Abstract
Objective
To evaluate and adjust for American Indian and Alaska Native (AI/AN) racial misclassification in two hospital discharge datasets in the Pacific Northwest.
Data Sources/Study Setting
Oregon (2010-2011) and Washington (2011) hospital discharge datasets were linked with the Northwest Tribal Registry (NTR), a registry of AI/AN individuals who accessed services at Indian health facilities in the Northwest.
Study Design
Record linkage was used to match state hospital records to the NTR. A state record was considered misclassified if it matched the NTR and was coded as non-AI/AN or missing race data. Effect of misclassification was evaluated by comparing prelinkage and postlinkage, age-adjusted hospital discharge rates.
Data Collection/Extraction Methods
Researchers used Link Plus 2.0 software (Atlanta, GA, USA) for linkages and SAS 9.4 (Cary, NC, USA) for statistical analyses.
Principal Findings
In Oregon, 55.4 percent of matching records were misclassified (66.5 percent miscoded white, and 22.1 percent were missing race information). In Washington, 44.9 percent of matching records were misclassified (61.8 percent miscoded white, and 32.7 percent were missing race information). Linkage increased ascertainment of AI/AN hospitalizations by 31.8 percent in Oregon and 33.9 percent in Washington. Linkage increased the rate ratio (RR) for AI/AN hospitalizations in comparison to non-Hispanic whites (NHW) from 0.81 to 1.07 in Oregon, and from 1.21 to 1.62 in Washington.
Conclusion
Correction of race in hospital discharge datasets through linkage with a reference file of known AI/AN individuals is an important first step before analytic research on AI/AN health care in the Pacific Northwest can be accomplished with administrative datasets.
Keywords: Hospital discharge, hospitalizations, data quality, racial misclassification, disparities, American Indian/Alaska Native, Pacific Northwest, Oregon, Washington
American Indians and Alaska Natives (AI/AN) have worse physical and mental health status than other racial and ethnic groups in the United States, and they face barriers in receiving adequate and timely health services (Roberts and Jones 2004; Barnes, Adams, and Powell-Griner 2010). The Indian Health Service (IHS) is the federal agency charged with providing health care to members of federally recognized AI/AN tribes, corporations, and villages. In the Pacific Northwest states of Idaho, Oregon, and Washington, these services are provided by IHS-operated clinics, tribally operated clinics, and Urban Indian Health Organizations. However, a sizeable proportion of the estimated 344,600 AI/AN in the Northwest do not receive health care from the IHS; in 2013, the IHS had 197,188 patients registered within the three-state area, and 60 percent of these had at least one patient encounter in the past 3 years (Indian Health Service 2014). Further, there are no inpatient hospital facilities within the Indian health system in these states. Therefore, all inpatient hospital services for Northwest AI/AN are provided through nonfederal hospitals.
Hospital discharge data are used in a wide variety of public health and health care applications and provide valuable information on health care utilization and health disparities (Schoenman et al. 2005). However, information on the race and ethnicity of patients may not be systematically or accurately collected in these datasets. AI/AN are frequently misclassified in surveillance and administrative data systems, with misclassification ranging from 30 to 70 percent (Kressin et al. 2003; Puuka, Stehr-Green, and Becker 2005; Johnson et al. 2009; Hoopes et al. 2010). Compared with other race groups, AI/AN have the lowest levels of agreement (approximately 60 percent) between self-reported race and race assigned in medical records (Boehrmer et al. 2002; Kressin et al. 2003; Gomez et al. 2005). Data quality issues compound other statistical challenges surrounding small population/cell size and make it difficult to accurately measure AI/AN health disparities at the state and local levels, where actions to address disparities are most likely to occur (Bilheimer and Klein 2010).
Record linkage of datasets with IHS, tribal, and urban clinic registration data is an effective strategy for reducing AI/AN misclassification in administrative datasets (Becker et al. 2002; Puuka, Stehr-Green, and Becker 2005; Foote et al. 2007; Johnson et al. 2009; Hoopes, Vinson, and Lopez 2012). Since 1999, the Improving Data and Enhancing Access—Northwest (IDEA-NW) project, part of the Northwest Tribal Epidemiology Center and Northwest Portland Area Indian Health Board, has conducted record linkage studies with state health datasets in Idaho, Oregon, and Washington. The current study evaluates AI/AN misclassification within Oregon and Washington’s hospital discharge data with the aim of providing more reliable measurements of AI/AN hospitalizations.
