Abstract
Objective
Evaluate the relationship between school climate and ADHD medication treatment among adolescents in Medicaid in Georgia (GA).
Methods
School climate and Medicaid claims data were aggregated for 159 GA counties. County-level school climate percentile and medicated ADHD prevalence were calculated. T-tests and regression evaluated the relationship between school climate, medicated ADHD, and demographics, weighted by county population. Poorer 2008 school climate (<25th percentile) was regressed on 2011 medicated ADHD prevalence, controlling for potential confounders.
Results
The prevalence of medicated ADHD was 7.8% among Medicaid-enrolled GA adolescents. The average county-level prevalence of medicated ADHD was 10.0% (SD=2.9%). Poorer school climate was associated with lower rates of medicated ADHD (p<0.0001) and with demographics accounted for 50% of the county variation in medicated ADHD.
Conclusions
School climate is associated with medicated ADHD among adolescents in Medicaid. Additional research may reveal whether high medicated ADHD may reflect a lack of access to non-pharmacological therapies.
Keywords: school climate, attention-deficit/hyperactivity disorder, ADHD, behavioral problems, health care utilization, medication treatment
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a chronic, neurodevelopmental disorder with childhood onset that impacts the regulation of attention, activity-level, and impulses (American Psychiatric Association, 2013). Approximately 11% of U.S. children (aged 4–17 years) have been diagnosed with ADHD by a health care provider as reported by parents (Susanna N. Visser et al., 2014), making ADHD the most prevalent mental disorder of childhood (Perou et al., 2013). The prevalence of diagnosed ADHD has increased by 3–6% per year since 1997 (Akinbami, Liu, Pastor, & Reuben, 2011; Susanna N. Visser et al., 2014). The estimated annual societal costs of childhood ADHD are massive and span multiple sectors, totaling $38–$72 billion (Doshi et al., 2012). The negative consequences of childhood ADHD include higher rates of unintentional injury, emergency room visits, peer problems, and academic failure (DiScala, Lescohier, Barthel, & Li, 1998; Hoare & Beattie, 2003; Loe & Feldman, 2007; Merrill, Lyon, Baker, & Gren, 2009). ADHD persists into adulthood for at least one-third of children and is associated with employment challenges, incarceration, co-occurring mental disorders, divorce, suicide, and significant family disturbance (Barbaresi et al., 2013; de Graaf et al., 2008; Harpin, 2005).
Clinical guidelines exist for the diagnosis and treatment of ADHD (American Academy of Child and Adolescent Psychiatry, 2007; American Academy of Pediatrics, 2011). Current treatment guidelines recommend that adolescents with ADHD be treated with an ADHD medication alongside behavioral therapy, if possible (American Academy of Pediatrics, 2011). ADHD treatment is very effective for managing ADHD symptoms and impairment, with effect sizes (proportion of a standard deviation) ranging from .6 for behavioral strategies and .7 for non-stimulant medications to 1.0 for stimulant medications (American Academy of Pediatrics, 2011).
Parents report that 11.4% of youth in middle-school and 10.2% of youth in high-school had current ADHD in 2011–12; 8.0% of middle-schoolers and 6.4% of high schoolers were taking medication for ADHD, a significant increase of approximately 25% since 2007–08 (Susanna N. Visser et al., 2014). These increases reflect the substantial (80%) increases in ADHD medication prescriptions for methylphenidate and amphetamine products among preteens and teens from 1998–2005 (Setlik, Bond, & Ho, 2009). Increasing academic demands and perceived school pressures are cited as factors in the increasing trends in adolescent ADHD (Graf et al., 2013), as is increased awareness of ADHD and its treatment among primary care practitioners (Wolraich, Bard, Stein, Rushton, & O’Connor, 2010). However, factors influencing these trends are not fully understood.
Previous research suggests that ADHD and medicated ADHD rates are associated with demographic factors, including being male, non-Hispanic, speaking English as a primary language, living in poverty and having insurance (Susanna N. Visser et al., 2014). There is also substantial state-based variability in rates of medicated ADHD, from 2% in Nevada to 10% in Kentucky and Louisiana (Susanna N. Visser et al., 2014). State variation in prevalence has been partially explained by state demographics (race and public insurance coverage) and the characteristics of the state’s physicians; higher state proportions of younger physicians (<45 years) are associated with higher state-based rates of diagnosed and medicated ADHD (Fulton et al., 2009). Ecological analyses suggest that school policies, practices, and accountability laws may contribute to state-based variation in ADHD rates. Specifically, consequential accountability laws and high school exit exams predict higher ADHD rates (Hinshaw & Scheffler, 2014). Thus, in addition to demographic characteristics of children and their health care practitioners, school policies and practices may contribute to ADHD and medicated ADHD rates. Among these, school policies and practices have received the least attention, despite the tremendous influence that schools have on child development, including the development of their attitudes, motivation, behaviors, cognitive abilities, and social competence (Sylva, 1994).
