Abstract
Background
Infant mortality rates (IMRs) are disproportionally high in the U.S. South; however, the proximate contributors that could inform regional action remain unclear.
Purpose
To quantify the components of excess infant mortality in the U.S. South by maternal race/ethnicity, underlying cause of death, and gestational age.
Methods
U.S. Period Linked Birth/Infant Death Data Files 2007–2009 (analyzed in 2013) were used to compare IMRs between the South (U.S. Public Health Regions IV and VI) and all other regions combined.
Results
Compared to other regions, there were 1.18 excess infant deaths per 1000 live births in the South, representing about 1600 excess infant deaths annually. New Mexico and Texas did not have elevated IMRs relative to other regions; excess death rates among other states ranged from 0.62 per 1000 in Kentucky to 3.82 per 1000 in Mississippi. Racial/ethnic compositional differences, generally the greater proportion of non-Hispanic black births in the South, explained 59% of the overall regional difference; the remainder was mostly explained by higher IMRs among non-Hispanic whites. The leading causes of excess Southern infant mortality were sudden unexpected infant death (SUID; 36%, range=12% in Florida to 90% in Kentucky) and preterm-related death (22%, range=−71% in Kentucky to 51% in North Carolina). Higher rates of preterm birth, predominantly <34 weeks, accounted for most of the preterm contribution.
Conclusions
To reduce excess Southern infant mortality, comprehensive strategies addressing SUID and preterm birth prevention for both non-Hispanic black and white births are needed, with state-level findings used to tailor state-specific efforts.
Introduction
Infant mortality is a sentinel population health metric, reflecting the cumulative health experience of women, families, and communities, and is a leading health indicator for Healthy People 2020.1 The U.S. infant mortality rate (IMR) currently ranks 27th among industrialized countries,2 with wide and persistent disparities by race, socioeconomic status, and geography.3–6 These factors collide in many Southern states, where infant mortality and several other population health indicators are among the poorest in the nation.3,7–11
Ecological studies suggest that common demographic and economic variables cannot entirely explain the Southern infant mortality disadvantage.7,10,12 Socioeconomic, political, cultural, and environmental factors likely undergird this regional health disparity, but the proximate contributors that could inform preventive action have not been recently examined.
An epidemiologic evaluation of regional IMR differences in 1980 found that 72% of excess infant mortality in the South was due to the greater proportion of black births, reflecting a persistent racial disparity.13 The remainder of the Southern excess was due to higher IMRs among white infants, which occurred in both neonatal and postneonatal periods and across various underlying causes of death. However, there have been marked changes in infant mortality over the last 3 decades, and state-specific differences within regions were not examined.
New knowledge and tools to promote infant health, such as improving women's access to health care prior to conception,14 preventing elective deliveries before 39 weeks of gestation,15,16 and reducing sleep-related risk factors for sudden unexpected infant death (SUID),17,18 underscore the importance of an updated data-based investigation to support programmatic initiatives, including a new public–private collaborative improvement and innovation network (CoIIN) to reduce infant mortality in the Southern U.S. (Public Health Regions IV and VI) in which states share best practices along common priority areas and monitor progress through the science of quality improvement and collaborative learning.19
To aid infant mortality prevention efforts in the South, this analysis provides a more current quantification of the components of excess infant mortality that could inform the selection of regionwide and state-specific prevention strategies. Specifically, excess infant mortality in the region and individual states relative to the rest of the country was examined by race/ethnicity, cause of death, and gestational age at birth.
Methods
Data are from the most recent National Center for Health Statistics (NCHS) Period Linked Birth/Infant Death Files 2007–20096,20,21 with state-level identifiers requested through the National Association of Public Health Statistics and Information Systems.22 These files contain birth certificate information on all births that occur in a calendar year (denominator) plus death certificate information linked to the birth certificate for all deaths that occur in the same calendar year (numerator). Between 2007 and 2009, more than 98% of all infant death certificates were linked to their corresponding birth certificate, with weights used to account for unlinked deaths by state of occurrence. Analyses were conducted in 2013.
Key Variables
To be relevant to the CoIIN which represents the most recent Southern infant mortality prevention effort, U.S. Public Health Regions IV (Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, and Tennessee) and VI (Arkansas, Louisiana, New Mexico, Oklahoma, and Texas) formed the definition of the South for this analysis and are referred to interchangeably as Regions IV/VI and the South. All other Public Health Regions are referred to as the rest of the country or other regions.
Underlying cause of death (ICD-10 codes) were grouped into the following summary categories: preterm-related,6,23 other perinatal conditions, congenital anomalies, SUID, injury, infection, and all other causes (see footnote in Table 3 for codes). The definition of preterm-related death follows the classification developed and used by the CDC, which considers only specific causes that are a direct consequence of prematurity.6,23
Therefore, it is a conservative definition that does not include nonspecific causes of death with a high percentage of preterm deaths (e.g., other perinatal conditions) and causes in which prematurity may contribute indirectly (e.g., SUID or general infections).6,23 The SUID category includes sudden infant death syndrome (SIDS); unknown cause; and accidental suffocation and strangulation in bed, owing to evidence of inconsistent reporting practices among these sleep-related codes.24
Gestational age was determined from the last menstrual period (LMP) estimate, with substitution by the clinical/obstetric estimate when the two estimates differed by more than 2 weeks. This practice has been shown to correct implausible birth weight for gestational age distributions that occur on the basis of LMP alone.25,26 Gestational age analyses were restricted to births within a consistent range of 20–44 weeks.