Methods
Oregon hospital inpatient discharge data for 2010–2011 (N = 746,196 records) were provided by the Office for Oregon Health Policy and Research (OHPR) at the Oregon Health Authority. The data exclude Veterans Administration hospitals, specialty or rehabilitative care hospitals, long-term care facilities, and psychiatric hospitals. To be considered an inpatient discharge, the patient must have stayed a minimum of 1 day in the hospital. Washington state inpatient discharge data for 2011 (N = 648,383 records) were provided by the Comprehensive Hospital Abstract Reporting System (CHARS) at the Washington State Department of Health. CHARS contains coded hospital inpatient discharge information derived from hospital billing systems from all nonfederal and non-State-run hospitals in Washington. Idaho currently does not maintain a statewide hospital discharge data system, precluding a linkage analysis for that state. All project protocols were reviewed and approved by the Portland Area IHS Institutional Review Board (IRB), the OHPR administration for the Oregon linkage, and the Washington State IRB for the Washington linkage.
Oregon and Washington differ in their laws on the collection of hospital discharge race data. Under Oregon Revised Statute 442.120 and detailed in Oregon Administrative Rule 409-022-0100 through 409-022-0080, OHPR requires that all Oregon hospitals collect patient race and ethnicity data (Oregon Health Authority 2013); CHARS recommends that hospital staff collect race and ethnicity data, but it is not required by law (Washington State Department of Health [WA DOH] 2014). Both states’ data contain separate race and ethnicity fields and follow the standards set by the Office of Management and Budget for race and ethnicity reporting; however, the Oregon data contain one race field (which best describes the race of the patient), while Washington has multiple race fields (up to five) for multiracial patients.
The Northwest Tribal Registry (NTR) is a demographic dataset of AI/AN individuals who accessed services at Indian health facilities in Idaho, Oregon, or Washington. The NTR is updated annually and maintained by the IDEA-NW project. The purpose of the NTR is to augment Northwest state health datasets with additional AI/AN race information through record linkages. The NTR represents an estimated 66 percent of the Oregon AI/AN population and 81 percent of the Washington AI/AN population as self-identified in the Census (Northwest Portland Area Indian Health Board 2012). The NTR used for this study contained a total of 208,132 AI/AN patient records. The majority (89.5 percent) of NTR records were from the Portland Area IHS (1986–2012). Exactly, 5.1 percent of NTR records were from the Seattle Indian Health Board (SIHB, an Urban Indian Health Organization located in the Puget Sound region of Washington) (2007–2012), and the remaining 5.4 percent of records were from a tribally operated clinic in the South Puget Sound region of Washington, 2005–2011. To be eligible to receive services at an IHS or tribal facility, patients must demonstrate current enrollment in a federally recognized tribe or prove descent from an enrolled member. The SIHB and some tribal facilities provide services to non-AI/AN or AI/AN who are not enrolled in federally recognized tribes. Specifically, the SIHB is designated as a Federally Qualified Health Center and offers services to anyone in need of assistance. However, because of the attention paid to sources of funding for services provided, AI/AN status is carefully documented in these facilities, either by self-report or proof of enrollment or descent. Thus, the NTR includes both documented and self-reported race data.
Data linkages aim to identify two records in two datasets that represent the same person (Johnson et al. 2009). Probabilistic record linkage employs algorithms to identify matching records between two files, even when there are minor differences in the matching fields (e.g., misspelled names, transposed digits in a birth date). We used Link Plus (version 2.0; Atlanta, GA, USA), a probabilistic record linkage software from the Centers for Disease Control and Prevention (CDC), to match records from the NTR to hospital discharge records. Link Plus uses a linkage algorithm to match records based on user-specified blocking and matching variables. Link Plus assigns each variable a score based on the m-probability (the probability that the variables agree for true matches) reduced by the u-probability (the probability that the variables agree by chance for false matches). Variables such as social security number, date of birth, and last name are given more weight than first name, middle name, and gender. The total match score for a record pair is the sum of weighted scores across all matching variables. Higher scores indicate greater probability of a match.
