Abstract
To examine the associations among social-emotional support, life satisfaction, and mental health with not having a routine checkup among women of reproductive age in the US, data from the 2009 Behavioral Risk Factor Surveillance System, a population-based telephone survey of health behaviors, were analyzed among reproductive aged (18–44 years) women in the US. Prevalence estimates were calculated for not having a routine checkup in the past year with measures of social-emotional support, life satisfaction, and mental distress. Independent multivariable logistic regressions for each measure assessed not having a routine checkup within the past year with adjustment for age, race/ethnicity, education level, and health care coverage. Among women of reproductive age, 33.7 % (95 % CI 33.0–34.4) did not have a routine checkup within the past year. Factors associated with not having a routine checkup included: having social-emotional support most of the time (AOR = 1.29, 95 % CI 1.20–1.38) or sometimes or less (AOR = 1.47, 95 % CI 1.34–1.61) compared to those who reported always having the social-emotional support they need; reporting life satisfaction as being satisfied (AOR = 1.27, 95 % CI 1.19–1.36) or dissatisfied (AOR = 1.65, 95 % CI 1.43–1.91) compared to being very satisfied; and frequent mental distress (AOR = 1.19, 95 % CI 1.09–1.30) compared to those without. Women who report lower levels of social-emotional support, less life satisfaction, and frequent mental distress are less likely to see a doctor for a routine checkup. Targeted outreach that provides appropriate support are needed so these women can access clinical services to increase exposure to preventive health opportunities and improve overall health.
Keywords: Social-emotional support, Mental health, Life satisfaction, Health services utilization, Behavioral Risk Factor Surveillance System
Introduction
Health is complex and defined by the World Health Organization (WHO) as not just the absence of disease but a state of complete physical, mental, and social well-being [1]. Access to appropriate health services including preventive health or routine visits is an important heath determinant. It may be helpful to characterize the WHO components of mental and social well-being by looking at associations between health care utilization and potentially modifiable measures of social-emotional support, life satisfaction, and mental health.
Social support includes positive relationships, encouragement, and emotional support that is often provided by a network of family, friends, colleagues, and others [2]. Social support is closely tied to effective coping [3] and has health-protective properties [4, 5]. Social support has been associated with reduced morbidity and mortality [6] and been found to aid successful aging [7]. Social support may contribute to these effects through many mechanisms including promoting better adherence to diet [8] and physical activity recommendations [9–11], as well as utilization of medical treatments and screenings [12, 13].
Life satisfaction, a subjective self-evaluation of an individual’s overall contentment with life and well-being [14–16], is a Healthy People 2020 marker of quality of life [17]. Associations have been documented between dissatisfaction with life and increased risk for all-cause morbidity, chronic conditions, injury, and mortality. Life satisfaction is associated with positive health behaviors, higher levels of self-reported health, decreasing prevalence of obesity, as well as smoking, heavy drinking, and physical inactivity [18, 19].
Mental distress can be intermittent or chronic and refers to a wide range of experiences, including stress, depression, and emotional problems. Frequent mental distress (mental health problems experienced on 14 or more of the past 30 days) has been found to be associated with unhealthy and high-risk behaviors such as smoking, alcohol and drug use [20–22, 26, 27]. Mental distress is also associated with medical conditions such as heart disease, asthma, and arthritis, as well as health outcomes such as mortality and hospitalizations. [23–25].
Routine checkups, during which clinical services are performed for a person who may not have any signs or symptoms of an illness [28], are an important aspect of preventive health care. The routine checkup also provides an opportunity for primary caregivers to offer personalized behavioral counseling to patients [29], provide recommended screenings [30, 31] and promote healthy behaviors. Those who regularly see doctors for health examinations develop a trusting relationship with physicians, and are more likely to receive preventive screening than those who only see doctors for treatment episodically [32]. The routine checkup is a cost-effective means of reducing morbidity and mortality caused by chronic diseases [30], since much of the morbidity and mortality related to chronic disease in the US is attributable to modifiable health behaviors [25, 31, 33] that could be addressed during a routine checkup. Routine periodic health exams provide opportunities for promoting healthy behaviors and chronic disease prevention.
Previous research on the effects of social, emotional, and mental health on the utilization of health services such as a routine checkup has not yet yielded a clear picture of these relationships. One previous study found that social support was positively associated with service use and annual physical examination use in older adults [34], which may suggest that social networks aid users in gaining access to care [32]. Contrastingly, other studies have found that lower social support was associated with higher health services utilization in a general population of adults [32, 35]. Variability in the conceptualization and categorization of social support [36] and the utilization of health services may have led to these mixed findings. Little research has examined the association between life satisfaction and health behaviors [19, 37]; with most existing studies conducted in the 1970s [19, 38–40]. An association has been shown to exist between increased distress and reduced utilization of health services [35]. In a study of older adults, frequent mental distress was shown to decrease the likelihood of practicing positive health behaviors and utilizing preventative health care services [31].
Overall, women are about twice as likely to receive a regular medical examination than men [28, 32]. However a recent study using BRFSS data demonstrated that women aged 25–44 were significantly less likely than women older than 44 to have had a recent checkup [28]. In addition to benefits provided to the women themselves, counseling on medical and behavioral risks provided during a routine checkup can improve pregnancy outcomes through the provision of anticipatory guidance [41]. Furthermore, women are more likely to experience life dissatisfaction [19] and frequent mental distress [31] than men, and these factors may have stronger associations with health services utilization for women. For example, in a study of Canada’s general population from 1994–1995, social structural and psychosocial determinants of health including social support was shown to generally have a stronger effect in women whereas behavioral determinants were generally more important in men [42]. No comparable examination of social and mental health on the utilization of health services for the US population could be found.
The main objective of this study was to examine the associations between social-emotional support, life satisfaction, and mental health with not having a routine checkup among women of reproductive age (18–44 years) in the US. Identifying relationships among these psychosocial measures among women, variation across sub-populations, and how they relate to receipt of routine checkups may contribute to focused strategies to increase access to clinical services and improve overall health outcomes.
