Abstract
IMPORTANCE
Efforts to transform primary care through the medical home model may have limited effectiveness if they do not incorporate families’ preferences for different primary care services.
OBJECTIVE
To assess parents' relative preferences for different categories of enhanced access services in primary care.
DESIGN, SETTING, AND PARTICIPANTS
Internet-based survey that took place with a national online panel from December 8, 2011, to December 22, 2011. Participants included 820 parents of children aged 0 to 17 years. Hispanic and black non-Hispanic parents were each oversampled to 20% of the sample. The survey included a discrete choice experiment with questions that asked parents to choose between hypothetical primary care practices with different levels of enhanced access and other primary care services.
MAIN OUTCOMES AND MEASURES
We estimated parents’ relative preferences for different enhanced access services using travel time to the practice as a trade-off and parents’ marginal willingness to travel in minutes for practices with different levels of services.
RESULTS
The response rate of parents who participated in the study was 41.2%. Parents were most likely to choose primary care offices that guaranteed same-day sick visits (coefficient, 0.57 [SE, 0.05]; P < .001) followed by those with higher professional continuity (coefficient, 0.36 [SE, 0.03]; P < .001). Parents were also significantly more likely to choose practices with 24-hour telephone advice plus nonurgent email advice (0.08 [0.04]; P < .05), evening hours 4 or more times a week (0.14 [0.04]; P < .001), and at least some hours on weekends. Parents were significantly less likely to choose practices that were closed during some weekday daytime hours or had wait times longer than 4 weeks for preventive care visits. There was very little variation in preferences among parents with different sociodemographic characteristics. Parents' marginal willingness to travel was 14 minutes (95% CI, 11–16 minutes) for guaranteed same-day sick visits and 44 minutes (95% CI, 37–51 minutes) for an office with idealized levels of all services.
CONCLUSIONS AND RELEVANCE
As primary care practices for children implement aspects of the medical home model, those that emphasize same-day sick care and professional continuity are more likely to meet parents’ preferences for enhanced access. Practices should seek to engage families in prioritizing changes in practice services as part of medical home implementation.
Enhanced access is a key component of recent efforts to improve primary care for children in the United States, particularly through implementation of the medical home model.1,2 Within the context of medical home implementation, enhanced access services typically include multiple options for communication during and after office hours, same-day sick visits, and extended weekday or weekend office hours.2–4 Enhanced access services are intended to improve the quality and family centeredness of care by providing families with additional options for communicating with primary care professionals, such as through 24-hour telephone services and email, and for getting direct care when needed.
Of the many components of the medical home, changes in enhanced access will likely be among the most apparent and tangible to families. However, implementation of enhanced access services is resource intensive for primary care practices and, as a result, practices typically must prioritize which services they will implement and consider potential trade-offs with services the practice currently provides.5–8 For example, holding a larger percentage of appointments for same-day sick visits might result in fewer appointments for preventive care visits and longer times to the next available appointment for a preventive care visit.
There is a small but growing body of evidence that patients’ preferences for the characteristics of health care services can significantly influence the use of current services and uptake of new services.9–12 If patient and family preferences are not considered when setting priorities for changes to existing services or implementing new services in the medical home, there is a significant risk that families may be dissatisfied with changes, new services will be underused, or the investment of resources will be inefficient or ineffective in improving care.
The objective of this study was to assess parents’ relative preferences for different attributes of enhanced access services in their child’s primary care practice and their willingness to make trade-offs with other aspects of primary care to have enhanced access services. Based on prior qualitative work, we hypothesized that parents would have the strongest preferences for the availability of telephone advice 24hours a day and same-day sick visits and would be willing to make some trade-offs with other aspects of care such as continuity and scheduling wait times for the next available preventive care visit.13
Methods
Sample and Study Design
We conducted an Internet-based survey of a national sample of 820 parents in the United States from December 8, 2011, to December 22, 2011. Participants were sampled from a nationally representative online panel of individuals maintained by Knowledge Networks, a survey research firm.14 This standing online panel is maintained through address-based sampling similar to the US Census. As part of the panel, households are provided free computer hardware and Internet access if they do not have these at the time of recruitment.
