Abstract
Objective
To measure the impact of Medicaid reforms, in particular increases in Medicaid dental fees in Connecticut, Maryland, and Texas, on access to dental care among Medicaid-eligible children.
Data
2007 and 2011–2012 National Survey of Children’s Health.
Study Design
Difference-in-differences and triple differences models were used to measure the impact of reforms.
Principal Findings
Relative to Medicaid-ineligible children and all children from a group of control states, preventive dental care utilization increased among Medicaid-eligible children in Connecticut and Texas. Unmet dental need declined among Medicaid-eligible children in Texas.
Conclusions
Increasing Medicaid dental fees closer to private insurance fee levels has a significant impact on dental care utilization and unmet dental need among Medicaid-eligible children.
Keywords: Dental care utilization, Medicaid reform, Medicaid dental fees
It is recommended that children have their first dental visit no later than their first birthday and thereafter have a visit every 6 months (American Academy of Pediatric Dentistry 2012). In Medicaid, states must guarantee eligible children access to comprehensive dental benefits (Centers for Medicaid and Medicare Services [CMS] Undated). However, a variety of reasons, including multiple claim forms and low reimbursement rates, may limit the number of providers that accept Medicaid (Government Accountability Office 2000).
Connecticut, Maryland, and Texas increased Medicaid dental fees paid to providers between 2007 and 2011. After a class-action lawsuit settlement, Connecticut increased Medicaid dental fees to the 70th percentile of private insurance fees in mid-2008. The settlement led to improved Medicaid program administration and a committed case management program to help ensure beneficiaries attended scheduled appointments. Connecticut started implementing these changes in 2007 (Beazoglou et al. 2013). Maryland increased Medicaid dental fees to the 50th percentile of private insurance fees in place in the South Atlantic region and carved Medicaid dental services out of managed care in 2009 (Thuku et al. 2012). Also in 2009, Maryland increased the dental provider network, improved customer services for providers and patients, streamlined credentialing and created a missed appointment tracker (National Academy for State Health Policy 2014). On September 1, 2007, Texas increased dental reimbursement by 52.5 percent (Texas Health and Human Services Commission 2009). This was in response to a U.S. Supreme Court decision that Texas must operate their Medicaid program in compliance with specific guidelines, which included requirements to increase utilization through increased access to Medicaid providers for dental services (United States Supreme Court 2004).
We study the impact of these Medicaid policy reforms in Connecticut, Maryland, and Texas on dental care utilization and unmet dental need among Medicaid-eligible children. We compare the experience of children in Connecticut, Maryland, and Texas to a control group of children in other states that had little or no change in Medicaid policy from 2007 through 2012.
Study Data and Methods
Data Source
We use data from the 2007 and 2011–2012 waves of the National Survey of Children’s Health (NSCH). Each wave has about 1,800 observations per state representing children under age 18 (Blumberg et al. 2012; Centers for Disease Control and Prevention [CDC] 2013). Interviews for the 2007 NSCH were conducted between April 5, 2007 and July 27, 2008, although 79 percent of the interviews took place by the end of 2007 (Blumberg et al. 2012). Interviews for the 2011–2012 NSCH were conducted from February 28, 2011 through June 25, 2012 (CDC 2013).
Study Sample and Variable Definitions
Household income in the NSCH is defined in eight categories (≤100 percent FPL, 100 percent <FPL≤ 133 percent, 133 percent <FPL≤ 150 percent, 150 percent <FPL≤ 185 percent, 185 percent <FPL≤ 200 percent, 200 percent <FPL≤ 300 percent, 300 percent <FPL≤ 400 percent, and >400 percent FPL).1 Based on reported household income and Medicaid income thresholds from the annual Kaiser Family Foundation 50-State Survey of Medicaid and CHIP Eligibility and Enrollment Policies (Kaiser Family Foundation 2014), we identify children eligible for Medicaid. The analysis includes children aged 1–17 years. Data from the 2007 NSCH constitute the prereform period and data from the 2011–2012 NSCH represent the postreform period. Although some of the reforms in Connecticut and Texas could have coincided with the 2007 NSCH interview period, we would expect some lag time between the time of the policy changes and any potential effect on dental care utilization.