Methods
Data Source
The Behavioral Risk Factor Surveillance System (BRFSS) is a state-based cross-sectional telephone survey of adults 18 years of age and older conducted each year by state health departments in collaboration with the Centers for Disease Control and Prevention. The BRFSS uses a standardized questionnaire to determine the distribution of demographic variables, health practices, risk behaviors, and health care access among the non-institutionalized adult population in the US. The Council of American Survey Research Organization (CASRO) response rate reflects both telephone sampling efficiency and the degree of participation among eligible respondents who were contacted. In 2009, the BRFSS median CASRO rate was 53 % and ranged from 38 to 67 % among states. The cooperation rate reflects the proportion that completed an interview among eligible persons contacted. The median cooperation rate for BRFSS in 2009 was 75 % and ranged from 55 to 88 % among states. Detailed information on the sampling methodology, survey weighting procedures, quality assurance of the survey, and other aspects of this survey is available online at http://www.cdc.gov/brfss/index.htm. Relative to other surveys, data from BRFSS have acceptable reliability and validity [43].
Study Participants
In 2009, a total of 67,730 women of reproductive age (18–44 years) completed the BRFSS. Women who responded “don’t know/not sure”, who refused to respond, or who were missing data for the question on time since last routine doctor visit (n = 776) were excluded from analysis. The final analysis sample included 66,954 women.
Dependent Variable
Having a routine checkup in the previous year was the primary outcome and was grouped into a dichotomous variable: had a checkup in the past year or no checkup in the past year from the available response options (Table 1).
Table 1.
Survey questions for social-emotional and mental health measures and routine checkups, BRFSSa, 2009
| Measure | Survey question | Response choices |
Categories for analysis |
Labels |
|---|---|---|---|---|
| Social-emotional support |
How often do you get the social and emotional support you need? |
Always Usually Sometimes Rarely Never |
Always Usually Sometimes, rarely, or never (lowest level) |
Always Most of the Time Sometimes or less |
| Life satisfaction | In general, how satisfied are you with your life? |
Very satisfied Satisfied Dissatisfied Very dissatisfied |
Very satisfied Satisfied Dissatisfied or very dissatisfied |
Very satisfied Satisfied Dissatisfied |
| Mental distress | Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good? |
Number of days (0-30) | <14 days >14 days (frequent mental distress) |
No Yes |
| Routine checkup | About how long has it been since you last visited a doctor for a routine checkup? A routine checkup is a general physical exam, not an exam for a specific injury, illness, or condition. |
Within past year Within past 2 years Within past 5 years 5 or more years ago Don’t know/Not sure Never |
Within past year Not within the past year |
Yes No |
Behavioral Risk Factor Surveillance System
Independent Variables
In this study, there were three primary independent variables: social-emotional support, life satisfaction, and mental distress derived from the available response options for each question (Table 1, Fig. 1). Social-emotional support was grouped into three categories: Always, Most of the Time, and Sometimes or Less. Life satisfaction was also grouped into three categories: Very Satisfied, Satisfied, and Dissatisfied. Frequent mental distress was grouped into a dichotomous variable: of No for less than 14 days versus Yes for 14 or more days of mental distress in the past 30 days. This dichotomization is consistent with literature examining frequent mental distress in BRFSS analyses [31]. For each independent variable, respondents who refused to answer, did not know the answer to a question, or had a missing response were excluded from analysis of the specific question. Missing responses for each variable ranged from 1 to 7 %. These three variables were highly correlated with each other and were analyzed separately in order to avoid the impact on the variance of parameter estimates that might result from collinearity.
Fig. 1.
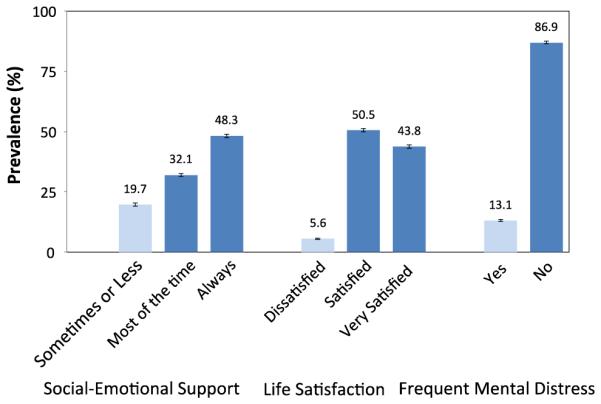
Distribution of socio-emotional support, life satisfaction, and frequent mental distress among women of reproductive age, US 2009
Covariates
Age was categorized into six groups: 18–24, 25–29, 30–34, 35–39, and 40–44. Self-identified race/ethnicity included non-Hispanic white, non-Hispanic black, Hispanic (any race), Asian, Native American, or all others. For this report, the terms white and black refer to non-Hispanic whites and non-Hispanic blacks, respectively. Native American was used for both American Indian and Alaska Natives. The “other” race category included the heterogeneous group of Native Hawaiians, Pacific Islanders, other racial groups, and those who indicated more than one race. Education level was classified as: less than a high school diploma or graduate equivalency degree (GED), high school diploma or GED, some college, and college graduate. Annual household income was classified into quintiles as follows to account for the distribution of income in BRFSS: less than $10,000, $10,000–$19,999, $20,000–$34,999, $35,000–$49,999, $50,000 or more, and refused or not known. Health care coverage status was categorized as those that were covered by health insurance, prepaid plans, or government plans compared to those without any health care coverage. Employment status was dichotomized with employed for wages and self-employed considered “Employed,” and being out of work, homemaker, student, retired, or unable to work considered “Not employed.” Marital status was dichotomized into married and “Not married.” Participants provided subjective ratings of general health status based on the question: “Would you say that in general your health is excellent, very good, good, fair, or poor?”, and these were dichotomized into “good or better” and “fair or worse”. Finally, participants were asked how many children less than 18 years of age live in their household. Their responses were dichotomized into children at home (number of children living at home > 0) or no children at home.