School climate reflects quality and character of school life and incorporates four key areas: safety, interpersonal relationships, teaching and learning, and institutional environment (Cohen & Geier, 2010; National School Climate Council, 2007). Poorer student-perceived school climate is associated with individual and community characteristics (Kuperminc, Leadbeater, Emmons, & Blatt, 1997; Way, Reddy, & Rhodes, 2007) as well as negative indicators of academic, socio-emotional, and behavioral health (Thapa, Cohen, Guffey, & Higgins-D’Alessandro, 2013), including higher rates of truancy (Sommer, 1985), lower global and academic self-esteem (Hoge & et al., 1990; Way et al., 2007), higher rates of self-reported and teacher-reported internalizing and externalizing problems among students, and more discipline referrals (Kuperminc et al., 1997; Way et al., 2007). There is a lack of research evaluating the association between student-perceived school climate and the presence of mental and behavioral disorders such as ADHD and associated health care utilization.
Identifying modifiable factors that may influence health-care utilization patterns of children and adolescents with ADHD may have important implications for school-based policy, practice, and health promotion of those with ADHD. Research at the school district and county levels may be most useful, as school policies and practices are often implemented at these levels. Focusing on factors associated with health care utilization among adolescents with ADHD has potential to identify opportunities to positively impact those most likely to have ADHD persisting into adulthood (i.e., symptomatic adolescents).
Earlier work has shown that estimates of medicated ADHD from a parent survey were similar to rates of medicated ADHD among children from data drawn from insurance data (S. N. Visser, Danielson, Bitsko, Perou, & Blumberg, 2013). These findings suggest the use of claims data on ADHD medication treatment as a reasonable proxy for identifying prevalence of medicated ADHD in state-based analyses of ADHD.
This study intends to evaluate the association between student-perceived school climate and medicated ADHD prevalence among low-income adolescents, using county-level school climate and Medicaid claims data from the state of Georgia (GA), which has an average state-based prevalence of current ADHD of 9.3%, ranked 25th in the nation (Centers for Disease Control and Prevention, 2014). Given previous research indicating a relationship between poorer school climate and poor socio-emotional and behavioral health, we expect that poorer school climate will be associated with higher ADHD prevalence and reflect higher rates of medicated ADHD.
Methods
This cross-system analysis utilizes school climate data from the GA Department of Education and Medicaid claims data from the GA Department of Community Health to explore the relationship between county-aggregated student ratings of school climate and ADHD medication treatment among adolescents enrolled in the GA Medicaid program. Data are aggregated to the county level at the respective Department to ensure patient and student privacy and reduce disclosure risks. The study methods were reviewed by the Human Subjects Protection offices of the University of Illinois at Chicago and the Centers for Disease Control and Prevention.
Data
School Climate
Student-perceived school climate is the primary independent variable. Since 2008, the GA Department of Education has conducted school climate assessments of middle and high school students through an anonymous annual web-based survey (Georgia Student Health Survey II: GSHS II), including questions on alcohol and drug use, nutrition and dietary behaviors, thoughts of suicide and self-harm, bullying, unsupervised time, and well-being. The survey also includes nine school climate questions that track to four school climate focus areas; safety, teaching and learning, inter-personal relationships, institutional environment, (Appendix) which sum to an overall school climate score (Cohen & Geier, 2010).
School climate scores were averaged across students for state and county to create state and county-averaged school climate indicators. The county-level school climate scores were standardized (z-score transformation), converted to percentiles based on the state-level score, and dichotomized for analysis (bottom versus top three quartiles). The 2008 and 2011 GSHS-II data were used in this analysis, with 2008 data used to create the primary independent variable to ensure that the school climate preceded in time the 2011 ADHD outcomes, regardless of age, thereby strengthening our ability to make causal assertions. To assess the potential impact that concurrent school climate had on 2011 medicated ADHD prevalence, a difference score was calculated between the 2011 and 2008 county-level school climate percentiles; this score was converted to a dichotomous indicator to indicate stability or improvement versus a decline in school climate from 2008–2011.
Medicated ADHD Prevalence
GA Medicaid data from 2011 were used to create a medicated ADHD indicator, the primary dependent variable. The indicator reflected the percentage of adolescents (aged 11–17 years) enrolled in Medicaid as of January 2011 with at least one ADHD ICD diagnosis code (314.×) and at least one claim for a medication approved by the Food and Drug Administration for pediatric ADHD treatment (Table 1), based on National Drug Codes. This indicator was aggregated at county-level based on child addresses and merged with county-level school climate data to facilitate analysis, with counts of five or less suppressed to reduce disclosure risks.
Table 1.
List of FDA-approved ADHD medications* used in the abstraction of medication claims for Attention-Deficit/Hyperactivity Disorder among adolescents in Medicaid
| Medication | Drug Class |
|---|---|
| Adderall | Central nervous system stimulant (CNS Stimulant) |
| Atomoxetine | Selective norepinephrine reuptake inhibitor (SNRI) |
| Concerta | CNS Stimulant |
| Daytrana Patch | CNS Stimulant |
| Dexedrine | CNS Stimulant |
| Dextrostat | CNS Stimulant |
| Dextro-Amphetamine | CNS Stimulant |
| Dexmethylphenidate | CNS Stimulant |
| Focalin | CNS Stimulant |
| Guanfacine | Centrally acting alpha-adrenergic receptor agonist |
| Intuniv | Centrally acting alpha-adrenergic receptor agonist |
| Kapvay | Central alpha-2 agonist |
| Metadate | CNS Stimulant |
| Methylin | CNS Stimulant |
| Methylphidate | CNS Stimulant |
| Ritalin | CNS Stimulant |
| Strattera | SNRI |
| Tenex | Centrally acting alpha-adrenergic receptor agonist |
| Vyvanse | CNS Stimulant |
As of 2011
In order to confirm that the Medicaid ADHD medication indicator was a good proxy for medicated ADHD prevalence, state-based weighted estimates of medication treatment for ADHD were calculated for GA adolescents (aged 11–17 years) with Medicaid health insurance, using data from the 2011–12 National Survey of Children’s Health (NSCH) (Centers for Disease Control and Prevention, 2013). The NSCH is a national cross-sectional, random-digit–dialed telephone survey of parents that collects information about health and well-being of non-institutionalized US children. Detailed information about the ADHD-related survey content has been summarized previously (Susanna N. Visser et al., 2014). The survey data were analyzed using SUDAAN 11.0 to account for NSCH’s complex design. The ADHD prevalence estimate with its associated confidence interval was then compared to the state-based indicator for medicated ADHD among adolescents (aged 11–17 years) in Medicaid.