We generate two binary outcome variables that measure whether a child had a preventive dental visit and an unmet dental need in the past 12 months.2 Medicaid fee-for-service dental fees are compared to private dental insurance fees across 14 commonly used dental procedures.3 We extract historical state-level Medicaid dental fees for 2005 through 2012 from prior research (Buchmueller, Orzol, and Shore-Sheppard 2013). We collect private dental insurance fees for 2005 through 2012 from the FAIR Health Dental Benchmark Module (FAIR Health, Inc. Undated). We compute Medicaid and private dental insurance indices using weights based on total billings aggregated from the 2010 through 2012 FAIR Health Dental Benchmark Module. We divide the Medicaid index by the private dental insurance index to measure Medicaid reimbursement relative to private dental insurance.
We compare children in Connecticut, Maryland, and Texas to a group of children in control states that experienced no significant change in Medicaid dental fees. Our selection of control states is based on whether the Medicaid-to-private-dental-insurance fee ratio was constant over the study period. Using this criterion, we include children from California, Florida, Hawaii, Illinois, Massachusetts, Maine, Missouri, Mississippi, North Dakota, Oregon, Pennsylvania, Utah, Washington State, and Wisconsin in the control group. The Medicaid-to-private-dental-insurance fee ratio was 45 percent in 2005 and 43 percent in 2012 in the control states. However, the fee ratio increased substantially in the treatment states between 2007 and 2012 (Appendix Figure S1). During the study period, private dental insurance reimbursement trended in a similar fashion in the treatment and control states (Appendix Figure S2). The increase in Medicaid reimbursement between 2007 and 2012 in the treatment states (Appendix Figure S3) accounted for the change in the Medicaid-to-private-dental insurance fee ratio. To check the robustness of our results, we conduct sensitivity analyses by changing the composition of the control states (see Appendix).
Methodology
We expect that higher Medicaid dental fees would, all else equal, lead to increased preventive dental care utilization and decreased unmet dental need among Medicaid-eligible children. In the control states, where Medicaid fees did not change, we would not expect to see such changes. We would also not expect to see any effect of Medicaid dental fee increases on preventive dental care use or unmet dental need among children who are not eligible for Medicaid. Our approach, therefore, is to compare changes in the level of preventive dental care use and unmet dental need between Medicaid-eligible children in the treatment and control states and between Medicaid-eligible and Medicaid-ineligible children within the treatment and control states.
Limiting the analysis to only the treatment states, a simple pre–post comparison could measure the impact of the reforms. However, there is a possibility that other changes in the treatment states occurring between 2007 and 2011–2012 could have confounded the impact of the Medicaid reforms, invalidating a simple pre–post approach. This is the rationale behind using Medicaid-eligible children from the control states as a comparison group, where no known policy changes occurred. This difference-in-differences approach isolates the impact of the reforms in the treatment states. However, we know that between 2007 and 2011–2012, significant exogenous factors, such as economic fluctuations, could have affected the dental care delivery system more broadly, both within and outside of Medicaid, in the treatment states. Hence, we add children not eligible for Medicaid as an additional control group. With this additional control group, a triple differences model is an additional method to measure the impact of the reforms on Medicaid-eligible children in the treatment states. We compare the policy impact estimates of the difference-in-differences model and the triple-differences model. Our policy impact estimates control for age, gender, ethnicity/race, parent’s education, and oral health status.
The econometric specification we use is as follows:
Model 1: Difference-in-Differences
Model 2: Triple Differences
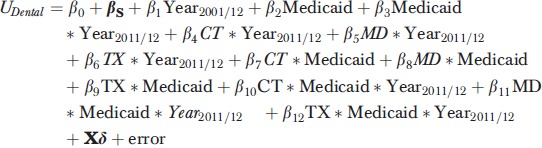 |
We estimate Model 1 among Medicaid-eligible children and Model 2 among all children. UDental measures preventive dental care utilization or unmet dental need. Medicaid is an income-based Medicaid eligibility indicator variable, and Year2011/12 is an indicator variable for the child being included in the 2011–2012 NSCH survey wave. CT,MD, and TX represent indicator variables for Connecticut, Maryland, and Texas, respectively. The vector X includes the previously described control variables and the coefficient vector βs represents state fixed effects. In Model 1, β2, β3, and β4 are estimates of the policy impact of the reforms in Connecticut, Maryland, and Texas, respectively, among Medicaid-eligible children. Coefficients β10, β11, and β12 in Model 2 measure the impact of the policy changes in Connecticut, Maryland, and Texas, respectively, on Medicaid-eligible children relative to Medicaid-ineligible children. We cluster standard errors at the state level since the policy reforms are state-specific. Because we use the imputed income files developed by the NSCH, our standard errors further account for multiply imputed data using standard combining rules (Rubin 1987). We use linear probability models to estimate Models 1 and 2.