For the Oregon linkage, we used last name (using the NYIIS phonetic system) and date of birth as blocking variables, and last name, first name, middle initial, date of birth, gender, and patient zip code as matching variables. We matched Washington records on these same blocking and matching variables, with the addition of the last four digits of the patient’s social security number as a blocking variable (this variable was not provided by OPHR, so was not used for Oregon). State of residence was used to aid in clerical review for both states, but it was not included as a matching variable.
We used the cut-off values recommended by Link Plus to determine the range of scores for clerical review. The upper cut-off for clerical review was the highest score from each linkage—40.7 for Oregon in 2010, 39.1 for Oregon in 2011, and 49.3 for Washington in 2011. The lower cut-off value of 7.0 was well below the beginning of nonmatches, and it is a conservative lower cut-off value. Reviewers then defined further cut-off values to determine true clerical reviews. Clerical reviews were conducted for records with scores between 14.2 and 25.2 for 2010 Oregon data, between 13.0 and 22.6 for 2011 Oregon data, and between 12.0 and 19.0 for 2011 Washington data. Potential matches with scores between these values were manually reviewed by 1–2 project staff members; clerical reviewers assigned match status for uncertain pairs, and uncertain matches were determined by consensus where possible. Project staff conducting clerical reviews have completed linkage training from the CDC and have conducted prior NTR linkages.
Reviewers determined match status by considering (in order of importance): score, last four digits of SSN (Washington only), date of birth, last and first name (considering that females’ last names may change and that members of the same family may have the same name across generations), middle initial, gender, zip code, and state of residence. On average, approximately 2.8 percent of potential matches resulting from the linkages were sent for clerical review. After clerical review, matched pairs (i.e., records in both the NTR and state dataset) were reported back to the state. After each linkage, IDEA-NW retained a deidentified dataset with record-level information for analysis.
A case of AI/AN misclassification was defined as a state record that matched the NTR and was either missing race data or coded as a race other than AI/AN in the state file. Prelinkage AI/AN included records with any mention of AI/AN race in the state dataset prior to linkage. Postlinkage AI/AN included prelinkage AI/AN, and any records that matched with the NTR but were not coded AI/AN in the state dataset (i.e., misclassified AI/AN records). Hospital records that were missing race information and did not match to the NTR were excluded from the pre- and postlinkage analyses.
Hospital discharge rates per 100,000 were calculated using Census bridged-race population estimates as the denominator (National Center for Health Statistics 2012). Bridged-race estimates account for differences in race data collection between the current 31 race categories used since Census 2000, and the previously used four race categories as specified under the 1977 OMB standards (Asian or Pacific Islander, black or African American, AI/AN, or white). Rates were age-adjusted to the 2000 U.S. standard population in 5-year age groupings. Rate ratios (RR) were used as a comparative measure of rates between AI/AN and non-Hispanic white (NHW) populations within each state. RR 95 percent confidence intervals (CI) were calculated; the threshold for statistical significance was set at p < .05 for all statistical tests. All statistical analyses were conducted using SAS (version 9.4; SAS Institute Inc., Cary, NC, USA).
Results
Oregon, 2010–2011
Of the 746,196 Oregon hospital discharge records from 2010 to 2011 that were sent for linkage, 5,062 matched to the NTR. Of these matched records, 2,806 (55.4 percent) were misclassified non-AI/AN (Figure1). Among misclassified records, 1,866 (66.5 percent) were coded white in the state dataset, while 620 (22.1 percent) were missing all race information (Figure1). Linkage increased the number of AI/AN records from 8,812 to 11,618 and improved ascertainment of AI/AN hospitalizations by 31.8 percent (Table1).
Figure 1.
