Abstract
Endocrine therapy, using tamoxifen or an aromatase inhibitor, remains first-line treatment for estrogen receptor (ESR1) positive breast cancer. However, tumor resistance limits the duration of response. The clinical efficacy of fulvestrant, a Selective Estrogen Receptor Degrader (SERD) that triggers receptor degradation, has confirmed that ESR1 often remains engaged in endocrine therapy resistant cancers. Recently developed Selective Estrogen Receptor Modulators (SERM)/SERD hybrids (SSHs) that facilitate ESR1 degradation in breast cancer cells and reproductive tissues have been advanced as an alternative treatment for advanced breast cancer, particularly in the metastatic setting. RAD1901 is one SSH currently being evaluated clinically that is unique among ESR1 modulators in that it readily enters the brain, a common site of breast cancer metastasis. In this study, RAD1901 inhibited estrogen activation of ESR1 in vitro and in vivo, inhibited estrogen-dependent breast cancer cell proliferation and xenograft tumor growth, and mediated dose-dependent downregulation of ESR1 protein. However, doses of RAD1901 insufficient to induce ESR1 degradation were shown to result in activation of ESR1 target genes and in stimulation of xenograft tumor growth. RAD1901 is an SSH that exhibits complex pharmacology in breast cancer models, having dose-dependent agonist/antagonist activity displayed in a tissue-selective manner. It remains unclear how this unique pharmacology will impact the utility of RAD1901 for breast cancer treatment. However, being the only SERD currently known to access the brain, RAD1901 merits evaluation as a targeted therapy for the treatment of breast cancer brain metastases.
Keywords: Selective estrogen receptor degrader, SERM, endocrine-resistant breast cancer, RAD1901
Introduction
Breast cancer remains the most commonly diagnosed cancer among women and a leading cause of cancer mortality (Carter 2014). While targeted therapies such as the selective estrogen receptor modulator (SERM) tamoxifen and aromatase inhibitors (AIs) are initially effective in the treatment of estrogen receptor alpha (ESR1) positive tumors, de novo and acquired resistance remain an impediment to durable clinical responses, particularly in the setting of advanced disease. However, ESR1 remains a therapeutic target in breast cancers that are resistant to both first and second line endocrine interventions (Perey, et al. 2007; Riggins, et al. 2007), a finding that has prompted the development of (a) SERMs with a mechanism distinct from tamoxifen and (b) selective estrogen receptor degraders (SERDs), competitive antagonists whose interaction with ESR1 induce its proteasome dependent degradation. Fulvestrant, currently the only SERD approved for the treatment of metastatic breast cancer, has been effective as both a first- and second-line therapy in advanced breast cancer (Chia, et al. 2008; Leo, et al. 2009; Robertson, et al. 2014; Robertson, et al. 2001); however, the pharmaceutical properties of this drug may prove dose-limiting in relapsed/resistant breast tumors bearing ESR1 mutations known to decrease SERD potency (Jeselsohn, et al. 2014; Robinson, et al. 2013; Toy, et al. 2013). SERDs with improved bioavailability are currently being evaluated in the clinic for efficacy in treating breast cancer patients who have progressed on endocrine therapies (Mayer, et al. 2013).
In recent years there has been a high level of interest in exploiting the complexities of ESR1 signaling to identify novel selective estrogen receptor modulators (SERMs), compounds whose relative agonist/antagonist activity is manifest in a cell/tissue restricted manner. Motivated by the observation that tamoxifen could exhibit agonist activities in the bone and the endometrium while functioning as an antagonist in breast, investigators have identified and developed a series of ESR1 ligands that display more clinically useful selectivity (i.e. raloxifene, ospemifene and lasofoxifene) (Dallenbach-Hellweg, et al. 2000; Komm and Chines 2012; Lindahl, et al. 2008). Unexpectedly, these discovery efforts also led to the identification of a series of compounds that exhibit some of the properties of both SERMs and SERDs. These SERM/SERD Hybrids (SSH) have been shown to function as agonists in bone, but remarkably inhibit ESR1-action in the reproductive system, and in animal models of breast cancer, by inducing receptor degradation. The first drug of this class, GW5638/DPC974, was shown to function as a competitive antagonist of ESR1 that induced a conformational change in the receptor that resulted in its being targeted it for proteasomal degradation in breast cancer cells (Willson, et al. 1997). Importantly, this drug exhibited favorable pharmaceutical properties, inhibited the growth of tamoxifen-resistant breast tumor xenografts and demonstrated efficacy in a small study of patients with advanced, heavily pretreated, breast cancer (Bentrem, et al. 2001; Connor, et al. 2001; Dardes, et al. 2002). Whereas this drug was abandoned for non-scientific reasons, its demonstrated efficacy led others to search for similar molecules that exhibited SSH activity. Of note is (a) the identification of ARN810 (GDC-0810) (Lai, et al. 2015), a structural analogue of GW5638, and (b) the observation that bazedoxifene, a drug approved for the treatment and prevention of osteoporosis in post-menopausal women, exhibits tissue-selective SERD activity (S. Wardell, unpublished observations). Both drugs effectively inhibit the growth of both treatment-naive and tamoxifen-resistant xenograft tumors in mice and are at different stages of clinical development for metastatic breast cancer (Lewis-Wambi, et al. 2011; Mayer et al. 2013; Wardell, et al. 2015; Wardell, et al. 2013).
Despite their efficacy in the treatment of postmenopausal osteoporosis, the currently available SERMs and SSHs do not treat the vasomotor instability (hot flushes) associated with menopause. One impediment to the identification of a SERM/SSH modulator for the treatment of hot flashes is inability to identify compounds that effectively cross the blood brain barrier. The identification of RAD1901, a SERM that readily enters the brain, was therefore of interest. Preclinical studies showed that RAD1901 mitigated vasomotor symptoms in animal models while also preventing ovariectomy associated bone loss (Hattersley, et al. 2007). Remarkably, however, when the utility of RAD1901 to reduce vasomotor symptoms was evaluated clinically, an unexpectedly complex dose response was observed. Specifically, vasomotor symptoms were improved at the lowest dose evaluated while higher dose administration was found to be ineffective or even to exacerbate symptoms when compared to placebo (O’Dea, et al. 2010). Thus, RAD1901 is unique among SERMs in that it displays a complex dose-related agonist/antagonist activity. Although a Phase I clinical trial was recently initiated evaluating RAD1901 as a potential therapy for advanced breast cancer (Clinical trial #NCT02338349), it is important to elucidate the mechanism underlying the complex pharmacology of this drug to ensure that it is evaluated in a manner that maximizes its potential for success. Thus, the objective of this study was to probe the molecular mechanism(s) underlying the complex pharmacology of RAD1901, studies that we believe will inform its optimal clinical development.
Materials and Methods
Reagents
Purchased ESR1 ligands included 17β-estradiol (Sigma, St. Louis, MO, USA), ICI 182,780 (Tocris, Bristol, United Kingdom), tamoxifen (Sigma), raloxifene (Tocris), and 4-hydroxytamoxifen (Sigma). (R)-6-(2-(N-(4-(2-(ethylamino)ethyl)benzyl)-N-ethylamino)-4-methoxyphenyl)-5,6,7,8-tetrahydronaphthalen-2-ol dihydrochloride (RAD1901) was provided by Radius Pharmaceuticals. Bazedoxifene and GW7604 were synthesized as previously described (Miller, et al. 2001; Wilson 1997 Oct 28). Ligands were dissolved in ethanol or DMSO.