Statistical Analyses
To account for the complex multistage, stratified sampling design of the BRFSS, we conducted the analysis using SAS-callable SUDAAN version 10.0.1 (RTI International, Research Triangle Park, NC, USA). We calculated weighted prevalence estimates and corresponding 95 % confidence intervals (CIs) for not having had a routine checkup in the year before the survey by socio-economic status and demographic characteristics among reproductive age women. We also calculated weighted prevalence estimates for all levels of the three independent variables by socio-economic status and demographic characteristics. However, only data from those with the lowest level of social-emotional support, the lowest level of life satisfaction, and those with frequent mental distress are presented in the third table for clarity. Significant differences in the distribution of these factors were determined by χ2 test with a p value <0.05. Three separate models were developed using multivariable logistic regression analysis to assess relationships for each of the three measures (social-emotional support, life satisfaction, and mental distress) with not having a routine checkup within the past year. After including all covariates in an initial model, a manual backward selection procedure was used to produce the final models. A change of 10 % in the log likelihood ratio between models was used as the criterion. The final model for each of the three main independent variables (social-emotional support, life satisfaction, or mental distress) included four covariates: age, race/ethnicity, income, and health care coverage.
Results
Among US women 18–44 years old, the majority were in good or better health, had health care coverage, and had at least one child under 18 years old living at home. More than one-third of the women were of racial/ethnic groups other than white, were college graduates, and had annual household incomes over $50,000 (Table 2).
Table 2.
Selected demographic characteristics among women of reproductive age, BRFSSa, 2009
| Characteristic | nb | %c | 95 % CId |
|---|---|---|---|
| Age (years) | |||
| 18–24 | 6985 | 22.2 | 21.5–23.0 |
| 25–29 | 9509 | 16.1 | 15.6–16.6 |
| 30–34 | 13930 | 22.3 | 21.7–22.9 |
| 35–39 | 17211 | 18.1 | 17.7–18.6 |
| 40–44 | 19319 | 21.2 | 20.7–21.7 |
| Race/ethnicity | |||
| White | 45517 | 61.2 | 60.5–61.9 |
| Black | 7494 | 11.6 | 11.2–12.1 |
| Hispanic any race | 8471 | 19.4 | 18.8–20.0 |
| Asian | 1796 | 3.7 | 3.4–4.0 |
| Native American | 1244 | 0.9 | 0.8–1.1 |
| Other | 2423 | 3.1 | 2.9–3.4 |
| Education level | |||
| <High school (HS)/graduate equivalent degree (GED) | 5341 | 10.4 | 9.9–10.9 |
| HS graduate/GED | 15707 | 23.9 | 23.3–24.6 |
| Some college | 19584 | 29.2 | 28.6–29.9 |
| College graduate | 26135 | 36.5 | 35.8–37.1 |
| Annual household income | |||
| <$10,000 | 3673 | 6.0 | 5.6–6.3 |
| $10,000–$19,999 | 7227 | 11.4 | 10.9–11.9 |
| $20,000–$34,999 | 11429 | 16.5 | 16.0–17.1 |
| $35,000–$49,999 | 8833 | 12.5 | 12.0–13.0 |
| ≥$50,000 | 29129 | 41.5 | 40.8–42.1 |
| Refused or not known | 6607 | 12.2 | 11.7–12.7 |
| Health care coverage | |||
| Yes | 55526 | 80.6 | 80.0–81.2 |
| No | 11274 | 19.4 | 18.8–20.0 |
| Employment status | |||
| Employed | 43456 | 59.5 | 58.8–60.2 |
| Not employed | 23219 | 40.5 | 39.8–41.2 |
| Marital status | |||
| Married | 39747 | 56.3 | 55.5–57.0 |
| Not married | 27011 | 43.7 | 43.0–44.5 |
| Children<18 years of age living at home | |||
| Yes | 50817 | 73.0 | 72.4–73.7 |
| No | 15922 | 27.0 | 26.3–27.6 |
| Self-reported general health status | |||
| Good or better | 59399 | 88.8 | 88.3–89.2 |
| Fair or worse | 7320 | 11.2 | 10.8–11.7 |
Behavioral Risk Factor Surveillance System
Unweighted number of survey respondents
Weighted percentages
Confidence interval around the weighted prevalence estimate
Approximately one-third of the women in this sample reported they had not had a routine checkup in the past year (Table 3). Women aged 18–34 were less likely to have had an annual checkup compared to women aged 35–39 and 40–44. The prevalence of not having had a routine checkup in the past year was significantly lower among women who were Black compared to all other race groups, college graduates compared to those of lower education, those with health care coverage compared to those without, and among those with an annual household income of $50,000 or more compared to all other levels of income. In addition, the prevalence of not having had a routine checkup in the past year was significantly higher among women who were not employed, not married, and reported a fair or worse general health status, compared to those that were employed, married, and reported good or better health status, respectively.
Table 3.
