Description
Posterior reversible encephalopathy (PRES) is a clinical-radiological syndrome characterised by brain symmetric lesions of vasogenic oedema, in white matter, basal ganglia or cerebral cortex, preferentially in posterior topography.1 Typical manifestations are headache and altered mental status. Epileptic seizures are also frequent, although status epilepticus (SE) is a rare occurrence.2 Chemotherapy may trigger PRES. Nevertheless, no single chemotherapy agent was consistently implicated.2
Two cases are presented: a young man (patient 1) with a Hodgkin lymphoma, under ABVD chemotherapy (adriamicin, vinblastine, bleomicine, dacarbazin), and an adult woman (patient 2), under docetaxel and gemcitabine treatment due to a femoral sarcoma. Both patients were admitted with a non-convulsive SE. Brain resonance MRI depicted bilateral, predominantly parietal-occipital lesions, hyperintense on T2/ fluid attenuated inversion recovery and with no water restriction on diffusion-weighted MRI/apparent diffusion coefficient maps, consistent with vasogenic oedema (figure 1); patient 2 also presented intracranial vasospasm on magnetic resonance angiography. Both patients were successfully treated for the SE with antiepileptic drugs plus blood pressure control and nimodipine. The first patient repeated ABVD afterwards without recurrence of PRES. In the second patient, no further chemotherapy regimens were performed due to neoplasm refractoriness. Furthermore, both patients showed complete resolution of cytotoxic oedema on repeated MRI.
Figure 1.
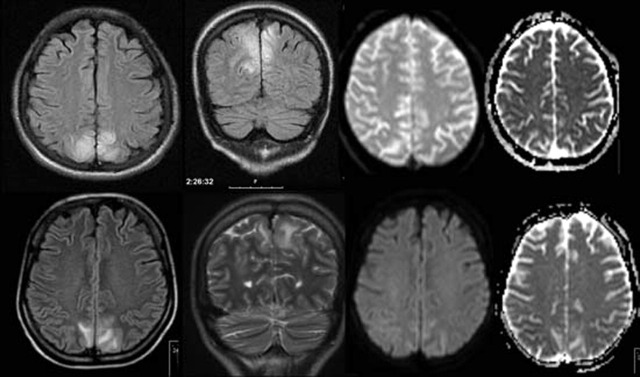
Brain MRI showing posterior hyperintense lesions on FLAIR/T2 sequences and no water restriction on DWI/ADC maps. Upper images form the first patient; bottom images from the second patient.
The association between PRES and platinum, taxanes, vinca alkaloids, biological agents and combination chemotherapy, is increasingly recognised. The exact mechanism of toxicity remains unknown. Vasospasm and loss of cerebrovascular auto-regulation, with the development of vasogenic oedema is a hypothesis. If PRES is left untreated, cytotoxic oedema and permanent neurological deficit may occur,2 hence the need for an early recognition is required.
Acknowledgments
The authors acknowledge Dr Bruno Miranda, Dr Rita Peralta and Dr Carla Bentes.
Footnotes
Competing interests: None.
Patient consent: Not obtained.
References
- 1.Hinchey J, Chaves C, Appignani B, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med 1996;334:494–500. [DOI] [PubMed] [Google Scholar]
- 2.Bhatt A, Farooq MU, Majid A, et al. Chemotherapy-related posterior reversible leukoencephalopathy syndrome. Nat Clin Pract Neurol 2009;5:163–9. [DOI] [PubMed] [Google Scholar]


