Abstract
Despite the growing prevalence of osteoporosis, many middle-age women do not engage in recommended bone health promotion behaviors. Based on the Integrated Theory of Health Behavior Change, an intervention was designed to increase the self-management behaviors of calcium and vitamin D intake by strengthening health beliefs and using self-regulation skills. In this repeated measures experimental study, a convenience sample of 148 healthy women between 40 and 60 were assigned to either the computer-based intervention group (CBIG) or usual care group (UCG). Measures of health beliefs and calcium and vitamin D intake were obtained at baseline, 8 and 14 weeks, and 6 months. An interaction effect was observed for self-efficacy and approached significance for goal congruence. The CBIG had higher level of calcium intake at 14 weeks than women in the UCG when analyzed using intention to treat. Self-efficacy predicted calcium intake.
Keywords: osteoporosis, health behavior, patient-centered care, calcium intake, electronic media, tailored
Osteoporosis is a serious and prevalent health condition affecting the strength and micro-architecture of bone. Left untreated osteoporosis has a 53.2% lifetime risk for fracture in White women resulting in acute and chronic pain and disfigurement, failure to return to normal functional status, and an increased mortality rate (Cole, Dennison, & Cooper, 2008). Once considered a disease of White and Asian women, the greatest increase in osteoporosis is now seen in Latinos and other minority populations (Cole et al., 2008; Holroyd, Cooper, & Dennison, 2008; Sanchez-Riera et al., 2010). In addition to genetics and hormonal status, bone health is related to nutrition, active lifestyle, appropriate and timely monitoring, and for some use of pharmacological agents (National Osteoporosis Foundation [NOF], 2008a; Osteoporosis Prevention, Diagnosis, and Treatment, 2000). Despite the growing prevalence of osteoporosis, many middle-age women do not engage in recommended health promotion behaviors (Recker, 2011; Schnatz, Marakovits, Dubois, & O’Sullivan, 2011). The disparity between the high prevalence of osteoporosis and the low number of persons engaging in preventative care highlights this condition as an example of the crucial role behavior change could play in improving health and decreasing health care costs.
Summary of the Literature and Theory of Health Behavior Change
Worldwide, health care professionals are using osteoporosis prevention programs to increase women’s engagement in health behaviors specifically recommended to prevent or delay the onset of osteoporosis. At the time the application for this study was developed (Ryan, 2006), 13 studies evaluating osteoporosis prevention programs were located. Designs ranged from randomized clinical trials (RCTs) to program evaluations. Calcium intake was measured in some but not all studies. By 2013, following completion of this study, a systematic review of osteoporosis prevention programs was published (Ryan, Schlidt, & Ryan, 2013). This review included 12 studies with RCT or quasi-experimental designs that described the impact of osteoporosis prevention programs on calcium intake. These reviews provide a basis for understanding what is known about osteoporosis prevention programs and the health behavior outcome of nutrition.
All of the osteoporosis prevention programs (Ryan et al., 2013) provided education. Select programs provided calcium supplements or skill training to enhance self-regulation capacities (e.g., self-monitoring, goal setting, or reflection). These studies included a variety of media (or delivery method intended to reach large audiences), including paper (ranging from brochures to manuals), telephone contact, small group sessions, individual sessions, and demonstration and short films. Small groups were the most commonly used media and often were complemented with other types of media. Standardized, individualized, and tailored approaches were used. The number of contacts ranged from single day (short and full day), to 6 to 12 weekly meetings, to peer monitoring on a daily basis over 18 months. Bone density (including dual-energy X ray absorptiometry and ultrasound) was used to determine eligibility, as part of the intervention, or as an outcome measure. Measurement of calcium intake varied and ranged from self-reported perception of changes in calcium intake to the use of comprehensive food diaries linked to software containing the nutritional value of foods. Successful interventions (significant difference between groups) were characterized by the use of multiple types of delivery media and skills training to enhance self-regulation, occurred over time, and were delivered by one or more health care professional from a variety of disciplines.
Samples contained women of all ages. Interventions were described with brevity and a theoretical framework was missing from many studies. More than half the studies were missing the critical data needed to compare results across studies. Computer-based interventions (CBIs), as a delivery media, were missing from this collection of studies. In an era of exploding technology and widespread use of computers for health care (Maierle & Ryan, 2011), there is a need for further research to determine the effect of using CBIs for osteoporosis prevention.
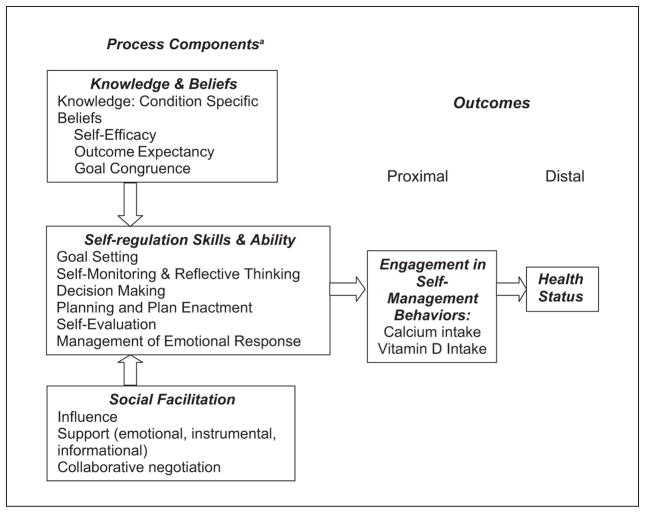
The Integrated Theory of Health Behavior Change (ITHBC; Figure 1; Ryan, 2009; later incorporated into the Individual and Family Self-Management Theory as the process and proximal outcome components; Ryan & Sawin, 2009) was foundational to this study. The ITHBC describes the processes used to change health behavior. The theory purports that initiation and maintenance of health behavior change can be facilitated by enhancing condition-specific health beliefs, self-regulation skills and abilities, and social facilitation. Change in the self-management of health behaviors leads to improvement in the distal or long terms outcomes related to health status. The ITHBC outlines the key components of health behavior change processes and provides the essential components for intervention development.
Figure 1.
Integrated Theory of Health Behavior Change.
Source: Ryan, 2009.
Note: ITHBC = integrated theory of health behavior change.
aIntervention developed to strengthen process components of knowledge and beliefs, self-regulation skills and ability, and social facilitation.
Purpose
The purpose of this study was to evaluate the impact of a theory-based, tailored, computerized intervention on women’s intake of calcium and vitamin D. At the time this study was prepared, there were no studies that had tested the effects of a CBI on osteoporosis prevention. It was hypothesized that women participating in the computer-based intervention group (CBIG) would reach and maintain higher levels of calcium and vitamin D intake over time when compared with women participating in the usual care group (UCG). Health beliefs from the process component of the ITHBC (self-efficacy, outcome expectancy, and goal congruence, osteoporosis beliefs) were evaluated as predictors of calcium and vitamin D intake.
