Abstract
The authors report a case of a 47-year-old professional driver with an acute, simultaneous tear of patellar tendon and anterior cruciate ligament (ACL). The patient was treated in two stages. Acute patellar tendon repair and delayed (6-month postinjury) ACL reconstruction was performed. The authors discuss the possible mechanism of injury and the rationality of the two-stage surgical treatment.
Background
Patellar tendon and anterior cruciate ligament (ACL) tear is an uncommon injury. Moreover, the mechanism of injury and the best surgical approach have not been established yet. We believe that case reports like ours contribute to a better understanding of the mechanism of injury and help the surgeon to decide whether to proceed in one- or two-stage procedure.
Case presentation
A 47-year-old professional driver presented in the outpatient clinic of our department after sustaining an injury in his left knee. He was manually unloading a heavy package from his truck and while descending to the ground he felt a double ‘pop’ in his left knee and fell down. Physical examination revealed diffuse knee swelling. The knee was extremely tender, even in slight palpation, especially anteriorly and medially. A palpable defect of the patella tendon was detected, and active knee extension was impossible. Valgus stress demonstrated medial collateral ligament (MCL) disruption while Lachman–Noulis and pivot-shift test could not be performed because of the intense pain. The anteroposterior and lateral radiographs showed superior displacement of the patella without any other osseous pathology. Consequently, the patient was admitted in our department, under the diagnosis of patellar tendon and MCL tear.
Investigations
The patient did not report any remarkable medical history that could predispose to tendon rupture. Clinical and laboratory (haematological and metabolic profile) investigations failed to reveal any of the risk factors that have been reported in the literature for tendon rupture (diabetes mellitus, chronic renal failure, hyperparathyroidism, atherosclerosis, gout, pseudo-gout, hyperlipidaemia, lupus erythematosus, systemic use of steroids, local injections of steroids, obesity, sports activity, local exposure to methidathion).1
Treatment
The patient was operated the next day. Under epidural anaesthesia, a midline, longitudinal incision was used to expose the patellar tendon. Superficial and deep dissection revealed mid-substance tear of the patellar tendon with fraying of both ends and medial retinaculum, and MCL tears (figure 1). The fat pad was also torn at the level of the patellar tendon tear (figure 1). Inspection of the joint revealed a chondral defect of the medial femoral condyle, an ACL rupture and tears of medial and lateral meniscus.
Figure 1.
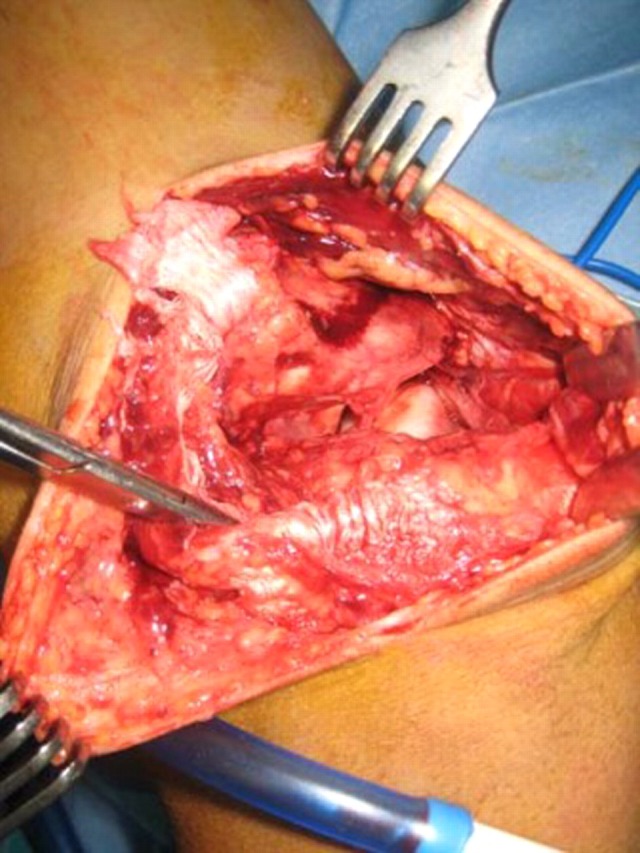
Patellar tendon, medial retinaculum and medial collateral ligament tear.
The chondral defect of the medial femoral condyle was small in size (1×2 cm) and was debrided. The radial tear of the posterior horn of the meniscus was treated with partial meniscectomy, and the incomplete, peripheral, stable (<1 cm in length) tear of the medial meniscus was left alone. Regarding the ACL tear, we decided not to proceed in acute ACL reconstruction. The medial retinaculum and capsule were torn in a horizontal fashion and were sutured separately. The capsule was sutured with No 3-0 absorbable sutures and the retinaculum with No 2-0 absorbable sutures. The patellar tendon tear was repaired using non-absorbable braided suture No 2. The tendon repair was protected by a figure-of-eight stainless steel wire loop (figure 2) which did not permit knee flexion beyond 90°.