County-Level Demographic Indicators
The following county-level factors were collected from the 2012–2013 Area Health Resource Files (ahrf.hrsa.gov) and used as control factors in the analyses: 2011 county population, county urbanicity (metro, non-metro), black race proportion, proportion of children living below the poverty threshold, the ratio of pediatricians to children, and the presence of a Federally Qualified Health Center (FQHC) in the county. An index of each county’s overall health outcomes was also included as a covariate (Robert Wood Johnson, 2014). The county factors related to child race and poverty were dichotomized (median split) to facilitate analysis and interpretation. County population was dichotomized using the top two deciles as an indicator of a large county population.
Statistical Approach
There are 159 Georgia counties; 150 had valid 2011 ADHD claims and 2008 school climate survey data. In the absence of a clear claims data algorithm for ADHD prevalence, this analysis focused on medicated prevalence, which was operationalized by having at least one ADHD diagnosis code and at least one ADHD medication claim in 2011. ArcGIS 10.0 was used to depict GA county-level school climate percentiles and the percentages of medicated ADHD among adolescents in Medicaid. Because the school climate indicators were based on individual-level ratings and county size varies dramatically across GA counties, all analyses evaluating the relationship between school climate, medicated ADHD prevalence, and the control variables were weighted by county population.
Weighted t-tests were used to evaluate the relationship between the independent and dependent variable and each of the potential confounding variables of county urbanicity, large population size, black race proportion, proportion of children below the 2010 poverty threshold, and county presence of a FQHC. Bivariate weighted linear regression was used to evaluate the relationship between the independent and dependent variable and the continuous variables of pediatrician to child ratio and the county health outcome index.
Weighted linear regression models estimated 2011 ADHD medication treatment from 2008 school climate, while adjusting for county-level demographics that were significantly associated with either 2011 medicated ADHD prevalence or 2008 school climate. To determine if school climate had a similar impact on medicated ADHD prevalence in counties with higher and lower proportions of children in poverty, which relates to the generalizability of this Medicaid-based analysis, an interaction term was tested for proportion of poverty and school climate. The model also included the school climate change indicator and the interaction term for school climate and poverty. To ensure model parsimony, the independent factors were manually trimmed in a backward stepwise manner, removing the demographic factor with the highest p-value from the model, one at a time, until removal of remaining factors reduced the model variation explained (R2) by 10% or more.
Results
County Demographics
The 150 counties varied in population size from 1,717 to 920,581, with an average county size of 63,845 (standard deviation (SD)=130,284; median=23,577). On average, the counties were 25.7% black race (SD=16.6%; median=25.1%) and 70.3% white race (SD=16.5%; median=70.5%). The county average for the percentage of children living under the 2010 poverty threshold was 30.9% (SD=9.3%; median=31.6%).
School Climate
Of the 150 counties, 33 (22%) fell below the 25th percentile for state-wide 2008 school climate and were categorized as having poorer school climate (Figure 1). County-level school climate ratings for 2008 and 2011 were significantly and positively correlated (r=0.245; p=0.0038). Of the 138 counties with school climate data for both 2008 and 2011, 43.5% had declining school climate percentiles and the remaining 56.5% had stable or increasing school climate percentiles.
Figure 1.
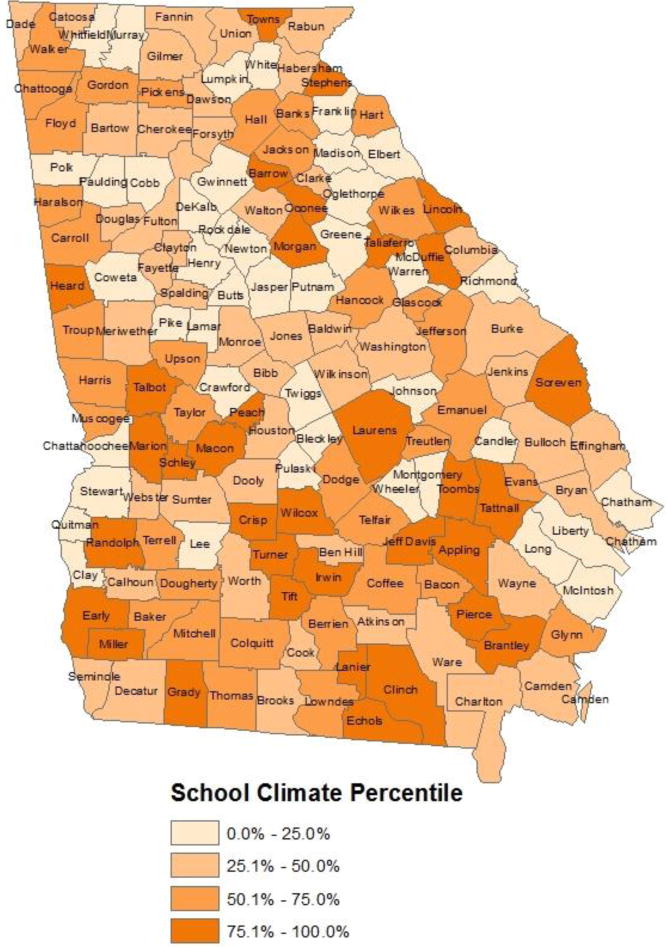
School climate percentile* by county in Georgia: Georgia Student Health Survey II, 2008
*School climate was assessed using the Georgia Student Health Survey II (Appendix), which assesses the quality and character of school life across four key areas (safety, interpersonal relationships, teaching and learning, and institutional environment).