Maternal race/ethnicity was classified into five groups based on Hispanic ethnicity and unified race categories, with multiple races bridged to a single race: non-Hispanic white, non-Hispanic black, Hispanic, non-Hispanic American Indian/Alaska Native, and non-Hispanic Asian/Pacific Islander.21
Other relevant variables (i.e., maternal education, prenatal care, or smoking) could not be reliably examined across all states given the inconsistency in data collection items between the two different versions of the birth certificate in use (1989 and 2003 revision).21 As of January 1, 2007, five states in Regions IV/VI (Florida, Kentucky, South Carolina, Tennessee, and Texas) had implemented the 2003 revision to the birth certificate.27
Analytic Methods
Infant mortality rates per 1000 live births were examined for each Southern state and the region overall, and compared to a combined rate for all other regions using simple differences. Because overall state and regional comparisons are heavily influenced by differences in racial/ethnic composition, excess infant mortality in Southern states was partitioned into differences in the racial/ethnic composition of births versus racial/ethnic-specific rates using the Kitagawa method.
The Kitagawa method multiplies the difference in the proportion of births in a factor-specific category (e.g., race/ethnicity or gestational age) between a given population and a reference (e.g., Southern states versus other regions) by the average factor-specific mortality rate to determine the distributional component.28–30 Similarly, the rate component is determined by multiplying the difference in factor-specific rates by the average distribution.
Excess infant mortality for each state and the regional total compared to other regions was then examined with respect to cause of death and gestational age. Differences in cause-specific IMRs (sum-to-total IMR differences) were apportioned as attributable fractions of excess infant mortality. To evaluate component contributions of preterm birth (PTB) due to greater rates of PTB- versus gestational age–specific mortality rates that may reflect variation in access to risk-appropriate neonatal care, a Kitagawa analysis was conducted to partition the overall difference in infant mortality between each Southern state and other regions combined into distributional differences in gestational age categories versus gestational age–specific IMRs.
In contrast to preterm-related causes of death, the overall preterm contribution revealed by Kitagawa analysis may be overstated (versus understated) given the inclusion of deaths due to congenital anomalies, often in premature infants. These analyses were conducted both overall and for non-Hispanic whites and blacks, given the geographic differences in race-specific components.
Results
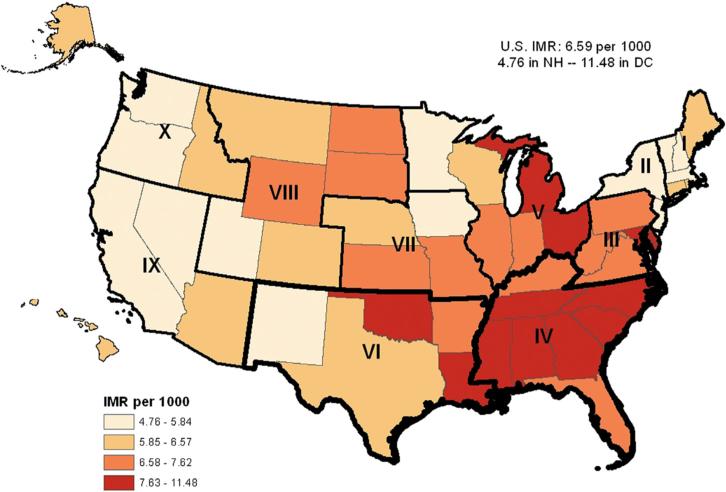
The overall U.S. IMR for 2007–2009 was 6.59 per 1000 live births. The majority (8 of 12) U.S. states with IMRs in the upper quartile (7.63–11.48) were located in Regions IV and VI (Figure 1). Overall, Regions IV/VI had 1.18 excess deaths per 1000 live births compared to all other regions, translating to 5018 excess infant deaths (16% of the total Region IV/VI infant deaths) between 2007 and 2009 (Table 1). Only New Mexico and Texas did not have elevated IMRs among Region IV/VI states, with a remaining range of 0.62 excess deaths per 1000 live births in Kentucky to 3.82 excess deaths per 1000 live births in Mississippi relative to other regions.
Figure 1.
Infant mortality rate (IMR) by state, 2007–2009
Table 1.