Method
Design
In this repeated measures experimental study, data were collected at baseline, 8 and 14 weeks, and 6 months. Women were randomly assigned to receive CBI or UC (Usual Care). Data for this study were collected from 2006 to 2009.
Sample
A convenience sample was recruited from an urban community in the Midwest via newspaper advertisements, radio, television, work site electronic and printed newsletters, and flyers widely distributed to public places, including libraries, beauty shops, churches, health clubs, and grocery stores. Women were eligible to participate if they were healthy by self-report, including no previous diagnosis of osteoporosis or osteoporosis treatment, were between the ages of 40 and 60 years, lived or worked within 30 miles of the study center, spoke and wrote English, and had a dietary intake of 200 milligrams (mg) less calcium (approximately one serving of calcium rich food) than recommended (U.S. Department of Health & Human Services [USDHHS], 2004) as determined by the Quick Calcium Assessment (NOF, 2008b). Approval from multiple IRBs was required as members of the research team were affiliated with multiple academic institutions. Verbal and written consents were used for different aspects of the study. The goal was to recruit a sample of 128 participants that would result in a power of .80 to detect differences in calcium intake between groups (α = .5). At the time this study was conducted, the attrition rate for osteoporosis prevention programs involving this age women was not well documented, so additional 20 participants were enrolled.
Interventions
CBI
The CBI was a theory-based, patient-centered, dynamically tailored intervention delivered via computer. Major constructs from the ITHBC (Ryan, 2009; Ryan & Sawin, 2009) provided the logic for intervention development. The intervention was designed to enhance engagement in self-management behaviors by (a) enhancing knowledge and beliefs (information related to osteoporosis and beliefs of self-efficacy, outcome expectancy, and goal congruence), (b) developing self-regulation skills and abilities (goal setting, self-monitoring, reflection, plan enactment, and evaluation), and c) fostering social facilitation (influence). The intervention meet criteria for a patient-centered intervention, specifically “(a) the content of the intervention was selected to address salient characteristics of the patients’ experiences (e.g., beliefs) and (b) the intervention was responsive to patients’ goals and preferences” (Lauver et al., 2002, p. 247). The patient-centered approaches of targeting, tailoring, and individualization were incorporated through-out the CBI (Lauver et al., 2002; Ryan & Lauver, 2002). Content on health beliefs and nutrition was dynamically tailored. As participants strengthened their beliefs or increased their intake of calcium or vitamin D, participants received new messages designed to match their changing knowledge, beliefs, and experiences. The intervention was used over an 8-week period of time. A chart outlining the linkages between the theoretical concepts, brief overview of intervention content, the delivery media, and measures can be found on Table 1. Available in previous publications is additional information detailing the relationship between the theory and intervention development (Ryan, 2009; Ryan & Sawin, 2009), content-theory congruence and laboratory and performance usability testing (Ryan, Pumilia, Henak, & Chang, 2009), and a description of participants use of and satisfaction with the intervention (Maierle & Ryan, 2011).
Table 1.
Linkages Among Theory, Intervention Content, Delivery Media, and Empirical Measures.
| Theoretical | Content | Delivery mediaa | Empirical measures |
|---|---|---|---|
| Knowledge | Factual information related to bone health, osteoporosis, risk, and dietary intake of calcium and vitamin D | Website and handheld computer | Facts on Osteoporosis Quiz (Ailinge, Harper, & LaSusa, 2003) |
| Health beliefs | Condition-specific beliefs about osteoporosis, risk, and prevention | Website | Osteoporosis Health Beliefs (Kim, Horan, Gendler, & Patel, 1991) |
| Self-efficacy: confidence to increase calcium and vitamin D intake, usual and difficult times | Website and handheld computer | Osteoporosis Self-Efficacy Scale (Horan, Kim, Gendler, Froman, & Patel, 1998) | |
| Outcome expectancy: Expectation that increasing calcium intake will result in desired outcomes | Website | Outcome expectancy (Horan et al., 1998) | |
| Goal congruence: Congruence among multiple personal competing goals | Website | Goal congruence (Ryan, 2009) | |
| Self-regulation skills and abilitiesb | Skills and abilities: Goal bsetting, self-monitoring, feedback and reflective thinking decision making, planning, doing, self- evaluation | Handheld computer | Use: time, frequency, and section (Maierle & Ryan, 2011) |
| Self-management behaviors (proximal outcomes) | Increasing calcium and vitamin D intake | NA | 3-day food diary |
Note: NA = not applicable; CBIG = computer-based information group; T = time: T1 (baseline), (Intervention), T2 (8 weeks), T3 (14 weeks), T4 (6 months); mg = milligrams; IU = international unit.
Both the tailored website and the handheld computer used by all women in CBIG only.
CBIG only.
CBI Content
Content was based on national and international guidelines (NOF, 2008b; Osteoporosis Prevention, Diagnosis, and Treatment, 2000; USDHHS, 2004; U.S. Preventive Services Task Force, 2011; World Health Organization, 2007). CBI focused on increasing calcium and vitamin D but also contained general information about bone development and health, hormones, osteoporosis, and risk factors. Specific recommendations for calcium intake were provided (premenopausal 1,000 to 1,200 mg and 1,300 to 1,500 mg for women in menopausal transition or post-menopausal (USDHHS, 2004). Use and types of supplements were discussed and participants were taught how to read and interpret food labels. Lists of calcium rich foods were provided alphabetically, by food group, and by meal choices. Links to additional resources were available.
Stories and activities were used to enhance knowledge, self-efficacy, outcome expectancy, and goal congruence. Strategies to increase self-efficacy included encouragement, mentoring through stories, and engagement in moderately challenging goals for which the woman had a high likelihood of succeeding. Outcome expectancy was addressed by sharing factual information presented by persons or groups of perceived authority who attested to the benefits of changing specific health behaviors. Strategies to increase goal congruence focused on assisting women to become consciously aware of dissonant goals (e.g., weight management and use of high calorie dairy food to increase calcium intake) and to provide tips and reframing strategies to decrease dissonance between goals (e.g., us of lower calorie dairy foods and other food sources of calcium).
Learning and using self-regulation skills and abilities were central to CBI. Women were guided to set goals and develop behavior specific plans to achieve these goals. Self-monitoring tools were available and narrative content and graphs and charts provided real-time feedback. The iterative nature of health behavior change was stressed and tools were available for continued goal modification.
Information Preparation and Preliminary Testing
The CBI was developed and tested in multiple steps with theory and research integral to each step (Ryan et al., 2009). The intervention included the key components of a tailored intervention specifically: assessment, message library, decisional algorithm, feedback, and delivery media (Ryan & Lauver, 2002). The intervention was tailored on concepts from the theoretical framework. The assessment component of the CBI measured individuals’ calcium and vitamin D intake and their health beliefs. The results were used to match select content to each participant. For example, the Quick Calcium Intake (NOF, 2008b), a 5-item measure, was used to evaluate calcium intake. Based on this assessment, women were identified as having very low, low, or adequate intake of calcium. Women with different levels of calcium intake received different messages.
