To the Editor
Antipsychotic (AP) medications are often used in the hospitalized geriatric population for the treatment of delirium.(1) Because of adverse events associated with APs, efforts have been made to reduce their use in hospitalized elders;(2) but it is not clear if these recommendations have been widely adopted. We studied the use of APs in a cohort of hospitalized elders to better understand why APs are started and how often they are continued on discharge.
Methods
We conducted a retrospective cohort study of patients 65 years or older admitted to a tertiary care hospital between 10/1/2012 and 9/31/2013. Using STATA’s “sample” command,(3) we included a subset of randomly selected inpatients who received more than 1 dose of oral APs (determined using the electronic medication administration summary). We excluded patients admitted under observation status or to the psychiatric service, those who were on APs prior to admission and those who only received prochloperazine for nausea. Using prior literature to identify terms frequently used to describe delirium, (Figure 1) we created an algorithm and a chart abstraction form (Appendix 1).(4) We tested these instruments in a preliminary chart review involving 30 patients. Disagreements were discussed with co-authors and resolved through consensus, resulting in some algorithm changes (e.g., excluding a large number of patients who received only one dose of haloperidol postoperatively because we hypothesized that this use could be prophylactic measure).(5) Two investigators extracted the remaining charts independently. We used descriptive statistics and performed cross-tabulations on the selected variables.
Figure 1.
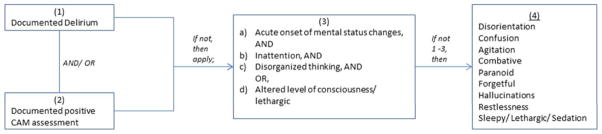
Methodology for defining Delirium during chart review
Results
Of 12,817 geriatric hospitalizations during the study period, 1120 (9%) were treated with antipsychotics. We randomly selected 300 of these for extraction: 54% were male and 67% were admitted to the medical service.(Table 1) The inpatient mortality rate was 10% (30/300). The most frequent indication for AP use was delirium (83%, 249/300). Only 35% of delirious patients received a formal assessment with the Confusion Assessment Method (CAM). The most commonly used atypical antipsychotic was quetiapine (86%); 55% received more than one antipsychotic medication during hospitalization, and 48% (143/297) of patients were continued on APs at discharge (excluding 3 patients transferred to other acute care hospitals).
Table 1.
Demographic data and circumstances surrounding APs initiation
| Variable | N (%) Total = 300 |
|---|---|
| Gender | |
| Male | 161 (54) |
| Female | 139 (46) |
|
| |
| Inpatient Mortality Rate | 30 (10) |
|
| |
| Services | |
| Medicine | 202 (67) |
| Surgery | 98 (33) |
|
| |
| Indication for APs use | |
| Delirium | 249 (83) |
| Hallucinations | 19 (6) |
| Anxiety | 20 (7) |
| Other | 38 (13) |
|
| |
| Atypical APs | |
| Quetiapine | 257 (86) |
| Olanzapine | 29 (10) |
| Risperidone | 26 (9) |
|
| |
| Typical APs | |
| Haloperidol | 166 (55) |
| Thorazine | 4 (1) |
|
| |
| Use of CAM | 79 (32)a |
|
| |
| Physical Restraints | 89 (30) |
|
| |
| Documented or Suspected Dementia | 134 (45) |
|
| |
| Geriatrics Consults | 120 (40) |
|
| |
| Psychiatric Consults | 29 (10) |
|
| |
| EKG | |
| Prior to APs Administration | 265 (88) |
| After APs Administration | 157 (52) |
|
| |
| QTc Prolongation >500msec | |
| Prior to APs Administration | 41 (15)b |
| After APs Administration | 39 (25)c |
|
| |
| Admitted from SNF | 36 (12) |
|
| |
| Discharge Destination | |
| Home | 68 (23) |
| SNFs, Short & Long-term Rehabilitations | 199 (66) |
| Transfer to Other Acute Care Hospitals | 3 (1) |
|
| |
| Continuation of APs at discharge | 143 (48)d |
Abbreviations: APs, antipsychotics; CAM, confusion assessment method; QTc, QT interval; SNF, skilled nursing facility.
Denominator = 249; number of patients on whom APs were started for delirium
Denominator = 265; number of patients with EKG performed prior to APs administration
Denominator = 157; number of patients with EKG performed after APs administration
Denominator = 297; three patients who were transferred to other acute care hospitals were excluded
Approximately 45% (134/300) had documented or suspected dementia, and 30% (89/300) were physically restrained during the hospital stay. Consultations with Geriatrics were obtained in 40% (120/300) of the cases; with Psychiatry, 10% (29/300) of cases. Neurology is rarely consulted for delirium in our institution; thus, we did not collect data on those referrals. EKGs (recommended for patients at high cardiac risk (6)) were performed in 88% (265/300) of patients prior to AP administration and 52% (157/300) after. The corrected QT interval (QTc) exceeded 500 milliseconds in 15% (41/265) of patients prior to APs administration and 25% (39/157) after. Although few patients (12%) were admitted from nursing facilities, 66% (199/300) were eventually discharged to SNFs or rehabilitation facilities; most of these patients (117/199, 59%) received APs treatment, compared to 38% of patients discharged home (26/68).