Infant mortality rates by race/ethnicity in Region IV/VI states compared to other regions, 2007–2009
| Region IV states |
Region VI states |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Other regions |
Alabama | Florida | Georgia | Kentucky | Mississippi | North Carolina |
South Carolina |
Tennessee | Arkansas | Louisiana | New Mexico |
Oklahoma | Texas | Regions IV/ VI Total |
|
| Births | 8,444,532 | 191,825 | 692,004 | 439,117 | 175,295 | 134,339 | 388,721 | 186,566 | 254,482 | 121,855 | 196,544 | 89,789 | 164,399 | 1,215,156 | 4,250,092 |
| Deaths | 52,298 | 1,772 | 4,905 | 3,417 | 1,194 | 1,345 | 3,200 | 1,467 | 2,075 | 925 | 1,771 | 510 | 1,288 | 7,470 | 31,339 |
| IMR per 1000 | 6.19 | 9.24 | 7.09 | 7.78 | 6.81 | 10.01 | 8.23 | 7.86 | 8.15 | 7.59 | 9.01 | 5.69 | 7.83 | 6.15 | 7.37 |
| Excess death rate compared to other regions | 3.05 | 0.90 | 1.59 | 0.62 | 3.82 | 2.04 | 1.67 | 1.96 | 1.40 | 2.82 | −0.51 | 1.64 | −0.05 | 1.18 | |
| Racial/ethnic birth composition (%) | |||||||||||||||
| Non-Hispanic white | 56.5 | 59.2 | 45.5 | 45.1 | 83.9 | 50.0 | 55.4 | 55.7 | 67.5 | 67.5 | 53.5 | 28.4 | 64.1 | 34.4 | 48.7 |
| Non-Hispanic black | 11.5 | 30.7 | 22.4 | 33.5 | 9.3 | 44.6 | 23.7 | 32.7 | 21.0 | 19.5 | 38.9 | 1.7 | 9.1 | 11.4 | 21.1 |
| Hispanic | 23.8 | 8.3 | 28.8 | 17.5 | 5.1 | 3.7 | 16.5 | 9.7 | 9.4 | 10.8 | 5.1 | 56.1 | 13.1 | 50.2 | 26.3 |
| Non-Hispanic AIAN | 1.0 | 0.3 | 0.2 | 0.1 | 0.1 | 0.7 | 1.4 | 0.3 | 0.1 | 0.6 | 0.7 | 12.2 | 11.4 | 0.2 | 1.0 |
| Non-Hispanic API | 7.1 | 1.5 | 3.1 | 3.7 | 1.6 | 1.1 | 3.1 | 1.7 | 2.0 | 1.7 | 1.8 | 1.6 | 2.3 | 3.9 | 2.9 |
| Racial/ethnic-specific IMR | |||||||||||||||
| Non-Hispanic white | 5.23 | 7.53 | 5.48 | 5.71 | 6.51 | 7.23 | 5.98 | 5.88 | 6.38 | 6.60 | 6.89 | 5.83 | 7.16 | 5.47 | 6.10 |
| Non-Hispanic black | 12.77 | 13.33 | 12.74 | 12.31 | 11.15 | 13.38 | 14.67 | 12.14 | 14.90 | 12.59 | 12.76 | 11.97 | 14.74 | 11.41 | 12.84 |
| Hispanic | 5.43 | 7.30 | 5.30 | 4.95 | 4.49 | 6.25 | 6.34 | 5.51 | 6.48 | 5.11 | 3.84 | 5.31 | 6.07 | 5.56 | 5.54 |
| Non-Hispanic AIAN | 9.23 | – a | – a | – a | – a | 19.48 | 15.52 | – a | – a | – a | – a | 6.14 | 8.79 | 7.90 | 8.77 |
| Non-Hispanic API | 4.40 | 4.95 | 5.39 | 3.85 | 4.03 | – a | 5.58 | 3.77 | 4.52 | – a | 5.42 | – a | 4.40 | 4.16 | 4.55 |
| Non-Hispanic black–white disparity | |||||||||||||||
| Rate difference | 7.54 | 5.79 | 7.26 | 6.60 | 4.64 | 6.15 | 8.69 | 6.26 | 8.52 | 5.98 | 5.87 | 6.14 | 7.58 | 5.95 | 6.74 |
| Rate ratio | 2.44 | 1.77 | 2.33 | 2.16 | 1.71 | 1.85 | 2.45 | 2.06 | 2.33 | 1.91 | 1.85 | 2.05 | 2.06 | 2.09 | 2.11 |
| Excess infant mortality components by race/ethnicityb | |||||||||||||||
| % due to racial/ethnic composition | 44 | 89 | 98 | 17 | 61 | 49 | 87 | 40 | 47 | 75 | N/A | 14 | N/A | 59 | |
| % due to higher non-Hispanic white IMR | 43 | 14 | 15 | 134 | 27 | 20 | 21 | 36 | 58 | 32 | N/A | 68 | N/A | 37 | |
| % due to higher non-Hispanic black IMR | 4 | 0 | –6 | –25 | 4 | 16 | –8 | 17 | –2 | 0 | N/A | 12 | N/A | 1 | |
| % due to higher other race/ethnicity IMRs | 9 | –2 | –7 | –26 | 7 | 15 | 0 | 7 | –4 | –7 | N/A | 5 | N/A | 2 | |
Note: Boldface indicates that a rate is significantly different from other regions, p < 0.05.
n < 10, not reportable
Calculated by the Kitagawa method, where differences in racial/ethnic-specific proportions between each state and other regions are multiplied by the average racial/ethnic-specific rate, and differences in racial/ethnic-specific rates between each state and other regions are multiplied by the average racial/ethnic-specific proportion; composition and rate components sum to the overall state excess in infant mortality. Percentages greater than 100 indicate that the state/region IMR would be lower than that of other regions if that factor were equalized. Negative percentages indicate that the excess IMR compared to other regions would increase if that factor were equalized (i.e., the factor favors the state/region)
AIAN, American Indian/Alaska Native; API, Asian/Pacific Islander; IMR, infant mortality rate; N/A, not applicable (no significant excess in infant mortality)
Racial/Ethnic Composition and Infant Mortality Rates
Compared to other regions, non-Hispanic black births accounted for a larger share of all births in Region IV/VI states (21.1% vs 11.5%; Table 1). Owing to substantial racial/ethnic IMR disparities, most notably the black–white gap, racial/ethnic compositional differences including the larger proportion of non-Hispanic black births explained 59% of the regional disparity compared to the rest of the country, and much of the remainder (37%) was explained by higher IMRs among non-Hispanic white infants (6.10 vs 5.23 per 1000 live births). The non-Hispanic black IMR was not greatly elevated in Regions IV/VI compared to the rest of the country and explained only 1% of the regional difference.