Tailored interventions contain a message library. Short messages were prepared and stored within the software. A message was developed for each potential response to the assessment questions. For example, women were identified as having an adequate calcium intake, a low intake (defined as needing 1–2 more servings of calcium rich foods), or a very low intake that required dietary changes and supplementation. Each woman received a message unique to her assessment results. Various permutations and combination of messages were developed to match all potential responses.
Tailored interventions contain a decisional algorithm, or the logic of matching assessment results with messages. The logic consisted of a series of “if then” statements. For example, “if” the participant’s calcium intake was very low, “then” she received a message designed just for women with a very low calcium intake. All messages were checked for conceptual coherence and seamless delivery prior to actual use of the intervention by participants.
Delivery Media
The intervention was provided via two related but different computer media: a website on a personal computer and a handheld computer. Factual information about osteoporosis and calcium intake was primarily on the website, whereas a program specifically designed to enhance self-regulation behaviors was on the handheld computer (a Dell Axim PDA; Dell, Round Rock, TX) running Windows Mobile (Microsoft, Redmond, WA). At the time the intervention was developed and usability testing was conducted, no single device could deliver large amounts of tailored information in a format acceptable to women and provide the portability needed to integrate self-regulation activities into women’s active lifestyles. Hence, all participants in the CBIG used both types of computer media (Table 1). Software was designed to be aesthetically appealing to women and contained pictures of middle-age women of different races and ethnicities and foods, charts and graphs, and activities.
The handheld computer contained six interactive sections, including “goals” (goal setting), “intake” (self-monitoring of calcium and vitamin D), “how am I doing” (normative and ipsative feedback provided via charts and graphs), “diary” (activities designed to facilitate self-reflection), “helpful facts” (calcium rich foods arranged alphabetically, by meal, and across restaurant chains, and pictures were provided to facilitate portion evaluation), and “tips” (including how to use the device and contact researchers).
Preparing and Supporting Participants to Use Computerized Intervention
The computerized intervention was given to participants for self-directed use. Each participant chose when and where they used CBI. They selected and sequenced content of interest, determined the amount of time they spent in each section, and how frequently they returned to the section. Women viewed the tailored informational content on the website thoroughly at least once and returned to the comprehensive content as needed—Essentially, once all the information had been read, women were encouraged to use sections that supported their current activities to achieve a goal. They were directed to use their pocket computer five times a week over 8 weeks.
UC Intervention
UC at the time the study was conducted consisted of care delivered by a primary care provider supplemented with printed educational material. To ensure comparability of knowledge across all participants all women in the UCG received a brochure about osteoporosis prevention and management (Arthritis Foundation, 1999). The printed information was based on current literature and guidelines, congruent with national standards, and contained information about osteoporosis, risk factors, standard prevention, diagnostic testing, and specific recommendations for management. Detailed description of calcium and vitamin D rich foods, directions on how to read labels, and supplements was included in the information. Women were encouraged to read the information on their own time, to track their calcium intake over time, and to refer back to the written information at any time during the study.
Key Differences Between Interventions
The informational content about the condition of osteoporosis, risk, diagnosis, and management is essentially the same between CBI and UC. The interventions differ in that persons in the UCG receive factual information. Persons in CBIG receive an intervention designed to provide them with standardized information plus increase their health beliefs, self-regulation abilities, and social facilitation. One group receives just information and the other group is guided through the process of health behavior change as identified by the theory.
Measures
The Quick Calcium Intake (NOF, 2008b), a 5-item scale that counts servings of milk, cheese, yogurt, and fortified orange juice and calcium supplementation, was used to determine the eligibility criteria related to calcium intake. Information on sociodemographic characteristics (age, socioeconomic status, risk of osteoporosis, race and ethnicity, education, living arrangement, and menopausal status) were collected at the baseline (Table 2). Socioeconomic status was measured using the 4-Factor Hollingshead Index. A score was determined by multiplying weighted values for education and occupation. Scores range from 8 to 55 with higher the score representing a higher the socioeconomic status (Hollingshead, 2011). Risk was assessed using a 17-item yes/no survey, which included questions about menopausal status, frame, family history, medications (including hormone replacement), consumption of dairy food and calcium supplements, falls, exercise, smoking, and alcohol consumption. The number of risk factors a woman reported was summed for a total score. A survey of health care that participants received during the course of the study was conducted at the end of the study (survey items are listed on Table 2). Data for all of the measures were collected at all four measurement periods with the exception of knowledge, which was collected pre- and post-intervention. In all scales, higher scores indicate greater presence of the characteristic measured.
Table 2.
Description of Participants at Baseline.
| UCG (n = 74)
|
CBIG (n = 74)
|
||
|---|---|---|---|
| N = 148 | Frequency (%) | Frequency (%) | Tests of difference |
| Race | |||
| White | 69 (93.2) | 60 (81.1) | χ2(1) = 4.89, p = .02 |
| Other | 5 (6.8) | 14 (18.9) | |
| Education | |||
| High school grad. | 8 (10.8) | 5 (6.8) | χ2(3) = 0.95, p = .81 |
| Partial college | 19 (25.7) | 21 (28.4) | |
| College grad. | 34 (45.9) | 33 (44.6) | |
| Graduate degree | 13 (17.6) | 15 (20.3) | |
| Living arrangements | |||
| Partnered | 55 (74.3) | 50 (67.6) | χ2(1) = 0.82, p = .37 |
| Nonpartnered | 19 (25.7) | 24 (32.4) | |
| Menopausal status | |||
| Pre-menopausal | |||
| Regular cycle | 20 (27) | 21 (28.4) | χ2(1) = 0.46 p = .49 |
| Irregular cycle | 7 (9.5) | 3 (4.1) | |
| Skipping cycles (<12/year) | 10 (13.5) | 15 (20.3) | |
| Post-menopausal | |||
| Cycles stopped naturally | 24 (32.4) | 16 (21.6) | |
| Cycles stopped due to surgery/medical treatment | 13 (17.6) | 19 (25.7) | |
| Care received during study | |||
| Bone density | |||
| Ever | 14 (43) | 23 (56) | χ2(1) = 1.09, p = .29 |
| Past 9 months | 6 (19) | 6 (15) | χ2(1) = 0.577, p = .44 |
| Advised by provider to … | |||
| Increase calcium intake | 9 (28) | 12 (29) | χ2(1) = 0.011, p = .91 |
| Take calcium supplements | 9 (28) | 15 (37) | χ2(1) = 0.583, p = .44 |
| Take vitamin D supplements | 11 (34) 11 (34) |
13 (31) 16 (39) |
χ2(1) = 0.058, p = .81 χ2(1) = 0.167, p = .68 |
| Increase exercise | 4 (13) | 5 (12) | χ2(1) = 0.002, p = .96 |
| Balance exercises | 0 (0) | 1 (2) | χ2(1) = 0.781, p = .37 |
| Stop smoking | 3 (9) | 3 (7) | χ2(1) = 0.101, p = .71 |
| Begin medication | 11 (34) | 19 (49) | χ2(1) = 1.482, p = .22 |
| Receive written info | 5 (16) | 13 (33) | χ2(1) = 2.700, p = .10 |
Note: UCG = usual care group; CBIG = computer-based intervention group; Other Race = (African American = 12; Latino = 1; Asian [n = 4]; Other [n = 1]).
