Abstract
Introduction
Cancer survivors are at increased risk for influenza-related complications. Racial disparities in preventive health services have not been extensively studied among cancer survivors. Our objective is to compare influenza vaccination prevalence among black and white cancer survivors
Methods
We performed a secondary data analysis of 41,346 white and black cancer survivors (excluding non-melanoma skin cancer) from the 2009 Behavioral Risk Factor Surveillance System survey. Respondents were asked whether they had received an influenza vaccination in the previous year. Multivariable logistic regression was used to estimate the odds of having influenza vaccine by race.
Results
Sixty-five percent of whites reported receiving the vaccine in the last year compared to 50 % of blacks. Blacks had significantly lower odds of vaccination after controlling for covariates significantly associated with the odds of influenza vaccination. Higher education, having health insurance, having a primary care provider, and having a routine check-up in the last year increased the odds of receiving an influenza vaccine.
Conclusions
Our analysis supports that racial disparities in vaccine coverage persist among cancer survivors, a group strongly recommended to receive annual influenza vaccine, even when predictors significantly associated with increased vaccination are controlled for.
Implications for Cancer Survivors
As a nationally representative survey with a large sample size, our study provides a picture of self-reported vaccine coverage among cancer survivors in the USA and the disparity that exists between blacks and whites in this population. Care teams can use these findings to better target follow-up care for cancer survivors.
Keywords: Cancer survivorship, Influenza vaccines, Healthcare disparities, Health services
Introduction
Influenza is a contagious viral respiratory illness that affects approximately 5–20 % of the USA population each year [1], with an average of 24,000 deaths annually [2]. Influenza is associated with an annual $87.1 billion economic burden, $10.1 billion of that in direct medical costs alone [3]. Vaccination is the single most effective tool to prevent influenza and its associated complications [4]. While it does not completely eliminate the risk of contracting influenza, vaccination dramatically reduces the likelihood of infection. For most Americans infection results in an uncomplicated illness, for others influenza can cause complications that require urgent medical care including hospitalization. This is particularly true for elderly individuals and those with underlying chronic medical conditions, including cancer [5].
There are now more than 12 million cancer survivors in the USA [6] and that number is projected to rise to 18 million by 2020 [7]. Cancer screening with earlier detection, combined with advances in cancer treatment, has resulted in people living longer after a diagnosis of cancer [8]. While it is not known if being a cancer survivor increases the risk of influenza infection, it is known that cancer survivors are at increased risk of influenza-related complications including death and hospitalization [9]. Similarly, morbidity and mortality related to influenza infection are usually highest among people aged 65 and older [10–12], which is the age group most associated with cancer in the USA [13].
Over the past two decades efforts have been made to reduce health disparities in the American population [14]. In addition to setting the goal of eliminating health disparities, Healthy people 2020 has set the target for influenza vaccination prevalence at 90 % for adults aged 65 and older and increased the target from 60 % to 90 % for high-risk non-institutionalized adults aged 18–64 [15]. While racial disparities in influenza vaccination have been reported [16, 17], most studies related to influenza vaccination and cancer survivors have not focused directly on race differences among cancer survivors and instead use individuals without cancer as the comparison group [10, 12, 18–20]. Our study is the first, to our knowledge, to directly investigate racial disparities in influenza vaccination among cancer survivors.
Influenza vaccination has been proposed as an indicator to monitor progress in eliminating racial disparities [21]. Influenza vaccination is administered frequently enough to closely monitor trends in health care seeking behavior. Seasonal flu vaccine does not require physician referral and is covered by Medicare; thereby, limiting the effect that access to healthcare should have on coverage. High-risk populations, such as cancer survivors, have historically been encouraged to receive this vaccination each year; therefore, examination of influenza vaccination as a health behavior provides data to explore disparity trends among black and white cancer survivors. We compared influenza vaccine prevalence in black and white cancer survivors using data from the 2009 Behavioral Risk Factor Surveillance System (BRFSS) [22].