Prevalence estimates of no routine checkup in past year, social-emotional support of Sometimes or less, life satisfaction of dissatisfaction, and frequent mental distress, among US women aged 18–44 years, BRFSSa, 2009
| Demographic characteristics | No routine checkup in past year |
Social-emotional support: sometimes or less |
Life satisfaction: dissatisfied |
Frequent mental distress |
||||
|---|---|---|---|---|---|---|---|---|
| %b | 95 % CIc | % | 95 % CI | % | 95 % CI | % | 95 % CI | |
| Total | 33.7 | 33.0–34.4 | 19.7 | 19.1–20.3 | 5.6 | 5.3–6.0 | 13.1 | 12.7–13.6 |
| Age (years) | p<0.0001* | p = 0.02 | p<0.0001 | p = 0.30 | ||||
| 18–24 | 34.6 | 32.8–36.6 | 19.5 | 17.9–21.3 | 5.6 | 4.7–6.8 | 13.3 | 12.1–14.7 |
| 25–29 | 38.0 | 36.3–39.7 | 20.0 | 18.6–21.5 | 5.7 | 4.9–6.7 | 14.2 | 13.0–15.4 |
| 30–34 | 35.3 | 33.9–36.6 | 18.9 | 17.7–20.1 | 5.5 | 4.8–6.2 | 12.6 | 11.7–13.5 |
| 35–39 | 31.3 | 30.1–32.6 | 19.5 | 18.4–20.7 | 5.3 | 4.7–5.9 | 12.9 | 12.0–13.8 |
| 40–44 | 29.9 | 28.8–31.0 | 20.6 | 19.6–21.7 | 6.1 | 5.6–6.7 | 12.8 | 12.1–13.7 |
| Race/ethnicity | p<0.0001 | p<0.0001 | p<0.0001 | p<0.0001 | ||||
| White | 35.0 | 34.2–35.8 | 14.7 | 14.1–15.3 | 5.0 | 4.6–5.4 | 12.7 | 12.1–13.2 |
| Black | 21.1 | 19.3–22.9 | 30.4 | 28.3–32.5 | 8.9 | 7.8–10.1 | 15.4 | 13.9–16.9 |
| Hispanic any race | 36.5 | 34.7–38.3 | 28.1 | 26.2–30.0 | 5.3 | 4.4–6.3 | 13.5 | 12.2–14.9 |
| Asian | 33.2 | 29.2–37.4 | 22.8 | 19.0–27.1 | 4.3 | 2.5–7.4 | 5.3 | 3.7–7.6 |
| Native American | 35.1 | 29.7–40.9 | 27.0 | 22.0–32.6 | 9.4 | 6.6–13.2 | 19.3 | 15.4–24.0 |
| Other | 38.2 | 34.2–42.4 | 25.4 | 22.1–29.1 | 10.2 | 7.6–13.6 | 18.7 | 15.6–22.3 |
| Education level | p<0.0001 | p<0.0001 | p<0.0001 | p<0.0001 | ||||
| <High school (HS)/graduate equivalent degree (GED) |
39.0 | 36.6–41.4 | 39.9 | 37.3–42.6 | 9.5 | 8.1–11.1 | 19.5 | 17.6–21.4 |
| HS graduate/GED | 37.0 | 35.5–38.5 | 25.2 | 23.9–26.6 | 7.9 | 7.0–8.9 | 16.6 | 15.6–17.8 |
| Some college | 33.6 | 32.4–34.8 | 18.5 | 17.4–19.6 | 5.9 | 5.4–6.6 | 14.6 | 13.7–15.6 |
| College graduate | 30.1 | 29.1–31.1 | 11.7 | 11.0–12.4 | 3.0 | 2.6–3.4 | 7.7 | 7.2–8.3 |
| Annual household income | p<0.0001 | p<0.0001 | p<0.0001 | p<0.0001 | ||||
| < $10,000 | 34.7 | 31.9–37.6 | 40.1 | 36.9–43.3 | 13.5 | 11.5–15.8 | 24.5 | 22.1–27.1 |
| $10,000-$19,999 | 41.1 | 38.9–43.3 | 35.4 | 33.2–37.7 | 11.9 | 10.5–13.5 | 23.4 | 21.6–25.3 |
| $20,000-$34,999 | 39.4 | 37.7–41.2 | 26.3 | 24.7–27.9 | 7.9 | 7.0–9.0 | 16.6 | 15.3–18.0 |
| $35,000-$49,999 | 34.2 | 32.3–36.2 | 17.2 | 15.6–18.8 | 4.8 | 3.8–6.1 | 12.6 | 11.3–14.1 |
| ≥ $50,000 | 28.5 | 27.6–29.4 | 10.4 | 9.7–11.0 | 2.1 | 1.9–2.5 | 7.5 | 7.0–8.0 |
| Refused or not known | 35.5 | 33.4–37.7 | 22.3 | 20.3–24.4 | 6.3 | 5.3–7.5 | 12.9 | 11.6–14.4 |
| Health care coverage | p<0.0001 | p<0.0001 | p<0.0001 | p<0.0001 | ||||
| Yes | 28.2 | 27.5–28.8 | 16.9 | 16.3–17.5 | 4.7 | 4.4–5.1 | 11.7 | 11.2–12.2 |
| No | 56.6 | 54.8–58.3 | 31.8 | 30.0–33.6 | 9.7 | 8.6–10.9 | 19.2 | 17.9–20.7 |
| Employment status | p<0.0001 | p<0.0001 | p<0.0001 | p<0.0001 | ||||
| Employed | 31.6 | 30.8–32.4 | 16.6 | 15.9–17.3 | 4.0 | 3.6–4.3 | 10.6 | 10.1–11.2 |
| Not employed | 36.8 | 35.6–38.0 | 24.1 | 23.1–25.2 | 8.1 | 7.4–8.8 | 16.7 | 15.9–17.6 |
| Marital status | p<0.01 | p<0.0001 | p<0.0001 | p<0.0001 | ||||
| Married | 32.8 | 32.0–33.6 | 14.9 | 14.2–15.5 | 3.2 | 2.9–3.6 | 10.2 | 9.7–10.8 |
| Not married | 34.9 | 33.8–36.1 | 26.0 | 24.9–27.1 | 8.8 | 8.1–9.5 | 16.9 | 16.0–17.7 |
| Children<18 years of age living at home | p = 0.94 | p<0.0001 | p<0.0001 | p = 0.09 | ||||
| Yes | 33.7 | 32.9–34.5 | 20.5 | 19.8–21.2 | 5.2 | 4.8–5.6 | 12.9 | 12.3–13.4 |
| No | 33.7 | 32.4–35.2 | 17.6 | 16.5–18.8 | 6.9 | 6.1–7.7 | 13.8 | 12.9–14.9 |
| Self–reported general health status | p<0.0001 | p<0.0001 | p<0.0001 | p<0.0001 | ||||
| Good or better | 33.2 | 32.4–33.9 | 16.8 | 16.2–17.4 | 4.1 | 3.8–4.5 | 10.2 | 9.8–10.7 |
| Fair or worse | 38.0 | 36.0–40.1 | 42.4 | 40.2–44.7 | 18.0 | 16.4–19.8 | 36.1 | 34.1–38.2 |
Behavioral Risk Factor Surveillance System
Weighted prevalence estimates
Confidence interval around the weighted prevalence estimate
p values were assessed based on tests of chi square distribution
Overall, nearly 20 percent of women reported receiving the lowest level (i.e., sometimes or less) of social-emotional support, while 5.6 % reported being dissatisfied with their lives, and 13.1 % reported experiencing frequent mental distress (Table 3). There were also several differences in prevalence for each of these three measures (e.g., social-emotional support, life satisfaction, and frequent mental distress) according to levels of other examined characteristics. Women with an education of high school or lower, the lowest incomes, without health care coverage, not employed, not married, and who reported a fair or worse general health status had the highest prevalence of all three measures, compared to their respective counterparts.