Cell culture
Cell lines were authenticated by STRS analysis performed by ATCC in 2013. Experiments were conducted using cell line passages 2–25. MCF7 and SKBR3 cell lines (ATCC, Manassas, VA) were maintained in DMEM/F12 or RPMI media (Invitrogen, Grand Island, NY, USA), respectively, supplemented with 8% (v/v) fetal bovine serum (FBS – Gemini Bio-products, West Sacramento, CA, USA), non-essential amino acids (Invitrogen), and sodium pyruvate (Invitrogen). Unless otherwise indicated, cells were plated for experiments in media lacking phenol red and supplemented with 8% charcoal stripped FBS (CFS - Gemini). LTED MCF7 cells were maintained and plated for experiments in phenol red free DMEM/F12 media supplemented with 8% CFS that had been charcoal stripped twice. 48 hours after plating, cells were treated with ESR1 ligands as indicated, and were harvested for immunoblot or real time quantitative PCR analysis 24 hours after treatment.
Immunoblot analysis
Protein expression was analyzed as described (Wittmann, et al. 2007) using antibodies purchased from Sigma - A5441 (β-actin) and Santa Cruz Biotechnology (Santa Cruz, CA, USA) - sc-6259 (cytokeratin 18), sc-20680 (lamin A), sc-5546 (α-tubulin) and sc-8005 (ESR1).
RNA isolation and real time quantitative PCR
RNA isolation and analysis was performed as described (Wardell, et al. 2011). mRNA abundance was calculated using the ΔΔCT method (Wardell et al. 2011). Primer sequences are available upon request.
Proliferation assays
Assays evaluating the effects of SERDs and SERMs on cell proliferation were performed as described (Wardell et al. 2013).
Transfections
Mammalian 2-hybrid analysis of VP16-ESR1 with conformation-selective peptide probes was performed essentially as previously described (Wardell, et al. 2012).
In vivo studies
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving animals were in accordance with the ethical standards of the Duke University Institutional Animal Care and Use Committee.
Uterine wet weight analysis
Ovariectomized (10 days prior) female C57Bl/6 mice (Charles River, Raleigh, NC, USA) were treated daily (n = 5) for 3 days with vehicle or estradiol benzoate (10 μg/kg sc) as well as vehicle, raloxifene (10 mg/kg sc), or RAD1901 (0.1–100 mg/kg sc). Ligands were dissolved in corn oil (Spectrum chemicals, New Brunswick, NJ, USA). On day 4, mice were euthanized and tissues were retained for analysis. Uterine wet weight was calculated as a ratio of uterus weight upon removal to body weight post-mortem.
Xenograft tumor analysis
Estrogen-stimulated MCF7 tumors were initiated in the axial mammary gland of 6-week old estrogen-treated (0.72mg/60days pellet sc, Innovative Research of America, Sarasota, FL, USA) ovariectomized female NU/NU mice (in-house colony) by serial transfer and were measured as described (Wardell et al. 2013). Fig. 1: At ~0.1cm3 tumor volume, mice were randomized (n = 9–10) to daily treatment with vehicle, RAD1901 (20 mg/kg), or tamoxifen (20 mg/kg). Fig. 4: At ~0.1cm3 tumor volume, the estrogen pellet was surgically removed, and mice were randomized (n = 6–10) to daily treatment with vehicle or RAD1901 (0.3–10 mg/kg). Treatments were formulated as above. Animal tissues were processed and analyzed as described (Wardell et al. 2015; Wardell et al. 2013).
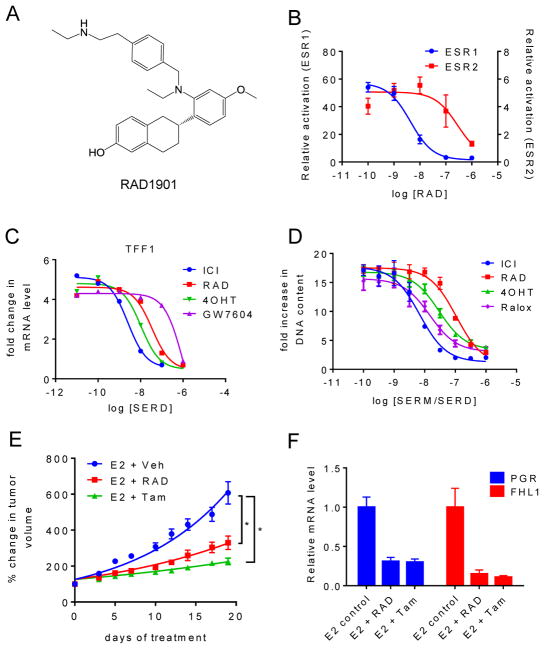
Fig. 1. RAD1901 inhibits ESR1 activity in vitro and in vivo.
A) Chemical structure of SERM RAD1901. B) SKBR3 cells were plated in phenol red free media supplemented with charcoal stripped FBS (CFS) 24 hours prior to transfection with an ERE-luciferase reporter together with ESR1 or ESR2 expression vectors. 24 hours after transfection, cells were treated with E2 (10 nM) together with RAD (10−10–10−6 M) for 24 hours prior to harvest and analysis of luciferase activity normalized to co-transfected β-galactosidase control. B) MCF7 cells were plated in phenol red free media supplemented with CFS 48 hours prior to treatment with 10−9 M E2 together with ICI 182,780 (ICI), RAD1901 (RAD), GW7604, or 4-hydroxytamoxifen (4OHT) (10−11–10−6 M) for 24 hours. mRNA levels of ESR1 target gene trefoil factor 1 (TFF1) were assessed using RT qPCR following RNA isolation. mRNA expression was normalized to the similarly detected 36B4 housekeeping gene, and expression levels are presented as fold change as compared to the vehicle-treated control. D) MCF7 cells were plated in phenol red free media supplemented with CFS 24 hours prior to treatment, and were treated with 10−9 M E2 as well as with the indicated ligands (10−11 – 10−6 M) on days 1, 4, and 6 of an 8 day proliferation assay. DNA content as assessed by fluorescence was measured as a surrogate for cell proliferation. The relative increase in DNA fluorescence was calculated by normalizing to baseline values detected in a duplicate plate of cells that was harvested on day 1 prior to the initial treatment. Data are representative of at least 3 independent experiments. E–F) MCF7 cell derived tumors were implanted into ovariectomized estrogen-treated nu/nu mice. When tumor volume reached ~0.1 cm3, animals (n = 9–10) were randomized to receive daily treatment with vehicle, tamoxifen (Tam, 20 mg/kg sc) or RAD (20 mg/kg sc). E) Mean tumor volume +/− SEM per day of treatment is presented. Significance (2-way ANOVA of matched values followed by Bonferroni comparison) as compared to the vehicle control is indicated (* p < 0.0001). F) Expression of ESR1 target genes in tumors was analyzed essentially as in (C).