Measures of the theoretical constructs include knowledge and health beliefs (general beliefs, self-efficacy, outcome expectancy, and goal congruence), self-regulation skills and abilities, social facilitation, and proximal outcomes (calcium and vitamin D intake; Table 1).
Knowledge and Health Beliefs: Facts on Osteoporosis Quiz (Ailinge, Harper, & LaSusa, 2003) is a 30-item multiple-choice tool that measures the general knowledge about osteoporosis and personal management obtained pre- and post-intervention. All correct responses equal to 100%. Prior studies indicated a content validity index of 0.92 and Cronbach’s alpha of .84 in middle-age women.
Osteoporosis Health Beliefs (Kim, Horan, Gendler, & Patel, 1991) was modified for this study by excluding question related to exercise. In this study, the tool contained 27 items measured on 5-point linear rating scale ranging from strongly disagree (0) to strongly agree (5). In prior studies, this dimension of the scale reported Cronbach’s alphas ranging from .74 to .84.
The Osteoporosis Self-Efficacy scale was developed as a 21-item scale measuring exercise and calcium (Horan, Kim, Gendler, Froman, & Patel, 1998). For the purposes of this study, the 11 calcium items were retained, and two items related to vitamin D were added. The modified scale contained 13 question rated on a visual analogue scale. Cronbach’s alpha of .93 has been reported for the calcium scale. Outcome expectancy for calcium is a 13-item scale, which was adapted from the self-efficacy scale (Horan et al., 1998) by retaining the items but changing the stem question to evaluate outcome expectancy.
Goal congruence is a newly developed 22-item linear rating scale with scores ranging from 0 (not able) to 6 (able) that measures personal goal congruence related to osteoporosis prevention. The seven most common areas of goal congruence identified by middle-age women included having the time or resources to change, weight management, lactose intolerance, constipation with supplementation, and putting the needs and desires of others first (Maierle & Ryan, 2011).
Use of the electronic intervention (time and frequency) and section use (goal setting, self-monitoring, feedback, reflective journaling, decision making, and planning) were used as measures of the self-regulation and automatically collected via computer. Self-management behaviors were measured via a 3-day food diary obtained for 3 consecutive days, including 2 weekdays and 1 weekend day. Using the data collection form provided, women were instructed to record all foods eaten by meal or snack, food brand or name of restaurant chain when available, serving size, number of servings, and all beverages. The food diary requested women to list use of calcium and vitamin D supplements and multivitamins (including brand, mg of calcium, and number taken). A researcher reviewed the first completed food diary with the participant, stressing the importance of noting specific brands and listing individual ingredients in food selections (e.g., type and amount of greens, other vegetables, cheeses, nuts and seed, and dressing rather than “small salad”). Content from the food diary was entered into ESHA Food Processor SQL software by a researcher (Bazzano et al., 2002) to determine calcium and vitamin D contained in each food and their daily intake of calcium and vitamin D.
Procedure
Community dwelling women responded to study advertisements via email or voice mail. A member of the research team contacted study volunteers to explain the study in greater depth, answer questions, determine eligibility, and obtain verbal consent. Women who met eligibility criteria received a mailing containing a written description of the study, an outline of participant activities, and a 3-day food diary with a request to complete the diary prior to the enrollment meeting. A 2-hr meeting was scheduled at one of the research offices or at a public site containing an Internet connection, such as a public library, office, or coffee shop. At the initial meeting, a written consent and baseline data were obtained and random assignment occurred.
A sealed opaque envelope containing assignment to group and a study identification number was included in folders prepared prior to initiation of the study. Folders, stored in large sealed manila envelopes, were randomly selected, sequentially numbered, and stored by number. At the time of an enrollment appointment, a member of the research team took the next sequentially numbered envelope to the appointment. The opaque envelope was opened by the participant following consent and collection of baseline data. Hence, participants and researchers were blinded to group only until initial data were collected.
Uses of all components of the intervention were demonstrated to participants by a member of the research team. Participants were requested to provide a return demonstration validating their ability to successfully work with the equipment and the intervention. Women received written directions on use of the intervention and a member of the research team was available 50 hr per week by telephone for questions and directions on media use. Additional in-person instruction was available if desired.
Participant burden was decreased by limiting appointments to the baseline. (A researcher picked up the handheld computer at the end of the intervention for women in CBIG.) Follow-up questionnaires were completed and returned by mail in prepaid envelopes at 8 and 14 weeks and 6 months. Women received a message (phone or email based on their preference) reminding them to mail the completed questionnaires. Ten percent of women (n = 16) returning data from all four times were randomly selected to receive a US $50 gift card to a local shopping mall.
Analysis
Analysis was performed on an intention to treat basis. The primary analysis approach was linear modeling using Generalized Estimating Equations (GEE) with autoregressive working correlation structure to account for within-person repeated measures. For the purposes of interpretation, the GEE model is similar to repeated measures ANOVA; however, it does not require the correct specification of the variance-covariance structure of the repeated observations. In addition, this approach allows incorporation of incomplete data from dropouts using the missing-at-random assumption; the response pattern of the dropouts is assumed to be similar to nondropouts with similar observed measurements. Standard errors were estimated using robust sandwich estimates. When means were reported, least-squares means were adjusted for attrition.
Analyses were performed using SPSS 17 (IBM, Armork, NY) and SAS 9.2 (SAS Institute, Cary, NC). Although used extensively by other disciplines, use of GEE in nursing is relatively new and offers a desirable approach for analysis of repeated measures studies with attrition (Liu, Dixon, Qiu, Tian, & McCorkle, 2013).