Bivariate analyses revealed that better county-level school climate ratings were associated with the following county characteristics: non-metro, smaller population size, and higher rates of poverty (Table 2). A lower ratio of pediatricians to children was significantly associated with higher school climate percentiles (F(1,148)=11.27, p=0.001), as was better overall county health (F(1,146)=33.58, p<0.0001).
Table 2.
County* population-weighted bivariate relationships between county demographic factors, school climate percentile, and the prevalence of medicated Attention-Deficit/Hyperactivity Disorder (ADHD) among Georgia adolescents in Medicaid
| County Demographic Factor | Mean Weighted Percentile County School Climate | t | p-value | Mean Weighted % of Medicated ADHDˆ | t | p-value |
|---|---|---|---|---|---|---|
| % Black+ | ||||||
| Higher (>25%) | 33.9% | 7.0% | ||||
| Lower (<=25%) | 38.2% | 1.23 | 0.2209 | 8.6% | 3.39 | 0.0009 |
| Urbanicity | ||||||
| Metro | 31.3% | 7.0% | ||||
| Non-Metro | 55.1% | 5.90 | <0.0001 | 10.5% | 5.87 | <0.0001 |
| % Poverty+ | ||||||
| Higher (>32%) | 49.1% | 9.4% | ||||
| Lower (<=32%) | 29.8% | −5.59 | <0.0001 | 6.9% | −4.80 | <0.0001 |
| FQHCϮ in County | ||||||
| No | 39.5% | 9.1% | ||||
| Yes | 33.3% | 1.72 | 0.0869 | 6.8% | 4.73 | <0.0001 |
| Population Size** | ||||||
| Smaller (<=89,890) | 50.5% | 10.5% | ||||
| Larger (89,891–920,581) | 26.7% | 7.16 | <0.0001 | 6.1% | 10.18 | <0.0001 |
Based on data from 150 of 159 counties in Georgia with valid data on school climate, the demographic factors, and medicated ADHD.
The prevalence of medicated ADHD reflects the percentage of adolescents in Medicaid with at least one ADHD diagnosis code and at least one ADHD medication claim in 2011
Grouped by median split
FQHC = Federally Qualified Health Center
Grouped into top two deciles and bottom 8 deciles
ADHD Medication Treatment
In 2011, 30,951 Medicaid-enrolled adolescents had at least one ADHD diagnosis code and at least one ADHD medication code (7.8% of adolescents in Medicaid). The prevalence of ADHD medication treatment from Medicaid claims data was similar to, but slightly lower than, the 2011–12 NSCH estimate of the percentage of GA adolescents in Medicaid taking medication for ADHD treatment (8.4%, 95% confidence interval: 4.4%–15.6%), suggesting convergence of the two indicators ADHD medication treatment estimates for adolescents in Medicaid. The average percentage of adolescents in Medicaid with at least one ADHD diagnosis code and one ADHD medication code in each county was 10.0% (range: 3.9%–17.1%; SD=2.9%; Figure 2).
Figure 2.
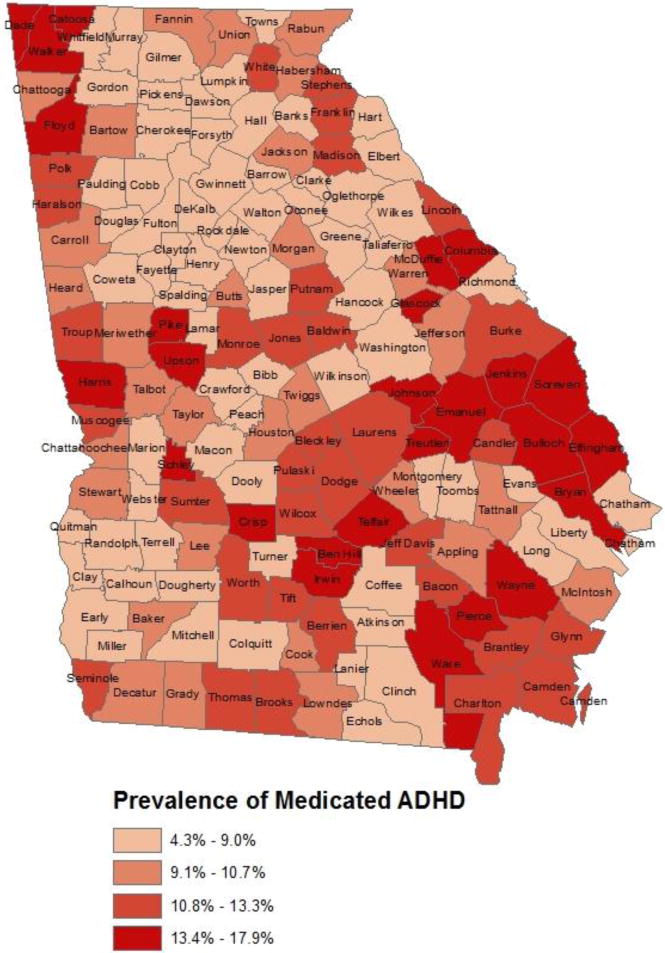
Prevalence of medicated Attention-Deficit/Hyperactivity Disorder* among adolescents (aged 11–17 years) in Medicaid: Georgia, 2011
*Attention-Deficit/Hyperactivity Disorder prevalence was assessed from 2011 Georgia Medicaid claims data, requiring at least one ADHD ICD-9 code (314.×) and at least one claim for an FDA-approved ADHD medication (see Table 1 for a list of medications).