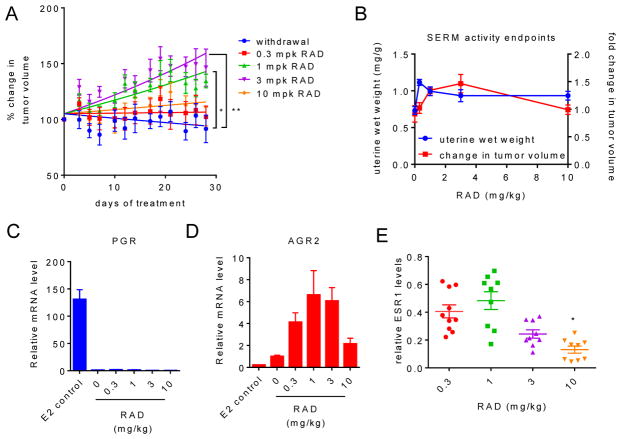
Fig. 4. RAD1901 exhibits dose dependent growth stimulation of MCF7 xenograft tumors.
MCF7 xenograft tumors were initiated in ovariectomized female nu/nu mice as in Fig. 1. Estrogen pellets were surgically removed when tumors reached ~0.1 cm3 volume, and animals (n = 6–10) then received daily treatment with vehicle or RAD (0.3–10 mg/kg sc). Mean tumor volume +/− SEM per day of treatment is presented. Significance as compared to the vehicle (2-way ANOVA of matched values followed by Bonferroni comparison) is indicated (* p < 0.05, ** p < 0.0005). B) Uterine wet weight at sacrifice (measured as in Fig. 3) and % change in tumor volume (as compared to size at randomization) calculated using the final measurement recorded for mice in (A) are graphically presented. C–D) Expression of ESR1 target genes in tumors was analyzed essentially as in Fig. 1. Estrogen only samples from Fig. 1D were included for comparison. E) ESR1 levels in tumor tissues were analyzed as in Fig. 3 and were normalized to similarly detected Lamin-A. Significant downregulation (* p < 0.05) of ESR1 was determined by ANOVA followed by Bonferroni comparion.
Statistical analyses
All statistical analyses were performed using GraphPad Prism 6. P values are indicated in figure legends. Tumor growth was analyzed by exponential growth curve analysis and by 2-way ANOVA of matched values followed by Bonferroni multiple comparisons to establish significance between groups at each day of treatment. Uterine weight, ESR1 expression in tumors and uteri, and cell proliferation (Figure 5E) were compared by ANOVA followed by Bonferroni multiple comparisons. Comparisons of ESR1 target gene regulation were conducted by 2-way ANOVA followed by Fisher’s LSD test.
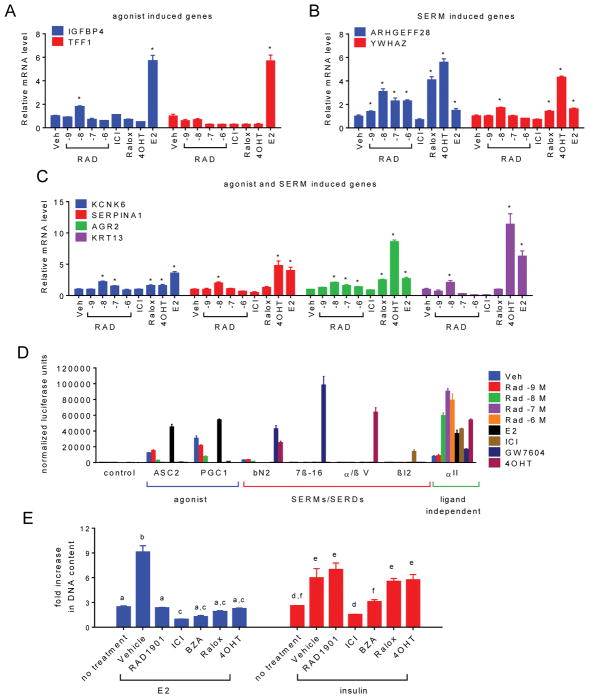
Fig. 5. RAD1901 exerts biphasic agonist/antagonist activity on ESR1 in a dose dependent manner.
A) MCF7 cells were treated for 24 hours with 10−7 M vehicle (Veh), ICI, 4OHT, raloxifene (Ralox), E2 (10−9 M) or RAD1901 (10−9–10−6 M). The expression of ESR1 target genes responsive to (A) agonists, (B) primarily SERMs, or (C) SERMs and agonists was analyzed as in Fig. 1. Relative changes of these and additional target genes designed to evaluate dose dependent response to RAD1901 are presented in Supplementary figure 2. Significant target gene regulation (* p < 0.05) as compared to the vehicle control was detected by 2 way ANOVA followed by Fisher’s LSD test. D) Interaction between ESR1 and conformation-specific peptides in a mammalian two-hybrid system. Triplicate wells of SKBR3 cells were transfected with plasmids expressing ESR1 fused to VP16 together with Gal4DBD alone (control) or Gal4DBD fused to ESR1 interacting peptides noted on the horizontal axis. Cells were then treated with the indicated ESR1 ligands (10−7 M unless otherwise indicated). Interaction of ESR1 with the Gal4DBD peptide constructs was detected through activation of a Gal4-responsive luciferase reporter construct and was normalized to detected β-galactosidase activity expressed in a constitutive manner using a second vector. Normalized response is expressed as fold increase over the detected level of interaction between Gal4DBD alone and ESR1-VP16 in the absence of ligand (Veh). E) The effect of SERMs and SERDs (10−6 M) on the proliferation of MCF7 cells in response to E2 (10−9 M) or insulin (2 × 10−9 M) was evaluated as in Fig. 1. Statistically similar treatments (2-way ANOVA followed by Bonferroni multiple comparison) are indicated by letters.
Results
RAD1901 inhibits ESR1 activity in vitro and in vivo
The ability of RAD1901 (Fig 1A) to modulate the 17-β estradiol (E2) dependent transcriptional activity of the human estrogen receptor alpha (ESR1) and human estrogen receptor beta (ESR2) was assessed in transiently transfected SKBR3 cells using a synthetic reporter gene. In this analysis it was determined that although RAD1901 effectively inhibits E2-dependent activation of an ERE-luciferase reporter by either isoform, it is a more potent inhibitor of ESR1 (100-fold) (Fig. 1B). Similarly, it was demonstrated in MCF7 breast cancer cells that RAD1901 inhibited E2-dependent (a) induction of target gene transcription and (b) stimulation of cell proliferation with an efficacy and potency similar to that of the SERMs 4-hydroxytamoxifen (4OHT) and raloxifene (Ralox) and the SERDs ICI 182,780 (ICI, fulvestrant) and GW7604 (Fig. 1C–D). To assess the activity of RAD1901 in vivo, we conducted a xenograft tumor study in estrogen-treated immunocompromised mice using the well-characterized ESR1-dependent MCF7 cell model. In this study, it was observed that RAD1901 (20mg/kg) inhibited E2-stimulated growth of the tumors with efficacy similar to tamoxifen (20mg/kg). Importantly, RAD1901 and tamoxifen were also shown to suppress the expression of the ESR1-target genes PGR and FHL1 to the same degree in treated tumors, a result that confirms target engagement (Fig. 1E–F).