Owing in large part to variation in racial/ethnic composition across Southern states, there was great variability in the contribution of racial/ethnic composition versus racial/ethnic-specific IMRs to excess infant deaths. For example, the majority of excess infant mortality was due to higher mortality rates among non-Hispanic white infants in Kentucky (134%) and Oklahoma (68%).
Conversely, a majority of excess infant mortality in Florida (89%); Georgia (98%); Mississippi (61%); South Carolina (87%); and Louisiana (75%) could be explained by compositional differences because of a larger proportion of non-Hispanic black births. North Carolina, Tennessee, and Oklahoma were the only states with significantly higher black IMRs, which accounted for more than 10% of their excess infant mortality compared to other regions (see Appendix Figures for race-specific maps).
Cause of Death
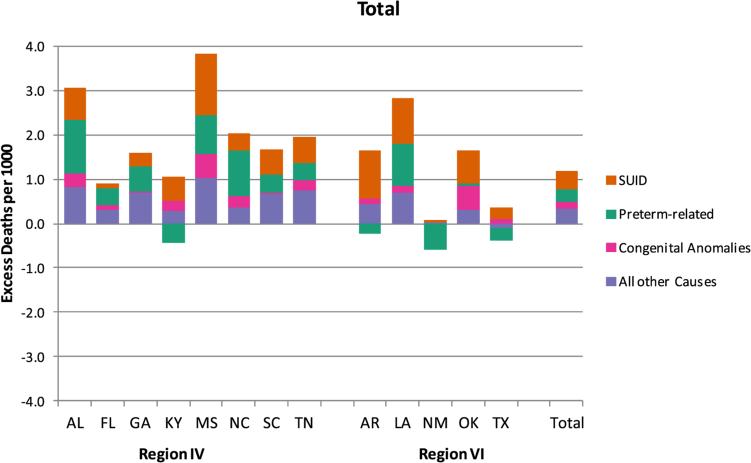
Overall, prematurity, congenital anomalies, and SUID were the three leading causes of death in the South and the rest of the U.S. (Appendix Table 1). However, SUID and preterm-related death were the largest causes of excess infant mortality in the South compared to other regions, accounting for 36% and 22% of all excess deaths, respectively, followed by congenital anomalies (14%, Figure 2, Appendix Table 1).
Figure 2.
Cause-specific excess infant mortality rates in Region IV/VI states compared to other regions, 2007–2009
SUID accounted for the overwhelming majority of excess deaths in Kentucky (90%) and Arkansas (76%) and was the leading cause of excess death in five other states (Mississippi, Tennessee, South Carolina, Louisiana, and Oklahoma); preterm-related death was the leading overall excess cause in four states (Alabama, Florida, Georgia, and North Carolina).
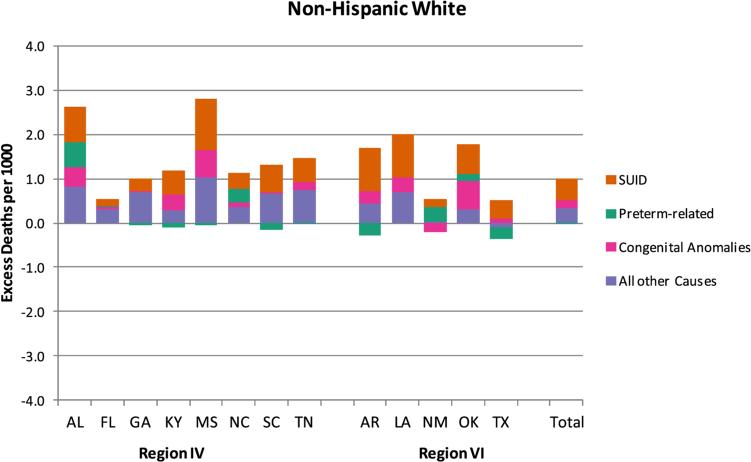
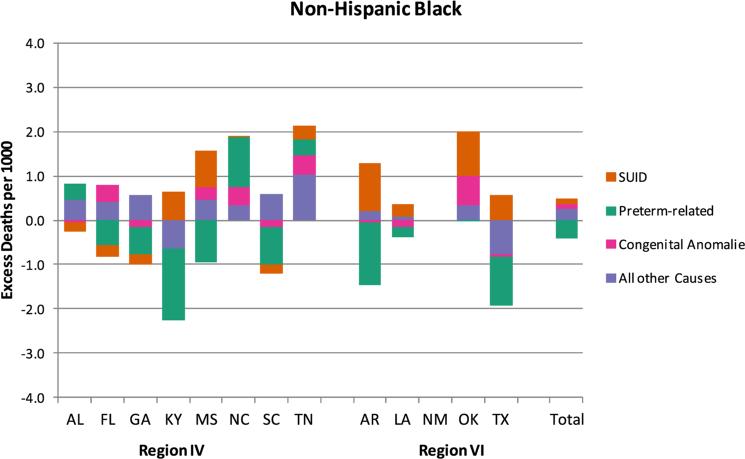
Among non-Hispanic whites, SUID was the leading cause of excess infant death in every Region IV/VI state, followed by congenital anomalies in seven states (Kentucky, Mississippi, Tennessee, Arkansas, Louisiana, Oklahoma, and Texas; Figure 3, Appendix Table 1). Among non-Hispanic blacks, preterm-related causes or other perinatal conditions were the leading contributors to excess infant death in North Carolina and Tennessee whereas SUID was the leading contributor in Oklahoma (Figure 4, Appendix Table 1).