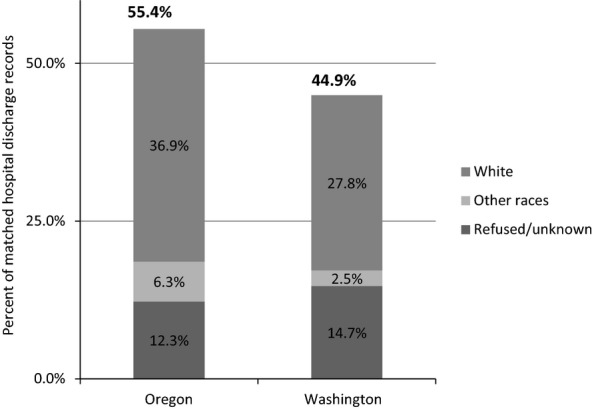
Race Coding Distribution of Misclassified AI/AN Hospitalization Records in Oregon (2010–2011) and Washington (2011) That Matched to the NTR
Table 1.
Characteristics of Misclassified AI/AN Hospitalizations by State
| Oregon 2010–2011 (N = 746,196 records) | Washington 2011 (N = 648,383 records) | |||
|---|---|---|---|---|
| n | % | n | % | |
| Prelinkage AI/AN | 8,812 | 1.2 | 10,812 | 1.7 |
| Postlinkage AI/AN | 11,618 | 1.6 | 14,472 | 2.2 |
| Increased AI/AN ascertainment† | 2,806 | 31.8 | 3,660 | 33.9 |
Percent increase in the proportion of hospital discharge records classified as AI/AN in the 2010–2011 Oregon hospital discharge dataset.
AI/AN, American Indian/Alaska Native; NTR, Northwest Tribal Registry.
Comparing prelinkage and postlinkage AI/AN hospitalizations, the age-adjusted rate of AI/AN hospital discharge increased by approximately 33.5 percent, from 6,348 to 8,380 hospitalizations per 100,000 (Table2). The addition of linkage-identified AI/AN changed the direction of the relationship between the hospital discharge rates for AI/AN versus NHW—the prelinkage AI/AN rate was lower than NHW (RR = 0.81, 95 percent CI: 0.79–0.82), while the postlinkage AI/AN rate was higher than the NHW rate (RR = 1.07, 95 percent CI: 1.04–1.09) (Figure2).
Table 2.
Prelinkage and Postlinkage Age-Adjusted Hospital Discharge Rates by Race and State
| AI/AN Rates per 100,000 | NHW Rates per 100,000 | |||
|---|---|---|---|---|
| Prelinkage Rate (95% CI) | Postlinkage Rate (95% CI) | Prelinkage Rate (95% CI) | Postlinkage Rate (95% CI) | |
| Oregon 2010–2011 | 6,348 (6,199–6,502) | 8,380 (8,207–8,557) | 7,882 (7,859–7,905) | 7,853 (7,830–7,876) |
| Washington 2011 | 8,290 (8,115–8,468) | 11,079 (10,877–11,286) | 6,856 (6,832–6,879) | 6,820 (6,796–6,844) |
AI/AN, American Indian/Alaska Native; NHW, non-Hispanic white.
Figure 2.

Ratios of Prelinkage and Postlinkage Age-Adjusted Hospitalization Rates (American Indian/Alaska Native vs. non-Hispanic White) in Oregon (2010–2011) and Washington (2011)
Washington, 2011
Of the 648,383 CHARS records sent for linkage, 8,144 matched with the NTR. Of these matched records, 3,660 (44.9 percent) were misclassified as a race other than AI/AN (Figure1). Among misclassified records, 2,260 (61.8 percent) were coded as white, while 1,197 (32.7 percent) were missing all race information (Figure1). Linkage increased the number of AI/AN records from 10,812 to 14,472, improving ascertainment of AI/AN hospitalizations by 33.9 percent (Table1).
Linkage with the NTR increased the age-adjusted AI/AN hospital discharge rate in Washington by approximately 33.7 percent, from 8,290 to 11,079 hospitalizations per 100,000 (Table2). As in Oregon, the Washington linkage increased the magnitude of the disparity between the AI/AN and NHW population. The rate ratio increased from 1.21 (95 percent CI: 1.19–1.23) prelinkage to 1.62 (95 percent CI: 1.60–1.65) postlinkage (Figure2).