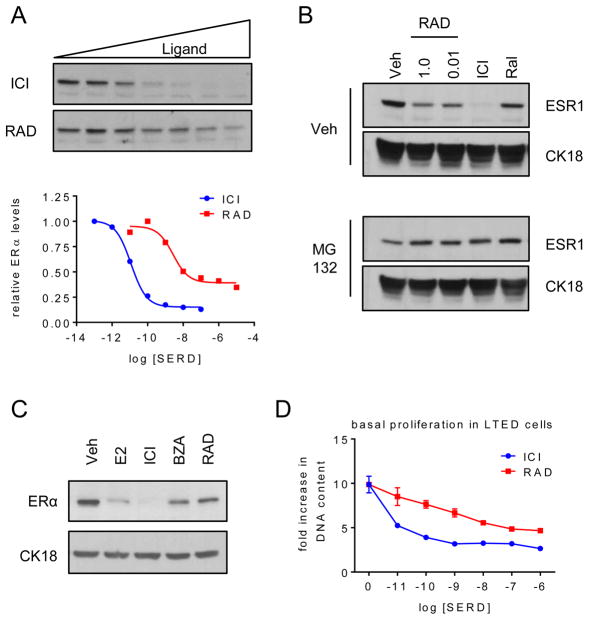
RAD1901 exhibits the pharmacological properties of a Selective Estrogen Receptor Degrader (SERD)
Of late there has been considerable interest in the development of compounds that not only function as ESR1 antagonists, but which also downregulate the expression of this receptor. It was of interest therefore that we demonstrated that ESR1 expression was significantly downregulated in MCF-7 cells treated with RAD1901. Whereas not as effective as the benchmark SERD, fulvestrant, the downregulation of the ESR1 by RAD1901 is likely to be a significant contributor to its antagonist efficacy (Fig. 2A). Interestingly, RAD1901 had no effect on ESR1 mRNA expression (not shown). However, as observed in ICI-treated cells, the downregulation of ESR1 by RAD1901 was completely blocked by pre-treatment of cells with the proteasome inhibitor MG132 (Fig. 2B). Similar results were obtained in the BT483 breast cancer cell line (Supplementary Figure B–D). For comparative purposes, we evaluated ESR1 expression levels in cells treated with tamoxifen, which stabilizes ESR1 expression, and SERDs bazedoxifene (BZA), GW7604 and ICI. These studies reveal that the degree of downregulation of ESR1 by RAD1901 was similar to that achieved by BZA under the same conditions (Fig. 2C). To assess the potential significance of this SERD activity, we evaluated the activity of RAD1901 in LTED MCF7 cells, an accepted model of aromatase resistance in which compounds with ER-antagonist activity alone, like tamoxifen, are minimally effective (not shown). In this assay, it was demonstrated that, like ICI and BZA, RAD1901 downregulated ESR1 expression and inhibited cell proliferation (Fig. 2D). Thus, considering its antagonist activity in several models of breast cancer and its ability to downregulate ESR1, it is appropriate to classify RAD1901 as a SERD.
Fig. 2. RAD1901 downregulates ESR1 expression through receptor degradation.
A) MCF7 cells were treated for 24 hours with ICI (10−13–10−7 M) or RAD (10−11–10−5 M). Expression of ESR1 and loading control cytokeratin 18 (CK18 – Supplementary figure 1A) in whole cell extracts were detected by immunoblot (top). ESR1 levels relative to CK18 were quantitated by densitometry using Adobe Photoshop (bottom). B) MCF7 cells were plated as in Fig. 1B prior to 1 hour pre-treatment with vehicle or MG132 (10 μg/ml), followed by 6 hours of treatment with 10−7 M vehicle, ICI, Ral or RAD (10−8 or 10−6 M). ESR1 expression was detected as in (A). C–D) LTED MCF7 cells were plated in phenol red free media supplemented with FBS that was stripped of growth factors twice using charcoal. C) After 48 hours, cells were treated for 24 hours with E2 (10−7 M) or SERDs (10−6 M) and ESR1 was analyzed as in (A). D) LTED MCF7 cells were treated with ICI or RAD (10−11 – 10−6 M) on days 1, 4, and 6 of an 8 day proliferation assay and analyzed as in Fig. 1.
RAD1901 exhibits dose dependent SERD activity in vivo
The observation that RAD1901 exhibited the pharmacological properties of a SERD was unexpected given that it was (a) identified in screens for compounds that manifest ESR1 agonist activity in the CNS and (b) evaluated in clinical trials as a potential treatment for the vasomotor symptoms (hot flashes) associated with menopause (O’Dea et al. 2010), an indication for which only estrogens have proven effective. However, the results of the clinical trials for hot flashes revealed that RAD1901 exhibited a complex pharmacology. At the lowest dose tested it appeared to effectively suppress hot flashes but was ineffective at the higher doses tested (O’Dea et al. 2010). This inverted U-shaped pharmacology suggested to us that at low doses this compound may have favorable agonist activity, but at higher doses the ability of RAD1901 to induce ESR1 turnover dominates. Thus, we embarked on a series of studies to explore the functional consequences of the complex pharmacological activities of RAD1901 in vivo.
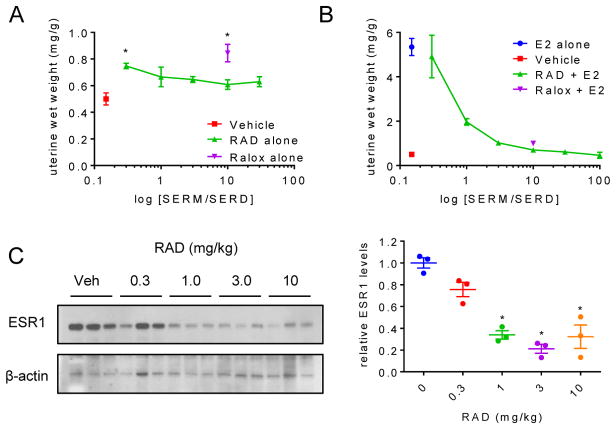
As a first step we evaluated the impact of RAD1901 on uterine wet weight in mice. For this study, increasing doses of RAD1901 was administered daily to ovariectomized C57Bl/6 mice receiving vehicle alone or E2 (10 μg/kg; a physiological replacement dose). A group of mice receiving 10 mg/kg of raloxifene was included for comparative purposes and for reference. When administered as a single agent, a statistically significant increase in uterine weight was observed in those animals receiving the lowest dose of RAD1901 (0.3 mg/kg). At doses of 1 mg/kg and above the uterine wet weights of treated animals were indistinguishable from vehicle treated animals (Fig. 3A). Further, RAD1901 administration was shown to inhibit E2-dependent increases in uterine wet weight (Fig. 3B), an activity that tracked with the dose dependent downregulation of ESR1 expression (Fig. 3C). Notably, we did not observe any decrease in ESR1 expression in animals treated with 0.3 mg/kg, the dose where the agonist activity of RAD1901 in the uterine wet weight assay was observed (Fig. 3C). We conclude from these studies that, as observed in clinical trial for hot flashes, RAD1901 exhibits a complex biphasic pharmacology that manifests as antagonist activity at the higher doses.
