Abstract
Background:
It is said that renal transplantation lithiasis is rare. However, literature has some different frequencies in this field and most of the studies related to this issue are case reports. Also the exact effect of this complication on the graft survival rate is not clear.
Objectives:
To determine the prevalence of nephrolithiasis among kidney transplant recipients and evaluate its association with the graft survival.
Methods:
We conducted a retrospective study to determine the prevalence of renal stone among 574 kidney transplant patients aged ≥18 years who had undergone renal transplantation in Baqiyatallah Transplant Center between 1990 and 2010. Cox regression analysis was used to determine the effect of renal stone on the graft survival.
Results:
The mean±SD follow-up time was 55±53 months. Kidney stones were diagnosed in 31 (4.4%) of all 574 kidney transplants studied. Cox regression analysis revealed that nephrolithiasis after transplantation had no significant effects on the survival of the transplanted kidney (OR 1.04, CI: 0.708–1.54).
Conclusion:
For the first time, we showed that nephrolithiasis in recipients does not have a significant effect on the transplant survival.
Key Words: Lithiasis, Calculi, Kidney transplantation, Graft survival
INTRODUCTION
In 1975, Rattiazzi, et al, for the first time described renal transplant lithiasis [1]. With a prevalence of 0.4% to 1%, some researchers said that lithiasis in the kidney transplantation is rare [2, 3]. Lancina Martín, et al, however, after evaluation of 794 renal grafts reported a prevalence of 2% for post-transplantation lithiasis [4]. Most of the studies related to post-kidney transplantation lithiasis are case reports. Narayana, et al, reported nephrolithiasis in a patient received cadaveric kidney transplant with the probable etiology of urinary tract infection (UTI) [5]. Rosenberg and collegues reported renal stones four months after kidney transplantation in a renal allograft. They thought renal tubular acidosis (RTA), UTI, and hyperparathyroidism could be the three major reasons for kidney transplant lithiasis [6]. In a case report in 1990, Sola, et al, reported a large staghorne calculus in renal pelvis five months after transplantation and said that purine metabolism in recipients with past history of gout should be taken into account [7]. Yigit, et al, after evaluation of 125 renal transplantation reported only five patients with allograft kidney stone included de novo lithiasis in two cadaveric donor-gifted in one and two cases with living related donor. UTI and existence of a double J-stent have been proposed as predisposing factors for de novo lithiasis in this study [8]. Pena, et al, have reported two renal calculi among 221 children with kidney transplants. Hyperparathyroidism and idiopathic hypercalcinuria have been considered the etiology for nephrolithiasis in this paper [2]. Therefore, kidney transplantation lithiasis has been described with different prevalence in the literature. However, the important questions to be answered are the effect of the transplantation lithiasis on the transplant survival, and whether living or deceased kidney transplants affect the development of nephrolithiasis after transplantation?
The objective of this study was to determine the prevalence of nephrolithiasis in kidney transplant recipients and also evaluate the effect of nephrolithiasis on the graft survival.
PATIENTS AND METHODS
We conducted a retrospective observational study to determine the prevalence of renal stone among 574 kidney transplant recipients aged ≥18 years who had undergone renal transplantation in Baqiyatallah Transplant Center between 1990 and 2010. Patients included all registered with the database of the renal transplant patients of Nephrology and Urology Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran. All patients received a kidney transplant for the first time. Living- and deceased-donor kidney transplants were included in this study. The study was approved by the local Ethics Committee of Baqiyatallah University of Medical Sciences. The patients received triple immunosuppressive agents including cyclosporine, mycophenolate mofetil or azathioprine, and prednisolone.
The data collected for the current study were age and sex of recipient and donor; history of cigarette smoking and opium addiction in recipients; history of dialysis; the underling disease of end-stage renal disease (ESRD) including diabetes mellitus (DM), hypertension (HTN), obstructive uropathy (OU) with and without renal stone, vesicourethral reflux (VUR), glomerulonephritis (GN), and autosomal dominant polycystic kidney disease (ADPKD); cytomegalovirus (CMV) infection; hospitalization after transplantation; consumption of allopurinol and calcitriol (based on available information about medicines in our database); systolic and diastolic blood pressures; as well as serum alkaline phosphatase (ALP), uric acid, phosphorus (P), calcium (Ca), and creatinine (Cr). The diagnosis of kidney stones after transplant was confirmed with ultrasonography. All laboratory values were recorded at three months, one year, and the last follow-up visit. It should be noted that the end-point for the calculation of graft survival was “graft loss.”