Conclusions
Inaccurate race coding impairs the utility of hospital discharge data for health disparities research, and it leads to inaccuracies that impact decisions on determining priority prevention targets, evaluating programs, and policy development (Schoenman et al. 2005). Record linkage is a cost-effective method of improving race data for AI/AN populations and has been used to improve the identification of AI/AN in various systems (Kressin et al. 2003; Puuka, Stehr-Green, and Becker 2005; Hoopes, Vinson, and Lopez 2012). The current study linked a registry of known AI/AN individuals to two state hospital inpatient discharge datasets, evaluated the race classification of matched records, and compared prelinkage and postlinkage hospital discharge rates by race.
In Oregon, 0.7 percent of hospital discharge records from 2010 to 2011 matched with the NTR, while 1.3 percent of Washington records from 2011 matched the NTR. In both states, approximately half of the matched records were misclassified. The majority of misclassified records were coded as white or were missing race information. That the misclassification in the majority of cases was for AI/AN to be classified as white is likely a reflection of the underlying demographic in these states. According to Census data, only 1.9 percent of the population of both states combined was AI/AN, compared to 87.5 percent white (the majority of whom are non-Hispanic) (National Center for Health Statistics 2014). AI/AN patients may not have been asked to report their race appropriately or at all. Further, almost half of AI/AN in the U.S. report belonging to more than one race (Norris, Vines, and Hoeffel 2010), and multiracial patients may self-identify differently depending on time, place, and circumstance (Sandefur, Campbell, and Eggerling-Boeck 2004). Among the factors that may influence self-reported race in the hospital setting, fear of discrimination has been found to play an important role in health care–seeking behavior among AI/AN women (Gonzalez et al. 2013).
The addition of misclassified AI/AN records identified through linkage with the NTR increased the age-adjusted hospitalization rate for AI/AN by approximately 34 percent for both states, and also increased the observed difference in AI/AN hospitalization rates relative to NHW. Disparities in hospitalization rates indicate potentially unmet health needs and inefficient use of health resources (Korenbrot, Ehlers, and Crouch 2003). This is important considering that the reduction in AI/AN health disparities is an overarching goal of the IHS. Further, the agency and many other AI/AN health organizations are grossly underfunded and must allocate their resources carefully and appropriately.
This linkage study has some important limitations. The NTR underrepresents certain subpopulations of AI/AN in the Northwest, particularly urban AI/AN populations (Northwest Portland Area Indian Health Board 2012). While the NTR version used in this study included patient records from the region’s largest Urban Indian Health Organization, it did not include records from Urban Indian Health Organizations in Portland, Oregon and Spokane, Washington, which also have sizable AI/AN populations. The NTR also underrepresents individuals who self-identify as AI/AN but are not members of federally recognized tribes, AI/AN who are not registered with IHS (e.g., those with private insurance), and patient records from Tribal clinics that do not report their registration information to the IHS (Northwest Portland Area Indian Health Board 2012). Therefore, some records likely remain misclassified in the Oregon and Washington datasets, underestimating the true hospitalization rate for AI/AN in these states. Further, a relatively large percentage of Oregon and Washington records were missing all race data. We do not know the extent to which this missing information introduces bias in our estimates, as we are unable to evaluate the distribution of race/ethnicity or clinical outcomes for these records.
The need for additional data sources for the NTR is exemplified by the number of false positives resulting from the current study’s linkages. In Oregon, 42.6 percent (n = 3,750) of records originally classified as AI/AN did not match to the NTR, and in Washington, 32.8 percent (n = 2,668) did not match to the NTR. These AI/AN patients may be from the groups least represented in the NTR, including urban Indians, AI/AN who do not utilize IHS, tribal or urban clinics, and younger AI/AN. The IDEA-NW project is working to address these limitations by recruiting other urban and tribal clinics to participate in linkage activities. By adding these data sources, we will improve the NTR’s representativeness of the Northwest AI/AN population. Despite its underrepresentation of some AI/AN in Oregon and Washington, the NTR served its purpose in the current study—to evaluate the validity of race/ethnicity data in state hospital discharge datasets, and augment these data to provide more accurate hospitalization estimates for AI/AN in these states.