Fig. 3. The in vivo pharmacology of RAD1901 is influenced by SERD activity.
Ovariectomized C57Bl/6 mice (n = 5) were treated daily for 3 days with (A) vehicle or (B) estradiol (10 μg/kg) together with vehicle, Ralox (10 mg/kg) or RAD (0.3–100 mg/kg). At euthanasia, body weight as well as uterine wet weight were measured prior to cryopreservation of the uterus. Significant changes in uterine weight observed in animals not receiving estrogen treatment (A) were determined by ANOVA followed by Bonferroni comparison to the vehicle control and are indicated (* p < 0.05). C) ESR1 and β-actin expression in extracts made from pulverized uterine tissues were analyzed by immunoblot as in Fig. 1 (left). ESR1 expression relative to β-actin was quantitated as in Fig. 2 (right). Significant downregulation (* p < 0.05) of ESR1 was determined by ANOVA followed by Bonferroni multiple comparison.
RAD1901 exhibits biphasic activity with respect to ESR1-dependent tumor growth
As shown above, high dose RAD1901 (20mg/kg) inhibited the growth of ESR1-dependent MCF7-cell derived tumors in mice. However, the observation that uterine wet weight was increased in mice treated with doses of RAD1901 that were lower than that required to effect ESR1 turnover highlighted the need to examine whether a similar biphasic pharmacology was manifest in breast tumors. To further evaluate the pharmacology of RAD1901, we conducted a second xenograft tumor study in which MCF7 tumors were established under estrogen stimulation. When tumors reached ~0.1 cm3 volume, estrogen was discontinued and animals were randomized to treatment with vehicle or RAD1901 (0.3, 1, 3 or 10 mg/kg). As observed in the uterine weight assay, RAD1901 exhibited a biphasic response, in that significant stimulation of tumor growth was observed in animals treated with 1 or 3 mg/kg RAD1901 that was not apparent at the higher dose (Fig. 4A). Although certainly less than that which was observed following E2 stimulation (Fig. 1E), the increased tumor volume in the 1 and 3mg/kg groups is significant and of similar magnitude to that which we have reported previously for partial ESR1 agonists (Nelson, et al. 2013). Interestingly, an evaluation of the final tumor size and uterine wet weight of these animals at sacrifice revealed that the pharmacology of RAD1901 is affected by both dose and tissue. Specifically, as reported above in a different strain of mice, stimulation of uterine weight was apparent in mice treated with only the 0.3 mg/kg dose of RAD1901, while tumor size was significantly increased in 1 or 3 mg/kg RAD1901 groups (Fig. 4B). Whereas the expression of classical ESR1 target genes such as PGR (Fig. 4C) and others (MYBL1, HSPB8, FHL1, and CXCL12 – not shown) was observed only in tumors treated with estrogen and was not observed in the tumors in the 1 or 3mg/kg RAD1901 treatment groups (Fig. 4C), RAD1901 induction of AGR2 (Fig. 4D) and others SERM-regulated genes associated with tamoxifen resistance (KRT13, KRT15, AGR3, and RFTN1 – not shown) was observed. Immunoblot analysis of tumor extracts revealed a dose-dependent downregulation of ESR1 by RAD1901 that reflected its actions as an inhibitor of tumor growth (Fig. 4E). Together these data highlight the complex pharmacology of RAD1901 and stress the importance of developing biomarkers that read on the partial agonist activity of the drug and which can be used for dose optimization in clinical studies.
Elucidation of the mechanisms that distinguish RAD1901 from other SERDs
We next sought to determine whether the dose-dependent agonist/antagonist activity of RAD1901 could be observed at the level of target gene regulation. Previously, we reported on the identification of specific sets of ESR1 target genes whose expression was differentially regulated by estrogens and SERMs and which could be used to distinguish between different SERMs and SERDs (Wardell et al. 2012). A subset of these genes, those regulated by a) agonists (with no or minimal response to SERMs), b) SERMs (with no or little response to E2), or c) either agonists or SERMs, were selected to profile RAD1901 activity (Wardell et al. 2012). Reflecting the pharmacology observed in vivo, the expression pattern of these target genes exhibited a biphasic response to RAD1901 with agonist activity been observed at lower doses and more complete antagonist activity apparent at higher doses (Fig. 5A–C and Supplementary Figure 2). These data confirm the unique pharmacology of RAD1901 and suggest that this drug may function by a mechanism that is distinct from other ESR1 downregulators.
It is now generally accepted that, notwithstanding differences in pharmaceutical properties, the pharmacology of ESR1 ligands reflects their influence on the overall structure of the receptor and on the impact which this has on coregulator recruitment. Given the distinct pharmacology exhibited by RAD1901, we hypothesized that it may enable ESR1 to adopt a unique conformation. To address this we took advantage of a conformational profiling tool we reported previously to interrogate the ESR1-RAD1901 complex (Norris, et al. 1999; Wardell et al. 2013). In this assay a modified two-hybrid assay is used to assess the binding of a series of short peptides that survey the protein-protein interaction surfaces on ESR1 that are presented when occupied by different ligands. As shown in Fig 5D, the interaction profile observed in the presence of RAD1901 is completely distinct from any other known ligand. Notable is the ability of RAD1901 to disengage the classical coregulator-binding surface (AF2) as indicated by the decreased interaction with the peptides that report on “agonist activity” (ASC1 and PGC1). No interaction is observed with peptides that report on the ESR1 structures adopted upon binding tamoxifen (αβV) or ICI (βI2). There is however, significant interaction of αII in the presence of RAD1901, a peptide that reports on a cryptic protein-protein interaction surface in the hinge region of the receptor, the significance of which remains to be determined. It is concluded, therefore, that RAD1901 enables ESR1 to assume a unique conformation that is distinct from that apparent upon binding agonists, the SERM tamoxifen, and other known SERDs (Fig. 5D).
In addition to classical agonists, ESR1 transcriptional activity can also be induced by treating cells with growth factors such as EGF, IGF1 or insulin. Whereas the mechanisms underlying this “ligand-independent” activity are likely to be complex, it is widely held that this alternate pathway of activation contributes to resistance to endocrine therapy in breast cancer (Johnston, et al. 2003). Therefore, as a final step in our evaluation of the comparative pharmacology of RAD1901, we evaluated its ability to suppress growth factor dependent activation of ESR1 (Wardell et al. 2013). In this assay, it was determined that although all of the SERMs and SERDs tested inhibited E2-stimulated proliferation, only BZA and ICI efficiently inhibited insulin-stimulated proliferation, while 4OHT, Ralox, and RAD1901 were without effect (Fig. 5E). These results again confirm the unique mechanism of action of RAD1901 but also highlight that this drug may need to be delivered in combination with another drug that inhibits ligand-independent activation of ESR1 in order to achieve maximal clinical response.