Significant bivariate associations were identified for all seven potential confounding variables and percentage of medicated ADHD. Specifically, associations were found for higher county-level percentages of medicated ADHD and counties that were non-metro, less populous, did not have a FQHC in the county, had lower black race proportions, and had higher proportions of children in poverty (Table 2). A higher pediatrician to child ratio was significantly associated with lower medicated ADHD percentages (F(1,148)=33.38, p<0.0001). Better overall county health was also associated with higher percentages of medicated ADHD (F(1,145)=43.26, p<0.0001).
Poorer school climate (below 25th percentile) was significantly associated with lower county-level medicated ADHD percentages. Specifically, the county-level percentage of medicated ADHD among adolescents in Medicaid was 29.9% lower in poorer school climate counties (6.1%) than in counties with better school climate (8.7%; p<0.0001; Table 3).
Table 3.
Weighted regression analyses of the county-level* prevalence of medicated Attention-Deficit/Hyperactivity Disorder* (ADHD) among Georgia adolescents in Medicaid as a function of 2008 county-level school climate
| Crude Modelˆ | Adjusted Model+ | |||||||
|---|---|---|---|---|---|---|---|---|
| Factor | B | SE B | t | p | B | SE B | t | p |
| Intercept | 0.087 | 0.003 | 26.36 | <0.0001 | 0.112 | 0.004 | 27.90 | <0.0001 |
| Poorer School Climate (bottom quartile) | −0.026 | 0.005 | −5.19 | <0.0001 | −0.010 | 0.004 | −2.37 | 0.019 |
| Large Population Size (>=136,152) | −0.028 | 0.006 | −4.66 | <0.0001 | ||||
| Higher Proportion Black | −0.012 | 0.005 | −2.61 | 0.010 | ||||
| Health Outcome z-score | 0.009 | 0.004 | 2.48 | 0.0143 | ||||
The prevalence of medicated ADHD reflects the percentage of adolescents in Medicaid with at least one ADHD diagnosis code and at least one ADHD medication claim in 2011
Based on the 135 counties with valid data on all factors in the adjusted model; R2 = 0.1685; Adj. R2 = 0.1622; Model F = 26.36, p <0.0001
Based on the 135 counties with valid data on all factors in the adjusted model; R2 = 0.4990; Adj. R2 = 0.4836; Model F = 32.37, p <0.0001
Total variables entered into the full model before backward stepwise procedures included dichotomous indicators of 2011 county population, county urbanicity (metro, non-metro), black race proportion, proportion of children living below the poverty threshold, the ratio of pediatricians to children, the presence of a Federally Qualified Health Center (FQHC) in the county, and an index of each county’s overall health outcomes.
Multivariate Regression Models
Based on the weighted regression model, poorer 2008 school climate, large population size, higher proportions of black race, and lower county health outcome score were significantly associated with lower 2011 county-level medicated ADHD prevalence for adolescents in Medicaid (Table 3; F(1,130)=32.37, p<0.0001); these factors collectively accounted for 50% of the county variation in medicated ADHD. The multivariate results suggest that the highest percentages of medicated ADHD were among counties with better school climate ratings, smaller county population, a lower proportion of black race, and better county health. Conversely, the counties with the lowest medicated ADHD percentages had poorer school climate ratings, larger county population, a higher proportion of black race, and poorer county health.
Discussion
Contrary to expectations, in this county-level analysis, low student-perceived school climate was associated with lower rates of later medicated ADHD prevalence among GA adolescents enrolled in Medicaid, independently accounting for 20% of the variation in this county-level health care utilization outcome. The percentage of Medicaid-enrolled adolescents who received ADHD medication treatment was 29.9% lower in counties with poorer school climate, compared to those with better school climate. After controlling for potential confounders, poorer school climate remained significantly associated with lower ADHD medication rates, independently accounting for a decrease of approximately one percentage point in the county-level percentage of medicated ADHD among adolescents in Medicaid.
In the multivariate analysis, the demographic factors associated with low county-level medicated ADHD prevalence included large county population size, high proportion of black race, and poor overall county health. This was unexpected because adolescents with greater demographic risk would be expected to have more behavioral health problems, including ADHD, resulting in a greater need for ADHD medication treatment. Because medicated ADHD is a complex outcome, partially reflecting prevalence of the disorder and partially reflecting health care availability and access, considering each significant factor individually may serve to explain this complex set of findings.