Limitations
Public insurance status in the NSCH is determined as of the date of the interview. However, utilization and unmet need are measured for the prior 12 months for each child. Respondents may not fully understand the type of insurance their child has because states use a variety of names for their public insurance programs; instead, parents may believe that their children are enrolled in a private insurance program when in fact they are enrolled in Medicaid. Low-income families eligible for Medicaid may also believe that preventive pediatric health care is beneficial, which could encourage enrollment in Medicaid. That is, participation in Medicaid among those that are eligible might induce endogeneity in the model. Because of these factors, we decided to use household income to determine Medicaid eligibility.
Study Results
As shown in Panel 1 of Table1, among Medicaid-eligible children, from 2007 to 2011–2012, preventive dental care utilization increased from 74.9 percent to 81.1 percent in Connecticut, from 69.9 percent to 71.9 percent in Maryland, and from 65.9 percent to 80.7 percent in Texas. In the control states, preventive dental care utilization was 66.8 percent in 2007 and 65.2 percent in 2011–2012 among Medicaid-eligible children. Relative to the control states, preventive dental care utilization among Medicaid-eligible children increased by 7.8 percentage points in Connecticut and by 16.4 percentage points in Texas, statistically significant changes. Relative to the control states, there was only a modest and statistically insignificant change (3.6 percentage points) in preventive dental care utilization among Medicaid-eligible children in Maryland. When Medicaid-ineligible children are added as an additional control group, preventive dental care utilization among Medicaid-eligible children increased by 17.0 percentage points in Texas (p < .01), by 5.3 percentage points in Maryland (p < .10), and by 6.2 percentage points in Connecticut (p < .10).
Table 1.
Preventive Dental Care Utilization and Unmet Dental Need among Medicaid-Eligible and Ineligible Children
| State | Medicaid-Eligible | Medicaid-Ineligible | Triple Difference (A minus B) | ||||
|---|---|---|---|---|---|---|---|
| Pre (2007) | Post (2011–2012) | Difference (Post minus Pre) | Pre (2007) | Post (2011–2012) | Difference (Post minus Pre) | ||
| Panel 1: Preventive Dental Care Utilization in the Past 12 Months | |||||||
| CT | 74.9% | 81.1% | 6.2 Pct Pts | 87.5% | 88.5% | 1.0 Pct Pts | 6.2 Pct Pts* |
| Control States | 66.8% | 65.2% | −1.6 Pct Pts | 81.3% | 80.7% | −0.6 Pct Pts | |
| Difference (CT minus Control States) | 8.1 Pct Pts** | 15.9 Pct Pts*** | (A) Difference in Difference: 7.8 Pct Pts*** | 6.2 Pct Pts*** | 7.8 Pct Pts*** | (B) Difference in Difference: 1.6 Pct Pts | |
| MD | 69.9% | 71.9% | 2.0 Pct Pts | 85.8% | 83.5% | −2.3 Pct Pts | 5.3 Pct Pts* |
| Control States | 66.8% | 65.2% | −1.6 Pct Pts | 81.3% | 80.7% | −0.6 Pct Pts | |
| Difference (MD minus Control States) | 3.1 Pct Pts | 6.7 Pct Pts** | (A) Difference in Difference: 3.6 Pct Pts | 4.5 Pct Pts** | 2.8 Pct Pts* | (B) Difference in Difference: −1.7 Pct Pts | |
| TX | 65.9% | 80.7% | 14.8 Pct Pts*** | 78.1% | 76.9% | −1.2 Pct Pts | 17.0 Pct Pts*** |
| Control States | 66.8% | 65.2% | −1.6 Pct Pts | 81.3% | 80.7% | −0.6 Pct Pts | |
| Difference (TX minus Control States) | −0.9 Pct Pts | 15.5 Pct Pts*** | (A) Difference in Difference: 16.4 Pct Pts*** | −3.2 Pct Pts* | −3.8 Pct Pts** | (B) Difference in Difference: −0.6 Pct Pts | |
| Panel 2: Unmet Dental Need in the Past 12 Months | |||||||
| CT | 3.7% | 4.0% | 0.3 Pct Pts | 1.7% | 0.9% | −0.8 Pct Pts | 1.2 Pct Pts |