Figure 3.
Cause-specific excess infant mortality rates in Region IV/VI states compared to other regions among non-Hispanic whites, 2007–2009
Figure 4.
Cause-specific excess infant mortality rates in Region IV/VI states compared to other regions among non-Hispanic blacks, 2007–2009
Several states had significantly higher non-Hispanic black SUID rates (Mississippi, Arkansas, and Texas), despite not having an overall excess black IMR. Preterm-related death and SUID were the leading causes of the black–white disparity in the South, similar to the rest of the country (data not shown).
Gestational Age–Specific Distribution and Infant Mortality Rates
The PTB rate was about 20% higher in Regions IV/VI than in other regions (12.2% vs 10.2%; Appendix Table 2) and was highest in Alabama, Mississippi, and Louisiana. The proportion of infants born at early term (37–38 weeks) was also elevated in the South. Overall, the higher PTB rate, particularly early PTB (<34 weeks), accounted for 51% of the excess infant mortality in Regions IV/VI. The excess early term delivery rate explained only 8% of excess infant mortality overall, but as much as 18% in Kentucky.
Higher gestational age–specific mortality rates among preterm infants generally explained less than 10% of excess infant mortality except for Mississippi (14%); North Carolina (18%); Tennessee (16%); and Oklahoma (24%). Consistent with the cause-of-death results, gestational age differences reflecting higher PTB rates were a greater source of the regional disparity among non-Hispanic blacks than that among non-Hispanic whites, but with considerable state-to-state variability.
Discussion
According to the most recently available data, an extra 1.2 infants per 1000 live births die in the South compared to other regions—a disadvantage resulting in more than 1600 excess infant deaths annually. Similar to findings reported nearly 30 years ago,13 a large portion of excess infant mortality in the South can be explained by a higher proportion of non-Hispanic black births (59%), with the remainder generally due to higher IMRs among non-Hispanic whites.
Thus, prevention efforts in the South should focus on reducing mortality among black infants, due to a persistent disparity that exists across the nation, as well as on reducing the higher white IMR. The higher IMRs for whites, but not for blacks, in the South relative to the rest of the country may reflect the greater concentration of poverty among whites in the South; poverty among blacks is high in many regions.31
Improved cause-of-death categories that collapse across codes related to SUID and prematurity showed that these were the largest causes of excess infant death in the South, accounting for 36% and 22% of excess deaths, respectively, followed by congenital anomalies (14%). SUID is a major component of the black–white disparity and accounted for more than half of all non-Hispanic white excess infant deaths, with congenital anomalies contributing 22%.
The prematurity-related contribution to regional differences was largely a product of the racial disparity, as these causes of death were not a major source of excess for non-Hispanic whites. The majority of the PTB contribution was due to excess rates of PTB, particularly births occurring before 34 weeks. Higher levels of gestational age–specific mortality among preterm infants, which may reflect poorer levels of perinatal regionalization and access to risk-appropriate care,32 explained less than 10% of excess infant mortality.
The overall regional pattern of the South masked considerable state variability, with implications for the selection of state-specific infant mortality strategies. For example, the majority of excess infant deaths in Kentucky and Oklahoma were due to higher non-Hispanic white IMRs. Disparities played a key role in most states, generally due to a greater proportion of non-Hispanic black births.
However, North Carolina, Tennessee, and Oklahoma also had higher non-Hispanic black IMRs than other regions. Several states also had higher IMRs for Hispanic and American Indian/Alaska Native infants that should not be overlooked. Although SUID was among the top two causes of excess infant death for every Southern state, it accounted for about half or more of excess deaths in Kentucky, Arkansas, and Oklahoma. Several states had higher IMRs among preterm infants that accounted for 15%–25% of excess infant deaths, suggesting the need for improved perinatal regionalization.
These state-level similarities and differences highlight the importance of a data-driven approach to facilitate regional and state-specific prevention strategies. Establishment of data systems to identify needs and program priorities, including the Pregnancy Risk Assessment and Monitoring System (PRAMS), Fetal and Infant Mortality Review programs, and the Region IV Network for Data Management Utilization, was a major success of the Southern Infant Mortality Task Force coordinated by the Southern Legislative Conference and Southern Governors’ Association between 1984 and 1997.33,34 These data systems can be coupled with new practice and policy approaches to successfully address the primary causes of excess infant mortality in the Southern region: SUID and congenital anomalies among non-Hispanic white infants and the black–white disparity in both SUID and PTB rates.