For this survey, we sampled parents (≥18 years) from the standing online panel with children between the ages of 0 and 17 years in the household. We oversampled Hispanic and black non-Hispanic parents to approximately 20% of the sample each to provide statistical power for cross-group comparisons. Parents reported demographic information for all children in the household. One child was then randomly selected and the parent was instructed to think of that child when answering questions.
This study was classified as exempt from human participants review by the University of Michigan Institutional Review Board and the need for informed consent was waived owing to the collection of deidentified data with minimal risk to the participants.
Survey Instrument
The online survey included a discrete choice experiment (DCE) designed to elicit parents’ preferences for enhanced access services in their child’s primary care office (sample question in the eFigure in the Supplement; full survey instrument in the eAppendix in the Supplement). Discrete choice experiments are part of a group of preference-based survey methods grounded in economic theory referred to as conjoint analysis.11,15 Discrete choice experiments are increasingly used to measure patients’ preferences for characteristics of a variety of health care services.9,10,16–20 In DCEs, respondents complete a series of questions each with a hypothetical scenario in which respondents are asked to make a choice between 2 or more options with defined characteristics (referred to as attributes) that are assigned different values (referred to as levels) for each of the options within the scenario. The choices that respondents make across multiple scenarios can be used to infer respondents’ relative preferences for the levels of each attribute and their willingness to make trade-offs between attributes.
Following methodological guidelines for DCEs,21 we identified important attributes of enhanced access services through a literature review of medical home programs,2–4 discussions with pediatricians and primary care administrators, and qualitative interviews with parents.13 The key attributes of enhanced access and potential trade-offs in this survey were communication outside of office visits, same-day sick visits, late office hours, weekend hours, wait times to next available preventive care visit, weekday hours, and professional continuity (Table 1). Discrete choice experiments also typically include an additional value attribute, such as cost or travel time, to allow for comparisons of preferences on a standardized scale.11 We chose travel time as a value attribute because in pilot testing it was meaningful and intuitively understandable for parents. Each of these attributes was then assigned 2 or 4 levels with the values of these levels based on the literature review, discussions with pediatricians and practice administrators, and qualitative interviews with parents.
Table 1.
Attributes and Levels for Enhanced Access Discrete Choice Questions
| Attributes | Levels |
|---|---|
| Communication outside office visits | Telephone advice only during office hours and no emaila Telephone advice 24 h, 7 d/wk and no email Telephone advice 24 h, 7 d/wk and nonurgent email Telephone advice 24 h, 7 d/wk and urgent and nonurgent email |
| Sick visits | Rarely the same day, usually in 1 to 2 da Usually on the same day but may be asked to wait 1 to 2 d, depending on how sick child is Always on the same day if requested Walk in on a first-come, first-serve basis |
| Checkups and physicals | Usually available within same day to 1 wka Usually available within 1 to 2 wk Usually available within 2 to 4 wk Usually available within 4 to 8 wk |
| Weekday hours | 3 Full days and 2 half days a weeka 5 Full days a week |
| Late hours | No office hours after 5 PMa 2 Evenings per wk, 5 to 8 PM 4 Evenings per wk, 5 to 8 PM 5 Evenings per wk, 5 to 8 PM |
| Weekend hours | No weekend hoursa Half day on Saturday Full day on Saturday Half days on Saturday and Sunday |
| Continuity | See the same physician for nearly all checkups and some sick visitsa See whoever is available for well and sick visits |
| Travel time | 5 min 15 min 30 min 45 min |
Reference level.
The survey included an introduction to the discrete choice scenarios with a description of the attributes and a practice question. Each respondent then received 8 discrete choice questions. Each question asked parents to choose between 2 primary care offices with different levels of enhanced access services and potential trade-off attributes. Each choice included levels for all 7 attributes (a full profile design). No opt-out option was included. A fractional factorial design was used with the randomization of blocks of 8 of 32 possible questions to respondents to maximize the statistical power of the survey to detect preferences while minimizing respondent burden.11
In addition to the discrete choice questions, the survey included questions about child sociododemographic characteristics including child age, special health care needs,22 insurance status and type, and parent-reported child health. As part of the standing panel, Knowledge Networks maintained information about respondent (parental) self-reports of race/ethnicity, education level, and household income. Because the sample was drawn from a standing panel, sociodemographic information was also available for nonrespondent adults.
