use an in vivo rat MRI atlas, comprising average images of intensity/shape and obtained via non-linear registration of T2 images of 31 Wistar rats9. The forward model for the generated volume conductor was computed by boundary element method (BEM)10. As in the case of humans, two typical patterns of IEDs (sharp-waves and spikes) were detected and sub-classified into different clusters through an intelligent feature extraction, feature selection, and classification process11. These sub-classified signals are used to estimate the brain source localizations associated with different types of irritative zones. We present the source analysis steps using a well-known public software called Brainstorm12. The EEG source localizations for each IED sub-type and the seizure onset time frames were performed using standardized low-resolution brain electromagnetic tomography (sLORETA)13, which is available in Brainstorm.
Protocol
Ethics statement: All experiments are performed following the policies established by the Institutional Animal Care and Use Committee (IACUC) at Florida International University (IACUC 13-004).
1. EEG Recordings
- Preparation of the EEG mini-cap
- Immerse the electrode tips of the EEG mini-cap at least 12 hrs in distilled water with 0.2% chloride. Rinse the EEG mini-cap gently in distilled water. Dry the cap and the electrodes in the air.
- Mix EEG electrode paste with 0.9% NaCl solution in the volume proportion of 2 : 1. Add a drop of methylene blue, which will help to visualize the electrode paste inside the electrodes and on the skin. Take the mixed paste in a syringe. Make sure there are no air bubbles in the syringe. Inject the gel into each of the 32 electrodes, filling them without introducing any air bubbles. It is recommended to inject from the bottom rather than the top. This provides better access to each electrode and reduces the possibility of the gel spilling over.
- Turn on EEG and physiological recording system, and open the corresponding recording software on the computer in use.
- Animal preparation and anesthesia NOTE: Chronic epilepsy was created using a protocol for FCD8 in Wistar rats. The EEG recording were conducted in adult Wistar rats (8 weeks old, 300 - 400 g).
- Record the rat’s weight in an experiment sheet. Use this information to calculate sedative dose (dexdomitor 0.25 mg/kg). Induce anesthesia in the rat with 5% isoflurane and 100% oxygen (1 L/min at 14.7 psi).
- After trim the rat’s head, reduce isoflurane to 2% and maintain it during the entire setting of the EEG mini-cap. Check rat reflexes are absent (toe-pinch). Place the rat on a heating pad in the stereotaxic apparatus by fixing the ear canals using ear bars. Make sure anesthesia nose cone is secure.
- Apply lubricant ophthalmic ointment to each eye.
- Shave the extra hair on the rat head and ears using a razor. Avoid any bleeding during shaving. NOTE: Any hair left on the skin will produce noise in the EEG recordings. Rub the rat’s skin with 90% isopropyl alcohol to stimulate the blood vessels and degrease the skin.
- Place a saline swab on the scalp and cover it completely to keep good skin conductance until the EEG mini-cap is ready to be placed.
- Connect temperature, respiration, and three lead electrocardiogram probes. Note that the temperature is measured by a rectal probe. Continuously monitor the physiology of the rat during the recording procedures. Ensure that the normal temperature is 37 °C, respiration range is 30 - 60 breaths per minute, and heart rate is around 350 - 450 beats per minute .
- Recording procedures
- Remove the saline swab on the rat’s scalp and place the prepared EEG mini-cap on its skin. Fix the mini-cap with rubber bands. Place one rubber band on the front side of the scalp, usually in front of the eyes, and another band at the back of the scalp between the ears and neck. Use a plastic protector under the neck to facilitate normal respiration.
- Put a layer of high conductance electrode paste on both the ground and reference electrodes. Place them on the respective ear. NOTE: The reference electrode can be possibly placed in other locations.
- Connect the EEG mini-cap to the amplifiers and observe a preview of the workbench for electrode impedance. Check the performance of all electrodes. For a high-quality recording, ensure that the impedance value is in the range of 5 - 30 kΩ. If there are any noisy electrodes, provide better contact with the scalp by either moving them inside the scaffold toward the scalp or gently injecting more gel from the top of the electrode.