For the social-emotional support measure, there were distinct differences among groups in the prevalence of not having a routine check up in the past year. Among those who reported that they received the social-emotional support they needed sometimes or less frequently, 40.9 % did not have a routine checkup in the past year (Table 4). Among those who reported they received the social-emotional support they needed most of the time, 35.4 % did not have a routine checkup in the past year. Among those who reported that they always received the social-emotional support they needed, 29.9 % did not have a routine checkup in the past year. The significant differences in the crude measures persisted in the final model adjusting for age, race, education, and health care coverage with women who reported receiving social-emotional support most of the time (AOR = 1.29, 95 % CI 1.20–1.38) and women who sometimes or never received social-emotional support (AOR 1.47, 95 % CI 1.34–1.61) more likely to have not had a routine checkup compared to women who always received the social-emotional support they needed.
Table 4.
Estimated prevalence and odds ratios for reporting no routine checkup in the past year according to self-reported levels of social-emotional support, life satisfaction, and mental distress among women of reproductive age, BRFSS, 2009
| Independent variables | No routine checkup in the past year |
|||||
|---|---|---|---|---|---|---|
| Overall prevalence |
Crude models |
Adjusted modelsd |
||||
| %a | 95 % CIb | ORc | 95 % CI | OR | 95 % CI | |
| Social-emotional support† | ||||||
| Sometimes or less | 40.9 | 39.2–42.6 | 1.62† | 1.49–1.77 | 1.47† | 1.34–1.61 |
| Most of the time | 35.4 | 34.3–36.7 | 1.29† | 1.20–1.38 | 1.29† | 1.20–1.38 |
| Always | 29.9 | 28.9–30.9 | 1.00 | Reference | 1.00 | Reference |
| Life satisfaction† | ||||||
| Dissatisfied | 44.7 | 41.4–48.0 | 1.95† | 1.69–2.24 | 1.65† | 1.43–1.91 |
| Satisfied | 36.5 | 35.5–37.5 | 1.39† | 1.30–1.48 | 1.27† | 1.19–1.36 |
| Very satisfied | 29.3 | 28.4–30.3 | 1.00 | Reference | 1.00 | Reference |
| Frequent mental distress† | ||||||
| Yes | 39.7 | 37.8–41.6 | 1.35† | 1.24–1.47 | 1.19‡ | 1.09–1.30 |
| No | 32.8 | 32.1–33.5 | 1.00 | Reference | 1.00 | Reference |
Weighted prevalence estimates
Confidence interval around the weighted prevalence estimate
Odds ratio
Adjusted for age, race, income, and health care coverage
p<0.0001;
p<0.001
There were differences in the life satisfaction measure among those not having a routine check up in the past year. Among those who reported being dissatisfied with life, 44.7 % did not have a routine checkup in the past year (Table 4). Among those who reported being satisfied with life, 36.5 % did not have a routine checkup in the past year. Among those who reported being very satisfied with life, 29.3 % did not have a routine checkup in the past year. The significant differences in the crude measures persisted in the final model adjusting for age, race, education, and health care coverage, with women who reported being satisfied (AOR = 1.27, 95 % CI 1.19–1.36) and those that were dissatisfied (AOR = 1.65, 95 % CI 1.43–1.91) more likely to have not had a routine checkup compared to women who reported they were very satisfied with their lives.
Among those who reported frequent mental distress, 39.7 % had no routine checkup in the past year compared to 32.8 % for those who did not report frequent mental distress (Table 4). The significant differences in the crude measures persisted in the final model adjusting for age, race, education, and health care coverage, with women with frequent mental distress (AOR = 1.19, 95 % CI 1.09–1.30) more likely to have not had a routine checkup compared to women who experienced less frequent mental distress.
Discussion
Over one-third (approximately 18.8 million) of US women aged 18–44 years had not been to the doctor for a routine checkup within the past year in 2009. This study found that women who experience lower levels of social-emotional support, low levels of life satisfaction, and frequent mental distress were more likely to have not had a routine checkup even after adjusting for factors related to socio-economics and health care coverage.
The routine checkup is considered the ideal occasion for screening for health behaviors [29, 32, 33, 36]. Previous research has shown that a recommendation by a physician has an impact on the use of screening services, suggesting that those who have not developed a trusting relationship with a physician may be even less likely to undergo screenings, or initiate and maintain behavioral change [44–46]. Women with low levels of social-emotional support, low levels of life satisfaction, and frequent mental distress maybe most in need yet are less likely to have a routine checkup where they could be screened for and treated for appropriate physical or mental health conditions. It may be helpful for other patient-provider interactions, such as family planning and prenatal care visits, to also include screening for social-emotional and mental health to provide more comprehensive care to women of reproductive age. Screening results indicating a lack of social-emotional support or poor mental health could then be used to refer patients to community resources to address these issues when available.