Survey instructions and questions were written at the ninth grade reading level (based on the Flesch-Kincaid grade level). The survey was pilot tested with a sociodemographically diverse group of 20 parents as part of a qualitative study13 and revisions were made based on responses during interviews to improve readability and comprehension. The survey was then pretested with an independent sample of parents from the Knowledge Networks panel (n = 122) to estimate response times and nonresponse rates for specific questions.
Data Analysis
We estimated preferences for the different levels of attributes using a mixed logit model. The coefficients from the mixed logit model represented estimates of the probability of choosing a primary care office as a function of the levels of the attributes for that office. The mixed logit accounted for repeated choices by the same respondent and allowed for random coefficients at the respondent level. Effects coding was used to allow estimation of preferences for all levels of each attribute including the reference level.23 We first estimated a main effects mixed logit model and then estimated models with interaction terms to assess potential differences in preferences across groups with different sociodemographic characteristics including child age, parent-reported child health, special health care needs, and health insurance; parent race/ethnicity; household income; and urban vs rural residence. We also tested stratified models by race/ethnicity to assess the size of any significant differences found from the interaction terms. Results from the main effects mixed logit model were used to calculate a marginal willingness to travel for each level of each attribute, representing how much farther respondents were willing to travel for an office with a given level of an attribute.11 All analyses were performed using Stata 12.1 (StataCorp LP). Statistical significance from 0 for coefficients and marginal willingness to travel of individual services was determined from the results of the mixed logit model at the P < .05 level. Statistical significance from 0 for marginal willingness to travel of primary care offices with hypothetical combinations of services was assessed using the linear combination of coefficients, also with a significance level of P < .05.
Results
Study Participants
Eight-hundred twenty parents participated and completed the survey, including the discrete choice experiment questions, with a response rate of 41.2%. The demographic characteristics of participating parents and their children are shown in Table 2. Based on comparisons with demographic characteristics of nonrespondents, there was less participation from parents who were female, younger, or black; had lower educational attainment; or lived in low-income households (eTable in the Supplement).
Table 2.
Characteristics of Parent Respondents and Their Children
| Characteristics | No. (%) |
|---|---|
| Parent | |
| Female | 443 (54) |
| Age, y | |
| 18–29 | 145 (18) |
| 30–44 | 474 (58) |
| 45–59 | 190 (23) |
| ≥60 | 11 (1) |
| Race/ethnicity | |
| White non-Hispanic | 436 (53) |
| Black non-Hispanic | 165 (20) |
| Hispanic | 174 (21) |
| Other/multiple | 45 (5) |
| Education | |
| Less than high school | 74 (9) |
| High school | 214 (26) |
| Some college | 232 (28) |
| Bachelor’s degree or higher | 300 (37) |
| Household income <200% FPL | 282 (34) |
| Child | |
| Female | 393 (48) |
| Age, y | |
| 0–5 | 270 (33) |
| 6–11 | 273 (33) |
| 12–17 | 277 (34) |
| Child health (parent reported) | |
| Excellent | 503 (61) |
| Very good | 235 (29) |
| Good/fair/poor | 82 (10) |
| Presence of special health care needa | 189 (23) |
| Health insurance | |
| Private | 496 (61) |
| Public | 271 (34) |
| Uninsured | 41 (5) |
Abbreviation: FPL, federal poverty level.
As defined by the Child and Adolescent Health Measurement Initiative’s Children With Special Health Care Needs Screener.22
Parents’ Preferences for Enhanced Access in Primary Care
In the discrete choice analysis, the coefficients for nearly all levels of the included attributes were significantly different from 0, suggesting the attributes were meaningful to parents in making choices between practices (Table 3). In analysis of discrete choice experiments, coefficients for levels of attributes that are significantly different from 0 indicate the level influenced the choices made by respondents; coefficients that are not significantly different from 0 suggest that the level was not meaningful to respondents.
Table 3.