Methods
Study sample
The BRFSS is supported and overseen by the Centers for Disease Control and Prevention (CDC) Behavioral Surveillance Branch (BSR). Designed to measure health behaviors and behavioral risk factors for disease among adults in the USA, it is conducted annually by all 50 states, the District of Columbia and the U.S. Territories of Guam, Puerto Rico, and the Virgin Islands. The 2009 BRFSS was a random digit dial telephone survey, collecting data on non-institutionalized adults 18 years of age and older, residing in households with a land-line telephone; households selected by dispro-portionate stratified random sampling. One adult per house-hold is eligible to respond. In 2009, data were collected from 432,607 respondents who lived in 54 states and territories [23]. The median response rate for interviews was 52.5 % [24]. Established in 1984, BRFSS is the longest continually conducted phone survey in the world. This dataset is publicly available on the CDC BRFSS website (http://www.cdc.gov/brfss/technical_infodata/surveydata.htm) and its use for this project was approved by the Institutional Review Board at the University of Maryland Baltimore as non-human subjects research.
Study variables
Data from the 2009 questionnaire were used to define the study sample, exposure variable, and outcome variable. Three questions were used to define cancer survivorship. Respondents were asked if they had “ever been told by a doctor, nurse, or other health professional that [they] had cancer,” the number of different types of cancer they had, and what was the type of cancer at the most recent diagnosis. Respondents who answered “yes” to the first question and did not have “other skin cancer” (presumed to be non-melanoma skin cancer) as their most recent diagnosis were included in our sample of cancer survivors.
Respondents were asked to self-identify their race. Those indicating white or black were included. Respondents indicating a race other than white or black, refused to answer or indicated that they did not know or were not sure of their race were excluded from the study sample. We determined who had received influenza vaccine by the subject's response to the question “during the last 12 months have you had a flu shot.” Respondents who replied “don't know,” “not sure,” or “refused” were excluded from the analysis.
We included the following independent predictor variables in our analyses: age (18–34, 35–44, 45–54, 55–64, or 65 years and older), sex, marital status (married/widowed/partnered, divorced, or separated/never married); education (high school graduate and less than high school vs. some college or more); general health status (excellent/very good/good or fair/poor); health care coverage (yes or no); has a health care provider (yes or no); could not see a doctor due to cost in last 12 months (yes or no); time since last routine check-up (within the last 12 months or 1 year or more); time since cancer diagnosis (less than or equal to 5 years or more than 5 years ago); and smoking status (never smoked, former smoker, or current smoker).
Statistical analysis
All statistical analyses were performed using SAS 9.2 (SAS Institute Inc., Carey, North Carolina). Frequencies by race were compared using the chi-square statistic. We used a three-step procedure to identify potential confounders and potential effect modifiers. The first step was to compute the crude (i.e., bivariate) association between our outcome variable, receipt (yes vs. no) of immunization, and each of our exposure variables. As a second step, the bivariate analyses were re-run adjusting for one additional covariate entered as a categorical variable (age, sex, marital status, education, general health status, health care coverage, has a health care provider, could not see a doctor due to cost in last 12 months, time since last routine check-up, time since cancer diagnosis, and smoking status). We used the Breslow–Day test to compare levels of the categorical variable to determine if the additional covariate was a potential confounder (Breslow– Day test p≥0.10 indicating homogeneity within levels of the additional covariate) or a potential effect modifier (Breslow–Day test p<0.10, indicating heterogeneity). As a third step, potential confounders were further tested by comparing the crude odds ratio with the adjusted odds ratio using the Mantel–Haensel odds ratio. If the crude OR and the Mantel–Haensel OR differed by 10 % or more, the additional covariate was treated as a potential confounder. Our adjusted analyses were performed using multivariable logistic regression that incorporated all the variables identified as potential confounders and effect modifiers (Table 2). Age was found to significantly modify the effect of race on vaccine status. In the adjusted analysis within each of the five age groups, we report the odds of receiving influenza vaccination in blacks compared to whites. For all other variables, we report the adjusted odds relative to a reference level within the variable (e.g., separated/never married is the reference category for the marital status variable).