| Control States | 4.7% | 4.4% | −0.3 Pct Pts | 2.4% | 2.2% | −0.2 Pct Pts | |
| Difference (CT minus Control States) | −1.0 Pct Pts | −0.4 Pct Pts | (A) Difference in Difference: 0.6 Pct Pts | −0.7 Pct Pts*** | −1.3 Pct Pts*** | (B) Difference in Difference: −0.6 Pct Pts* | |
| MD | 3.7% | 3.8% | 0.1 Pct Pts | 1.4% | 1.0% | −0.4 Pct Pts | 0.6 Pct Pts |
| Control States | 4.7% | 4.4% | −0.3 Pct Pts | 2.4% | 2.2% | −0.2 Pct Pts | |
| Difference (MD minus Control States) | −1.0 Pct Pts | −0.6 Pct Pts | (A) Difference in Difference: 0.4 Pct Pts | −1.0 Pct Pts*** | −1.2 Pct Pts*** | (B) Difference in Difference: −0.2 Pct Pts | |
| TX | 4.5% | 2.4% | −2.1 Pct Pts | 2.7% | 4.3% | 1.6 Pct Pts | −3.6 Pct Pts*** |
| Control States | 4.7% | 4.4% | −0.3 Pct Pts | 2.4% | 2.2% | −0.2 Pct Pts | |
| Difference (TX minus Control States) | −0.2 Pct Pts | −2.0 Pct Pts*** | (A) Difference in Difference: −1.8 Pct Pts* | 0.3 Pct Pts* | 2.1 Pct Pts*** | (B) Difference in Difference: 1.8 Pct Pts** | |
Notes Estimates are weighted. Control states include CA, FL, HI, IL, ME, MA, MO, MS, ND, OR, PA, UT, WA, and WI.
Significant at 1% level (p ≤ .01)
significant at 5% level (p ≤ .05)
significant at 10% level (p ≤ .10).
Source: 2007 and 2011–2012 National Survey of Children’s Health.
As shown in Panel 2 of Table1, compared to Medicaid-eligible children in the control states, there was little change in unmet dental need among Medicaid-eligible children in Connecticut and Maryland. In Texas, unmet dental need declined from 4.5 percent in 2007 to 2.4 percent in 2011–2012. Relative to Medicaid-eligible children in the control states, unmet dental need declined by 1.8 percentage points in Texas (p < .10). When Medicaid-ineligible children are added as an additional control group, unmet dental need declined by 3.6 percentage points (p < .01) among Medicaid-eligible children in Texas.
These policy impact estimates differ little when we control for various individual factors in multivariate difference-in-differences (Table2) and triple differences models (Table3). This suggests that there are no observable factors that confound the relationship between the policy changes and dental care outcomes. The fact that our bivariate (Table1) and multivariate (Tables2 and 3) difference-in-differences and triple differences results are so similar indicates that there were similar changes in preventive dental care utilization and unmet dental need for Medicaid-ineligible children in the treatment and control states. Model 1 and 2 results are robust to changes in the composition of the control states (Appendix Table S2–S5).
Table 2.
Impact of Medicaid Reforms on Preventive Dental Care Utilization and Unmet Dental Need in the Past Twelve Months on Medicaid-Eligible Children in Connecticut, Maryland, and Texas Relative to Medicaid-Eligible Children in the Control States
| State | Preventive Dental Visit in Past 12 Months | Unmet Dental Need in Past 12 Months |
|---|---|---|
| CT | 0.077*** | 0.006 |
| MD | 0.020 | 0.003 |
| TX | 0.158*** | −0.020* |
| Sample size | 12,614 | 12,614 |
Notes Difference-in-differences models estimated over Medicaid-eligible sample. Estimates are weighted. Standard errors are clustered at the state level. Regressions control for age, gender, highest level of parent’s education, ethnicity/race, and oral health status. Regressions exclude children below age one. All regressions include state fixed-effects. Control states include CA, FL, HI, IL, ME, MA, MO, MS, ND, OR, PA, UT, WA, and WI.
Significant at 1% level (p ≤ .01)
significant at 5% level (p ≤ .05)
significant at 10% level (p ≤ .10).
Source: 2007 and 2011–2012 National Survey of Children’s Health.
Table 3.