Parents’ Preferences and WTT for Enhanced Access and Other Attributes of Primary Care
| Attributes | Coefficient (SE)a | WTT (95% CI), minb | Importance Scorec |
|---|---|---|---|
| Communication outside of office visits | 8.4 | ||
| Telephone (office hours only) and no email | −0.242 (0.045)d | −6 (−8 to −4)e,f | |
| Telephone (24 h, 7 d/wk) and no email | 0.029 (0.042)e | 1 (−1 to 3) | |
| Telephone (24 h, 7 d/wk) and nonurgent email | 0.129 (0.041)d | 3 (1 to 5)d | |
| Telephone (24 h, 7 d/wk) and urgent and nonurgent email | 0.084 (0.043)e | 2 (0 to 4) | |
| Same-day sick visits | 29.0 | ||
| Rarely | −0.713 (0.054)d | −17 (−20 to −14)e,f | |
| Usually | 0.131 (0.040)d | 3 (1 to 5)e | |
| Always | 0.571 (0.053)d | 14 (11 to 16)e,f | |
| Walk in | 0.011 (0.043) | 0 (−2 to 2) | |
| Preventive visits, wk | 14.8 | ||
| Same day to 1 | 0.253 (0.044)d | 6 (4 to 8)e | |
| 1 to 2 | 0.143 (0.040)d | 3 (2 to 5)e | |
| 2 to 4 | 0.005 (0.046) | 0 (−2 to 2) | |
| 4 to 8 | −0.401 (0.043)d | −10 (−12 to −8)e,f | |
| Weekday hours | 5.2 | ||
| 3 Full days and 2 half days | −0.114 (0.025)d | −3 (−4 to −2)e,f | |
| 5 Full days | 0.114 (0.025)d | 3 (2 to 4)e | |
| Late hours, evenings | 13.9 | ||
| None | −0.417 (0.043)d | −10 (−12 to −8)e,f | |
| 2 | 0.077 (0.042) | 2 (0 to 4) | |
| 4 | 0.142 (0.039)d | 3 (2 to 5)e | |
| 5 | 0.198 (0.043)d | 5 (3 to 7)e | |
| Weekend hours | 12.5 | ||
| No weekend hours | −0.359 (0.044)d | −9 (−11 to −6)e,f | |
| Half day on Saturday | 0.060 (0.043) | 1 (−1 to 3) | |
| Full day on Saturday | 0.105 (0.041)e | 3 (1 to 4)e | |
| Half days on Saturday and Sunday | 0.193 (0.043)d | 5 (3 to 7)e | |
| Continuity | 16.3 | ||
| See same physician for nearly all visits | 0.361 (0.032)d | 9 (7 to 10)d | |
| See whoever is available | −0.361 (0.032)d | −9 (−10 to −7)e,f | |
| Travel time, min | −0.042 (0.003)d | ||
| Primary care office | |||
| Idealg | NA | 44 (37 to 51)e | |
| Goodh | NA | 19 (14 to 24)e | |
| Good with fewer weekday hoursi | NA | 13 (8 to 18)e |
Abbreviations: NA, not available; WTT, willingness to travel.
Results using effects coding in a mixed logit model. Coefficients represent the change in utility for a respondent for a specific level of a given attribute.
Willingness to travel calculations are mean estimates derived from the mixed logit model without interactions.
The relative importance of each attribute is calculated as follows: for each attribute, the difference between the utilities of its levels is divided by the sum of the differences between the utilities for all of the attributes and multiplied by 100.24
P < .001.
P < .05.
Negative values represent the average amount of travel time that would have to be decreased for a parent to choose a practice with that characteristic.
Practice with most preferred attributes: telephone advice 24 hours a day and nonurgent email access, same-day sick visits always available, preventive visits available within 1 week, office open 5 full days a week, late hours 5 evenings a week, office open for half days on Saturday and Sunday, and professional continuity for nearly all checkups and some sick visits.
Practice with telephone advice 24 hours a day and no email access, same-day sick care usually available but could wait 1 to 2 days, preventive visits available within 2 to 4 weeks, office open 5 full days a week, late hours 2 evenings a week, office open for half days on Saturday, and professional continuity for nearly all checkups and some sick visits.
Practice with telephone advice 24 hours a day and no email access, same-day sick care usually available but could wait 1 to 2 days, preventive visits available within 2 to 4 weeks, office open 3 full days a week and 2 half days, late hours 2 evenings a week, office open 2 half days a week, and professional continuity for nearly all checkups and some sick visits.