Other factors that may influence health care utilization among reproductive-aged women include age, race, education, type of health care coverage, and accessibility of providers [28, 29, 32]. Our study identified similar results among the available variables, with women who had lower education, lower incomes, and those without health care coverage being less likely to have had a routine checkup. Many of these same factors also are increasingly being referred to as Social Determinants of Health, are complex in nature, and may result from long-term health inequalities [47]. A recent study of women by Mosca et al. [48] showed that awareness that cardiovascular disease was the leading cause of death in women nearly doubled from 1997 to 2005 and was associated with positive action to reduce risks (added more physical activity, avoided more unhealthy foods, quit smoking, and lost weight). The most frequently cited barriers were not related to health care access, but were to confusion in the media (49 %), the belief that health is determined by a higher power (44 %), caretaker responsibilities (42 %), and didn’t perceive themselves to be at risk (36 %). Thus, it is important to develop programs that can address multiple factors such as these, other Social Determinants of Health, and some of the more typical barriers to care (i.e., health coverage, availability of providers, costs, and adequacy of health coverage) in order to promote effective utilization of routine health care services.
Strengths of this study include a large sample size of women of reproductive age to assess these three measures of social-emotional and mental health. Another strength is that the estimates are generalizable to the US population of women aged 18–44 years in all states. However, this study is subject to some limitations. First, BRFSS data is based on self-report and subject to recall bias. For example, previous research has demonstrated that self-reports of health services utilization tend to overestimate the actual extent of screening and doctor visits [49, 50]. Additionally, some individuals may have reported receipt of a routine checkup for what was in fact an illness-related visit [30]. However, there is no reason to believe that over-reporting of routine checkups affected any group more than another in this study. Thirdly, BRFSS is limited to community-dwelling adults with a landline telephone and does not include institutionalized adults nor those without access to a landline telephone. Therefore, the social-emotional and mental health measures presented in this study thus may be underestimates and not representative of populations not surveyed. A fourth limitation could result if women who were pregnant within the past year accessed health care services for prenatal care when many preventive primary care services are provided and may or may not have considered it to be a routine checkup as listed in the BRFSS question. Unfortunately, this level of detail about pregnancy in the past year is not available in the data and a differential response to this question based on pregnancy history is not anticipated. There is a question about being currently pregnant in the survey and it was decided to those that were pregnant in the analysis in order to be representative of the age group. Lastly, the cross-sectional nature of BRFSS only captures information on the measures in this study at a single point in time and does not allow examination of temporality. Therefore, the study cannot determine causality; but does identify potential areas for additional investigation into the relationships among social emotional support, life satisfaction, and mental distress with having a routine checkup.
These limitations notwithstanding, the results of this study provide useful information on the prevalence of low levels of social-emotional support, low levels of life satisfaction, frequent mental distress, and their associations with the utilization of preventive health services by women of reproductive age after controlling for potential confounding factors. These measures are important health constructs that help identify women less likely to utilize health services. This information can be used in conjunction with established risk factors to develop focused strategies that provide appropriate support so these women access clinical services in order to increase exposure to preventative health opportunities and improve overall health.
Acknowledgments
The authors of this study sincerely thank Drs. Kristin Rankin and Deborah Rosenberg for their assistance in the analysis and preparation of this manuscript as part of the 2009–2011 Survey Analysis Course administered by the University of Illinois-Chicago and the Division of Reproductive Health at the Centers for Disease Control & Prevention. We acknowledge the support and assistance of Drs. David Goodman and Charlan Kroelinger in the Division of Reproductive Health at the Centers for Disease Control and Prevention, who assisted in oversight and general review of the analysis. This study was supported in part by an appointment of Ms. Zaha to the Applied Epidemiology Fellowship Program administered by the Council of State and Territorial Epidemiologists (CSTE) and funded by the Centers for Disease Control and Prevention (CDC) Cooperative Agreement U60/CCU007277; and the Altrum Institute who administered the Graduate Student Internship Program funded by the Maternal and Child Health Information Resource Center in the Health Resources and Services Administration and provided a stipend for Ms. Willet.
Footnotes
CDC Disclaimer: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Contributor Information
Michelle N. Willet, Family Health Services Division, Hawaii State Department of Health, 3652 Kilauea Avenue, Honolulu, HI 96816, USA
Donald K. Hayes, Family Health Services Division, Hawaii State Department of Health, 3652 Kilauea Avenue, Honolulu, HI 96816, USA, don.hayes@doh.hawaii.gov
Rebecca L. Zaha, Family Health Services Division, Hawaii State Department of Health, 3652 Kilauea Avenue, Honolulu, HI 96816, USA
Loretta J. Fuddy, Hawaii State Department of Health, Honolulu, HI, USA
References