Discussion
In this study it was demonstrated that the ESR1 modulator RAD1901 exhibits a complex pharmacology, functioning as a weak partial agonist activity at lower doses of the compound and as an antagonist at higher doses. Whereas the molecular basis for the partial agonist activity remains elusive, it was observed that the binding of RAD1901 enabled the presentation of protein-protein interaction surfaces within the hinge region (flexible structure linking the DNA and hormone binding domains) of ESR1 that we have previously shown to be important for transcriptional activity. Identification of the coregulators that interact with these surfaces on ESR1 will enable a definition of their importance in RAD1901 pharmacology. Importantly, however, it was also observed that as the occupancy of the receptor increases it is targeted for degradation and that this results in a quantitative inhibition of ESR1 signaling. Interestingly, this pharmacological profile resembles that of a classical agonist, such as 17β-estradiol, where the agonist signal is terminated by proteasome-dependent receptor degradation. It has already been established that ability to induce transcriptional activation and receptor turnover are integrally linked activities of ESR1 agonists. The findings of our study are consistent with the model that the pharmacological actions of RAD1901 represent an uncoupling of ESR1-dependent transcriptional activation from degradation. Genetic experiments are underway to define the components of the processes required for ESR1 turnover by RAD1901 and other ligands. The results of these studies should be informative with respect to differences in the mechanisms that regulate ESR1 stability in breast cancer and should help in patient stratification of breast cancer patients where ESR1 is the primary target. Regardless, we conclude that at appropriate doses the SERD activity manifest by RAD1901 may result in useful clinical activity in breast cancer in some settings.
RAD1901 is unique among SERMs and SERDs in that it readily crosses the blood brain barrier. Thus, not surprisingly there was significant interest in the results of clinical studies that evaluated its activity as a treatment for vasomotor instability (hot flashes) (O’Dea et al. 2010). Unfortunately, the results of the studies completed thus far were equivocal. Patients on lower doses of the drug clearly demonstrated benefit whereas exposure to higher doses was ineffective or associated with a worsening of response. We considered potential mechanistic explanations for this pharmacology and herein present data suggesting that RAD1901 manifests partial agonist activity when assessed on gene transcription, in assays of uterine function and in cellular and animal models of breast cancer at doses where ESR1 degradation is not apparent. However, at doses of RAD1901 where ESR1 degradation occurs, we note that the drug quantitatively inhibits the activity of this axis. Studies examining RAD1901 as treatment for hot flashes at doses lower than that originally evaluated appear justified, although it remains to be determined if such protocols would have to include a progestin to mitigate potential liabilities in the uterus that may be manifest at such doses.
The establishment of the relationship between the conformation of ESR1/ligand complexes, coregulator recruitment and phenotypic response was an important advance in efforts to discover new molecules with unique pharmacological activities (Wardell, et al. 2014). Most of these efforts have focused on the identification of SERMs for use in the prevention and treatment of osteoporosis, for breast cancer prevention in high risk patients, and for dyspareunia. Of late however, there has been significant interest in developing SERDs for use in patients with advanced breast cancer. The first SERD approved, ICI, was identified in an empirical manner. However, emerging from specific mechanism-based screens are a series of new, orally bioavailable drugs, that exhibit substantial SERD activity and which all preclinical evidence suggests should have utility in the treatment of advanced disease (Mayer et al. 2013). The most clinically advanced of these molecules, ARN810 (GDC-0810), induces ESR1 turnover by a mechanism distinct from ICI and thus may have advantages as an intervention in certain patient populations (Lai et al. 2015). Bazedoxifene, a SERM, was also determined to induce substantial ESR1 turnover although the mechanism by which this occurs is elusive (Lewis-Wambi et al. 2011; Wardell et al. 2013). The latter molecule is approved in several countries for the treatment and prevention of osteoporosis and near term clinical studies to evaluate its efficacy in breast cancer are anticipated (Komm, et al. 2005). With the number of options available, the challenge, therefore, with a new molecule like RAD1901 is to identify the clinical niche where it might have particular utility in the clinic. In cellular and animal models of breast cancer this drug does not suppress ESR1 activity as well as other SERMs and SERDs, and its complex pharmacology may be problematic in classical dose escalation studies where tumor growth/progression may occur at lower doses. Further, it has been determined that RAD1901 does not inhibit growth factor mediated induction of ESR1 transcriptional activity, a significant liability in our estimation. However, the demonstrated ability of RAD1901 to cross the blood brain barrier, a shortcoming of other SERMs and SERDs, is a significant positive attribute that has led us to propose to the innovators that this drug may have particular utility in the treatment of ESR1 positive Breast Cancer Brain Metastasis (BCBM).
Advancements in systemic breast cancer therapies have led to an unanticipated increase in the incidence of BCBM (Frisk, et al. 2012). This is likely a consequence of the fact that metastasis to the brain is a very slow processes in ESR1-positive breast cancers, and thus more apparent in long-term survivors. However, few treatments can access the brain, one of three most frequent sites of metastasis for breast cancer, leaving targeted or whole brain radiation as the standard of care for patients diagnosed by BCBM (Freedman and Anders 2012). Importantly, in the majority of BCBM occurring in patients diagnosed with ESR1-positive breast tumors, ESR1 expression is retained, and the high expression of aromatase in the brain suggests that the disruption of ESR1 signaling may be beneficial in this setting (Duchnowska, et al. 2012). Indeed, anecdotal evidence would support a role for ESR1 as a therapeutic target in BCBM (Madhup, et al. 2006; Pors, et al. 1991; Salvati, et al. 1993). While several SERDs are currently in development for the treatment of breast cancers that have progressed during endocrine intervention, and their approval is anticipated to be beneficial in managing peripheral disease, the ability of these drugs to cross the blood brain barrier is currently unknown. However, RAD1901 is not only brain penetrative; it was shown to inhibit ESR1 signaling in the vasomotor symptom trial upon dose escalation (O’Dea et al. 2010). Further, fluoroestradiol (FES)-PET imaging recently demonstrated reduced estradiol binding within the brain of healthy volunteers administered a relatively high dose of RAD1901 (Hattersley, et al. 2014). While these analyses do not measure ESR1 levels, as originally claimed, they do confirm substantial target engagement of ESR1 in the brain. Because patients diagnosed with BCBM are likely to have already progressed following endocrine therapies, the utility of RAD1901 in this setting may be dictated by the pharmacology exhibited by RAD1901 in breast tumors resistant to tamoxifen and/or aromatase inhibitors. Regardless, in the absence of a SERD with a less complicated pharmacological profile, RAD1901 may be beneficial in the BCBM setting when combined with additional therapeutic(s) that will ensure the inhibition of growth of peripheral metastases.
Supplementary Material
Acknowledgments
Funding
Supporting funding for all authors was provided by the National Institutes of Health (grant number R37DK048807) and a research grant from Radius Pharmaceuticals.
Footnotes
Declaration of interest
D.P.M. has previously served as a scientific advisory board member for Radius Pharmaceuticals, Inc. D.P.M., S.E.W., and E.R.N. have applied for a patent for the use of RAD1901 for the treatment of breast cancer brain metastases.