Results
Sample
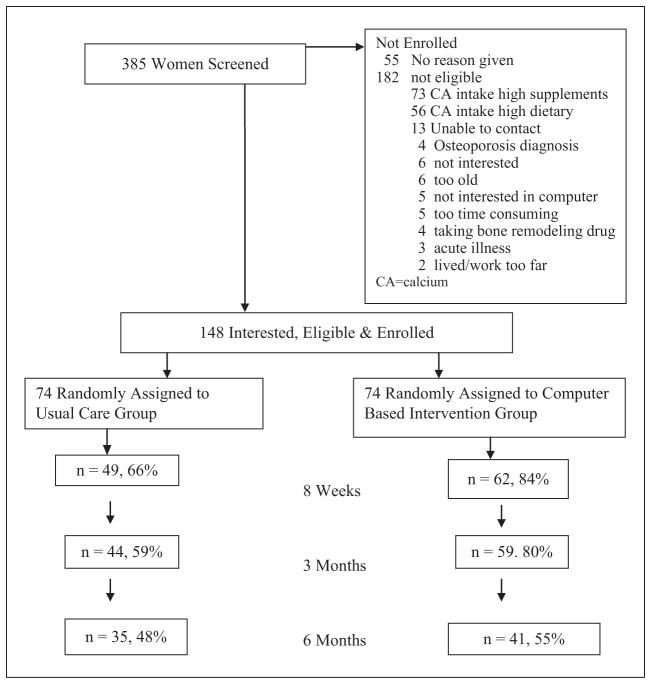
A total of 148 women were enrolled in the study (74 in CBIG and UC groups; Table 2). In general, the sample consisted of well-educated, partnered, White women 50 years of age, in various stages of menopause. There were no significant differences between groups with the exception of race—with the CBIG having a higher number of non-White women than the UCG (p = .02). Mean age of women in the UCG was 50.55 (SD = 5.36) and 49.68 (SD = 5.53) in the CBIG, t(146) = .98, p = .33. The mean socioeconomic status in the UCG was 31.90 (SD = 9.83) and 30.96 (SD = 9.49) in the CBIG, t(144) = .58, p = .56. The mean number of risk factors for osteoporosis in the UCG was 5.02 (SD = 1.65) and 5.05 (SD = 1.73) for the CBIG, t(133) = .15, p = 88. Attrition varied over time and between groups with a higher percent of participants in the UCG dropping out earlier and dropping out altogether than participants in the CBIG (Figure 2). Attrition was higher than the estimated 20% as 87% of the sample participated at 8 weeks, 80% at 3 months, and 59% at 6 months.
Figure 2.
Participant flow.
Measures
Measures had good estimates of reliability in this sample. Cronbach’s alphas of self-efficacy, outcome expectancy, goal congruence, and satisfaction with computer were greater than .90 (.93, .97, .94, and .94, respectively) except for the general Health Belief measure (.65). With the assistance of a nutritionist, the research team achieved and maintained greater than 95% interrater agreement in matching foods listed on the 3-day diary to food choices listed in the software to calculate calcium and vitamin D intake (Bazzano et al., 2002).
Attrition
Out of 148 participants in total, 35 did not have a measurement for the second time point. A two-sample t test was performed under the assumption of unequal variance to compare baseline measurement for the two groups. Persons completing data at baseline but failing to complete data at 8 weeks were similar to those who did not drop out on most characteristics, except that they had significantly lower calcium taken via supplement (M = 75.2 mg vs. 196.9 mg), t(106.0) = 3.1, p < .05, and total calcium intake (926.7 mg vs. 1,104.4 mg), t(61.3) = 2.0, p = 0.05, than persons completing data at baseline and 8 weeks.
Minimal or decreasing use of the intervention over time by individuals has been identified as a precursor to attrition (Eysenbach, 2005). The impact of total use of the intervention on calcium and vitamin D intake was evaluated using GEE in CBIG. There was no statistically significant differences for the average intake from food, χ2(3) = 0.85, p = .83, supplementation, χ2(3) = 1.86, p = .601, or for the combined total of food and supplementation, χ2 = 0.80, p = .85, among women who used the intervention with different intensity. Similarly, there was no statistically significant differences for the average intake of vitamin D from food, χ2(3) = 0.56, p = .90, supplementation, χ2(3) = 2.28, p = .56, or the combination of food and supplementation, χ2(3) = 2.14, p = .54, among women who used the intervention with different intensity.
Calcium and Vitamin D
The GEE models showed statistically significant differences for the average calcium (measured in mg) intake from food (p < .02), average calcium intake from supplement (p < .04; Table 3), and the average total calcium intake (p < .01) between the CBIG and the UCG over time (Table 3 and Figure 3). The specific results of the analysis of GEE parameter estimates for calcium intake from food are presented on Table 4. There were no differences between groups for vitamin D intake from food, supplement, or total (measured in international unit [IU]; Table 3 and Figure 3). Specifically, the 14-week follow-up time stands out for its increased calcium intake from all sources in the CBIG group, but not in the UCG. Analysis of percentage calcium intake, accounting for menopausal status, revealed comparable results between the CBIG and UCG.
Table 3.
Knowledge, Measures of Beliefs, Calcium, and Vitamin D by Group Over Time.
| Variable | Group | Baseline: M (SD) | 8 weeks: M (SD) | 14 weeks: M (SD) | 6 months: M (SD) | Tests of difference between groups over time |
|---|---|---|---|---|---|---|
| CBIG | n = 74 | n = 62 | n = 48 | n = 40 | ||
| UCG | n = 74 | n = 49 | n = 42 | n = 32 | ||
| Knowledge | CBIG | 64 (17) | 75 (16) |
F(1) = 2.060 p = .15 |
||
| UCG | 66 (19) | 79 (14) | ||||
| Health beliefs | GEE statistic group × Time | |||||
| Osteoporosis | CBIG | 79 (14) | 80 (13) | 80 (12) | 78 (11) | χ2(3) = 4.56 p = .21 |
| UCG | 78 (13) | 81 (14) | 77 (13) | 74 (15) | ||
| Self-efficacy | CBIG | 74 (13) | 73 (15) | 75 (18) | 69 (17) | χ2(3) = 8.29 p = .04 |
| UCG | 74 (15) | 70 (18) | 71 (17) | 73 (17) | ||
| Outcome expectancy | CBIG | 76 (18) | 77 (14) | 78 (18) | 77 (19) | χ2(3) = 3.23 p = .35 |
| UCG | 78 (14) | 79 (16) | 78 (14) | 79 (17) | ||
| Goal congruence | CBIG | 88 (12) | 85 (17) | 87 (16) | 86 (14) | χ2(3) = 7.53 p = .06 |
| UCG | 87 (14) | 86 (13) | 83 (16) | 86 (18) | ||
| Proximal outcomes | ||||||
| Calcium (mg) | ||||||
| CBIG | n = 70 | n = 60 | n = 48 | n = 41 | GEE statistic group × Time | |
| UCG | n = 71 | n = 50 | n = 42 | n = 34 | ||
| Food | CBIG | 884 (347) | 913 (382) | 1,023 (404) | 915 (349) | χ2(3) = 10.41 p = .02 |
| UCG | 902 (397) | 914 (515) | 848 (364) | 931 (377) | ||
| Supplement | CBIG | 184 (272) | 378 (410) | 432 (453) | 305 (472) | χ2(3) = 8.07 p = .04 |
| UCG | 149 (263) | 331 (449) | 263 (363) | 425 (510) | ||
| Total | CBIG | 1,069 (461) | 1,291 (616) | 1,456 (634) | 1,220 (619) | χ2(3) = 12.99 p < .01 |
| UCG | 1,051 (491) | 1,245 (683) | 1,111 (569) | 1,356 (694) | ||
| Vitamin D (IU) | GEE Statistic Group × Time | |||||
| Food | CBIG | 103 (100) | 133 (99) | 150 (107) | 116 (94) | χ2(3) = 5.70 p = .17 |
| UCG | 117 (105) | 133 (96) | 141 (107) | 145 (109) | ||
| Supplement | CBIG | 201 (324) | 224 (281) | 348 (440) | 372 (554) | χ2(3) = 0.19 p = .97 |
| UCG | 157 (360) | 223 (277) | 320 (452) | 298 (379) | ||
| Total | CBIG | 304 (353) | 378 (310) | 499 (483) | 488 (551) | χ2(3) = 0.05 p = .99 |
| UCG | 276 (389) | 356 (317) | 462 (453) | 443 (398) | ||
Note: CBIG = computer-based information group, UCG = usual care group; mg = milligrams; IU = international unit; GEE = generalized estimating equations. All results have been rounded to whole number. Bold indicates statistically significant differences (p < .1).