- Administer dexdomitor (0.25 mg/kg) intraperitoneally and immediately reduce isoflurane rate to 0%. If the respiration rate is not within 30 - 60 breaths per minute range, start increasing the isoflurane rate gently. Do not exceed the value of 1% isoflurane. Monitor this step carefully because the mixture of isoflurane and dexdomitor could prompt the animals to a critical condition. NOTE: On the preclinical model of focal epilepsy, isoflurane affects IEDs, whereas dexdomitor does not. Subjects under isoflurane have weaker epileptogenic property, i.e., relatively fewer IEDs can be detected compared to other conditions7,14. The dexdomitor dose is effective for about 2 hrs. Thus, to save the time for its effect, the preparation was carried out under isoflurane.
- Conduct EEG recordings. After the recording, mark the positions of the three jutting circles of the EEG mini-cap on top of the skin by inserting a color pen inside them before the EEG mini-cap is removed. Use them as landmarks for MRI co-registration. Take a picture of the rat head with the landmarks. Place the rat back inside the cage and monitor it until complete recovery from dexdomitor’s effect. NOTE: In this experiment, red color (opponent color to green) was used to distinguish from the electrode positions (green). However, it is recommended to use other colors (purple/green) if small bleeding spots are observed in the skin.
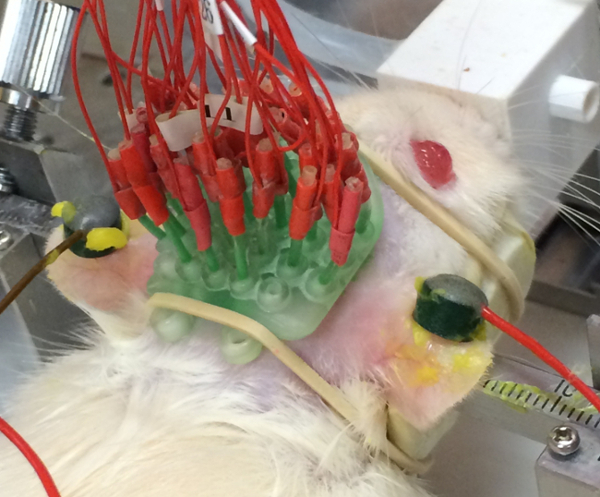 Figure 1. A picture of the EEG mini-cap placed on a particular rat.
Figure 1. A picture of the EEG mini-cap placed on a particular rat.
2. Brain Source Imaging
- IED classification NOTE: The IED detection and classification is performed using self-developed codes in MATLAB based on the previous study15. This software will be available by request.
- Discard noisy channels by visually inspecting the EEG tracers. Remove EKG artifacts using an automatic method for periodic waveform subtraction, which is based on a template and a correlation analysis. NOTE: Usually, the experimenter who recorded the EEG shares the written experimental sheet for the observed bad channel information based on the impedance values. Software to remove EKG artifacts will be also available by request.
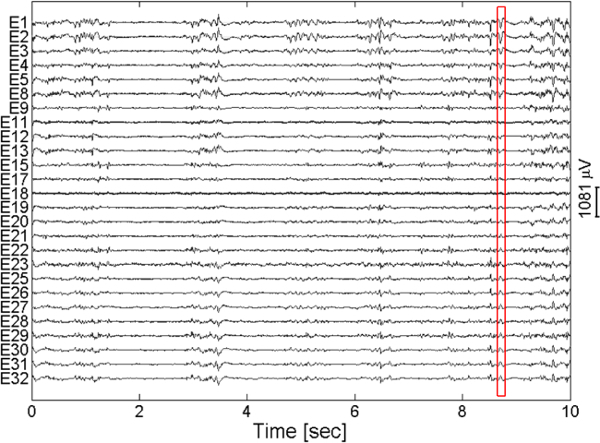 Figure 2. An example of the EEG trace showing different types of IEDs. The red box indicates one type of IEDs. Please click here to view a larger version of this figure.
Figure 2. An example of the EEG trace showing different types of IEDs. The red box indicates one type of IEDs. Please click here to view a larger version of this figure. - Apply a band-pass filter with cutoff frequencies of 3 - 150 Hz and a notch filter to remove the line frequency (60 Hz in general and 50 Hz in some countries) component offline.