Impact of Medicaid Reforms on Preventive Dental Care Utilization and Unmet Dental Need in the Past Twelve Months on Medicaid-Eligible Children in Connecticut, Maryland, and Texas Relative to Medicaid-Ineligible Children in Connecticut, Maryland, and Texas and all Children in the Control States
| State | Preventive Dental Visit in Past 12 Months | Unmet Dental Need in Past 12 Months |
|---|---|---|
| CT | 0.063** | 0.013 |
| MD | 0.033 | 0.004 |
| TX | 0.155*** | −0.035** |
| Sample size | 58,162 | 58,162 |
Notes Triple differences model estimated over entire sample (Medicaid-eligible and ineligible). Estimates are weighted. Standard errors are clustered at the state level. Regressions control for age, gender, highest level of parent’s education, ethnicity/race, and oral health status. Regressions exclude children below age one. All regressions include state fixed-effects. Control states include CA, FL, HI, IL, ME, MA, MO, MS, ND, OR, PA, UT, WA, and WI.
Significant at 1% level (p ≤ .01)
significant at 5% level (p ≤ .05)
significant at 10% level (p ≤ .10).
Source: 2007 and 2011–2012 National Survey of Children’s Health.
Discussion
Our findings show that increases in Medicaid dental fees led to increased preventive dental care utilization in Connecticut and Texas, and lower unmet dental need in Texas among Medicaid-eligible children. The impact of the reforms on Medicaid-eligible children in Maryland proved to be more modest. The increase in the Medicaid-to-private-dental insurance fee ratio in Maryland was more modest than in Connecticut and Texas (Appendix Table S1). The 2012 fee ratio level was also lower in Maryland than in Connecticut and Texas. This may be a reason for the modest changes in preventive dental care utilization and unmet dental need in Maryland among Medicaid-eligible children compared to Connecticut and Texas.
Our results also varied across dental care outcomes, with Medicaid fee increases having a stronger effect on preventive dental care utilization than unmet dental need. It could be that higher dental fees may induce providers to expand dental care services that are more discretionary in nature and not necessarily related to a pressing oral health need. Conversely, lower dental fees may induce providers to limit services but not to the point where urgent needs are left untreated. In Texas, the Supreme Court had to intervene to spur the state to reform its Medicaid program. Due to a possible high level of pent-up demand for dental care in Texas prior to 2007, there may have been a high level of unmet dental need, which the reforms subsequently reduced.
Looking forward, the Affordable Care Act (ACA) may expand dental benefits to about 8.7 million children who are uninsured for dental care, 3.2 million of whom are expected to gain dental benefits through Medicaid (Nasseh, Vujicic, and O’Dell 2013). At the same time, more dentists are reporting that they “are not busy enough and can treat more patients” and wait times for dental appointments have declined (Vujicic, Munson, and Nasseh 2013). These trends suggest that there is unused capacity within the dental care delivery system and that the current supply of dentists may be sufficient to handle the increased demand for dental services from children in Medicaid programs in the coming years. An increase in Medicaid dental fees, in certain circumstances, may entice the existing supply of dentists to treat more Medicaid patients (Buchmueller, Orzol, and Shore-Sheppard 2013).
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The views expressed by the authors do not necessarily reflect those of the American Dental Association. Mr. Tom Wall provided research assistance in helping to gather the data. Ms. Cassandra Yarbrough helped prepare background information on the three states analyzed in the research brief: Connecticut, Maryland, and Texas. Dr. Thomas Buchmueller of the University of Michigan kindly provided historical Medicaid dental reimbursement fee data. Dr. Anthony LoSasso of the University of Illinois-Chicago provided helpful comments on earlier drafts of this paper. Research for this article is based partly upon health care charge data compiled and maintained by FAIR Health, Inc. The authors are responsible for the research and conclusions reflected in this article. FAIR Health, Inc. is not responsible for the conduct of the research or for any of the opinions expressed in this article.
Disclosures: None.
Disclaimers: None.
Footnotes
For each respondent, the prior calendar year’s income is reported. For example, year 2007 FPL guidelines were used with 2006 income for interviews conducted from April 5, 2007 through December 31, 2007. Year 2007 guidelines were also used with 2007 income reported in interviews conducted from January 1, 2008 through July 27, 2008.