To more effectively address and reduce SUID and SUID disparities, newly expanded guidelines from the American Academy of Pediatrics emphasize the importance of safe sleep environments beyond supine positioning (e.g., room sharing but not bed sharing and avoidance of soft bedding) and recommend additional protective practices (e.g., breastfeeding and avoiding exposure to tobacco smoke and other drugs).17
Pregnancy Risk Assessment and Monitoring System analyses and data from a new CDC-sponsored SUID case registry program, in which Georgia, Louisiana, and New Mexico have participated,35 can be used to identify race-specific and state-level risk and protective factors that can be targeted for intervention. The newly launched Safe to Sleep campaign includes culturally appropriate outreach materials.36
Additionally, the SUID/SIDS Resource Center provides technical assistance to states in identifying and implementing best practices, such as provider training, legislation, and crib distribution.37 These resources are now informing the work of a Region IV/VI CoIIN priority area focused on improving safe sleep practices.
To reduce prematurity and racial/ethnic disparities in birth outcomes, there is a growing emphasis on promoting healthy behaviors and preventing chronic conditions prior to pregnancy in a life-course approach from childhood to adulthood.38,39 A focus on preconception health may also help to reduce congenital anomalies through the prevention and management of diabetes and obesity,14 both of which have been shown to be higher in the South.40 Although primary prevention of a first adverse outcome would be ideal, expanding interconception care through Medicaid for women who have had a previous poor birth outcome represents an important strategy adopted by the CoIIN.
Additional CoIIN strategies that may help to reduce prematurity or morbidity and mortality among premature infants include promoting prenatal smoking cessation, strengthening perinatal regionalization, and reducing early elective deliveries (<39 weeks) both through public and provider education, such as the March of Dimes’ Healthy Babies Are Worth the Wait program41 as well as policy changes at the hospital and financing levels.15,16
Although not a CoIIN strategy, many states are also working to promote access and utilization of progesterone therapy for preterm birth prevention among women who have had a previous spontaneous PTB, which may have a larger impact in reducing the early PTBs42,43 that have highest risk of morbidity and mortality.
Limitations of this study include the data delay for the national linked file, which fails to incorporate the impact of more recent efforts, as well as the limited information on the birth/death certificates and inability to examine new or revised items (e.g., insurance, education, smoking, or pre-pregnancy BMI). However, these factors could be examined in the future—all states are expected to use the 2003 birth certificate revision by 2014.44
Finally, state-level comparisons may be significantly affected by reporting differences in live births less than 500 g.45 Mortality rates among births less than 500 g were actually lower in the South compared to other regions, suggesting a potentially selective under-registration of Southern infant deaths, which would only serve to underestimate IMR disparities, generally, and those related to prematurity, specifically. A sensitivity analysis excluding births less than 500 g weight did not alter the main findings.
Conclusions
To reduce excess Southern infant mortality, comprehensive strategies addressing SUID and PTB for both non-Hispanic black and white births are needed, with state-level findings used to tailor state-specific efforts. These findings can be used to assist regional and state-level planning both within the CoIIN and through other public and private efforts to improve birth outcomes and reduce infant mortality at local and national levels.46–54
Supplementary Material
Acknowledgments
The findings and conclusions in this article are those of the authors and do not necessarily reflect the official position of the Health Resources and Services Administration, CDC, or USDHHS. The authors express gratitude to Lieutenant Commander Deborah Dee, PhD, MPH, CDC colleagues, and anonymous peer reviewers for helpful comments and suggestions to improve the clarity and presentation of results.
Footnotes
No financial disclosures were reported by the authors of this paper.
Appendix
Supplementary data
Supplementary data associated with this article can be found at http://dx.doi.org/10.1016/j.amepre.2013.12.006.