Discussion
In a cohort of hospitalized elders, we found that 9% were treated with APs. Most received APs for perceived delirium; in-hospital EKG monitoring was suboptimal. Half of patients started on APs remained on them at discharge; those discharged to SNFs were more likely to receive ongoing AP treatment.
Our study is limited by its retrospective, single-center design, a lack of inter-rater reliability measurement (although our training process was designed to standardize extraction methods), and the infrequent use of formal CAM assessment. Additionally, we were unable to determine how frequently APs were initiated in the ICU. Any retrospective study is limited by the difficulty of distinguishing delirium from the behavioral and psychiatric symptoms of dementia, but we identified delirium using standard terms described in previous literature.
Our study also has a number of important implications. Because of a reported association between use of APs and risk of death in the post-acute setting,(7) national provider organizations have called for a reduction in AP initiation in hospitalized elders.(2) Yet, this study indicates that APs continue to be prescribed for delirium, which may be attributed to the lack of behavioral modification options in most hospitals, such as Acute Care for Elders (ACE) units and Hospital Elder Life Programs (HELP). Our findings suggest that this problem would be further amplified in hospitals that lack access to geriatrics expertise.
Without alternative behavioral options, patients are at risk for prolonged delirium, which is associated with significant suffering and subsequent risk of further cognitive impairment and death.(8) Although evidence for the efficacy of APs in the treatment of delirium is limited and inconclusive, no better pharmacologic options exist. Hospitals that wish to reduce use of APs should therefore consider investing in environmental interventions (e.g., ACE units, HELP) that lower the incidence of delirium and could, in turn, decrease the prescription and continuation of antipsychotics. (9, 10)
Supplementary Material
Acknowledgments
Funding: Dr. Lagu is supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number K01HL114745.
We would like to acknowledge Michaela Stefan, MD, FACP for her comments on an earlier draft of this manuscript.
Footnotes
Author Contributions: Drs. Lagu and Loh had full access to all of the data in the study. They take responsibility for the integrity of the data and the accuracy of the analysis. Drs. Loh, Brennan, Lindenauer and Lagu conceived of the study. Drs. Loh and Ramdass acquired the data. Ms Garb analyzed and interpreted the data. Dr. Loh drafted the manuscript. Drs Brennan, Lindenauer and Lagu and Ms. Garb critically reviewed the manuscript for important intellectual content.
Conflict of Interest
The authors have no conflicts of interest.
References
- 1.Witlox J, Eurelings LSM, de Jonghe JFM, Kalisvaart KJ, Eikelenboom P, van Gool WA. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA. 2010 Jul 28;304(4):443–451. doi: 10.1001/jama.2010.1013. [DOI] [PubMed] [Google Scholar]
- 2.Flores L. Off-label use of antipsychotics for dementia patients discouraged. [Accessed June 29, 2014];The Hospitalist. 2012 Nov; Available from: http://www.the-hospitalist.org/details/article/2785121/Off-Label_Use_of_Antipsychotics_for_Dementia_Patients_Discouraged.html.
- 3.StataCorp. STATA/MP. 13.1 for Windows. College Station, TX: StataCorp; 2013. [Google Scholar]
- 4.Rothberg MB, Herzig SJ, Pekow PS, Avrunin J, Lagu T, Lindenauer PK. Association between sedating medications and delirium in older inpatients. J Am Geriatr Soc. 2013 Jun;61(6):923–930. doi: 10.1111/jgs.12253. [DOI] [PubMed] [Google Scholar]
- 5.Wang W, Li H-L, Wang D-X, et al. Haloperidol prophylaxis decreases delirium incidence in elderly patients after noncardiac surgery: a randomized controlled trial. Crit Care Med. 2012 Mar;40(3):731–739. doi: 10.1097/CCM.0b013e3182376e4f. [DOI] [PubMed] [Google Scholar]
- 6.Shah AA, Aftab A, Coverdale J. QTc prolongation with antipsychotics: is routine ECG monitoring recommended? J Psychiatr Pract. 2014 May;20(3):196–206. doi: 10.1097/01.pra.0000450319.21859.6d. [DOI] [PubMed] [Google Scholar]
- 7.Schneeweiss S, Setoguchi S, Brookhart A, Dormuth C, Wang PS. Risk of death associated with the use of conventional versus atypical antipsychotic drugs among elderly patients. CMAJ. 2007 Feb 27;176(5):627–632. doi: 10.1503/cmaj.061250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cole MG, Ciampi A, Belzile E, Zhong L. Persistent delirium in older hospital patients: a systematic review of frequency and prognosis. Age Ageing. 2009 Jan;38(1):19–26. doi: 10.1093/ageing/afn253. [DOI] [PubMed] [Google Scholar]
- 9.Fox MT, Persaud M, Maimets I, et al. Effectiveness of acute geriatric unit care using acute care for elders components: a systematic review and meta-analysis. J Am Geriatr Soc. 2012 Dec;60(12):2237–2245. doi: 10.1111/jgs.12028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Inouye SK, Bogardus ST, Baker DI, Leo-Summers L, Cooney LM. The Hospital Elder Life Program: a model of care to prevent cognitive and functional decline in older hospitalized patients. J Am Geriatr Soc. 2000 Dec;48(12):1697–1706. doi: 10.1111/j.1532-5415.2000.tb03885.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