Figure 2.

The tendon repair was protected by a figure-of-eight stainless steel wire loop.
Postoperatively, the knee was immobilised in a plaster for 6 weeks in full extension. Subsequently, the plaster was removed and replaced by a hinged knee brace. Knee range of motion 0–60° was allowed for 4 weeks and 0–90° for another 6 weeks. Weight bearing as tolerated was permitted 6-week postoperatively. Four months after the operation, the wire loop was removed under local anaesthesia and full knee flexion was permitted. The patient regained full range of motion at 6 months after the patellar tendon repair. The knee was evaluated for instability signs. Lachman–Noulis and pivot shift tests were positive, and the patient elected to undergo ACL reconstruction despite the fact that he did not experience any giving-way episodes. At this point, an MRI was undertaken to evaluate the patellar tendon repair. MRI demonstrated a healed patellar tendon with sites of abnormal signal because of the non-absorbable sutures and ACL tear (figure 3). Hamstrings autograft was used for the ACL reconstruction, and the postoperative period was uneventful.
Figure 3.
MRI demonstrated a healed patellar tendon with sites of abnormal signal because of the non-absorbable sutures and anterior cruciate ligament tear.
Outcome and follow-up
The patient returned to the preinjury level of activity at 8 months after the ACL reconstruction and in total 14 months after the initial injury. Three years postoperatively he remains asymptomatic.
Discussion
Simultaneous patellar tendon and ACL tear is an uncommon injury with seven reports in the literature so far.2–8 Predisposing factors for patellar tendon tear were either not investigated or found, and, consequently, trauma was considered the cause of rupture in all cases including ours.2–8 The most common mechanism of injury was forceful contraction of quadriceps.2 4 5 7 Nevertheless, the mechanism of injury is not fully understood. During landing from a jump, the quadriceps is eccentrically contracted to decelerate knee flexion. Moreover, landing with the ankle joint in plantar flexion reduces the contribution of the calf to the squat, and, in that way, knee extensors and the patellar tendon are maximally loaded.9 That could cause the patellar tendon rupture10 because of the high stress applied, but it could also cause ACL tear because of the anterior translation of the upper tibia which resulted from the quadriceps contraction.11 In the first scenario described, patellar tendon rupture ‘releases’ the upper tibia thus making the anterior translation more intense and as a result causes the ACL tear. In the second scenario, ACL fails first and the anterior translation of the tibia tuberosity makes the stress on the patellar tendon even higher causing the rupture. Both scenarios are in accordance with the mechanism of injury of our patient and with the fact that he felt two consecutive ‘pop’ that represent the patellar tendon and ACL tear. Nevertheless, this issue needs to be further investigated with biomechanical studies which will reveal the behaviour of these structures in quadriceps overload.
Concomitant injuries of MCL and medial and lateral meniscus are frequent.2–8 In our case, we encountered an additional chondral defect of medial femoral condyle. These injuries could be the result of valgus stress and rotation of tibia during knee injury.
Another common feature of this combined injury is the high incidence of missing the clinical diagnosis of either the patellar tendon or the ACL tear.2–8 We failed to recognise the ACL tear preoperatively because of the intense knee pain and swelling that obstructed a thorough physical examination. Patellar tendon tear is a clinical emergency, and we proceeded in operative treatment without further investigation. Nevertheless, MRI is a valuable diagnostic tool which could be helpful in detecting ACL tear preoperatively.
Patellar tendon repair and ACL reconstruction was the treatment of choice in most cases. However, whether to proceed in one- or two-stage procedure has not been established yet. There is an agreement that immediate repair of the patellar tendon should be performed in order to avoid quadriceps muscle atrophy and contraction and scar formation.2–8 10 Nevertheless, timing of ACL reconstruction is still a matter of debate in this combined injury. Some patients underwent acute patellar tendon repair and delayed ACL reconstruction, whereas concomitant acute ACL reconstruction and patellar tendon repair was performed in other patients. The main disadvantage of the one-stage procedure is the potential knee motion deficit postoperatively. However, the one-stage procedure offers the benefit of saving time because of the parallel healing of both injuries. Satisfactory results were recently reported with the one-stage procedure.5 8 Nevertheless, both cases were complicated by arthrofibrosis which required arthroscopic lysis of the adhesions.5 8
The aetiology of motion loss is multifactorial, involving a combination of mechanical and biologic factors. Major risk factors include, among others, injury severity, timing of surgery and prolonged immobilisation.12 Most authors recommend a period of 6-week immobilisation in extension after patellar tendon repair. As a result, the only modifiable risk factor for arthrofibrosis is timing of surgery. Keeping that in mind, injury severity is of paramount importance in electing the one- or two-stage surgical treatment. It has been reported that the magnitude of soft tissue and bony injury associated with ligament injury is directly related to the pathogenesis of motion loss, whereas additional trauma to the capsule may cause an elevated fibrotic response.12 In our case, additional injury to the medial retinaculum and capsule was encountered. This structure plays a role in unloading the patellar tendon by resisting tensile forces created by the extensor mechanism.13 As a result, the ruptured medial retinaculum makes the arthroscopic procedure impossible, due to fluid extravasation, and signifies the severity of the injury. The importance of retinaculum integrity in the treatment of combined ACL and patella tendon tear has not been discussed in the literature so far. In our opinion, the retinaculum disruption is a major contributor to the diffuse swelling of the knee and should discourage surgeons in performing the one-stage operative treatment in this combined injury. Obviously, only prospective, randomised studies comparing the one- and two-stage surgical treatment would reveal the best approach in avoiding arthrofibrosis and obtaining satisfactory results. Nevertheless, patellar tendon and ACL tear is a rare injury and, consequently, is almost impossible to organise such a study. As a result, case reports like ours contribute to a better understanding and treatment of this injury.