Statistical Analysis
The SPSS® ver 21 for Windows® was used for data analyses. Qualitative variables were expressed as frequencies and percentages. Quantitative variables were expressed as mean±SD. Continuous data were compared by Student’s t test; categorical data were analyzed by χ2 test. Cox regression analysis was used to determine the association of nephrolithiasis with the graft survival. A p value <0.05 was considered statistically significant.
RESULTS
A total of 574 kidney transplant recipients (378 males and 196 females) was studied. They received kidney from 493 male and 81 female donors. The transplants came from either deceased (n= 44) or living donors (n= 533). The mean±SD ages of recipients and donors at transplantation were 38.7±13.7 and 28.2±5.8 years, respectively. The mean±SD follow-up was 55±53 months. Kidney stones were diagnosed in 25 (4.4%) of 574 kidney transplants studied. Cigarette smoking was found in 2.9% of recipients and 11.5% of donors; there was a history of opium addiction in 1% of recipients and 4.3% of donors. In neither donors nor recipients, age, sex, cigarette smoking, and opium addiction had significant associations with nephrolithiasis after transplantation. No significant difference in the prevalence of nephrolithiasis was observed between transplants from deceased and living donors (p=0.58). The mean±SD duration of dialysis recipients was 19.9±26.0 months. There was no significant association between history of dialysis and stone formation (p=0.63).
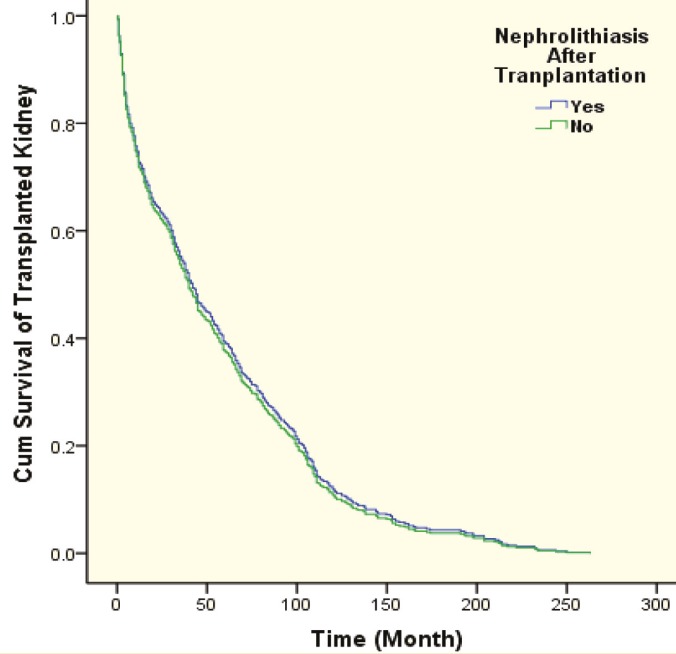
In majority of the studied recipients, the reason for ESRD was unknown. However, among patients with determined etiology, DM and HTN were the most common reasons for ESRD (Table 1). Prevalence of post-transplantation stone formation stratified by the cause of ESRD is shown in Table 2. Based on the table 2, among these causes of ESRD, only obstructive uropathy due to renal stone had a statistically significant association with the nephrolithiasis after transplantation. Cox regression analysis revealed that nephrolithiasis after transplantation have no significant association with the survival of the transplanted kidney (OR 1.04 CI: 0.708-1.54 p=0.824). Figure 1 completely confirms this finding and shows that the survival rate for kidney transplantation in recipients with and without stone is approximately same.
Table 1.
Prevalence of ESRD causes in recipients
| Cause of ESRD | Prevalence (%) |
|---|---|
| DM | 9.7 |
| HTN | 8.8 |
| Obstructive uropathy due to renal stone | 1.7 |
| Obstructive uropathy other than renal stone | 1.2 |
| VUR | 0.7 |
| GN | 8.6 |
| ADPKD | 5.9 |
| Unknown | 62.8 |
DM: diabetes mellitus; HTN: hypertension; VUR: vesicoureteral reflux; GN: glomerulonephritis; ADPKD: autosomal dominant polycystic kidney
Table 2.