References
- Bentrem DJ, Dardes RC, Liu H, Maccgregor-Schafer J, Zapf JW, Jordan VC. Molecular mechanism of action at estrogen receptor alpha of a new clinically relevant antiestrogen (GW7604) related to tamoxifen. Endocrinology. 2001;142:838–846. doi: 10.1210/endo.142.2.7932. [DOI] [PubMed] [Google Scholar]
- Carter D. New global survey shows an increasing cancer burden. American Journal of Nursing. 2014;114:17. doi: 10.1097/01.NAJ.0000444482.41467.3a. [DOI] [PubMed] [Google Scholar]
- Chia S, Gradishar W, Mauriac L, Bines J, Amant F, Federico M, Fein L, Romieu G, Buzdar A, Robertson J, et al. Double-blind, randomized placebo controlled trial of Fulvestrant compared with exemestane after prior nonsteroidal aromatase inhibitor therapy in postmenopausal women with hormone receptor-positive, advanced breast cancer: results from EFECT. Journal of Clinical Oncology. 2008;26:1664–1670. doi: 10.1200/JCO.2007.13.5822. [DOI] [PubMed] [Google Scholar]
- Connor CE, Norris JD, Broadwater G, Willson TM, Gottardis MM, Dewhirst MW, McDonnell DP. Circumventing tamoxifen resistance in breast cancers using antiestrogens that induce unique conformational changes in the estrogen receptor. Cancer Research. 2001;61:2917–2922. [PubMed] [Google Scholar]
- Dallenbach-Hellweg G, Schmidt D, Hellberg P, Bourne T, Kreuzwieser E, Doren M, Rydh W, Rudenstam G, Granberg S. The endometrium in breast cancer patients on tamoxifen. Archives of Gynecology and Obstetrics. 2000;263:170–177. doi: 10.1007/s004040050276. [DOI] [PubMed] [Google Scholar]
- Dardes RC, O’Regan RM, Gajdos C, Robinson SP, Bentrem D, Reyes Adl, Jordan VC. Effects of a new clinically relevant antiestrogen (GW5638) related to tamoxifen on breast and endometrial cancer growth in vivo. Clinical Cancer Research. 2002;8:1995–2001. [PubMed] [Google Scholar]
- Duchnowska R, Dziadziuszko R, Trojanowski T, Mandat T, Och W, Czartoryska-Arlukowicz B, Radecka B, Olszewski W, Szubstarski F, Kozlowski W, et al. Conversion of epidermal growth factor receptor 2 and hormone receptor expression in breast cancer metastases to the brain. Breast Cancer Res. 2012;14:R119. doi: 10.1186/bcr3244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman RA, Anders CK. Treatment of Breast Cancer Brain Metastases. Curr Breast Cancer Rep. 2012;4:1–9. doi: 10.1007/s12609-011-0061-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frisk G, Svensson T, Backlund LM, Lidbrink E, Blomqvist P, Smedby KE. Incidence and time trends of brain metastases admissions among breast cancer patients in Sweden. British Journal of Cancer. 2012;106:1850–1853. doi: 10.1038/bjc.2012.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hattersley G, David F, Harris A, Clarkin M, Banks K, Williams G, Glaudemans A, Doorduin J, Koole M, de Vries E, et al. RAD1901, a novel tissue-selective estrogen receptor degrader (SERD) demonstrates estrogen receptor engagement in a phase 1 clinical study. San Antonio Breast Cancer Meeting; San Antonio, Texas: United States of America; 2014. pp. Abstract OT2-1–10. [Google Scholar]
- Hattersley G, Paquin D, Ho S, Merchenthaler I, Ogasawara A, Nakagawa M, Ogura H, Lyttle CR. RAD-1901, a Novel SERM, has Efficacy in an Animal Model of Vasomotor Symptoms. 89th Annual Meeting of the Endocrine Society; Toronto, Ontario, Canada. 2007. pp. Abstract P1–415. [Google Scholar]
- Jeselsohn R, Yelensky R, Buchwalter G, Frampton G, Meric-Bernstam F, Gonzalez-Angulo AM, Ferrer-Lozano J, Perez-Fidalgo JA, Cristofanilli M, Gomez H, et al. Emergence of constitutively active estrogen receptor-alpha mutations in pretreated advanced estrogen receptor-positive breast cancer. Clinical Cancer Research. 2014;20:1757–1767. doi: 10.1158/1078-0432.CCR-13-2332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston SR, Head J, Pancholi S, Detre S, Martin LA, Smith IE, Dowsett M. Integration of signal transduction inhibitors with endocrine therapy: an approach to overcoming hormone resistance in breast cancer. Clinical Cancer Research. 2003;9:524S–532S. [PubMed] [Google Scholar]
- Komm BS, Chines AA. An update on selective estrogen receptor modulators for the prevention and treatment of osteoporosis. Maturitas. 2012;71:221–226. doi: 10.1016/j.maturitas.2011.11.018. [DOI] [PubMed] [Google Scholar]
- Komm BS, Kharode YP, Bodine PV, Harris HA, Miller CP, Lyttle CR. Bazedoxifene acetate: a selective estrogen receptor modulator with improved selectivity. Endocrinology. 2005;146:3999–4008. doi: 10.1210/en.2005-0030. [DOI] [PubMed] [Google Scholar]
- Lai A, Kahraman M, Govek S, Nagasawa J, Bonnefous C, Julien J, Douglas K, Sensintaffar J, Lu N, Lee KJ, et al. Identification of GDC-0810 (ARN-810), an Orally Bioavailable Selective Estrogen Receptor Degrader (SERD) that Demonstrates Robust Activity in Tamoxifen-Resistant Breast Cancer Xenografts. Journal of Medicinal Chemistry. 2015;58:4888–4904. doi: 10.1021/acs.jmedchem.5b00054. [DOI] [PubMed] [Google Scholar]
- Leo AD, Jerusalem G, Petruzelka L, Torres R, Bondarenko I, Khasanov R, Verhoeven D, Pedrini J, Lichinitser M, Pendergrass K, et al. CONFIRM: A Phase III, randomized, parallel-group trial comparing fulvestrant 250 mg vs fulvestrant 500 mg in postmenopausal women with estrogen receptor-positive advanced breast cancer. Cancer Research. 2009;69:Abstract nr 25. [Google Scholar]
- Lewis-Wambi JS, Kim H, Curpan R, Grigg R, Sarker MA, Jordan VC. The selective estrogen receptor modulator bazedoxifene inhibits hormone-independent breast cancer cell growth and down-regulates estrogen receptor alpha and cyclin D1. Molecular Pharmacology. 2011;80:610–620. doi: 10.1124/mol.111.072249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindahl B, Andolf E, Ingvar C, Ranstam J, Willen R. Adjuvant tamoxifen in breast cancer patients affects the endometrium by time, an effect remaining years after end of treatment and results in an increased frequency of endometrial carcinoma. Anticancer Research. 2008;28:1259–1262. [PubMed] [Google Scholar]
- Madhup R, Kirti S, Bhatt ML, Srivastava PK, Srivastava M, Kumar S. Letrozole for brain and scalp metastases from breast cancer--a case report. Breast. 2006;15:440–442. doi: 10.1016/j.breast.2005.07.006. [DOI] [PubMed] [Google Scholar]