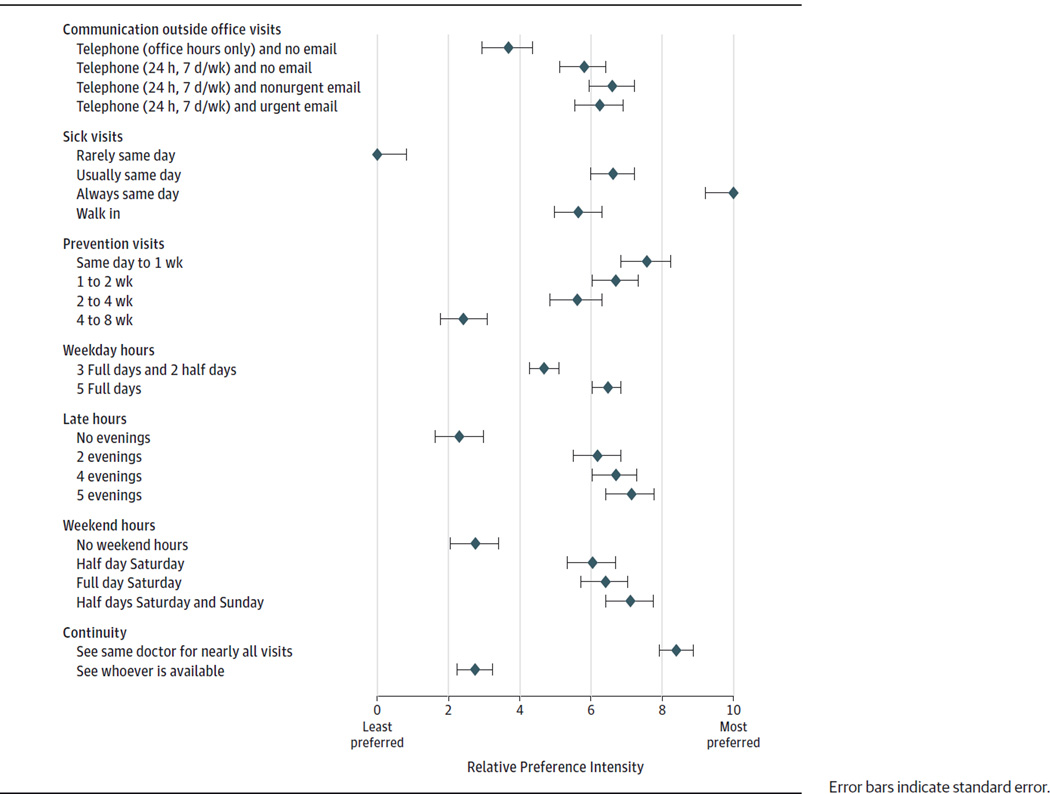
Respondents’ relative preferences for different levels of attributes are important in interpreting results of a DCE. The Figure shows a visual representation of the results of the DCE with the coefficients rescaled, with 0 representing the least preferred and 10 representing the most preferred attributes in this study. In relation to the levels of other attributes, parents’ strongest preference was for primary care practices that guaranteed same-day sick visits. The largest change in preference (gain in utility) was between practices that rarely provided same-day sick care and those that usually provided same-day visits with some triaging to the next day. Parents also had strong preferences for professional continuity, outweighing the levels of all other services except same-day sick care. Another way to assess the relative strength of preferences for these attributes was the importance score, the results of which caused the same inferences (Table 3).24
Figure.
Relative Preferences for Enhanced Access Services and Potential Trade-offs in Other Primary Care Services
Other attributes showed large increases in preferences between the worst level and the first level of improvement with only incremental gains for each subsequent level. For example, parents strongly preferred practices with 24-hour telephone access compared with those without this service but there was little change in preference with the addition of access by email or a secure website. Similarly, offices with some evening and weekend hours were strongly preferred compared with offices with no evening or weekend hours, but beyond that, increases in the number of evenings or weekend hours made little change in preferences.
Variation in Parents’ Preferences for Enhanced Access
When we tested interaction terms between sociodemographic characteristics and preferences for different levels of practice attributes, we found little significant variation (data available on request). Parents of younger children had stronger preferences for evening hours compared with parents of older children. Parents of children with special health care needs had stronger preferences for professional continuity. Parents of children with public insurance had stronger preferences for evening hours compared with parents of children with private insurance. Black non-Hispanic parents and Hispanic parents had stronger preferences for same-day sick visits and walk-in visits and had weaker preferences for being open 5 full weekdays compared with white non-Hispanic parents. Despite being statistically significant, the magnitude of differences in preferences across groups was small.