The preventive dental question is asked as follows: “During the past 12 months since (his/her) birth, how many times did [S.C.] see a dentist for preventive dental care, such as check-ups and dental cleanings? The unmet dental need question is asked as follows: “During the past 12 months/Since (his/her) birth, was there any time when [S.C.] needed health care but it was delayed or not received? What type of care was delayed or not received? Was it medical care, dental care, mental health services, or something else?”
Dental procedures include the following CDT codes: D0120, D0150, D0210, D0272, D0330, D1120, D1203, D1351, D2150, D2331, D2930, D3220, D3310, and D7140.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Table S1. Summary Statistics of Dental Care Utilization, Unmet Dental Need, and Explanatory Variables (Pre and Post Reform).
Table S2. Impact of Medicaid Reforms on Preventive Dental Care Utilization and Unmet Dental Need in the Past Twelve Months on Medicaid-Eligible Children in Connecticut, Maryland, and Texas Relative to Medicaid-Eligible Children in the Control States (Control States: CA, FL, HI, IL, ME, MA, ND, OR, UT, WA, and WI).
Table S3. Impact of Medicaid Reforms on Preventive Dental Care Utilization and Unmet Dental Need in the Past Twelve Months on Medicaid-Eligible Children in Connecticut, Maryland, and Texas Relative to Medicaid-Ineligible Children in Connecticut, Maryland, and Texas and All Children in the Control States (Control States: CA, FL, HI, IL, ME, MA, ND, OR, UT, WA, and WI).
Table S4. Impact of Medicaid Reforms on Preventive Dental Care Utilization and Unmet Dental Need in the Past Twelve Months on Medicaid-Eligible Children in Connecticut, Maryland, and Texas Relative to Medicaid-Eligible Children in the Control States (Control States: CA, FL, ME, MA, MO, MS, ND, PA, UT, and WA).
Table S5. Impact of Medicaid Reforms on Preventive Dental Care Utilization and Unmet Dental Need in the Past Twelve Months on Medicaid-Eligible Children in Connecticut, Maryland, and Texas Relative to Medicaid-Ineligible Children in Connecticut, Maryland, and Texas and All Children in the Control States (Control States: CA, FL, ME, MA, MO, MS, ND, PA, UT, and WA).
Table S6. Triple Differences Model: Impact of Reforms on Preventive Dental Care Utilization.
Table S7. Triple Differences Model: Impact of Reforms on Unmet Dental Need.
Figures S1–S3. Private Dental Insurance and Medicaid Reimbursement.
References
- American Academy of Pediatric Dentistry. 2012. “ Parent Resources. Frequently Asked Questions ” [accessed on September 17, 2013]. Available at http://www.aapd.org/resources/frequently_asked_questions/
- Beazoglou T, Douglass J, Bailit H. Myne-Joslin V. 2013. “ Connecticut Health Foundation. Impact of Increased Dental Reimbursement Rates on Husky A-Insured Children: 2006-2011 ” [accessed on July 21, 2014]. Available at http://www.cthealth.org/wp-content/uploads/2013/02/impact-of-increased-dental-reimbursement-rates.pdf. [DOI] [PubMed]
- Blumberg SJ, Foster EB, Frasier AM, Satorius J, Skalland BJ, Nysse-Carris KL, Morrison HM, Chowdhury SR. O’Connor KS. Design and Operation of the National Survey of Children’s Health, 2007. Vital and Health Statistics. 2012;1(55):1–149. National Center for Health Statistics. [PubMed] [Google Scholar]
- Buchmueller TC, Orzol S. Shore-Sheppard LD. 2013. “ The Effect of Medicaid Payment Rates on Access to Dental Care among Children.” NBER Working Paper No. 19218 [accessed on September 19, 2013]. Available at http://www.nber.org/papers/w19218.pdf?new_window=1.
- Centers for Disease Control and Prevention. 2013. , National Center for Health Statistics, State and Local Area Integrated Telephone Survey. “ 2011-2012 National Survey of Children’s Health Frequently Asked Questions ” [accessed on March 25, 2014] Available at ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/slaits/nsch_2011_2012/01_Frequently_asked_questions/NSCH_2011_2012_FAQs.pdf.
- Centers for Medicaid and Medicare Services [CMS] . Undated. “ Early and Periodic Screening, Diagnostic, and Treatment ” [accessed on March 25, 2014]. Available at http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Benefits/Early-and-Periodic-Screening-Diagnostic-and-Treatment.html.