- Detect two types of IEDs (spikes and sharp-waves). Spikes and sharp-waves constitute large electrical events of 20 - 70 ms and 70 - 200 ms in duration respectively. Therefore, after applying a respective band-pass filter (cutoff frequencies of 15 - 50 Hz for spikes and 5 - 15 Hz for sharp-waves), the IEDs are detected based on amplitude thresholds15. NOTE: The thresholds are automatically set to 4σ as suggested in the previous study for multiunit activity15. Here, σ is an estimated standard deviation of the bandpass-filtered signal, σ = median{|filtered signal| ⁄ 0.6745}.
- Sub-classify spikes and sharp-waves into different clusters. The distinctive features of different spikes and sharp-waves are extracted using wavelet transform15. They are sub-classified into multiple clusters using k-means, and the optimal cluster number k is determined using silhouette.
- Average the sub-classified signals within the same cluster. The average EEG signals for each IED sub-type will be used for brain source analysis.
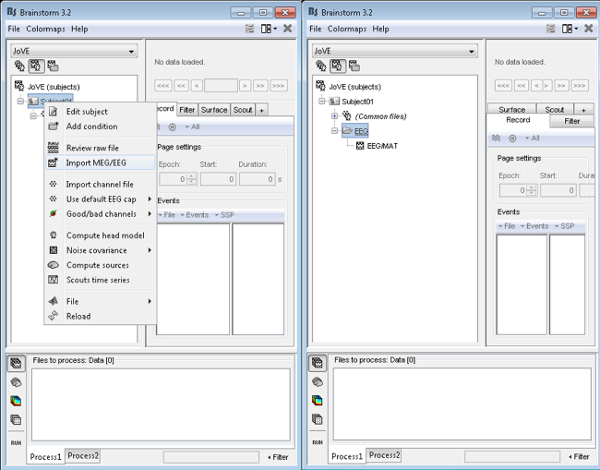
- Volume conductor model NOTE: For the following sections, the open source software, Brainstorm12, will be used with the MRI atlas for Wistar rats9. However, individual rat’s MRI can also be used to generate the volume conductor model if available. The MRI atlas9 can be downloaded at http://www.idac.tohoku.ac.jp/bir/en/. This website provides the atlas as NIFTI format under “Wistar Rat MRI Atlas” section, and it can be accessible after registration. The software needed for pre-processing can be also found in this website.
- Input MRI and brain surface to the software12.
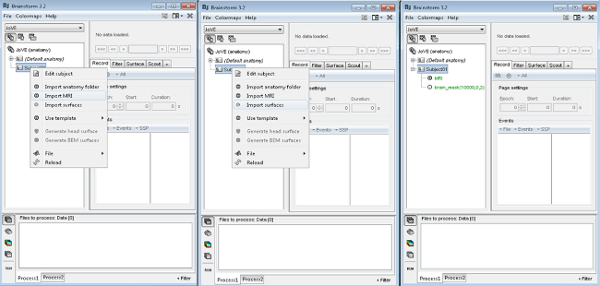 Please click here to view a larger version of this figure.
Please click here to view a larger version of this figure.
- Generate head surface with default setting.
 Please click here to view a larger version of this figure.
Please click here to view a larger version of this figure.
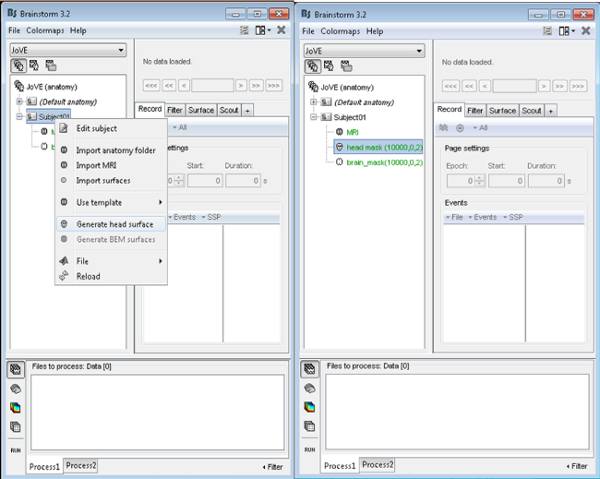
- Generate scalp and inner/outer skull surfaces based on MRI for lead field computation12. NOTE: The resolution of the vertices influences the accuracy of the estimated source, but large number of vertices results in high computational complexity. Recommended number of vertices of each layer is 642 for acceptable accuracy with fair computational complexity. The thickness of the skull can be checked from the MRI, and in the case of the MRI atlas, it is approximately 1 mm. After inserting above values in the software, corresponding triangle face-vertex meshes for each surface will be created.