Frequency of nephrolithiasis stratified by cause of ESRD
| Cause of ESRD | Prevalence | p value |
|---|---|---|
| DM | 3.6% | 0.5 |
| HTN | 3.9% | 0.6 |
| Obstructive uropathy due to renal stone | 40% | <0.001 |
| OU | 14.3% | 0.2 |
| VUR | 0% | 0.6 |
| GN | 4% | 0.6 |
| ADPKD | 11.8% | 0.08 |
DM: diabetes mellitus; HTN: hypertension; OU: obstructive uropathy; VUR: vesicoureteral reflux; GN: glomerulonephritis; ADPKD: autosomal dominant polycystic kidney
Figure 1.
Cumulative survival curve for kidney transplantation for recipients with and without post-transplantation nephrolithiasis
Allopurinol and calcitriol were used in 59 (10.2%) and 247 (42.7%) recipients, respectively. The prevalence of nephrolithiasis in patients who were taking calcitriol was significantly (p=0.01) lower than those who were not (2.4% [n=6] vs 7.2% [n=24]). Using of allopurinol had also a significant effect on the renal stone formation (p=0.01). Available laboratory data and blood pressure for kidney transplant patients at three-month, one-year and the last follow-up visits did not have a significant effect on the stone formation (Table 3).
Table 3.
Mean±SD of laboratory data and blood pressure at follow-up visits
| Parameter | 3 monthof follow up | one year of follow up | follow-up visits |
|---|---|---|---|
| Alkaline phosphatase | 222±165 | — | 220±140 |
| Uric Acid | 5.7±1.6 | 6.3±1.9 | 6.5±1.9 |
| phosphorus | — | — | 3.88±0.85 |
| calcium | — | — | 9.22±0.88 |
| Creatinine | — | — | 1.92±1.52 |
| Systolic blood pressure | 127±17 | 129±19 | 129±20 |
| Diastolic blood pressure | 75±13 | 75±12 | 75±13 |
DISCUSSION
We found that stone formation after nephrolithiasis did not affect the survival of the transplanted kidney. It is thought that renal transplant lithiasis could lead to obstruction and if this situation keeps on, could lead to loss of kidney function or even acute rejection [3, 9]. However, based on the results of Cox regression analysis, post-transplantation nephrolithiasis did not affect the graft survival. To the best of our knowledge, this is the first study that evaluated this issue.
As mentioned above, lithiasis has been reported as a rare complication in kidney transplantation. However, most of the studies are case reports. Furthermore, in few reported studies the variance in the reported prevalence rates is large. In our study we followed 549 kidney recipients for a mean of 55 months and observed only 31 patients (5.3%) with nephrolithiasis. Moreover, it should be taken into account that this frequency depended on the follow-up time. UTI, RTA, hyperparathyroidism, double J catheter, hypercalcinuria have been reported as probable etiologies for post-transplantation lithiasis [2, 6, 8, 10]. In our study among the reasons mentioned for ESRD, only obstructive uropathy due to stone had a significant association with post-transplantation nephrolithiasis. We also found that age, gender, cigarette smoking and addiction in both donors and recipients did not have a significant association on the stone formation after kidney transplantation. To the best of our knowledge, this is the first study that evaluated the association between these variables and post-transplantation lithiasis.
Another important subject that was addressed in this study was the effect of living and deceased donors on post-transplantation lithiasis. Donor-gifted stone can be proposed for both living and deceased donors [8]. We could not find any significant difference in the rate of post-transplantation lithiasis between these two groups of donors. Data about the effect of renal stones existing in living donors on the risk of transplantation lithiasis is limited. Kim, et al, studied 294 kidney transplantation and found 11 donated allografts with stone. However, only one recipient developed symptomatic nephrolithiasis due to hyperoxaluria [11]. Based on the American and British guidelines, current nephrolithiasis in donors is a relative contraindication for donation [12, 13]. However Ennis and coworkers conducted a survey on the US kidney transplant program in 2009, found an increased tendency towards accepting donors with a history of kidney stones [14]. In accord to this finding, Rizkala, et al, studied 54 kidney transplants and found no case of lithiasis on recipients and finally concluded that small caliceal stones in donors should not be considered as an exclusion criterion for living donors in kidney transplantation [15]. It has also been shown that in Germany, 96% of kidney transplantation centers accept donors with a history of nephrolithiasis, however, the rate for donors with current nephrolithiasis 36% of centers do so. Comparison of urological and surgical centers in this study revealed that donors with nephrolithiasis were more accepted in urological centers than surgical centers [13].