- FAIR Health, Inc. Standard Products. Dental Module. Undated [accessed on October 6, 2014] Available at http://www.fairhealth.org/DataSolution.
- Government Accountability Office. 2000. “ Oral Health. Factors Contributing the Low Use of Dental Services by Low-Income Populations.” GAO/HEHS-00-149 [accessed on October 6, 2014]. Available at http://www.gao.gov/assets/240/230602.pdf.
- Kaiser Family Foundation. 2014. “ Medicaid ” [accessed on March 26, 2014]. Available at http://kff.org/medicaid/
- Nasseh K, Vujicic M. O’Dell A. 2013. Health Policy Resources Center. American Dental Association. “ Affordable Care Act Expands Dental Benefits for Children but Does Not Address Critical Access to Dental Care Issues ” [accessed on October 30, 2013]. Available at http://www.ada.org/sections/professionalResources/pdfs/HPRCBrief_0413_3.pdf.
- National Academy for State Health Policy. 2014. “ Promoting Oral Health through the Medicaid Benefit for Children and Adolescents ” [accessed on July 8, 2014]. Available at http://www.nashp.org/sites/default/files/Promoting.Oral_.Health.Through.the_.Medicaid.Benefit.for_.Children.pdf.
- Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley; 1987. [Google Scholar]
- Texas Health and Human Services Commission. 2009. “ Health and Human Services Consolidated Budget ” [accessed on July 15, 2014]. Available at http://www.hhsc.state.tx.us/ConsolidatedBudget_2010-2011.pdf.
- Thuku NM, Carulli K, Costello S. Goodman HS. Breaking the Cycle in Maryland: Oral Health Policy Change in the Face of Tragedy. Journal of Public Health Dentistry. 2012;72(Suppl 1):S7–13. doi: 10.1111/j.1752-7325.2012.00328.x. [DOI] [PubMed] [Google Scholar]
- United States Supreme Court. 2004. “ Frew, on Behalf of her Daughter, Frew, et al. v. Hawkins, Commissioner, Texas Health and Human Services Commission, et al ” [accessed on July 15, 2014]. Available at http://caselaw.lp.findlaw.com/scripts/getcase.pl?court=US&vol=000&invol=02-628.
- Vujicic M, Munson B. Nasseh K. 2013. Health Policy Resources Center. American Dental Association. “ Despite Economic Recovery, Dentist Earnings Remain Flat ” [accessed on October 30, 2013]. Available at http://www.ada.org/sections/professionalResources/pdfs/HPRCBrief_1013_4.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Table S1. Summary Statistics of Dental Care Utilization, Unmet Dental Need, and Explanatory Variables (Pre and Post Reform).
Table S2. Impact of Medicaid Reforms on Preventive Dental Care Utilization and Unmet Dental Need in the Past Twelve Months on Medicaid-Eligible Children in Connecticut, Maryland, and Texas Relative to Medicaid-Eligible Children in the Control States (Control States: CA, FL, HI, IL, ME, MA, ND, OR, UT, WA, and WI).
Table S3. Impact of Medicaid Reforms on Preventive Dental Care Utilization and Unmet Dental Need in the Past Twelve Months on Medicaid-Eligible Children in Connecticut, Maryland, and Texas Relative to Medicaid-Ineligible Children in Connecticut, Maryland, and Texas and All Children in the Control States (Control States: CA, FL, HI, IL, ME, MA, ND, OR, UT, WA, and WI).
Table S4. Impact of Medicaid Reforms on Preventive Dental Care Utilization and Unmet Dental Need in the Past Twelve Months on Medicaid-Eligible Children in Connecticut, Maryland, and Texas Relative to Medicaid-Eligible Children in the Control States (Control States: CA, FL, ME, MA, MO, MS, ND, PA, UT, and WA).
Table S5. Impact of Medicaid Reforms on Preventive Dental Care Utilization and Unmet Dental Need in the Past Twelve Months on Medicaid-Eligible Children in Connecticut, Maryland, and Texas Relative to Medicaid-Ineligible Children in Connecticut, Maryland, and Texas and All Children in the Control States (Control States: CA, FL, ME, MA, MO, MS, ND, PA, UT, and WA).
Table S6. Triple Differences Model: Impact of Reforms on Preventive Dental Care Utilization.
Table S7. Triple Differences Model: Impact of Reforms on Unmet Dental Need.
Figures S1–S3. Private Dental Insurance and Medicaid Reimbursement.