Our findings demonstrate the extent of racial misclassification for AI/AN in hospital discharge datasets and the effect of this misclassification on estimates of inpatient discharge rates in Oregon and Washington. Several states, including Oregon (Oregon Health Authority 2013), California (Zigmond 2013), and New Mexico (Landen 2013), have implemented strategies to improve the collection of race and ethnicity data within their hospital discharge data systems. These include laws requiring the collection of race and ethnicity in hospital discharge data, as well as developing protocols and training for data collection, compliance plans, patient education materials, and implementing verification and tracking mechanisms such as postdischarge surveys and record linkages (Landen 2013). However, it may take several years for these strategies to translate into actual improvements in data quality in hospital discharge datasets. Further, it is not yet clear if these strategies will address some of the issues that result in the systematic underrepresentation of AI/AN in these datasets.
As it is difficult to accurately assess health disparities within the AI/AN population with currently available data, the strategy to improve racial classification used within this study can be advantageous for Pacific Northwest AI/AN communities, state and local agencies, hospitals, and health care providers to more accurately describe hospitalization patterns for AI/AN. This step is critical in using such data for researchers and other stakeholders to more effectively address disparities in health care quality, utilization, and outcomes for AI/AN populations.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The authors acknowledge the study’s principal investigator, Victoria Warren-Mears, PhD, and the Northwest Portland Area Indian Health Board for supporting this project, as well as our Northwest Tribal Registry data contributors, including the Portland Area Indian Health Service and the Seattle Indian Health Board. Thank you to the Washington and Oregon tribes and AI/AN patients who participated in this work, and to the staff at the Washington Department of Health and the Oregon Health Authority for supporting the linkage and providing guidance. This study was supported by grant R01HS019972 from the Agency for Healthcare Research and Quality and grant AIAMP120012 from the Office of Minority Health.
Disclosures: None.
Disclaimers: None.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
References
- Barnes P, Adams P. Powell-Griner E. Health Characteristics of the American Indian or Alaska Native Adult Population: United States, 2004-2008. Hyattsville, MD: National Center for Health Statistics; 2010. National Health Statistics Report No. 20. [PubMed] [Google Scholar]
- Becker T, Bettles J, Lapidus J, Campo J, Johnson CJ, Shipley D. Robertson LD. Improving Cancer Incidence Estimates for American Indians and Alaska Natives in the Pacific Northwest. American Journal of Public Health. 2002;92(9):1469–71. doi: 10.2105/ajph.92.9.1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilheimer LT. Klein RJ. Data and Measurement Issues in the Analysis of Health Disparities. Health Services Research. 2010;45(5):1489–507. doi: 10.1111/j.1475-6773.2010.01143.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boehrmer U, Kressin NR, Berlowitz DR, Christiansen CL, Kazis LE. Jones JA. Self-Reported vs. Administrative Race/Ethnicity Data and Study Results. American Journal of Public Health. 2002;92(9):1471–3. doi: 10.2105/ajph.92.9.1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foote M, Matloub J, Strickland R, Stephenson L. Vaughan-Batten H. Improving Cancer Incidence Estimates for American Indians in Wisconsin. Wisconsin Medical Journal. 2007;106(4):196–204. [PubMed] [Google Scholar]
- Gomez SL, Kelsey JL, Glaser SL, Lee MM. Sidney S. Inconsistencies between Self-Reported Ethnicity and Ethnicity Recorded in a Health Maintenance Organization. Annals of Epidemiology. 2005;15(1):71–9. doi: 10.1016/j.annepidem.2004.03.002. [DOI] [PubMed] [Google Scholar]