Table 2. Demographic and general health status characteristics of cancer survivor respondents to the 2009 Behavioral Risk Factor Surveillance System Questionnaire by Influenza Vaccination (n=41,346).
| Characteristic | Received influenza vaccine in last 12 months n (Row %) | Did not receive influenza vaccine in last 12 months n (Row %) | Chi-square p value |
|---|---|---|---|
| Total | 26,317 (63.7) | 15,029 (36.3) | |
| Race | |||
| White | 25,118 (64.5) | 13,817 (35.5) | <0.0001 |
| Black/African American | 1,199 (49.7) | 1,212 (50.3) | |
| Sex | |||
| Male | 9,644 (67.2) | 4,704 (32.8) | <0.0001 |
| Female | 16,673 (61.8) | 10,325 (38.2) | |
| Age (yr) | |||
| 18–34 | 237 (30.7) | 534 (69.3) | <0.0001a |
| 35–44 | 584 (32.4) | 1,216 (67.6) | |
| 45–54 | 2,193 (44.4) | 2,748 (55.6) | |
| 55–64 | 5,333 (56.0) | 4,195 (44.0) | |
| 65+ | 17,970 (73.9) | 6,336 (26.1) | |
| Marital status | |||
| Married/widowed/partnered | 21,082 (66.2) | 10,784 (33.8) | <0.0001 |
| Divorced | 3,433 (55.3) | 2,774 (44.7) | |
| Separated/never married | 1,733 (54.8) | 1,430 (45.2) | |
| Education | |||
| High school grad or less | 10,476 (62.7) | 6,244 (37.3) | <0.001 |
| Some college or more | 15,799 (64.3) | 8,763 (35.7) | |
| General health | |||
| ≥ Good | 17,662 (62.8) | 10,464 (37.2) | <0.0001 |
| ≤Fair | 8,447 (65.5) | 4,456 (34.5) | |
| Health care coverage | |||
| Yes | 25,623 (65.3) | 13,637 (34.7) | <0.0001 |
| No | 661 (32.5) | 1,370 (67.5) | |
| Has a health care provider | |||
| Yes | 25,482 (65.1) | 13,658 (34.9) | <0.0001 |
| No | 796 (37.2) | 1,346 (62.8) | |
| Could not see a doctor due to cost in last 12 months | |||
| Yes | 1,509 (41.2) | 2,152 (58.8) | <0.0001 |
| No | 24,769 (65.9) | 12,838 (34.1) | |
| Last routine check up | |||
| <12 months | 22,795 (67.2) | 11,114 (32.8) | <0.0001 |
| ≥1 year | 3,238 (46.6) | 3,713 (53.4) | |
| Years since cancer diagnosis | |||
| ≤5 years | 8,690 (62.4) | 5,242 (37.6) | <0.0001 |
| >5 years | 16,630 (64.4) | 9,211 (35.6) | |
| Smoking status | |||
| Never | 12,065 (63.9) | 6,827 (36.1) | <0.0001 |
| Former | 11,534 (69.3) | 5,105 (30.7) | |
| Current | 2,613 (46.3) | 3,031 (53.7) | |
Cochran–Armitage Trend Test p<0.0001
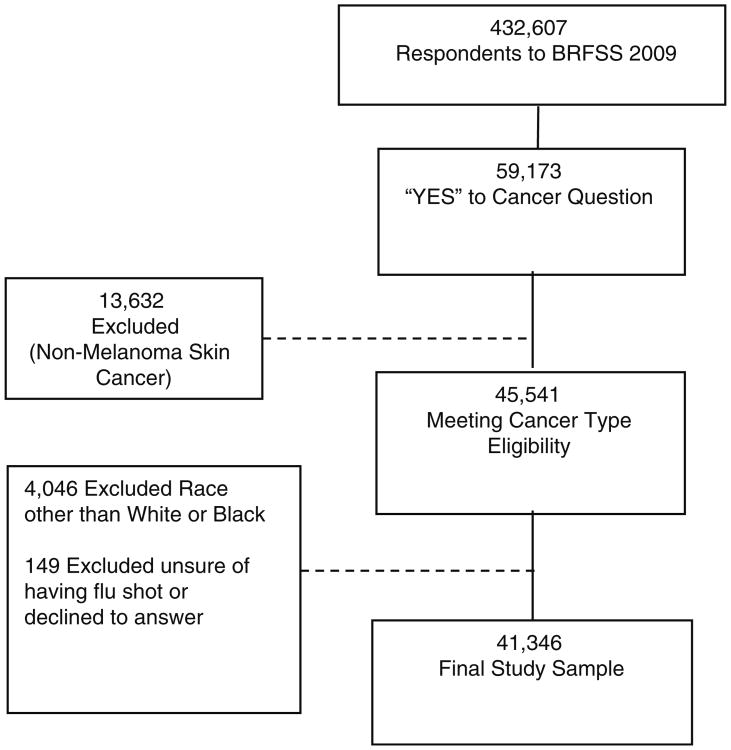
In 2009, 432,607 adults responded to the BRFSS survey. A total of 59,173 (14 %) reported that they had been told by a health professional that they had had cancer. After excluding those reporting a most recent diagnosis of “other” skin cancer, 45,541 met the criteria for inclusion in the analysis. One-hundred forty-nine respondents who indicated that they were unsure whether they had received the influenza vaccine or refused to provide a response were excluded (Fig. 1). After excluding respondents whose race was other than white or black (n=4,046), 41,346 respondents remained in the final analysis. A comparison of the crude results, including and excluding the 149 subjects who indicated they were unsure or refused to answer whether they received the influenza vaccine, revealed no difference in the results (data not shown). Only participants who answered “yes” or “no” to the influenza vaccination question were included (data not shown).