Parents’Willingness to Travel for Enhanced Access
Parents reported a mean travel time of 16 minutes (95% CI, 15–17 minutes) and median of 15 minutes (interquartile range, 10–20 minutes) to their child’s current primary care professional. Based on the discrete choice analysis, parents were willing to travel an additional 14 minutes (95% CI, 11–16minutes) for a practice that always had same-day sick visits and an additional 9 minutes (95% CI, 7–10 minutes) for good professional continuity (Table 3). Parents’ willingness to travel to a practice with the highest levels of all attributes was 44 minutes compared with a standard pediatric office setting (95% CI, 37–51 minutes).
Discussion
In this study in a national sample of parents, we used a DCE to assess the enhanced access services that parents would be likely to prioritize in the resource-constrained environment of most primary care practices. We found that parents’ preferences were strongest for access to same-day sick visits followed closely by their strong preferences for good continuity with their child’s primary care professional. Parents reported a willingness to increase the travel time to their child’s primary office by significant durations to obtain these services. Parents had significant preferences for other enhanced access services, such as 24-hour telephone advice, access by electronic communication, and evening and weekend office hours but these preferences were not as strong as those for same-day sick care and professional continuity. The strength of these preferences was similar across parents with different sociodemographic characteristics.
Implementation of the medical home model has been criticized for being driven by the preferences of practices and health systems and not being truly patient centered in responding to the needs and expectations of patients and their families.25,26 The results from this study could be used by practices at any stage of medical home implementation to consider which enhanced access services they should prioritize to best meet the preferences of families. Short of directly using the results from this study, our results illustrated the importance of considering parents’ preferences and the trade-offs parents might be willing to make for services in their child’s primary care office. Future research is needed to assess whether incorporating parents’ preferences into medical home implementation has the potential to improve primary care use and, ultimately, child health outcomes.
Practices should continue to weigh other factors, such as evidence for effectiveness, in addition to patient and family preferences in considering new or enhanced services. Practices will need to consider how they will make implementation decisions when evidence for effectiveness conflicts with patient and family preferences. To date, the evidence base for enhanced access services has been limited, with some suggestion that services, such as same-day sick care and evening hours (services preferred by parents in our study), are associated with decreased emergency department use.27–29
The results of this study should be viewed in the context of several limitations. First, the response rate for the survey was modest at 41.2% and, although Knowledge Networks maintains a nationally representative panel, actual survey respondents were not necessarily nationally representative. We were able to compare sociodemographic characteristics between responders and nonresponders and found relatively lower response rates from several groups including mothers, younger parents, African American parents, parents with lower educational attainment, and parents living in low-income households. Despite this, our sample was comparable with other national surveys in terms of parent and child sociodemographics.30 Additionally, the survey was only fielded in English, so preferences of Hispanic parents were only representative of those who primarily spoke English. Second, the national sample for this survey may have limited the applicability of results to practices that serve populations that are not well represented in our survey. However, the similarities in preferences among parents across different sociodemographic characteristics suggest that these results are likely applicable to most populations. Third, we restricted our survey questions to enhanced access services commonly included in medical home recognition programs and did not include other models proposed to enhance access, such as group visits and increased delivery of services by nonphysician professionals.31,32
Conclusions
Primary care practices for children that emphasize same-day sick care and professional continuity are more likely to meet parents’ preferences for enhanced access. Our study provided important information for practices that could inform which enhanced access services to implement to meet parent preferences. Practices should engage families in prioritizing services that may be added or changed as part of medical home implementation.
Supplementary Material
Acknowledgments
Funding/Support: This work was supported by a grant from the Blue Cross Blue Shield of Michigan Foundation. Development of the survey was supported by seed grant UL1RR024986 through the Michigan Institute for Clinical and Health Research at the University of Michigan. Dr Zickafoose was a research fellow in the CHEAR Unit, Division of General Pediatrics, University of Michigan at the time of the study and was supported by training grant T32 HD07534 from the National Institute of Child Health and Human Development.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr Zickafoose had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: All authors.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Zickafoose.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Zickafoose, Prosser.
Obtained funding: Zickafoose, DeCamp.
Study supervision: Prosser.