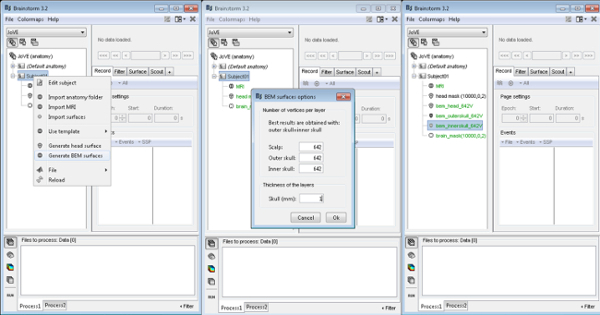 Please click here to view a larger version of this figure.
Please click here to view a larger version of this figure.
- Check the orientation and location of each surface with respect to the MRI using the visualization option. Modify accordingly, if any surfaces are not co-registered12.
 Please click here to view a larger version of this figure.
Please click here to view a larger version of this figure.
- Using the rat head picture acquired in 1.3.5. co-register the positions of the 3 landmarks (R1, R2, and R3) in the MRI. Use the grid points of the landmarks as references to generate the electrode positions as the electrodes are fixed on the scaffold (Figure 3B).
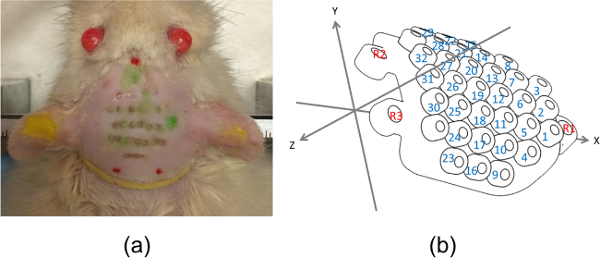 Figure 3. (A) Rat head picture used to obtain electrode positions and (b) the EEG mini-cap diagram with the coordinate system. Red dots in (A) indicate the landmarks mentioned in 1.3.5. which correspond to the red numbers in (B). Also, the green marks in (A) depict the 32 electrode positions, and they correspond to the blue numbers in (B). Please click here to view a larger version of this figure.
Figure 3. (A) Rat head picture used to obtain electrode positions and (b) the EEG mini-cap diagram with the coordinate system. Red dots in (A) indicate the landmarks mentioned in 1.3.5. which correspond to the red numbers in (B). Also, the green marks in (A) depict the 32 electrode positions, and they correspond to the blue numbers in (B). Please click here to view a larger version of this figure. - Generate N × 3 electrode position matrix based on the 3 landmarks. Here, N is the number of channels (N = 32) and the column represents the corresponding x, y, and z coordinate values. NOTE: The EEG mini-cap is a rigid scaffold. Therefore, once the 3 reference grids (R1, R2, and R3) are obtained, the position of the electrodes are automatically set. The user will only need to redefine the Z-values on a way that the mini-cap is appropriately projected on the scalp. The N point grids can be numbered sequentially as depicted in Figure 3B blue numbers. The standard scaffold for the EEG mini-cap is commercially available (Table of Materials). The software for co-registration is also available to the community.
- Input the generated channel file.
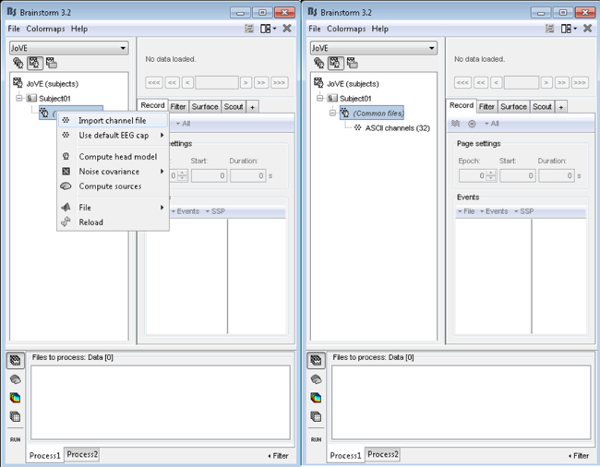 Please click here to view a larger version of this figure.