Fig. 1. Cancer survivor respondents to the 2009 Behavioral Risk Factor Surveillance System Questionnaire.
Results
The study sample was predominantly female (65 %) and white (94 %; Table 1). Compared to blacks, whites had a higher proportion of respondents in the oldest age group and had a higher proportion in the married/widowed/partnered categories. Whites also had a higher proportion of respondents that had some college or more, reported excellent, very good, or good health status, and reported having health insurance. Compared to blacks, whites had a higher proportion reporting more than 5 years since their most recent cancer diagnosis. Blacks had a higher proportion of respondents indicating they had received a routine check-up in the last 12 months. Blacks also had a significantly higher proportion of respondents indicating they had not been able to see a doctor in the last 12 months due to cost.
Table 1. Demographic and general health characteristics of cancer survivor respondents to the 2009 Behavioral Risk Factor Surveillance System Questionnaire by Race (n=41,346).
| Characteristic | Total n=41,346 | White n=38,935 column (%) | Black/African-American n=2,411 column (%) | Chi-square p value |
|---|---|---|---|---|
| Total | 38,935 (94.2) | 2,411 (5.8) | ||
| Age (yr) | ||||
| 18–34 | 771 (1.8) | 698 (1.8) | 73 (3.0) | <0.0001 |
| 35–44 | 1,800 (4.4) | 1,666 (4.3) | 134 (5.6) | |
| 45–54 | 4,941 (12.0) | 4,583 (11.8) | 358 (14.9) | |
| 55–64 | 9,528 (23.0) | 8,865 (22.8) | 663 (27.5) | |
| 65+ | 24,306 (58.8) | 23,123 (59.4) | 1,183 (49.1) | |
| Sex | ||||
| Male | 14,348 (34.7) | 13,526 (34.7) | 822 (34.1) | 0.52 |
| Female | 26,998 (65.3) | 25,409 (65.3) | 1,589 (65.9) | |
| Marital status | ||||
| Married/widowed/partnered | 31,866 (77.2) | 30,498 (78.5) | 1,368 (57.0) | <0.0001 |
| Divorced | 6,207 (15.1) | 5,669 (14.6) | 538 (22.4) | |
| Separated/never married | 3,163 (7.7) | 2,667 (6.9) | 496 (20.6) | |
| Education | ||||
| High school grad or less | 16,720 (40.5) | 15,441 (39.7) | 1,279 (53.2) | <0.0001 |
| Some college or more | 24,562 (59.5) | 23,435 (60.3) | 1,127 (46.8) | |
| General health | ||||
| ≥Good | 28,128 (68.6) | 26,808 (69.4) | 1,320 (55.3) | <0.0001 |
| ≤Fair | 12,903 (31.4) | 11,836 (30.6) | 1,067 (44.7) | |
| Health care coverage | ||||
| Yes | 39,260 (95.1) | 37,085 (95.4) | 2,175 (90.4) | <0.0001 |
| No | 2,031 (4.9) | 1,799 (4.6) | 232 (9.6) | |
| Has a health care provider | ||||
| Yes | 39,140 (94.8) | 36,890 (94.9) | 2,250 (93.7) | 0.01 |
| No | 2,142 (5.2) | 1,991 (5.1) | 151 (6.3) | |
| Could not see a doctor due to cost in last 12 months | ||||