Additional Contributions:We thank Achamyeleh Gebramariam, MS, Child Health Evaluation and Research (CHEAR) Unit, Division of General Pediatrics, University of Michigan, for his assistance with the statistical analyses in this study. A portion of his time was subsidized by the grant from the Blue Cross Blue Shield of Michigan Foundation listed above.
Conflict of Interest Disclosures: None reported.
REFERENCES
- 1.Medical Home Initiatives for Children With Special Needs Project Advisory Committee: American Academy of Pediatrics. The medical home. Pediatrics. 2002;110(1, pt 1):184–186. [PubMed] [Google Scholar]
- 2.American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians and AOA. [Accessed November 18, 2014];Joint Principles of the Patient-Centered Medical Home. http://www.aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMHJoint.pdf. Published 2007. [Google Scholar]
- 3.Blue Cross Blue Shield of Michigan. Physician Group Incentive Program: Patient-Centered Medical Home Initiatives. Detroit, MI: Blue Cross Blue Shield of Michigan; 2010. [Google Scholar]
- 4.National Committee for Quality Assurance. Standards and Guidelines for NCQA’s Patient-Centered Medical Home (PCMH) Washington, DC: National Committee for Quality Assurance; 2011. [Google Scholar]
- 5.Abrams M, Schor EL, Schoenbaum S. How physician practices could share personnel and resources to support medical homes. Health Aff (Millwood) 2010;29(6):1194–1199. doi: 10.1377/hlthaff.2010.0088. [DOI] [PubMed] [Google Scholar]
- 6.Nutting PA, Crabtree BF, Miller WL, Stange KC, Stewart E, Jaén C. Transforming physician practices to patient-centered medical homes: lessons from the national demonstration project. Health Aff (Millwood) 2011;30(3):439–445. doi: 10.1377/hlthaff.2010.0159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Safety Net Medical Home Initiative. Neal R, Moore L, Powell J. Enhanced Access: Providing the Care Patients Need, When They Need It. [Accessed November 18, 2014]; http://www.safetynetmedicalhome.org/sites/default/files/Implementation-Guide-Enhanced-Access.pdf. Published 2013. [Google Scholar]
- 8.Crabtree BF, Nutting PA, MillerWL, Stange KC, Stewart EE, Jaén CR. Summary of the National Demonstration Project and recommendations for the patient-centered medical home. Ann Fam Med. 2010;8(suppl 1):S80–S90. S92. doi: 10.1370/afm.1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burge P, Devlin N, Appleby J, Rohr C, Grant J. London Patient Choice Project Evaluation: A Model of Patients’ Choices of Hospital From Stated and Revealed Preference Choice Data. Cambridge, England: RAND Corporation; 2005. [Google Scholar]
- 10.Kruk ME, Rockers PC, Tornorlah Varpilah S, Macauley R. Population preferences for health care in liberia: insights for rebuilding a health system. Health Serv Res. 2011;46(6, pt 2):2057–2078. doi: 10.1111/j.1475-6773.2011.01266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ryan M, Gerard K, Amaya-Amaya M, editors. Using Discrete Choice Experiments to Value Health and Health Care. Dordrecht, the Netherlands: Springer; 2008. [Google Scholar]
- 12.Brown DS, Johnson FR, Poulos C, Messonnier ML. Mothers’ preferences and willingness to pay for vaccinating daughters against human papillomavirus. Vaccine. 2010;28(7):1702–1708. doi: 10.1016/j.vaccine.2009.12.024. [DOI] [PubMed] [Google Scholar]
- 13.Zickafoose JS, DeCamp LR, Sambuco DJ, Prosser LA. Parents’ preferences for enhanced access to the pediatric medical home: a qualitative study. J Ambul Care Manage. 2013;36(1):2–12. doi: 10.1097/JAC.0b013e318276dc2f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Knowledge Networks. Knowledge panel design summary. [Accessed April 6, 2012]; http://www.knowledgenetworks.com/knpanel/KNPanel-Design-Summary.html. Published 2010. [Google Scholar]
- 15.Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. Pharmacoeconomics. 2008;26(8):661–677. doi: 10.2165/00019053-200826080-00004. [DOI] [PubMed] [Google Scholar]