Urban, more populous counties are typically more likely to receive preventative health care services, due to improved access to health care services and facilities (Casey, Thiede Call, & Klingner, 2001). In this analysis, more populous county size was the strongest predictor of lower medicated ADHD prevalence, independently accounting for a 2.8% lower rate of medicated ADHD. Having a FQHC in the county was associated with lower county-level medicated ADHD prevalence in bivariate analyses, although it was not a significant factor in the model alongside population size. One way of explaining this is that adolescents in larger, urban areas may have increased access to behavioral therapy by having greater access to specialists who provide these therapies (e.g., psychologists), potentially resulting in less reliance on pharmacological treatments.
After county population size, poorer school climate and high proportion of black race each accounted for slightly more than a one percentage point decrease in the county-level percentage of medicated ADHD. Previous research has documented that black children are just as likely to have and be diagnosed with ADHD, but are less likely to receive ADHD medication treatment (Morgan, Staff, Hillemeier, Farkas, & Maczuga, 2013; Susanna N. Visser et al., 2014). Our county-level results are consistent with these findings. Lower rates of medicated ADHD among black children may result from cultural differences in the perception of ADHD diagnosis and medication treatment (Bussing, Schoenberg, & Perwien, 1998; Yeh, Hough, McCabe, Lau, & Garland, 2004) or health care utilization barriers.
Better overall county health was significantly associated with higher ADHD medication rates. Although one might expect counties with higher county health ratings to have better adolescent behavioral health, healthier counties may also be more likely to have greater health care utilization overall, resulting in higher county-level ADHD medication rates. Future research that incorporates a direct assessment of behavioral health taking into account school climate, ADHD-related health care utilization, and demographics could disentangle these contextual factors.
Given the extensive research documenting association between better school climate and fewer student- and teacher-reported internalizing and externalizing problems (Kuperminc, Leadbeater, & Blatt, 2001; Kuperminc et al., 1997), it was surprising that better school climate was not associated with less ADHD medication treatment. The similarity between the GA NSCH parent survey estimate and GA Medicaid rate suggests that the Medicaid claims indicator is a valid indicator of medicated ADHD among adolescents in Medicaid and reduces the likelihood that this finding is spurious. One explanation for this finding is that poorer school climate may be associated with factors that negatively influence health care utilization patterns, resulting in unexpectedly low rates of medicated ADHD. For example, schools with poorer school climate could be less attentive to student behavioral needs, resulting in lower rates of student referrals for behavioral assessment and lower subsequent rates of ADHD-related health care utilization. Indeed, improving school climate is recommended as a strategy to increase school connectedness (Centers for Disease Control and Prevention, 2009) and the GA school climate survey specifically asks about the availability of a counselor that would help a needy student. Therefore, better school climate could reflect greater connectedness between students and school staff and, potentially, greater connection to behavioral resources that include ADHD-related health care utilization.
It is also important to recognize that higher rates of ADHD medication treatment do not necessarily constitute a better outcome. Although it is important that children with ADHD receive evidence-based ADHD treatments to improve their functional, developmental, and health outcomes (American Academy of Pediatrics, 2011), there is also concern about risk of over-medication, particularly in light of rapidly increasing rates of medicated ADHD (Setlik et al., 2009; Susanna N. Visser et al., 2014). It may be appropriate to be concerned both about counties with the lowest (4%, approximately half the state-average) and highest (17%, more than twice the state-average) rates of medicated ADHD. While school climate may be an important correlate of ADHD medication treatment, it is important to consider other factors that relate to higher rates of medicated ADHD, particularly among smaller, predominantly white GA counties.
There are several important limitations to this county-level analysis. First, this study focused on Georgia adolescents in Medicaid and the results are not necessarily generalizable to other states, children with other insurance, or children in poverty who are eligible but not enrolled in Medicaid. Second, 21 Georgia city school districts were allocated to counties for analysis, making it impossible to determine if there were unique patterns among city districts. Third, school climate data were collected from public school students and do not represent the 7.5% of Georgia students in private schools. Finally, and importantly, the school climate surveys were anonymous and could not be linked to claims data at the individual-level. Therefore, this study is subject to the limitations of ecological analyses in that without individually-linked data, findings can suggest but not determine relationships between the county-level factors. Further, the analysis is relatively crude in that it does not account for the intra-county variation of school climate ratings.
Despite these limitations, this study is the first of its kind to use school climate data and behavioral health claims data to help us better understand the relationship between school climate and medicated ADHD, an indicator of socio-emotional and behavioral health. Results of this analysis suggest that school climate improvement is associated with more health care utilization and ADHD medication treatment in particular, among adolescents in Medicaid. This finding adds to the body of knowledge that suggests that school-related factors may play a role in medicated ADHD prevalence (Connor, 2011; Hinshaw & Scheffler, 2014; McDonald & Jalbert, 2013). School climate is modifiable and typically asset-based. Therefore, if ADHD is undertreated in some schools, then school climate improvement may benefit the outcomes of adolescents with ADHD in Medicaid, further supporting efforts to train school staff on multi-tiered school climate improvement programs (U.S. Department of Education, 2014). However, additional research is needed to better understand factors related to high county-level medicated ADHD rates and if these counties lack access to other evidence-based ADHD treatments, such as behavioral therapy.
Implications and Contribution.