- 1.Preamble to the Constitution of the World Health Organization as adopted by the international health conference . Official Records of the World Health Organization. Vol. 2. New York: 1946. p. 100. [Google Scholar]
- 2.Spahn JM, Reeves RS, Keim KS, Laquatra I, Kellogg M, Jortberg B, et al. State of the evidence regarding behavior change theories and strategies in nutrition counseling to facilitate health and food behavior change. Journal of the American Dietetic Association. 2010;110(6):879–891. doi: 10.1016/j.jada.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 3.Kasparian NA, McLoone JK, Butow PN. Psychological responses and coping strategies among patients with malignant melanoma. Archives of Dermatology. 2009;145(12):1415–1427. doi: 10.1001/archdermatol.2009.308. [DOI] [PubMed] [Google Scholar]
- 4.Richmond CAM, Ross NA, Egeland GM. Social support and thriving health: A new approach to understanding the health of indigenous Canadians. American Journal of Public Health. 2007;97(10):1827–1833. doi: 10.2105/AJPH.2006.096917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 6.Ozbay F, Fitterling H, Charnery D, Southwick S. Social support and resilience to stress across the life span: A neurobiologic framework. Current Psychiatry Reports. 2008;10(4):304–310. doi: 10.1007/s11920-008-0049-7. [DOI] [PubMed] [Google Scholar]
- 7.Jeste DV, Depp CA, Vahia IV. Successful cognitive and emotional aging. World Psychiatry. 2010;9(2):78–84. doi: 10.1002/j.2051-5545.2010.tb00277.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aggarwal B, Liao M, Allegrante JP, Mosca L. Low social support level is associated with non-adherence to diet at 1 year in the family intervention trial for heart health (FIT Heart) Journal of Nutrition Education. 2010;42(6):380–388. doi: 10.1016/j.jneb.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duncan TE, McAuley E. Social support and efficacy cognitions in exercise adherence: A latent growth curve analysis. Journal of Behavioral Medicine. 1993;16(2):199–218. doi: 10.1007/BF00844893. [DOI] [PubMed] [Google Scholar]
- 10.Eyler AA, Brownson RC, Donatelle RJ, King AC, Brown D, Sallis JF. Physical activity, social support and middleand older-aged minority women: Results from a US survey. Social Science and Medicine. 1999;49(6):781–789. doi: 10.1016/s0277-9536(99)00137-9. [DOI] [PubMed] [Google Scholar]
- 11.McNeill LH, Wyrwich KW, Brownson RC, Clark EM, Kreuter MW. Individual, social environmental, and physical environmental influences on physical activity among black and white adults: A structural equation analysis. Annals of Behavioral Medicine. 2006;31(1):36–44. doi: 10.1207/s15324796abm3101_7. [DOI] [PubMed] [Google Scholar]
- 12.DiMatteo MR. Social support and patient adherence to medical treatment: A meta-analysis. Health Psychology. 2004;23(2):207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- 13.Honda K, Kagawa-Singer M. Cognitive mediators linking social support networks to colorectal cancer screening adherence. Journal of Behavioral Medicine. 2006;29(5):449–460. doi: 10.1007/s10865-006-9068-1. [DOI] [PubMed] [Google Scholar]
- 14.Saris WE, Scherpenzeel AC, Veenhoven R, Bungting B. A comparative study of satisfaction with life In Europe. Eotvos University Press; Budapest: 1996. [Google Scholar]
- 15.Moons P, Budts W, De Geest S. Critique on the conceptualisation of quality of life: A review and evaluation of different conceptual approaches. International Journal of Nursing Studies. 2006;43(7):891–901. doi: 10.1016/j.ijnurstu.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 16.Cummins RA. Living with support in the community: Predictors of satisfaction with life. Mental Retardation and Developmental Disabilities Research Reviews. 2001;7(2):99–104. doi: 10.1002/mrdd.1014. [DOI] [PubMed] [Google Scholar]
- 17.US Department of Health and Human Services . Healthy People 2020. Washington, DC: Office of Disease Prevention and Health Promotion. Available at http://www.healthypeople.gov/2020. Accessed 18 Dec 2011. [Google Scholar]
- 18.Kouvumaa-Honkanen H, Honkanen R, Viinamaki H, Heikkila K, Kaprio J, Koskenvuo M. Self-reported life satisfaction and 20-year mortality in healthy Finnish adults. American Journal of Epidemiology. 2000;152(10):983–991. doi: 10.1093/aje/152.10.983. [DOI] [PubMed] [Google Scholar]
- 19.Strine TW, Chapman DP, Balluz LS, Moriarty DG, Mokdad AH. The associations between life satisfaction and health-related quality of life, chronic illness, and health behaviors among US community-dwelling adults. Journal of Community Health. 2008;33(1):40–50. doi: 10.1007/s10900-007-9066-4. [DOI] [PubMed] [Google Scholar]
- 20.Strine TW, Balluz L, Chapman DP, Moriarty DG, Owens M, Mokdad AH. Risk behaviors and healthcare coverage among adults by frequent mental distress status. American Journal of Preventive Medicine. 2004;26(3):213–216. doi: 10.1016/j.amepre.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 21.Strine TW, Chapman DP, Kobau R. Associations of self-reported anxiety symptoms with health-related quality of life and health behaviors. Social Psychiatry and Psychiatric Epidemiology. 2005;40(6):432–438. doi: 10.1007/s00127-005-0914-1. [DOI] [PubMed] [Google Scholar]
- 22.Strine TW, Okoro CA, Chapman DP. Health-related quality of life and health risk behaviors among smokers. American Journal of Preventive Medicine. 2005;28(2):182–187. doi: 10.1016/j.amepre.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 23.Dominick KL, Ahern FM, Gold CH, Heller DA. Relationship of health-related quality of life to health care utilization and mortality among older adults. Aging Clinical and Experimental Research. 2002;14(6):499–508. doi: 10.1007/BF03327351. [DOI] [PubMed] [Google Scholar]
- 24.Alexopolous GS, Katz IR, Reynolds CFIII, Carpenter D, Docherty JP, Ross RW. Pharmacotherapy of depression in older patients: A summary of the expert consensus guidelines. Journal of Psychiatric Practice. 2001;7(6):361–376. doi: 10.1097/00131746-200111000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Moore MJ, Moir P, Patrick MM. The state of aging and health in America 2004. Centers for Disease Control and Prevention and Merck Institute of Aging and Health; Washington, DC: 2004. Merck Institute of Aging and Health, and Centers for Disease Control and Prevention. [Google Scholar]