References
- 1.USDHHS Leading health indicators—Healthy People 2020. www.healthypeople.gov/2020/LHI/
- 2.National Center for Health Statistics . Infant mortality rates and international rankings: Organisation for Economic Co-operation and Development (OECD) countries, selected years 1960–2009. Health, U.S., 2012: with special feature on emergency care. NCHS; Hyattsville MD: 2013. [Google Scholar]
- 3.National Center for Health Statistics . Health, U.S., 2011: with special feature on socioeconomic status and health. NCHS; Hyattsville MD: 2012. [PubMed] [Google Scholar]
- 4.Singh GK, Kogan MD. Persistent socioeconomic disparities in infant, neonatal, and postneonatal mortality rates in the U.S., 1969-2001. Pediatrics. 2007;119(4):e928–e939. doi: 10.1542/peds.2005-2181. [DOI] [PubMed] [Google Scholar]
- 5.Wise PH. The anatomy of a disparity in infant mortality. Annu Rev Public Health. 2003;24:341–62. doi: 10.1146/annurev.publhealth.24.100901.140816. [DOI] [PubMed] [Google Scholar]
- 6.Mathews TJ, MacDorman MF. Infant mortality statistics from the 2009 period linked birth/infant death data set. Natl Vital Stat Rep. 2013;61(8) [PubMed] [Google Scholar]
- 7.Goldhagen J, Remo R, Bryant T, 3rd, et al. The health status of southern children: a neglected regional disparity. Pediatrics. 2005;116(6):e746–e753. doi: 10.1542/peds.2005-0366. [DOI] [PubMed] [Google Scholar]
- 8.Heisler EJ. The U.S. infant mortality rate: international comparisons, underlying factors, and federal programs. Congressional Research Service; Washington DC: 2012. [Google Scholar]
- 9.Kaiser Family Foundation State health facts. www.statehealthfacts.org/
- 10.Menifield CE, Dawson J. Infant mortality in southern states: a bureaucratic nightmare. J Health Hum Serv Adm. 2008;31(3):385–402. [PubMed] [Google Scholar]
- 11.National Center for Health Statistics Health indicators warehouse. healthindicators.gov/
- 12.Paul DA, Mackley A, Locke RG, Stefano JL, Kroelinger C. State infant mortality: an ecologic study to determine modifiable risks and adjusted infant mortality rates. Matern Child Health J. 2009;13(3):343–8. doi: 10.1007/s10995-008-0358-9. [DOI] [PubMed] [Google Scholar]
- 13.Allen DM, Buehler JW, Hogue CJ, Strauss LT, Smith JC. Regional differences in birth weight-specific infant mortality, U.S., 1980. Public Health Rep. 1987;102(2):138–45. [PMC free article] [PubMed] [Google Scholar]
- 14.Johnson K, Posner SF, Biermann J, et al. Recommendations to improve preconception health and health care—U.S. A report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR Recomm Rep. 2006;55(RR–6):1–23. [PubMed] [Google Scholar]
- 15.Main E, Oshiro BT, Chagolla B, Bingham D, Dang-Kilduff L, Kowalewski L. Elimination of non-medically indicated (elective) deliveries before 39 weeks gestational age (California Maternal Quality Care Collaborative Toolkit to Transform Maternal Care) 1st ed. www.marchofdimes.com/professionals/medicalresources_39weeks.html.
- 16.Oshiro BT, Kowalewski L, Sappenfield W, et al. A multistate quality improvement program to decrease elective deliveries before 39 weeks of gestation. Obstet Gynecol. 2013;121(5):1025–31. doi: 10.1097/AOG.0b013e31828ca096. [DOI] [PubMed] [Google Scholar]
- 17.American Academy of Pediatrics Policy statement—SIDS and other sleep-related infant deaths: expansion of recommendations for a safe infant sleeping environment. Pediatrics. 2011;128(5):1030–9. doi: 10.1542/peds.2011-2284. [DOI] [PubMed] [Google Scholar]
- 18.American Academy of Pediatrics Technical report—SIDS and other sleep-related infant deaths: expansion of recommendations for a safe infant sleeping environment. Pediatrics. 2011;128(5):e1341–e1367. doi: 10.1542/peds.2011-2285. [DOI] [PubMed] [Google Scholar]
- 19.Maternal and Child Health Bureau Collaborative Improvement and Innovation Network to Reduce Infant Mortality. mchb.hrsa.gov/infa ntmortality/coiin/index.html.
- 20.Mathews TJ, MacDorman MF. Infant mortality statistics from the 2007 period linked birth/infant death data set. Natl Vital Stat Rep 2011. 59(6):1–30. [PubMed] [Google Scholar]
- 21.Mathews TJ, MacDorman MF. Infant mortality statistics from the 2008 period linked birth/infant death data set. Natl Vital Stat Rep. 2012;60(5):49. [PubMed] [Google Scholar]
- 22.National Association for Public Health Statistics Vital statistics research request process. www.naphsis.org/Pages/VitalStatisticsDataResearchRequestProcess.aspx.
- 23.Callaghan WM, MacDorman MF, Rasmussen SA, Qin C, Lackritz EM. The contribution of preterm birth to infant mortality rates in the U.S. Pediatrics. 2006;118(4):1566–73. doi: 10.1542/peds.2006-0860. [DOI] [PubMed] [Google Scholar]
- 24.Shapiro-Mendoza CK, Tomashek KM, Anderson RN, Wingo J. Recent national trends in sudden, unexpected infant deaths: more evidence supporting a change in classification or reporting. Am J Epidemiol. 2006;163(8):762–9. doi: 10.1093/aje/kwj117. [DOI] [PubMed] [Google Scholar]
- 25.Callaghan WM, Dietz PM. Differences in birth weight for gestational age distributions according to the measures used to assign gestational age. Am J Epidemiol. 2010;171(7):826–36. doi: 10.1093/aje/kwp468. [DOI] [PubMed] [Google Scholar]