Figure 3.
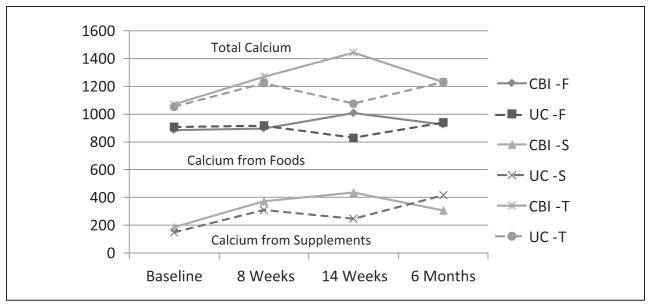
Calcium intake (milligrams): Total, food, supplement between groups over time.
Note: CBI = computer-based intervention; UC = usual care; F = food; S = supplement; T = total.
Table 4.
Calcium Intake (in Milligrams) From Food: Analysis of GEE Parameter Estimates.
| Estimate (CI)
|
Estimate (CI)
|
|
|---|---|---|
| Parameter | p value | p value |
| Intercept | Baseline usual care | Group effect at baseline CBI-UC |
| 906.8 [815.0, 998.6] | −20.7 [−142.8, 101.4] p = .74 |
|
| Time | UC | Group by time interaction CBI-UC |
| 8 weeks–baseline | 11.2 [−120.1, 142. 5] p = .87 |
0.6 [−164.1, 165.4] p = .99 |
| 14 weeks 3–baseline | −78.0 [−171.8, −15.8] p = .10 |
200.2 [54.8, 345.6] p = .01 |
| 6 months–baseline | 33.0 [−88.2, 154.3] p = .59 |
7.0 [−156.4, −170.4] p = .94 |
| Across all times | Interaction effect: Time by group | |
| p = .11 | p < .02 |
Note: GEE = generalized estimating equations; CI = confidence interval; CBI = computer-based information; UC = usual care. Bold indicates statistically significant differences (p < .1)
Knowledge and Health Beliefs
Knowledge was measured at baseline and 8 weeks. Results of an ANOVA indicated there were no significant differences in knowledge between groups (Table 3) at baseline (M = 61.95–67.71) but increased in both groups at T2 (M = 73.64–79.38).
The GEE models showed statistically significant differences for self-efficacy (p = .04) between the CBIG and UCG over time (Table 3). The p value approached significance for goal congruence with differences between groups over time (p = .05). There were no differences between groups for outcome expectancy (p = 3.57) or health beliefs (p = .20) between groups over time (Table 3).
Health beliefs were further evaluated by extending the GEE model for calcium and vitamin D intake. The extended model included self-efficacy, outcome expectancy, goal congruence, and osteoporosis beliefs in addition to time, group, and interaction. Self-efficacy was a consistent predictor of calcium and vitamin D intake in food, supplement, and total intake (all p < .05) with the exception of vitamin D intake in food. Osteoporosis belief was a predictor of calcium supplement intake only (Table 5).
Table 5.
Effects of Health Beliefs on Calcium and Vitamin D Intake, Adjusted for Intervention Group and Follow-Up Time.
| Food: M (CI)
|
Supplement: M (CI)
|
Total: M (CI)
|
|
|---|---|---|---|
| p | p | p | |
| Calcium | |||
| Self-efficacy |
4.6 [1.5, 7.7] p = .04 |
5.5 [2.2, 8.8] p < .01 |
10.2 [5.3, 15.0] p < .01 |
| Outcome expectancy | 0.0 [−2.5, 2.5] p = .98 |
−0.6 [−3.4, 2.1] p = .64 |
−0.5 [−4.2, 3.3] p = .80 |
| Goal congruence | 2.9 [−0.8, 6.7] p = .13 |
0.2 [−3.0, 3.3] p = .90 |
3.2 [−2.0, 8.4] p = .22 |
| Osteoporosis beliefs | −2.0 [−5.0, 1.0] p = .20 |
4.7 [1.4, 8.1] p = .01 |
2.7 [−1.7, 7.1] p = .23 |
| Vitamin D | |||
| Self-efficacy | 0.3 [−0.3, 1.0] p = .31 |
6.0 [3.6, 8.4] p < .01 |
6.8 [4.1, 9.4] p < 01 |
| Outcome expectancy | −0.1 [−0.7, 0.6] p = .87 |
−0.2 [−2.6, 2.2] p = .88 |
−0.2 [−2.8, 2.5] p = .89 |
| Goal congruence | 0.6 [−0.3, 1.6] p = .21 |
0.7 [−2.3, 3.6] p = .66 |
1.3 [−2.0, 4.7] p = .43 |
| Osteoporosis beliefs | −0.7 [−1.6, 0.1] p = .09 |
3.0 [−0.1, 6.1] p = .05 |
2.1 [−1.1, 5.3] p = 0.20 |
Note: M = estimate of the mean, accounting for attrition; CI = confidence interval. Predictive effect of a 1-point change in score. Bold indicates statistically significant or approaching statistically significant differences.
Discussion
Findings from this study supported the hypothesis that women in CBIG would reach a higher level of calcium intake than women in the UCG. Specifically, with respect to outcomes, there was a statistically significant difference for calcium from foods, supplementation, and total between groups over time. Noteworthy is the finding that these women were able to increase their calcium by increasing the dietary source of calcium—clearly the most desirous and difficult behavior change to make. The study did not support maintenance of calcium intake over time, a finding noted in other studies evaluating health behavior change over time (Sedlak, Doheny, Estok, Zeller, & Winchell, 2007; Winzenberg et al., 2006).
With respect to health beliefs, there was a statistically significant difference in self-efficacy between groups over time and difference in goal congruence approached statistical significant differences between groups over time. Self-efficacy was identified as a predictor of calcium intake from foods, supplements, and total intake.
Recruitment efforts were effective, and for this sample, approximately 2.6 volunteers needed to be screened for every woman enrolled in the sample. The most common reason volunteers were ineligible to participate was too high of a calcium intake. Women in this sample were willing to use a CBI for osteoporosis health prevention.