| Yes | 3,661 (8.9) | 3,258 (8.4) | 403 (16.8) | <0.0001 |
| No | 37,607 (91.1) | 35,611 (91.6) | 1,996 (83.2) | |
| Last routine check up | ||||
| <12 months | 33,909 (83.0) | 31,807 (82.7) | 2,102 (88.1) | <0.0001 |
| ≥ 1 year | 6,951 (17.0) | 6,666 (17.3) | 285 (11.9) | |
| Years since cancer diagnosis | ||||
| ≤ 5 years | 13,932 (35.0) | 13,020 (34.7) | 912 (40.1) | <0.0001 |
| > 5 years | 25,841 (65.0) | 24,477 (65.3) | 1,364 (59.9) | |
| Smoking status | ||||
| Never | 18,892 (45.9) | 17,723 (45.7) | 1,169 (48.9) | <0.0001 |
| Former | 16,639 (40.4) | 15,801 (40.7) | 838 (35.1) | |
| Current | 5,644 (13.7) | 5,261 (13.6) | 383 (16.0) | |
The overall prevalence of influenza vaccination among this study sample of cancer survivors was 64 % (Table 2). The unadjusted prevalence of self-reported influenza vaccination increased significantly as age increased, from only 31 % of those aged 18–34 to 74 % among respondents aged 65 and older (Cochran–Armitage trend test, p<0.0001). Influenza vaccination was also higher among men, married/widowed/partnered respondents, those with “fair” or “poor” self-reported health status, the insured, those with a primary care physician, and those with a routine check-up in the last year. Influenza vaccination prevalence was lower among those who could not see a doctor in the last year due to cost and among current smokers. A significantly lower proportion of black respondents reported having the influenza vaccination (50 %) compared to white respondents (65 %). In the unadjusted analysis, blacks had 0.54 (95 % CI 0.50–0.59) times the odds of having influenza vaccination in the last year compared to whites (data not shown).
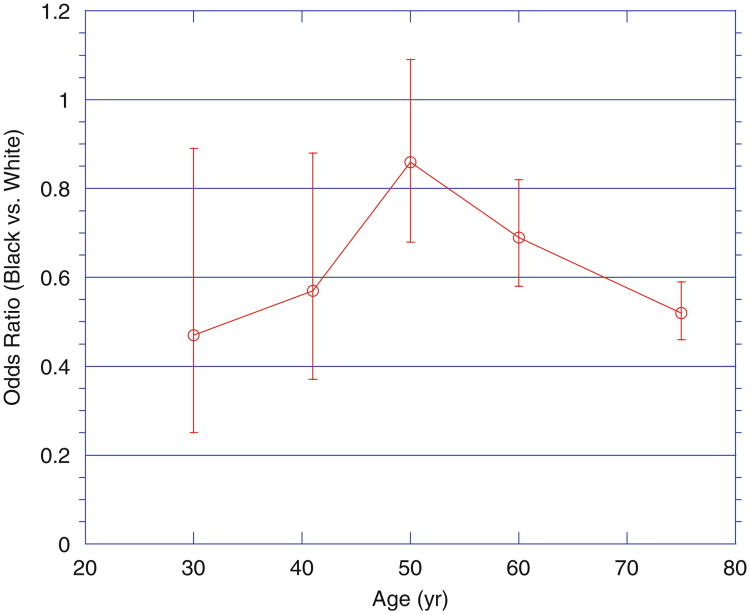
In the fully adjusted model (Table 3), blacks at all ages had a lower adjusted odds of receiving influenza vaccination than whites and the odds were significantly lower in all but the 45 to 54 age group (Fig. 2). Of note, blacks who were 65 years of age or older had lower odds of receiving influenza vaccination, 0.52 (95 % CI 0.46–0.59) times the odds of vaccination in comparison with whites. Having some college education or higher, having health insurance, having a primary care provider, having a routine check-up in the last year, and being a former smoker were significantly associated with increased odds of vaccination. Individuals who could not see a doctor in the last year due to cost or were current smokers had significantly lower odds of vaccination. A significant difference was not seen between individuals whose most recent cancer diagnosis was within the last 5 years or more than 5 years ago.