This county-level analysis is the first to evaluate ADHD-related health care utilization as a function of school climate. The results suggest that poorer school climate is associated with lower ADHD medication rates among adolescents in Medicaid. Better school climate is related to and may promote ADHD-related health care utilization, specifically ADHD medication treatment.
Footnotes
Publisher's Disclaimer: Disclaimers:
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- Akinbami LJ, Liu X, Pastor PN, Reuben CA. NCHS data brief. Vol. 70. Hyattsville, MD: CDC National Center for Health Statistics; 2011. Attention deficit hyperactivity disorder among children aged 5–17 years in the United States, 1998–2009. [PubMed] [Google Scholar]
- American Academy of Child and Adolescent Psychiatry. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2007;46(7):894–921. doi: 10.1097/chi.0b013e318054e724. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics. ADHD: Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128(5):1007–1022. doi: 10.1542/peds.2011-2654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. American Psychiatric Publishing; 2013. [Google Scholar]
- Barbaresi WJ, Colligan RC, Weaver AL, Voigt RG, Killian JM, Katusic SK. Mortality, ADHD, and psychosocial adversity in adults with childhood ADHD: a prospective study. Pediatrics. 2013;131(4):637–644. doi: 10.1542/peds.2012-2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bussing R, Schoenberg NE, Perwien AR. Knowledge and information about ADHD: Evidence of cultural differences among African-American and White parents. Soc Sci Med. 1998;46(7):919–928. doi: 10.1016/s0277-9536(97)00219-0. [DOI] [PubMed] [Google Scholar]
- Casey MM, Thiede Call K, Klingner JM. Are rural residents less likely to obtain recommended preventive healthcare services? American Journal of Preventive Medicine. 2001;21(3):182–188. doi: 10.1016/S0749-3797(01)00349-X. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. School connectedness: Strategies for increasing protective factors among youth. Atlanta, GA: U.S. Department of Health and Human Services; 2009. [Google Scholar]
- Centers for Disease Control and Prevention. 2011–2012 National Survey of Children’s Health Frequently Asked Questions. 2013 Apr; 2013. from http://www.cdc.gov/nchs/slaits/nsch.htm.
- Centers for Disease Control and Prevention. State Profile: Georgia. Parent-Reported Diagnosis of ADHD by a Health Care Provider and Medication Treatment Among Children 4–17 Years: National Survey of Children’s Health* – 2003 to 2011. 2014 Retrieved January, 18, 2014, 2014 from http://www.cdc.gov/ncbddd/adhd/stateprofiles/stateprofile_Georgia.pdf.
- Cohen J, Geier VK. School Climate Research Summary. Vol. 1. Center for Social and Emotional Education; 2010. [Google Scholar]
- Connor DF. Problems of Overdiagnosis and Overprescribing in ADHD. Psychiatric Times. 2011 http://www.psychiatrictimes.com/adhd/problems-overdiagnosis-and-overprescribing-adhd.
- de Graaf R, Kessler RC, Fayyad J, Ten Have M, Alonso J, Angermeyer M, Posada-Villa J. The prevalence and effects of Adult Attention-Deficit/hyperactivity Disorder (ADHD) on the performance of workers: Results from the WHO World Mental Health Survey Initiative. Occup Environ Med. 2008 doi: 10.1136/oem.2007.038448. published online 27 May 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiScala C, Lescohier I, Barthel M, Li G. Injuries to children with Attention Deficit Hyperactivity Disorder. Pediatrics. 1998;102(6):1415–1421. doi: 10.1542/peds.102.6.1415. [DOI] [PubMed] [Google Scholar]
- Doshi JA, Hodgkins P, Kahle J, Sikirica V, Cangelosi MJ, Setyawan J, Neumann PJ. Economic Impact of Childhood and Adult Attention-Deficit/Hyperactivity Disorder in the United States. Journal of the American Academy of Child & Adolescent Psychiatry. 2012;51(10):990–1002. doi: 10.1016/j.jaac.2012.07.008. [DOI] [PubMed] [Google Scholar]
- Fulton BD, Scheffler RM, Hinshaw SP, Levine P, Stone S, Brown TT, Modreck S. National variation of ADHD diagnostic prevalence and medication use: Health care providers and education policies. Psychiatric Services. 2009;60(8):1075–1083. doi: 10.1176/ps.2009.60.8.1075. [DOI] [PubMed] [Google Scholar]
- Graf WD, Nagel SK, Epstein LG, Miller G, Nass R, Larriviere D. Pediatric neuroenhancement: Ethical, legal, social, and neurodevelopmental implications. Neurology. 2013;80(13):1251–1260 d. doi: 10.1212/WNL.0b013e318289703b. [DOI] [PubMed] [Google Scholar]
- Harpin VA. The effect of ADHD on the life of an individual, their family, and community from preschool to adult life. Archives of Diseases in Childhood. 2005;90(Suppl 1):i2–7. doi: 10.1136/adc.2004.059006. 90/suppl_1/i2 [pii] 10.1136/adc.2004.059006 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinshaw SP, Scheffler RM. The ADHD Explosion: Myths, Medication, Money, and Today’s Push for Performance. USA: Oxford University Press; 2014. [Google Scholar]