The main limitation in our project was related to its retrospective design. We did not have enough information about composition, number and size of the stones in our database. So we could not use these data in the analyses.
In conclusion, it seems that nephrolithiasis in recipients does not have a significant effect on the transplant survival. Further studies are needed to consider other potentially important variables that might affect this issue. The variables to be considered include composition, number, and size of stones.
Acknowledgements: We would like to thank all of the participants in this study and the personnel of our Kidney Transplant Center for their kind cooperation.
CONFLICTS OF INTEREST: None declared.
References
- 1.Rattiazzi LC, Simmons RL, Markland C. et al. Calculi complicating renal transplantation into ileal conduits.Urology. 1975;5:29–31. doi: 10.1016/0090-4295(75)90296-4. [DOI] [PubMed] [Google Scholar]
- 2.Pena DR, Fennell RS, Iravani A, et al. Renal calculi in pediatric renal transplant recipients. Child Nephrol Urol. 1990;10:58–60. [PubMed] [Google Scholar]
- 3.Stravodimos KG, Adamis S, Tyritzis S, et al. Renal transplant lithiasis: analysis of our series and review of the literature. J Endourol. 2012;26:38–44. doi: 10.1089/end.2011.0049. [DOI] [PubMed] [Google Scholar]
- 4.Lancina Martín JA, García Buitrón JM, Díaz Bermúdez J, et al. [Urinary lithiasis in transplanted kidney] Arch Esp Urol. 1997;50:141–50. [PubMed] [Google Scholar]
- 5.Narayana AS, Loening S, Culp DA. Kidney stones and renal transplantation. Urology. 1978;12:61–3. doi: 10.1016/0090-4295(78)90369-2. [DOI] [PubMed] [Google Scholar]
- 6.Rosenberg JC, Arnstein AR, Ing TS, et al. Calculi complicating a renal transplant. Am J Surg. 1975;129:326–30. doi: 10.1016/0002-9610(75)90251-2. [DOI] [PubMed] [Google Scholar]
- 7.Solà R, del Río G, Villavicencio H. Staghorn renal stone in a transplanted kidney. Urol Int. 1990;45:188–9. doi: 10.1159/000281706. [DOI] [PubMed] [Google Scholar]
- 8.Yiğit B, Aydin C, Titiz I, et al. Stone disease in kidney transplantation. Transplant Proc. 2004;36:187–9. doi: 10.1016/j.transproceed.2003.11.063. [DOI] [PubMed] [Google Scholar]
- 9.Van Gansbeke D, Zalcman M, Matos C, et al. Lithiasic complications of renal transplantation: the donor graft lithiasis concept. Urol Radiol. 1985;7:157–60. doi: 10.1007/BF02926876. [DOI] [PubMed] [Google Scholar]
- 10.Shamsa A. Results of 226 live renal transplantations. Br J Urol. 1997;80(SUPPL. 2):153. [Google Scholar]
- 11.Kim IK, Tan JC, Lapasia J, et al. Incidental kidney stones: a single center experience with kidney donor selection. Clin Transplant. 2012;26:558–63. doi: 10.1111/j.1399-0012.2011.01567.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kasiske BL, Ravenscraft M, Ramos EL, et al. The evaluation of living renal transplant donors: clinical practice guidelines. Ad Hoc Clinical Practice Guidelines Subcommittee of the Patient Care and Education Committee of the American Society of Transplant Physicians. J Am Soc Nephrol. 1996;7:2288–313. doi: 10.1681/ASN.V7112288. [DOI] [PubMed] [Google Scholar]
- 13.Giessing M, Fuller F, Tuellmann M, et al. Attitude to nephrolithiasis in the potential living kidney donor: a survey of the German kidney transplant centers and review of the literature. Clin Transplant. 2008;22:476–83. doi: 10.1111/j.1399-0012.2008.00812.x. [DOI] [PubMed] [Google Scholar]
- 14.Ennis J, Kocherginsky M, Schumm LP, et al. Trends in kidney donation among kidney stone formers: a survey of US transplant centers. Am J Nephrol. 2009;30:12–8. doi: 10.1159/000197115. [DOI] [PubMed] [Google Scholar]
- 15.Rizkala E, Coleman S, Tran C, et al. Stone disease in living-related renal donors: long-term outcomes for transplant donors and recipients. J Endourol. 2013;27:1520–4. doi: 10.1089/end.2013.0203. [DOI] [PubMed] [Google Scholar]