Please click here to view a larger version of this figure.
- Display and confirm the location of all electrodes. Modify any misplaced electrodes12. The final coordinate system for the electrode positions should coincide with the coordinate system used for the above-mentioned surfaces. NOTE: The created surfaces can be visually inspected on an MRI by using the visualization option, “MRI registration\Check MRI/surface registration.” And then, a selected surface will be displayed as yellow line on the MRI. In addition, the 3 landmarks and the 32 electrode positions can be displayed on the MRI by selecting the toolbox’s option, “Display Sensors\MRI Viewer.” The locations can be visually inspected by comparing the distributions based on the rat’s eye and ear locations (Figure 4).
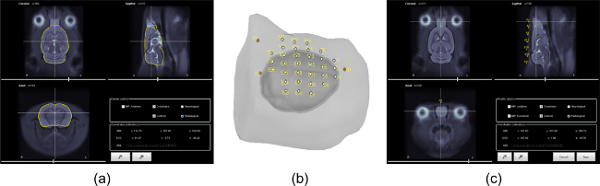 Figure 4. (A) MRI atlas with co-registered brain surface (yellow line), (B) the created volume conductor model with the aligned 32 electrodes and 3 landmarks (red dots), and (C) MRI atlas with co-registered reference grid R1. Please click here to view a larger version of this figure.
Figure 4. (A) MRI atlas with co-registered brain surface (yellow line), (B) the created volume conductor model with the aligned 32 electrodes and 3 landmarks (red dots), and (C) MRI atlas with co-registered reference grid R1. Please click here to view a larger version of this figure.
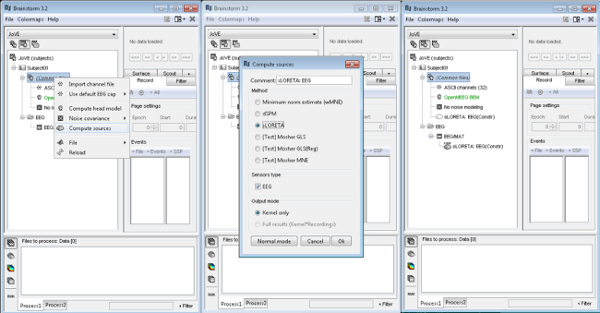
- Brain Source Imaging
- Compute lead field matrix13. Input the conductivity values which satisfy the ratio of skin, skull, and brain as 1 : 1/80 : 1. Obtain the lead field matrix based on the volume conductor model and the electrode positions created in 2.2. NOTE: The toolbox12 offers the interface with the other software to compute BEM10. Therefore, only the conductivity values are required as input.
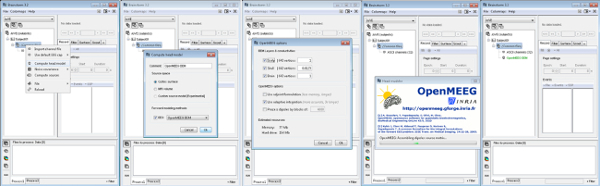 Please click here to view a larger version of this figure.
Please click here to view a larger version of this figure.
- Input the average EEG signals for each IED sub-type stored in 2.1.4.
 Please click here to view a larger version of this figure.
Please click here to view a larger version of this figure.
- Obtain sLORETA solution13 based on the computed lead field matrix and the input EEG signals. By selecting the source estimation method option, the inverse solution can be obtained12.
 Please click here to view a larger version of this figure.
Please click here to view a larger version of this figure.
- Plot the estimated sources.
Representative Results
Once all procedures are properly completed, estimated sources can be visualized in the brain surface of the pre-clinical model. Figure 5 shows the estimated sources from one particular sub-type of spikes (top) and sharp-waves (bottom) from IEDs. In addition, Figure 6 displays how the source distribution changes in sequential time frames during a seizure establishment. These results support the capability of the proposed methodologies to record high-resolution EEG on rats with focal epilepsy and to conduct source analysis using the recorded EEG.