- Gonzalez K, Harding AK, Lambert WE, Fu R. Henderson WG. Perceived Experiences of Discrimination in Health Care: A Barrier for Cancer Screening among American Indian Women with Type 2 Diabetes. Women’s Health Issues. 2013;23(1):e61–7. doi: 10.1016/j.whi.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoopes M, Vinson E. Lopez K. Regional Differences and Tribal Use of American Indian/Alaska Native Cancer Data in the Pacific Northwest. Journal of Cancer Education. 2012;27(1):73–9. doi: 10.1007/s13187-012-0325-4. [DOI] [PubMed] [Google Scholar]
- Hoopes MJ, Taualii M, Weiser TM, Brucker R. Becker TM. Including Self-Reported Race to Improve Cancer Surveillance Data for American Indians and Alaska Natives in Washington State. Journal of Registry Management. 2010;37(2):43–8. [PubMed] [Google Scholar]
- Indian Health Service. 2014. “ About IHS ” [accessed on April 1, 2014]. Available at www.ihs.gov/aboutihs/
- Johnson JC, Soliman AS, Tadgerson D, Copeland GE, Seefeld DA, Pingatore NL, Haverkate R, Banerjee M. Roubidoux MA. Tribal Linkage and Race Data Quality for American Indians in a State Cancer Registry. American Journal of Preventive Medicine. 2009;36(6):549–54. doi: 10.1016/j.amepre.2009.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korenbrot CC, Ehlers S. Crouch JA. Disparities in Hospitalizations of Rural American Indians. Medical Care. 2003;41(5):626–36. doi: 10.1097/01.MLR.0000062549.27661.91. [DOI] [PubMed] [Google Scholar]
- Kressin NR, Chang B, Hendricks A. Kazis LE. Agreement between Administrative Data and Patients’ Self-Reports of Race/Ethnicity. American Journal of Public Health. 2003;93(10):1734–9. doi: 10.2105/ajph.93.10.1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landen M. 2013. “ New Mexico Race Ethnicity Data Project ” [accessed on April 1, 2014]. Available at http://repository.academyhealth.org/ehealthsnapshots/5/
- National Center for Health Statistics. Documentation for Vintage 2011 Bridged-Race Postcensal Population Estimates for Calculating Vital Rates. Atlanta, GA: National Center for Health Statistics; 2012. [Google Scholar]
- National Center for Health Statistics. 2014. “ Bridged-Race Population Estimates, U.S. July 1st Resident Population by State, County, Age, Sex, Bridged-Race, and Hispanic Origin, Compiled from 1990-1999 Bridged-Race Intercensal Population Estimates and 2000-2009 (Vintage 2009) Bridged-Race Postcensal Population Estimates ” [accessed on September 22, 2014]. Available at http://wonder.cdc.gov/bridged-race-v2009.html.
- Norris T, Vines PL. Hoeffel EM. 2010. “ Census Briefs – The American Indian and Alaska Native Population: 2010 ” [accessed on October 1, 2014]. Available at http://www.census.gov/prod/cen2010/briefs/c2010br-10.pdf.
- Northwest Portland Area Indian Health Board. Northwest Tribal Registry, 9th Version (NTR9) Data Assessment. Portland, OR: Northwest Tribal Epidemiology Center; 2012. [Google Scholar]
- Oregon Health Authority. 2013. “ Race, Ethncity and Language Data Collection ” [accessed on April 1, 2014]. Available at http://www.oregon.gov/oha/oei/Pages/race-ethnicity-language.aspx.
- Puuka E, Stehr-Green P. Becker TM. Measuring the Health Status Gap for American Indians/Alaska Natives: Getting Closer to the Truth. American Journal of Public Health. 2005;95(5):838–43. doi: 10.2105/AJPH.2004.053769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts J. Jones J. Health Disparities Challenge Public Health among Native Americans. Northwest Public Health. 2004;21(2):8–9. [Google Scholar]
- Schoenman JA, Sutton JP, Kintala S, Love D. Maw R. The Value of Hospital Discharge Databases. Bethesda, MD: NORC at the University of Chicago; 2005. , and. [Google Scholar]
- Washington State Department of Health (WA DOH) 2014. “ Health of Washington State: Hospitalizations ” [accessed on August 9, 2014]. Available at http://www.doh.wa.gov/Portals/1/Documents/5500/GHS-HOSP2014.pdf.
- Zigmond D. 2013. “ Improving Reporting of Race, Ethnicity, and Language in California ” [accessed on April 1, 2014]. Available at http://repository.academyhealth.org/ehealthsnapshots/12.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.