- 26.Qin C, Dietz PM, England LJ, Martin JA, Callaghan WM. Effects of different data-editing methods on trends in race-specific preterm delivery rates, U.S., 1990-2002. Paediatr Perinat Epidemiol. 2007;21(S2):41–9. doi: 10.1111/j.1365-3016.2007.00860.x. [DOI] [PubMed] [Google Scholar]
- 27.Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2007. Natl Vital Stat Rep. 2010;58(24):1–85. [PubMed] [Google Scholar]
- 28.Kitagawa EM. Components of a difference between two rates. J Am Stat Assoc. 1955;50(272):1168–94. [Google Scholar]
- 29.Sappenfield WM, Peck MG, Gilbert CS, Haynatzka VR, Bryant T., 3rd Perinatal periods of risk: phase 2 analytic methods for further investigating feto-infant mortality. Matern Child Health J. 2010;14(6):851–63. doi: 10.1007/s10995-010-0624-5. [DOI] [PubMed] [Google Scholar]
- 30.Schempf AH, Branum AM, Lukacs SL, Schoendorf KC. The contribution of preterm birth to the Black-White infant mortality gap, 1990 and 2000. Am J Public Health. 2007;97(7):1255–60. doi: 10.2105/AJPH.2006.093708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Macartney S, Bishaw A, Fontenot K. Poverty rates for selected detailed race and Hispanic groups by state and place: 2007–2011. U.S. Census Bureau; Washington DC: 2013. [Google Scholar]
- 32.Lasswell SM, Barfield WD, Rochat RW, Blackmon L. Perinatal regionalization for very low-birth-weight and very preterm infants: a meta-analysis. JAMA. 2010;304(9):992–1000. doi: 10.1001/jama.2010.1226. [DOI] [PubMed] [Google Scholar]
- 33.Hallman YN. The Southern Regional Project on Infant Mortality: a 20-year retrospective. Southern Legislative Conference; Atlanta GA: 2005. [Google Scholar]
- 34.University of North Carolina Region IV Network for Data Management and Utilization: project overview. www.shepscenter.unc.edu/data/rndmu/
- 35.Shapiro-Mendoza CK, Camperlengo LT, Kim SY, Covington T. The sudden unexpected infant death case registry: a method to improve surveillance. Pediatrics. 2012;129(2):e486–e493. doi: 10.1542/peds.2011-0854. [DOI] [PubMed] [Google Scholar]
- 36.National Institute of Child Health & Human Development Safe to Sleep public education campaign. www.nichd.nih.gov/sids/
- 37.National SUID/SIDS Resource Center What works: changing knowledge and behavior to reduce sudden unexpected infant death. www.sidscenter.org/whatworks.html.
- 38.Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Matern Child Health J. 2003;7(1):13–30. doi: 10.1023/a:1022537516969. [DOI] [PubMed] [Google Scholar]
- 39.Lu MC, Kotelchuck M, Hogan V, Jones L, Wright K, Halfon N. Closing the black-white gap in birth outcomes: a life-course approach. Ethn Dis. 2010;20(1S2):S2, S62–S76. [PMC free article] [PubMed] [Google Scholar]
- 40.CDC Estimated county-level prevalence of diabetes and obesity—U.S., 2007. MMWR Morb Mortal Wkly Rep. 2009;58(45):1259–63. [PubMed] [Google Scholar]
- 41.March of dimes Healthy babies are worth the wait. www.marchofdimes.com/professionals/medicalresources_hbww.html. [PubMed]
- 42.Meis PJ, Klebanoff M, Thom E, et al. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348(24):2379–85. doi: 10.1056/NEJMoa035140. [DOI] [PubMed] [Google Scholar]
- 43.Spong CY, Meis PJ, Thom EA, et al. Progesterone for prevention of recurrent preterm birth: impact of gestational age at previous delivery. Am J Obstet Gynecol. 2005;193(3 Pt 2):1127–31. doi: 10.1016/j.ajog.2005.05.077. [DOI] [PubMed] [Google Scholar]
- 44.National Association for Public Health Statistics and Information Systems (NAPHSIS) More, better, faster: strategies for improving the timeliness of vital statistics. NAPHSIS; Silver Spring MD: 2013. [Google Scholar]
- 45.Ehrenthal DB, Wingate MS, Kirby RS. Variation by state in outcomes classification for deliveries less than 500 g in the U.S. Matern Child Health J. 2011;15(1):42–8. doi: 10.1007/s10995-010-0566-y. [DOI] [PubMed] [Google Scholar]
- 46.Association of Maternal and Child Health Programs . Forging a comprehensive initiative to improve birth outcomes and reduce infant mortality: policy and program options for state planning. AMCHP; Washington DC: 2012. [Google Scholar]
- 47.Association of State and Territorial Health Officials Healthy Babies initiative. www.astho.org/healthybabies/
- 48.Berns SD, editor. Toward improving the outcomes of pregnancy III. March of Dimes; White Plains NY: 2010. [Google Scholar]
- 49.Best Babies Zone . www.bestbabieszone.org/ [Google Scholar]
- 50.Centers for Medicaid and Medicare Services Strong Start for Mothers and Newborns. innovation.cms.gov/initiatives/strong-start/index.html.
- 51.CityMatCH Institute for equity in birth outcomes. www.citymatch.org/projects/institute-equity-birth-outcomes-0.
- 52.Health Resources and Services Adminstration About the Secretary's Advisory Committee on Infant Mortality. www.hrsa.gov/advisorycom mittees/mchbadvisory/InfantMortality/About/about.html.
- 53.Johnson K, Floyd RL, Humphrey JR, et al. Action plan for the national initiative on Preconception Health and Health Care. www.cdc.gov/preconception/documents/ActionPlanNationalInitiativePCHHC2012-2014.pdf.
- 54.Maternal and Child Health Bureau Healthy Start. mchb.hrsa.gov/programs/healthystart/index.html.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.