- Mayer I, Bardia A, Dickler M, Manning H, Mahmood U, Ulaner G, Hager J, Rix P, Zack N, Maneval E, et al. Abstract OT3-2-07: Phase I study of ARN-810, a novel selective estrogen receptor degrader, in post-menopausal women with locally advanced or metastatic estrogen receptor positive breast cancer. Cancer Research. 2013;73:Abstract nr OT3-2-07. [Google Scholar]
- Miller CP, Collini MD, Tran BD, Harris HA, Kharode YP, Marzolf JT, Moran RA, Henderson RA, Bender RH, Unwalla RJ, et al. Design, synthesis, and preclinical characterization of novel, highly selective indole estrogens. Journal of Medicinal Chemistry. 2001;44:1654–1657. doi: 10.1021/jm010086m. [DOI] [PubMed] [Google Scholar]
- Nelson ER, Wardell SE, Jasper JS, Park S, Suchindran S, Howe MK, Carver NJ, Pillai RV, Sullivan PM, Sondhi V, et al. 27-Hydroxycholesterol links hypercholesterolemia and breast cancer pathophysiology. Science. 2013;342:1094–1098. doi: 10.1126/science.1241908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris JD, Paige LA, Christensen DJ, Chang CY, Huacani MR, Fan D, Hamilton PT, Fowlkes DM, McDonnell DP. Peptide antagonists of the human estrogen receptor. Science. 1999;285:744–746. doi: 10.1126/science.285.5428.744. [DOI] [PubMed] [Google Scholar]
- O’Dea L, McCarthy D, Guerriero J, Miller C, Hattersley G, Lyttle CR. RAD1901, a Novel Selective Estrogen Receptor Modulator (SERM), Demonstrates Evidence of Efficacy on Postmenopausal Hot Flashes in an Early Phase Human Study. 92nd Annual Meeting of the Endocrine Society; San Diego, California, United States of America. 2010. pp. Abst P1–726. [Google Scholar]
- Perey L, Paridaens R, Hawle H, Zaman K, Nole F, Wildiers H, Fiche M, Dietrich D, Clement P, Koberle D, et al. Clinical benefit of fulvestrant in postmenopausal women with advanced breast cancer and primary or acquired resistance to aromatase inhibitors: final results of phase II Swiss Group for Clinical Cancer Research Trial (SAKK 21/00) Annals of Oncology. 2007;18:64–69. doi: 10.1093/annonc/mdl341. [DOI] [PubMed] [Google Scholar]
- Pors H, von Eyben FE, Sorensen OS, Larsen M. Longterm remission of multiple brain metastases with tamoxifen. Journal of Neuro-Oncology. 1991;10:173–177. doi: 10.1007/BF00146879. [DOI] [PubMed] [Google Scholar]
- Riggins RB, Schrecengost RS, Guerrero MS, Bouton AH. Pathways to tamoxifen resistance. Cancer Letters. 2007;256:1–24. doi: 10.1016/j.canlet.2007.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson J, Llombart-Cussac A, Feltl D, Dewar J, Jasiówka M, Hewson N, Rukazenkov Y, Ellis M. Fulvestrant 500 mg versus anastrozole as first-line treatment for advanced breast cancer: overall survival from the phase II ‘FIRST’ study. San Antonio Breast Cancer Symposium; San Antionio, Texas, USA. 2014. pp. Abstract S6–04. [Google Scholar]
- Robertson J, Nicholson R, Bundred N, Anderson E, Rayter Z, Dowsett M, Fox J, Gee J, Webster A, Wakeling A, et al. Comparison of the short-term biological effects of 7alpha-[9-(4,4,5,5,5-pentafluoropentylsulfinyl)-nonyl]estra-1,3,5, (10)-triene-3,17beta-diol (Faslodex) versus tamoxifen in postmenopausal women with primary breast cancer. Cancer Research. 2001;61:6739–6746. [PubMed] [Google Scholar]
- Robinson DR, Wu YM, Vats P, Su F, Lonigro RJ, Cao X, Kalyana-Sundaram S, Wang R, Ning Y, Hodges L, et al. Activating ESR1 mutations in hormone-resistant metastatic breast cancer. Nature Genetics. 2013;45:1446–1451. doi: 10.1038/ng.2823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvati M, Cervoni L, Innocenzi G, Bardella L. Prolonged stabilization of multiple and single brain metastases from breast cancer with tamoxifen. Report of three cases. Tumori. 1993;79:359–362. doi: 10.1177/030089169307900516. [DOI] [PubMed] [Google Scholar]
- Toy W, Shen Y, Won H, Green B, Sakr RA, Will M, Li Z, Gala K, Fanning S, King TA, et al. ESR1 ligand-binding domain mutations in hormone-resistant breast cancer. Nature Genetics. 2013;45:1439–1445. doi: 10.1038/ng.2822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardell SE, Ellis MJ, Alley HM, Eisele K, VanArsdale T, Dann SG, Arndt KT, Primeau T, Griffin E, Shao J, et al. Efficacy of SERD/SERM Hybrid-CDK4/6 inhibitor combinations in models of endocrine therapy resistant breast cancer. Clinical Cancer Research. 2015 doi: 10.1158/1078-0432.CCR-15-0360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardell SE, Kazmin D, McDonnell DP. Research resource: Transcriptional profiling in a cellular model of breast cancer reveals functional and mechanistic differences between clinically relevant SERM and between SERM/estrogen complexes. Molecular Endocrinology. 2012;26:1235–1248. doi: 10.1210/me.2012-1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardell SE, Marks JR, McDonnell DP. The turnover of estrogen receptor alpha by the selective estrogen receptor degrader (SERD) fulvestrant is a saturable process that is not required for antagonist efficacy. Biochemical Pharmacology. 2011;82:122–130. doi: 10.1016/j.bcp.2011.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardell SE, Nelson ER, Chao CA, McDonnell DP. Bazedoxifene exhibits antiestrogenic activity in animal models of tamoxifen-resistant breast cancer: implications for treatment of advanced disease. Clinical Cancer Research. 2013;19:2420–2431. doi: 10.1158/1078-0432.CCR-12-3771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardell SE, Nelson ER, McDonnell DP. From empirical to mechanism-based discovery of clinically useful Selective Estrogen Receptor Modulators (SERMs) Steroids. 2014;90:30–38. doi: 10.1016/j.steroids.2014.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willson TM, Norris JD, Wagner BL, Asplin I, Baer P, Brown HR, Jones SA, Henke B, Sauls H, Wolfe S, et al. Dissection of the molecular mechanism of action of GW5638, a novel estrogen receptor ligand, provides insights into the role of ER in bone. Endocrinology. 1997;138:3901–3911. doi: 10.1210/endo.138.9.5358. [DOI] [PubMed] [Google Scholar]
- Wilson T. Oct 28 A method of preventing or treating estrogen-dependent diseases and disorders. United States: Glaxo Wellcome Inc; 1997. [Google Scholar]
- Wittmann BM, Sherk A, McDonnell DP. Definition of functionally important mechanistic differences among selective estrogen receptor down-regulators. Cancer Research. 2007;67:9549–9560. doi: 10.1158/0008-5472.CAN-07-1590. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.