Strengths of this study included use of a theoretical framework, use of RCT with random assignment of participant to one of two groups (CBI or UCG), measures with good estimates of reliability and validity, and the use of GEE to measure differences between groups over time accounting for attrition.
The comparison group in this study consisted of UC. Baseline evaluation indicated all women in the study had a reasonably high level of knowledge about osteoporosis and behaviors involved in prevention. Providing all women in the UCG with identical printed information provided the potential for similar levels of knowledge within that group.
Study limitations included an intervention that required two types of computer technology, unexpected high rates of attrition, and limited focus on nutrition. Use of two types of the computers needed to deliver CBI created additional complexity to the delivery media, a factor that could have affected study outcomes. The impact of the CBI was evaluated by examining enrollment, use, and satisfaction. Five of the 385 women screened, approximately 1.3%, identified the computerized intervention as the reason for not participating. Analysis of use of the intervention demonstrated no difference in calcium or vitamin D intake by the intensity of intervention use. In addition, as documented in an earlier publication, women in CBIG reported high levels of satisfaction with the computerized intervention (Maierle & Ryan, 2011). Available information did not support the complexity of the intervention as a reason for failure to maintain behavior change over time. It is recommended that the relationships among delivery media, content, and outcomes continue to be evaluated in future studies. Assessment tools are now available to measure e-literacy, a factor that may moderate the effect of computerized interventions (Norman & Skinner, 2006).
This study had higher than anticipated rates of attrition. Attrition is a problem common to repeated-measure designs with attrition increasing over time (Polit & Beck, 2004; Shadish, Cook, & Campbell, 2002). Attrition decreases the power to determine differences between groups, and differential attrition suggests that the intervention in addition to the participants differentially affected groups. In this study, little difference between groups was observed. The computer group retained a higher level of participation than the UCG over time.
Eysenbach (2005) proposed the “Law of Attrition” noting that e-Health interventions (electronic delivery media) have extremely high rates of attrition with studies reporting as few as 1% of participants completing electronic interventions with similar decreases in intervention use over time. He hypothesized that 14 factors led to decrease use, a precursor to attrition, and to actual attrition. Although intervention use can be more closely studied in electronic media than in other types of media, better access to utilization data does not account for the high rates of attrition in computer-based studies. Among the factors associated with diminishing use and attrition are the ease of drop out, lack of personal contact, lack of buy-in from health care providers, and the burden of data collection without personal benefit. He suggested that attrition from studies might mirror adoption problems people experience on a day-to-day basis and identified an opportunity for e-health researchers to include evaluation of use and discontinuation as it relates to achievement of outcomes.
Creative and comprehensive programs to reduce attrition are needed for futures studies testing the effectiveness of computer-based osteoporosis prevention programs. Results of a systematic review of effective strategies to decrease attrition identified gradually increasing incentives over time and having a dedicated member of the research team responsible maintenance of participants (Caldwell, Hamilton, Tan, & Craig, 2010). Use of quality management systems are recommended to automatically track enrollment and participation rates increasing the capacity of researchers to have the flexibility to make adjustments based on data (Dow, McNees, & Loerzel, 2005; McNees, Dow, & Loerzel, 2005). Increased contact with members of the research team and other study participants has become increasingly possible with computer delivery methods, and additional research is needed to evaluate the impact of electronic communication on attrition.
The participants for this study were recruited from community dwelling women between the ages of 40 and 60 years. These participants were well educated and generally employed, factors limiting generalizability of these results.
This study focused on nutritional intake, one of several health behaviors related to osteoporosis prevention. Rather than testing all osteoporosis prevention behaviors (activity and exercise, balance, monitoring, pharmacology), this study tested the effects of using all dimensions of the processes of health behavior change (knowledge and health beliefs, self-regulation skills and abilities, and social facilitation). The process of changing health behaviors, as explicated in the ITHBC, is newly conceptualized and smaller scale research was needed prior to developing and testing a comprehensive osteoporosis prevention program.
The results of this randomized control feasibility trial provided support for the use of a tailored, patient-centered, theoretically based intervention delivered via computer media on women’s intake of calcium and vitamin D in this group of women. Based on these preliminary findings, additional testing of osteoporosis health promotion behaviors using computer-based deliver media is warranted prior to its widespread use.
The newly developed midrange theory, ITHBC, was foundational to intervention development as well as the research method. The intervention developed for this study uniquely focused on the process of health behavior change, specifically enhancing knowledge and health beliefs, developing self-regulation skills and abilities, and fostering social facilitation. Focusing on process added a new and unique dimension to current behavior change interventions.
The challenge to determine how to maintain health behavior change remains. This study provides evidence that this group of midlife women used technology to change their calcium intake. Commercially developed computer software is available and being purchased by people interested in changing their health behaviors. These programs are trendy and in demand, but these programs may or may not incorporate scientific evidence and are rarely based on theory. Additional research on the efficacy of computer intervention on the long-term maintenance of health behavior change is necessary prior to widespread adoption.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported, in part, by the Clinical and Translational Science Award (CTSI) program of the National Center for Research Resources, National Institutes of Health (5M01RR000058-45 Dunn; Effectiveness of a Tailored Intervention for Osteoporosis, Ryan); Center for Enhancement of Self-Management in Individuals and Families (Marek, 1P20NR0010674-01); Tailored Computerized Intervention for Behavior Change (Ryan, 1R15NR009021-01A2); and Tailored Computerized Intervention for Behavior Change (Brennan, Ryan Post-Doctoral Fellow, T32, NR07102).