- 16.Grol R, Wensing M, Mainz J, et al. Patients’ priorities with respect to general practice care: an international comparison: European Task Force on Patient Evaluations of General Practice (EUROPEP) Fam Pract. 1999;16(1):4–11. doi: 10.1093/fampra/16.1.4. [DOI] [PubMed] [Google Scholar]
- 17.Ryan M, Watson V. Counting the cost of fast access: using discrete choice experiments to elicit preferences in general practice. Br J Gen Pract. 2006;56(522):4–5. [PMC free article] [PubMed] [Google Scholar]
- 18.Gerard K, Salisbury C, Street D, Pope C, Baxter H. Is fast access to general practice all that should matter? a discrete choice experiment of patients’ preferences. J Health Serv Res Policy. 2008;13(suppl 2):3–10. doi: 10.1258/jhsrp.2007.007087. [DOI] [PubMed] [Google Scholar]
- 19.Gerard K, Lattimer V, Surridge H, et al. The introduction of integrated out-of-hours arrangements in England: a discrete choice experiment of public preferences for alternative models of care. Health Expect. 2006;9(1):60–69. doi: 10.1111/j.1369-7625.2006.00365.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gidengil C, Lieu TA, Payne K, Rusinak D, Messonnier M, Prosser LA. Parental and societal values for the risks and benefits of childhood combination vaccines. Vaccine. 2012;30(23):3445–3452. doi: 10.1016/j.vaccine.2012.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bridges JF, Hauber AB, Marshall D, et al. Conjoint analysis applications in health, a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 2011;14(4):403–413. doi: 10.1016/j.jval.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 22.Bethell CD, Read D, Stein RE, Blumberg SJ, Wells N, Newacheck PW. Identifying children with special health care needs: development and evaluation of a short screening instrument. Ambul Pediatr. 2002;2(1):38–48. doi: 10.1367/1539-4409(2002)002<0038:icwshc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 23.Bech M, Gyrd-Hansen D. Effects coding in discrete choice experiments. Health Econ. 2005;14(10):1079–1083. doi: 10.1002/hec.984. [DOI] [PubMed] [Google Scholar]
- 24.Wouters H, Van Dijk L, Van Geffen ECG, et al. Do the benefits of statins outweigh their drawbacks? assessing patients’ trade-off preferences with conjoint analysis. Int J Cardiol. 2014;176(3):1220–1222. doi: 10.1016/j.ijcard.2014.07.219. [DOI] [PubMed] [Google Scholar]
- 25.Berenson RA, Hammons T, Gans DN, et al. A house is not a home: keeping patients at the center of practice redesign. Health Aff (Millwood) 2008;27(5):1219–1230. doi: 10.1377/hlthaff.27.5.1219. [DOI] [PubMed] [Google Scholar]
- 26.Bechtel C, Ness DL. If you build it, will they come? designing truly patient-centered health care. Health Aff (Millwood) 2010;29(5):914–920. doi: 10.1377/hlthaff.2010.0305. [DOI] [PubMed] [Google Scholar]
- 27.Zickafoose JS, DeCamp LR, Prosser LA. Association between enhanced access services in pediatric primary care and utilization of emergency departments: a national parent survey. J Pediatr. 2013;163(5):1389, 95.e1–95.e6. doi: 10.1016/j.jpeds.2013.04.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Paneth N, Bell D, Stein REK. Emergency room utilization in the first 15 months of life: a randomized study. Pediatrics. 1979;63(3):486–490. [PubMed] [Google Scholar]
- 29.O’Malley AS, Samuel D, Bond AM, Carrier E. After-hours care and its coordination with primary care in the US. J Gen Intern Med. 2012;27(11):1406–1415. doi: 10.1007/s11606-012-2087-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.National Center for Health Statistics. National Survey of Children’s Health. [Accessed June 3, 2014]; http://www.cdc.gov/nchs/slaits/nsch.htm.
- 31.Coker TR, Chung PJ, Cowgill BO, Chen L, Rodriguez MA. Low-income parents’ views on the redesign of well-child care. Pediatrics. 2009;124(1):194–204. doi: 10.1542/peds.2008-2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Coker TR, Thomas T, Chung PJ. Does well-child care have a future in pediatrics? Pediatrics. 2013;131(suppl 2):S149–S159. doi: 10.1542/peds.2013-0252f. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.