- 26.Ahuwalia IB, Mack KA, Mokdad A. Mental and physical distress and high-risk behaviors among reproductive-age women. Obstetrics and Gynecology. 2004;104(3):477–483. doi: 10.1097/01.AOG.0000137920.58741.26. [DOI] [PubMed] [Google Scholar]
- 27.Kobau R, Safran MA, Zack MM, Moriarty DG, Chapman D. Sad, blue, or depressed days, health behaviors and health-related quality of life, Behavioral Risk Factor Surveillance System, 1995–2000. 2004. Health and Quality of Life Outcomes. 2004;2(40):1–8. doi: 10.1186/1477-7525-2-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Culica D, Rohrer J, Ward M, Hilsenrath P, Pomrehn P. Medical checkups: Who does not get them? American Journal of Public Health. 2002;92(1):88–91. doi: 10.2105/ajph.92.1.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wolff LS, Massett HA, Weber D, Mockenhaupt RE, Hassmiller S, Maibach EW. Opportunities and barriers to disease prevention counseling in the primary care setting: a multisite qualitative study with US health consumers. Health Promotion International. 2010;25(3):265–276. doi: 10.1093/heapro/daq030. [DOI] [PubMed] [Google Scholar]
- 30.Hagdrup NA, Simoes EJ, Brownson RC. Health care coverage: traditional and preventive measures and associations with chronic disease risk factors. Journal of Community Health. 1997;22(5):387–399. doi: 10.1023/a:1025131721791. [DOI] [PubMed] [Google Scholar]
- 31.McGuire LC, Strine TW, Okoro CA, Ahluwalia IB, Ford ES. Modifiable characteristics of a healthy lifestyle in US older adults with or without frequent mental distress: 2003 Behavioral Risk Factor Surveillance System. The American Journal of Geriatric Psychiatry. 2003;15(9):754–761. doi: 10.1097/JGP.0b013e3180986125. [DOI] [PubMed] [Google Scholar]
- 32.Lai DW, Kalyniak S. Use of annual physical examinations by aging Chinese Canadians. Journal of Aging and Health. 2005;17(5):573–591. doi: 10.1177/0898264305279778. [DOI] [PubMed] [Google Scholar]
- 33.Coups EJ, Gaba A, Orleans CT. Physician screening for multiple behavioral health risk factors. American Journal of Preventive Medicine. 2004;27(Suppl 2):34–41. doi: 10.1016/j.amepre.2004.04.021. [DOI] [PubMed] [Google Scholar]
- 34.Slivinske LR, Fitch VL, Mosca J. Predicting health and social service utilization of older adults. Journal of Social Service Research. 1995;20(1–2):21–40. [Google Scholar]
- 35.Kouzis AC, Eaton WW. Absence of social networks, social support and health services utilization. Psychological Medicine. 1998;28(6):1301–1310. doi: 10.1017/s0033291798007454. [DOI] [PubMed] [Google Scholar]
- 36.Nausheen B, Gidron Y, Peveler R, Moss-Moris R. Social support and cancer progression: A systematic review. Journal of Psychosomatic Research. 2009;67(5):403–415. doi: 10.1016/j.jpsychores.2008.12.012. [DOI] [PubMed] [Google Scholar]
- 37.Strine TW, Chapman DP, Balluz L, Mokdad AH. Health-related quality of life and health behaviors by social and emotional support. Social Psychiatry and Psychiatric Epidemiology. 2008;43(2):151–159. doi: 10.1007/s00127-007-0277-x. [DOI] [PubMed] [Google Scholar]
- 38.Clemente F, Sauer WJ. Life satisfaction in the United States. Social Forces. 1976;54(3):621–631. [Google Scholar]
- 39.Edwards JN, Klemmack DL. Correlates of life satisfaction: A re-examination. Journal of Gerontology. 1973;28(4):497–502. [PubMed] [Google Scholar]
- 40.Palmore E, Luikart C. Health and social factors related to life satisfaction. Journal of Health and Social Behavior. 1972;13(1):68–80. [PubMed] [Google Scholar]
- 41.Conway T, Hu TC, Mason E, Mueller C. Are primary care residents adequately prepared to care for women of reproductive age? Family Planning Perspectives. 1995;27(2):66–70. [PubMed] [Google Scholar]
- 42.Denton M, Prus S, Walters V. Gender differences in health: A Canadian study of the psychosocial, structural, and behavioural determinants of health. Social Science and Medicine. 2004;58(12):2585–2600. doi: 10.1016/j.socscimed.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 43.Nelson DE, Holtzman D, Bolen J, Stanwyck CA, Mack KA. Reliability and validity of measures from the Behavioral Risk Factor Surveillance System (BRFSS) Social and Preventive Medicine. 2001;46(Suppl 1):S03–S42. [PubMed] [Google Scholar]
- 44.Kemp BJ, Krause JS. Depression and life satisfaction among people ageing with post-polio and spinal cord injury. Disability and Rehabilitation. 1999;21(5–6):241–249. doi: 10.1080/096382899297666. [DOI] [PubMed] [Google Scholar]
- 45.Holtzman D. The behavioral risk factor surveillance system. In: Blumenthal DS, DiClemente RJ, editors. Community-based health research: Issues and methods. Springer; New York: 2004. [Google Scholar]
- 46.Mroczek DK, Spiro A. Change in life satisfaction during adulthood: Findings from the veterans affairs normative aging study. Journal of Personality and Social Psychology. 2005;88(1):189–202. doi: 10.1037/0022-3514.88.1.189. [DOI] [PubMed] [Google Scholar]
- 47.Commission on Social Determinants of Health . Closing the gap in a generation: Health equity through action on the social determinants of health. World Health Organization; Geneva: 2008. Available online at: http://whqlibdoc.who.int/hq/2008/WHO_IER_CSDH_08.1_eng.pdf. [DOI] [PubMed] [Google Scholar]
- 48.Mosca L, Mochari H, Christian A, Berra K, Taubert K, Mills T, et al. National study of women’s awareness, preventive action, and barriers to cardiovascular health. Circulation. 2006;113:525–534. doi: 10.1161/CIRCULATIONAHA.105.588103. [DOI] [PubMed] [Google Scholar]
- 49.Sirovich BE, Schwartz LM, Woloshin S. Screening men for prostate and colorectal cancer in the United States: Does practice reflect the evidence? Journal of the American Medical Association. 2003;289(11):1414–1420. doi: 10.1001/jama.289.11.1414. [DOI] [PubMed] [Google Scholar]
- 50.Bellon JA, Lardelli P, Luna JD, Delgado A. Validity of self reported utilisation of primary health care services in an urban population in Spain. Journal of Epidemiology and Community Health. 2000;54(7):544–551. doi: 10.1136/jech.54.7.544. [DOI] [PMC free article] [PubMed] [Google Scholar]