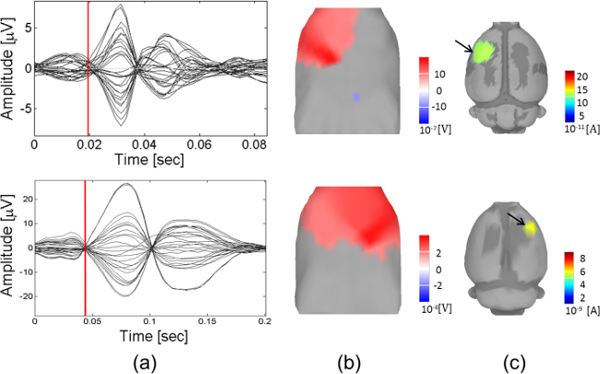
Figure 5. Estimated brain source locations of IEDs with respect to different clusters in spikes (top) and sharp-waves (bottom).(A) Time series, (B) EEG topography, and (C) cortical current sources. The evaluation is performed at a specific time marked with a red vertical line in (A). Please click here to view a larger version of this figure.
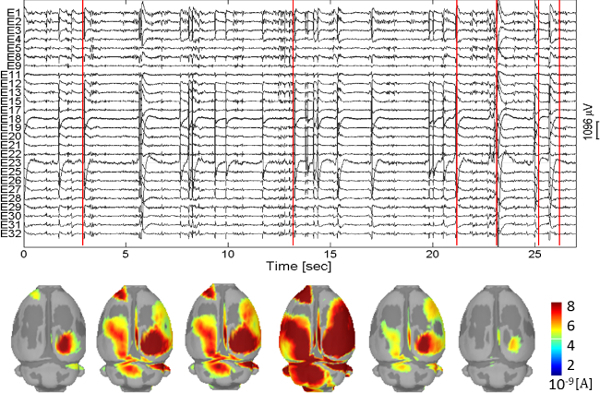 Figure 6. Estimated brain sources during seizure. The time instants are marked as red vertical lines. Please click here to view a larger version of this figure.
Figure 6. Estimated brain sources during seizure. The time instants are marked as red vertical lines. Please click here to view a larger version of this figure.
Discussion
A new methodology to non-invasively record multichannel EEG in a particular preclinical model of focal epilepsy is described. The particulars for the recording and analysis procedures, with specific experimental tips, are provided. There were key factors to consider achieving successful results. First, for EEG recordings, obtaining high quality signals is essential. Proper viscosity of the EEG paste should be applied to each electrode during the mini-cap preparation, and the rat’s head and ear hair should be completely removed during shaving. Impedance check is the most important step to confirm the quality of EEG recordings. Second, for brain source imaging, generating proper volume conductor model is crucial. Each surface should be co-registered. Also, the generated electrode positions should have minimum distance error from the actual electrode locations on the rat’s scalp.
Even though this manuscript introduces source analysis procedures using Brainstorm12, they can be conducted using other open softwares16,17 and commercial products18,19. Also, besides sLORETA13, other inverse solutions such as multiple dipole models and Beamformer can be applied4.
One limitation of this approach is that behavior analysis cannot be conducted since the EEG recording is carried out under sedation. However, compared to the other methods for EEG recording in rats5,6, this approach is noninvasive.
Our preliminary results support the importance for a precise classification of IED markers from EEG recordings to determine the irritative zones in a rat with focal epilepsy, as well as to evaluate their relationship with the underlying mechanisms for seizure initiation11. In addition, it has been shown that EEG source localization for such specific IEDs showed a good correspondence with the respective BOLD activation and deactivation regions20.
Our study will stimulate the use of preclinical models to evaluate bed-bench-bed strategies developed by biomedical engineers. For example, IED extraction is nowadays performed in hospitals manually, which required a considerable human effort. The methodology proposed in this study does it automatically. We hypothesize that the use of this methodology will produce similar results when applied to patients with FCD. We are preparing IRB protocols for the evaluation of this and other aspects of the methodology in human dataset.