Footnotes
Authors’ Note
Detailed results of the analysis of GEE Parameter Estimates for calcium intake from supplements and total, self-efficacy, and goal congruence are available upon request.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Ailinge RL, Harper DC, LaSusa HA. Facts on osteoporosis quiz. In: Redman B, editor. Measurement tools in patient education. 1. New York, NY: Springer; 2003. pp. 379–380. [Google Scholar]
- Arthritis Foundation. Osteoporosis and you! What’s all the talk about my bones? Atlanta, GA: Author; 1999. [Google Scholar]
- Bazzano LA, He J, Ogden LG, Loria CM, Vupputuri S, Myers L, Whelton PK. Agreement on nutrient intake between the databases of the first national health and nutrition examination survey and the ESHA food processor. American Journal of Epidemiology. 2002;156:78–85. doi: 10.1093/aje/kwf003. [DOI] [PubMed] [Google Scholar]
- Caldwell PHY, Hamilton S, Tan A, Craig JC. Strategies for increasing recruitment to randomised controlled trials: Systematic review. PLoS Medicine. 2010;7(11):e1000368. doi: 10.1371/journal.pmed.1000368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole ZA, Dennison EM, Cooper C. Osteoporosis epidemiology update. Current Rheumatology Reports. 2008;10:92–96. doi: 10.1007/s11926-008-0017-6. [DOI] [PubMed] [Google Scholar]
- Dow KH, McNees P, Loerzel VW. Novel application of the CuSum technique to evaluate changes in recruitment strategies on referral and enrollment: Implications for prospective recruitment management. Oncology Nursing Forum. 2005;32(1):155. doi: 10.1097/00006199-200511000-00006. [DOI] [PubMed] [Google Scholar]
- Eysenbach G. The law of attrition. Journal of Medical Internet Research. 2005;7(1):e11. doi: 10.2196/jmir.7.1.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead AB. Four factor index of social status. Yale Journal of Sociology. 2011;8:21–53. [Google Scholar]
- Holroyd C, Cooper C, Dennison E. Epidemiology of osteoporosis. Best Practice & Research Clinical Endocrinology & Metabolism. 2008;22:671–685. doi: 10.1016/j.beem.2008.06.001. [DOI] [PubMed] [Google Scholar]
- Horan ML, Kim KK, Gendler P, Froman RD, Patel MD. Development and evaluation of the osteoporosis self-efficacy scale. Research in Nursing & Health. 1998;21:395–403. doi: 10.1002/(sici)1098-240x(199810)21:5<395::aid-nur3>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Kim KK, Horan ML, Gendler P, Patel MK. Development and evaluation of the osteoporosis health belief scale. Research in Nursing & Health. 1991;14:155–163. doi: 10.1002/nur.4770140210. [DOI] [PubMed] [Google Scholar]
- Lauver DR, Ward SE, Heidrich SM, Keller ML, Bowers BJ, Brennan PF, Wells TJ. Patient-centered interventions. Research in Nursing & Health. 2002;25:246–255. doi: 10.1002/nur.10044. [DOI] [PubMed] [Google Scholar]
- Liu S, Dixon J, Qiu G, Tian Y, McCorkle R. Using generalized estimating equations to analyze longitudinal data in nursing research. Western Journal of Nursing Research. 2013;31:948–964. doi: 10.1177/0193945909336931. [DOI] [PubMed] [Google Scholar]
- Maierle D, Ryan P. Evaluation of satisfaction and use of electronic intervention for behavior change. Computers, Informatics, Nursing. 2011;29:622–629. doi: 10.1097/NCN.0b013e318224b4b2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNees P, Dow KH, Loerzel VW. Application of the CuSum technique to evaluate changes in recruitment strategies. Nursing Research. 2005;54:399–405. doi: 10.1097/00006199-200511000-00006. [DOI] [PubMed] [Google Scholar]
- National Osteoporosis Foundation. Clinician’s guide to prevention and treatment of osteoporosis. Washington, DC: Author; 2008a. [Google Scholar]
- National Osteoporosis Foundation. Boning up on osteoporosis: A guide to prevention and treatment. Washington, DC: Author; 2008b. Called calcium calculator; p. 20. [Google Scholar]
- Norman CD, Skinner HA. eHEALS: The eHealth Literacy Scale. Journal of Medical Internet Research. 2006;8(4):e27. doi: 10.2196/jmir.8.4.e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osteoporosis, Prevention, Diagnosis, and Treatment. NIH consensus statement. 2000 Mar 27–29;17(1):1–45. [PubMed] [Google Scholar]
- Polit DF, Beck CT. Nursing research: Principles and methods. 7. Philadelphia, PA: Lippincott Williams & Wilkins; 2004. [Google Scholar]
- Recker R. NOF President, Dr. Robert Recker, delivered remarks Friday, September 9 at the joint meeting of the FDA reproductive health drugs and drug safety and risk management advisory committee; 2011. Retrieved from http://nof.org/news/127. [Google Scholar]
- Ryan P. Tailored computerized intervention for behavior change. Bethesda, MD: National Institutes of Health, National Institute of Nursing Research; 2006. (NINR [Ryan, 1R15NR009021-01A2] NIH Award No. 1R15NR00 9021-01A2), Patient Centered Information Interventions (Brennen, Ryan Post-doctoral Fellowship, T32NR07102) [Google Scholar]
- Ryan P. Integrated theory of health behavior change: Background and intervention development. Clinical Nurse Specialist. 2009;23:161–710. doi: 10.1097/NUR.0b013e3181a42373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan P, Lauver DR. The efficacy of tailored interventions. Journal of Nursing Scholarship. 2002;34:331–337. doi: 10.1111/j.1547-5069.2002.00331.x. [DOI] [PubMed] [Google Scholar]
- Ryan P, Pumilia NJ, Henak B, Chang T. Development and performance usability testing of a theory-based, computerized, tailored intervention. Computers, Informatics, Nursing. 2009;27:288–298. doi: 10.1097/NCN.0b013e3181b21779. [DOI] [PubMed] [Google Scholar]
- Ryan P, Sawin KJ. The individual and family self-management theory: Background and perspectives on context, process, and outcomes. Nursing Outlook. 2009;57:217–225.e6. doi: 10.1016/j.outlook.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan P, Schlidt A, Ryan C. The impact of osteoporosis prevention programs on calcium intake: A systematic review. Osteoporosis International. 2013 doi: 10.1007/s00198-012-2259-4. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Sanchez-Riera L, Wilson N, Kamalaraj N, Nolla JM, Kok C, Li Y, March L. Osteoporosis and fragility fractures. Best Practice & Research: Clinical Rheumatology. 2010;24:793–810. doi: 10.1016/j.berh.2010.10.003. [DOI] [PubMed] [Google Scholar]
- Schnatz PF, Marakovits KA, Dubois M, O’Sullivan DM. Osteoporosis screening and treatment guidelines: Are they being followed? Menopause. 2011;18:1072–1078. doi: 10.1097/gme.0b013e318215101a. [DOI] [PubMed] [Google Scholar]
- Sedlak CA, Doheny MO, Estok PJ, Zeller RA, Winchell J. DXA, health beliefs, and osteoporosis prevention behaviors. Journal of Aging and Health. 2007;19:742–756. doi: 10.1177/0898264307304303. [DOI] [PubMed] [Google Scholar]
- Shadish WR, Cook TP, Campbell DT. Experimental and quasi-experimental design. Boston, MA: Houghton Mifflin; 2002. [Google Scholar]
- U.S. Department of Health & Human Services. Bone health and osteoporosis: A report of the surgeon general. Rockville, MD: Author; 2004. [Google Scholar]
- U.S. Preventive Services Task Force. Screening for osteoporosis: U.S. preventive services task force recommendation statement. Annals of Internal Medicine. 2011;154:356–364. doi: 10.7326/0003-4819-154-5-201103010-00307. [DOI] [PubMed] [Google Scholar]
- Winzenberg T, Oldenburg B, Frendin S, De Wit L, Riley M, Jones G. The effect on behavior and bone mineral density of individualized bone mineral density feedback and educational interventions in premenopausal women: A randomized controlled trial. BMC Public Health. 2006;6:12. doi: 10.1186/1471-2458-6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. WHO scientific group on the assessment of osteoporosis at primary health care level. Brussels, Belgium: Author; 2007. [Google Scholar]