- Hoare P, Beattie T. Children with Attention Deficit Hyperactivity Disorder and attendance at hospital. Eur J Emerg Med. 2003;10(2):98–100. doi: 10.1097/01.mej.0000072631.17469.71. [DOI] [PubMed] [Google Scholar]
- Hoge DR, et al. School Experiences Predicting Changes in Self-Esteem of Sixth- and Seventh-Grade Students. Journal of Educational Psychology. 1990;82(1):117–127. [Google Scholar]
- Kuperminc GP, Leadbeater BJ, Blatt SJ. School Social Climate and Individual Differences in Vulnerability to Psychopathology among Middle School Students. Journal of School Psychology. 2001;39(2):141–159. doi: 10.1016/S0022-4405(01)00059-0. [DOI] [Google Scholar]
- Kuperminc GP, Leadbeater BJ, Emmons C, Blatt SJ. Perceived School Climate and Difficulties in the Social Adjustment of Middle School Students. Applied Developmental Science. 1997;1(2):76–88. doi: 10.1207/s1532480xads0102_2. [DOI] [Google Scholar]
- Loe I, Feldman H. Academic and Educational Outcomes of Children With ADHD. J Pediatr Psychol. 2007;32(6):643–654. doi: 10.1093/jpepsy/jsl054. [DOI] [PubMed] [Google Scholar]
- McDonald DC, Jalbert SK. Geographic Variation and Disparity in Stimulant Treatment of Adults and Children in the United States in 2008. Psychiatric Services. 2013;64(11):1079–1086. doi: 10.1176/appi.ps.004442012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrill R, Lyon J, Baker R, Gren L. Attention Deficit Hyperactivity Disorder and increased risk of injury. Advances in Medical Sciences. 2009;54(1):20–26. doi: 10.2478/v10039-009-0022-7. [DOI] [PubMed] [Google Scholar]
- Morgan PL, Staff J, Hillemeier MM, Farkas G, Maczuga S. Racial and Ethnic Disparities in ADHD Diagnosis From Kindergarten to Eighth Grade. Pediatrics. 2013 doi: 10.1542/peds.2012-2390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National School Climate Council. School Climate. 2007 Retrieved 6/18/2013 from http://www.schoolclimate.org/climate/
- Perou R, Bitsko RH, Blumberg SJ, Pastor P, Ghandour RM, Gfroerer JC, Huang LN. Mental health surveillance among children–United States, 2005–2011. MMWR Surveill Summ. 2013;62(Suppl 2):1–35. [PubMed] [Google Scholar]
- Robert Wood Johnson. County Health Rankins and Roadmaps: Data Sources and Measures. 2014 Retrieved Jauary 18, 2014 from http://www.countyhealthrankings.org/ranking-methods/data-sources-and-measures.
- Setlik J, Bond GR, Ho M. Adolescent prescription ADHD medication abuse Is rising along with prescriptions for these medications. Pediatrics. 2009;124(3):875–880. doi: 10.1542/peds.2008-0931. [DOI] [PubMed] [Google Scholar]
- Sommer B. What’s different about truants? A comparison study of eighth-graders. Journal of Youth and Adolescence. 1985;14(5):411–422. doi: 10.1007/BF02138836. [DOI] [PubMed] [Google Scholar]
- Sylva K. School influences on children’s development. J Child Psychol Psychiatry. 1994;35(1):135–170. doi: 10.1111/j.1469-7610.1994.tb01135.x. [DOI] [PubMed] [Google Scholar]
- Thapa A, Cohen J, Guffey S, Higgins-D’Alessandro A. A Review of School Climate Research. Review of Educational Research. 2013 doi: 10.3102/0034654313483907. [DOI] [Google Scholar]
- U.S. Department of Education. OSEP Center on Positive Behavioral Intervenions and Supports: Effective Schoolwide Interventions. 2014 Retrieved January 18, 2014, from http://www.pbis.org/default.aspx.
- Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD, Ghandour RM, Blumberg SJ. Trends in the Parent-Report of Health Care Provider-Diagnosed and Medicated Attention-Deficit/Hyperactivity Disorder: United States, 2003–2011. J Am Acad Child Adolesc Psychiatry. 2014;53(1):34–46. doi: 10.1016/j.jaac.2013.09.001. e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser SN, Danielson ML, Bitsko RH, Perou R, Blumberg SJ. Convergent validity of parent-reported attention-deficit/hyperactivity disorder diagnosis: A cross-study comparisonconvergent validity of parent-reported adhdletters. JAMA Pediatrics. 2013;167(7):674–675. doi: 10.1001/jamapediatrics.2013.2364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Way N, Reddy R, Rhodes J. Students’ perceptions of school climate during the middle school years: associations with trajectories of psychological and behavioral adjustment. Am J Community Psychol. 2007;40(3–4):194–213. doi: 10.1007/s10464-007-9143-y. [DOI] [PubMed] [Google Scholar]
- Wolraich ML, Bard DE, Stein MT, Rushton JL, O’Connor KG. Pediatricians’ attitudes and practices on ADHD before and after the development of ADHD pediatric practice guidelines. J Atten Disord. 2010;13(6):563–572. doi: 10.1177/1087054709344194. [DOI] [PubMed] [Google Scholar]
- Yeh M, Hough RL, McCabe K, Lau A, Garland A. Parental beliefs about the causes of child problems: exploring racial/ethnic patterns. J Am Acad Child Adolesc Psychiatry. 2004;43(5):605–612. doi: 10.1097/00004583-200405000-00014. [DOI] [PubMed] [Google Scholar]