Moreover, the use of preclinical models will help us understand the capabilities and limitations of EEG source localization in epilepsy21. Accurate estimation of brain sources underling epileptogenesis is crucial for therapeutic strategies and surgical planning. Also, having a standard platform for EEG recording in rats will be useful for the evaluation of the effectiveness of several anti-epileptic drugs in preclinical trials. This is the first study in which epileptic rats are recorded non-invasively under sedation, which will open new doors for the evaluation of EEG biomarkers for epilepsy. However, the entire methodology presented in this study is extendable to other experimental conditions and brain disorders. The EEG mini-cap can be also used in other rodent’s types.
In the past, a forepaw stimulation paradigm in Wistar rats has been used to evaluate the quality and reproducibility of data recorded with the EEG mini-cap2. Moreover, validations for the brain source reconstruction have been performed from high-resolution skull EEG concurrently recorded with laminar local field potentials from Wistar rats under a whisker stimulation paradigm22. This methodology has been developed for Wistar rats because of the existence of an MRI atlas for this particular rat strain. However, it can be applied to other rodent types with their standard format of atlas including mouse23, Sprague-Dawley rats24, and Paxinos and Watson rats25. In addition, the fundamental procedures of our proposed methodology could be used in any rodent preclinical models for which EEG is an important modality. However, many aspects of this methodology are particularly for epilepsy, especially those related to EEG preprocessing (IED detection and classification). Also, researchers must be aware of proper drugs used for sedation in different cases. The use of isoflurane and dexdomitor in our study has been carefully considered due to the reduced impact on IEDs. Regarding EEG recordings, in the case of mouse, the relatively small scalp surface area would reduce the number of channels considerably.
Disclosures
No conflicts of interest declared.
Acknowledgments
The authors would like to thank Pedro A. Valdes Hernandez, Francois Tadel, and Lloyd Smith for their valuable advice and fruitful discussion. We also thank Rafael Torres for the proof reading.
References
- Furman M. Seizure Initiation and Propagation in the Pilocarpine Rat Model of Temporal Lobe Epilepsy. Journal of Neuroscience. 2013;33(42):16409–16411. doi: 10.1523/JNEUROSCI.3687-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sumiyoshi A, Riera JJ, Ogawa T, Kawashima R. A Mini-Cap for simultaneous EEG and fMRI recording in rodents. NeuroImage. 2011;54(3):1951–1965. doi: 10.1016/j.neuroimage.2010.09.056. [DOI] [PubMed] [Google Scholar]
- Engel J, et al. Epilepsy biomarkers. Epilepsia. 2013;54(4):61–69. doi: 10.1111/epi.12299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baillet S, Mosher JC, Leahy RM. Electromagnetic Brain Mapping. IEEE Signal Processing Magazine. 2001;18(6):14–30. [Google Scholar]
- Quairiaux C, Megevand P, Kiss JZ, Michel CM. Functional Development of Large-Scale Sensorimotor. Cortical Networks in the Brain. Journal of Neuroscience. 2011;31(26):9584–9510. doi: 10.1523/JNEUROSCI.5995-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee M, Kim D, Shin HS, Sung HG, Choi JH. High-density EEG recordings of the freely moving mice using polyimide-based microelectrode. Journal of Visualized Experiments. 2011. p. e2562. [DOI] [PMC free article] [PubMed]
- Bernal B, Grossman S, Gonzalez R, Altman N. fMRI under sedation: what is the best choice in children. Journal of Clinical Medicine Research. 2012;4(6):363–370. doi: 10.4021/jocmr1047w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colciaghi F, et al. Status epilepticus-induced pathologic plasticity in a rat model of focal cortical dysplasia. Brain. 2011;134(10):2828–2843. doi: 10.1093/brain/awr045. [DOI] [PubMed] [Google Scholar]
- Valdez-Hernandez PA, et al. An in vivo MRI Template Set for Morphometry, Tissue Segmentation, and fMRI Localization in Rats. Frontiers in Neuroinformatics. 2011;5(26):1–59. doi: 10.3389/fninf.2011.00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gramfort A, Papadopoulo T, Olivi E, Clerc M. OpenMEEG: opensource software for quasistatic bioelectromagnetics. BioMedical Engineering OnLine. 2010;9(45) doi: 10.1186/1475-925X-9-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song Y, Sanganahalli B, Hyder F, Lin W, Riera J. An fMRI and EEG Study of Epileptogenesis in a Rat Model of Focal Cortical Dysplasia. Organization for Human Brain Mapping. 2014. Available from: https://ww4.aievolution.com/hbm1401/index.cfm?do=abs.viewAbs&abs=4046.