In conclusion, this complex injury requires a high suspicion index and should be treated with caution in order to obtain a correct diagnosis and satisfactory outcome.
Learning points.
-
▶
Patellar tendon and ACL tear is a complex injury and part of the diagnosis could be initially missed.
-
▶
Mechanism of injury involves powerful contraction of quadriceps, and the patient may feel two consecutive ‘pop’ representing the disruption of patellar tendon and ACL.
-
▶
Injury severity is very important in deciding the one or two-stage surgical treatment.
-
▶
The ruptured medial retinaculum makes the arthroscopic procedure impossible, due to fluid extravasation, and signifies the severity of the injury.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Papastergiou SG, Koukoulias NE, Ziogas E, et al. Spontaneous, bilateral, quadriceps tendon rupture caused by local exposure to methidathion. BMJ Case Reports 2009;(In Press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baker BE. O’Donoghue’s triad plus patellar tendon rupture. N Y State J Med 1980;80:1436–7. [PubMed] [Google Scholar]
- 3.Rae PJ, Davies DR. Simultaneous rupture of the ligamentum patellae, medial collateral, and anterior cruciate ligaments. A case report. Am J Sports Med 1991;19:529–30. [DOI] [PubMed] [Google Scholar]
- 4.Levakos Y, Sherman MF, Shelbourne KD, et al. Simultaneous rupture of the anterior cruciate ligament and the patellar tendon. Six case reports. Am J Sports Med 1996;24:498–503. [DOI] [PubMed] [Google Scholar]
- 5.Chiang AS, Shin SS, Jazrawi LM, et al. Simultaneous ipsilateral ruptures of the anterior cruciate ligament and patellar tendon: a case report. Bull Hosp Jt Dis 2005;62:134–6. [PubMed] [Google Scholar]
- 6.Costa-Paz M, Muscolo DL, Makino A, et al. Simultaneous acute rupture of the patellar tendon and the anterior cruciate ligament. Arthroscopy 2005;21:1143. [DOI] [PubMed] [Google Scholar]
- 7.Chow FY, Wun YC, Chow YY. Simultaneous rupture of the patellar tendon and the anterior cruciate ligament: a case report and literature review. Knee Surg Sports Traumatol Arthrosc 2006;14:1017–20. [DOI] [PubMed] [Google Scholar]
- 8.Futch LA, Garth WP, Folsom GJ, et al. Acute rupture of the anterior cruciate ligament and patellar tendon in a collegiate athlete. Arthroscopy 2007;23:112, e1–4. [DOI] [PubMed] [Google Scholar]
- 9.Zwerver J, Bredeweg SW, Hof AL. Biomechanical analysis of the single-leg decline squat. Br J Sports Med 2007;41:264–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matava MJ. Patellar Tendon Ruptures. J Am Acad Orthop Surg 1996;4:287–96. [DOI] [PubMed] [Google Scholar]
- 11.Torzilli PA, Deng X, Warren RF. The effect of joint-compressive load and quadriceps muscle force on knee motion in the intact and anterior cruciate ligament-sectioned knee. Am J Sports Med 1994;22:105–12. [DOI] [PubMed] [Google Scholar]
- 12.Magit D, Wolff A, Sutton K, et al. Arthrofibrosis of the knee. J Am Acad Orthop Surg 2007;15:682–94. [DOI] [PubMed] [Google Scholar]
- 13.Powers CM, Chen YJ, Farrokhi S, et al. Role of peripatellar retinaculum in transmission of forces within the extensor mechanism. J Bone Joint Surg Am 2006;88:2042–8. [DOI] [PubMed] [Google Scholar]