- Tadel F, Baillet S, Mosher JC, Pantazis D, Leahy RM. Brainstorm: A User-Friendly Application for MEG/EEG Analysis. Computational Intelligence and Neuroscience. 2011;2011:1–13. doi: 10.1155/2011/879716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascual-Marqui RD. Standardized low resolution brain electromagnetic tomography (sLORETA): technical details. Methods & Findings in Experimental & Clinical Pharmacology. 2002;24(D):5–12. [PubMed] [Google Scholar]
- Iijima T, Nakamura Z, Iwao Y, Sankawa H. The Epileptogenic Properties of the Volatile Anesthetics Sevoflurane and Isoflurane in Patients with Epilepsy. Anesthesia and Analgesia. 2000;91(4):989–995. doi: 10.1097/00000539-200010000-00041. [DOI] [PubMed] [Google Scholar]
- Quiroga QR, Nadasdy Z, Ben-Shaul Y. Unsupervised spike detection and sorting with wavelets and super-paramagnetic clustering. Neural Computation. 2004;16(8):1661–1687. doi: 10.1162/089976604774201631. [DOI] [PubMed] [Google Scholar]
- Delorme A, Makeig S. EEGLAB: an open source toolbox for analysis of single-trial EEG dynamics including independent component analysis. Journal of Neuroscience Methods. 2004;134(1):9–21. doi: 10.1016/j.jneumeth.2003.10.009. [DOI] [PubMed] [Google Scholar]
- Oostenveld R, Fries P, Maris E, Schoffelen JM. FieldTrip: Open Source Software for Advanced Analysis of MEG, EEG, and Invasive Electrophysiological Data. Computational Intelligence and Neuroscience. 2011;2011:1–9. doi: 10.1155/2011/156869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koessler L, et al. Source localization of ictal epileptic activity investigated by high resolution EEG and validated by SEEG. NeuroImage. 2010;51(2):642–653. doi: 10.1016/j.neuroimage.2010.02.067. [DOI] [PubMed] [Google Scholar]
- Manganotti P, et al. Scalp topography and source analysis of interictal spontaneous spikes and evoked spikes by digital stimulation in benign rolandic epilepsy. Electroencephalography and Clinical Neurophysiology. 1998;107(1):18–26. doi: 10.1016/s0013-4694(98)00037-6. [DOI] [PubMed] [Google Scholar]
- Bae J, Deshmukh A, Song Y, Brain Riera J. Source Analysis of Interictal Epileptiform Discharges Using a Rat Model of Focal Epilepsy. Organization for Human Brain Mapping. 2014. Available from: https://ww4.aievolution.com/hbm1401/index.cfm?do=abs.viewAbs&abs=4098.
- Birot G, et al. Head model and electrical source imaging: A study of 38 epileptic patients. NeuroImage: Clinical. 2014;16(5):77–83. doi: 10.1016/j.nicl.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riera JJ, et al. Pitfalls in the dipolar model for the neocortical EEG sources. Journal of Neurophysiology. 2012. [DOI] [PubMed]
- Hawrylycz M, et al. The Allen Brain Atlas. Springer Handbook of Bio-Neuroinformatics. 2014. pp. 1111–1126.
- Schweinhardt P, Fransson P, Olson L, Spenger C, Andersson JL. A template for spatial normalization of MR images of the rat brain. Journal of Neuroscience Methods. 2003;129(2):105–113. doi: 10.1016/s0165-0270(03)00192-4. [DOI] [PubMed] [Google Scholar]
- Schwarz AJ, et al. A stereotaxic MRI template set for the rat brain with tissue class distribution maps and co-registered anatomical atlas: application to pharmacological MRI. Neuroimage. 2006;32(2):538–550. doi: 10.1016/j.neuroimage.2006.04.214. [DOI] [PubMed] [Google Scholar]