Table 3. Adjusted Odds Ratios and 95 % confidence intervals for the receipt of influenza vaccination in the last 12 months among cancer survivor respondents to the 2009 Behavioral Risk Factor Surveillance System Questionnaire.
| Characteristic | Adjusted odds ratio | 95 % CI |
|---|---|---|
| Age (the reference group is whites in the same age category) | ||
| 18–34 | 0.47 | 0.25–0.90 |
| 35–44 | 0.57 | 0.37–0.88 |
| 45–54 | 0.86 | 0.68–1.09 |
| 55–64 | 0.69 | 0.58–0.82 |
| 65+ | 0.52 | 0.46–0.59 |
| Sex | ||
| Female | Ref. | |
| Male | 1.03 | 0.99–1.08 |
| Marital status | ||
| Separated/never married | Ref. | |
| Divorced | 0.85 | 0.77–0.93 |
| Married/widowed/partnered | 0.99 | 0.91–1.07 |
| Education | ||
| High school grad or less | Ref. | |
| Some college or more | 1.19 | 1.13–1.24 |
| Health care coverage | ||
| No | Ref. | |
| Yes | 1.51 | 1.35–1.69 |
| Has a health care provider | ||
| No | Ref. | |
| Yes | 1.85 | 1.66–2.05 |
| Could not see a doctor due to cost in last 12 months | ||
| No | Ref. | |
| Yes | 0.79 | 0.73–0.86 |
| Last routine check up | ||
| ≥1 year | Ref. | |
| <12 months | 1.76 | 1.66–1.87 |
| Years since most recent cancer | diagnosis | |
| ≤5 years | Ref. | |
| >5 years | 1.04 | 0.99–1.09 |
| Smoking status | ||
| Never | Ref. | |
| Former | 1.15 | 1.10–1.21 |
| Current | 0.71 | 0.66–0.76 |
All OR adjusted for all other predictors in the model. All covariates reported relative to a reference level within the covariate, e.g., within marital status, divorced was the reference level
Fig. 2. Adjusted odds of influenza vaccination among black cancer survivor respondents compared to white cancer survivor respondents to the 2009 Behavioral Risk Factor Surveillance System Questionnaire by age group (n=38,921).
Discussion
We found that the overall prevalence of vaccine coverage among cancer survivors was 64 %; far lower than what is desirable in a population at increased risk for influenza-related complications. We also found that a significantly lower proportion of cancer survivors who identified their race as black reported having received the influenza vaccine in the last year. This difference is consistent with data reported on immunization coverage in the US by the CDC in 2003 [25]. While other studies have shown that racial disparities in influenza vaccination coverage persist even after controlling for other factors [26–28], few have focused on racial disparities among high-risk populations such as cancer survivors.
Age significantly modified the effect of race on influenza vaccination. The odds of black respondents having influenza vaccination were consistently lower in every age group, although not statistically different for blacks aged 45–54 compared to whites of the same age. Our findings of no significant difference by race for those aged 45–54 are similar to those reported by Setse et al. in the January 2011 MMWR supplemental report on vaccine coverage in the USA [29]. They reported no difference by race in vaccine coverage for BRFSS and National 2009 H1N1 Flu Survey respondents aged 18 to 49 with high-risk conditions. The MMWR article included conditions such as asthma, diabetes, heart disease, and kidney problems which may contribute to the slight difference in findings. The prevalence of vaccine coverage in our study increased significantly as age increased in both racial groups which may be consistent with the general increase in comorbid conditions as people age necessitating more frequent and or intensive health care by older adults. This age trend is also consistent with the 2010 study by Shih and Pan which looked at families of cancer survivors compared to families with no history of cancer where vaccination prevalence was significantly higher among older age groups. This article also showed that blacks had significantly lower odds of vaccination prevalence [19]. All cancer survivors are recommended to have the influenza vaccine each year. The low prevalence of vaccine coverage in the youngest age groups in our study appears to reflect a similar age trend among the non-cancer respondents to the 2009 BRFSS survey. This low prevalence among younger cancer survivors is of significant concern and may represent an opportunity for the health care community to reemphasize the importance of preventing influenza through vaccination among younger cancer survivors.
Of particular interest are the significantly lower odds of vaccination in blacks among the population at highest risk for influenza-related complications, those aged 65 and older. As Medicare pays for one influenza vaccine each year [30], there may be other factors related to race such as cultural belief or access to care that contribute to blacks in this age group having decreased odds of vaccination compared to insured whites. However, as information related to insurance type is not available for our study sample, conclusions should be drawn cautiously and further study may be necessary to more accurately determine factors that contribute to this disparity.
Our study also confirms the findings of several other studies that investigated predictors related to influenza vaccine coverage. Respondents with a primary care provider [12], at least some college education [17, 19], and a routine checkup [31] in the last 12 months had significantly higher odds of vaccination than those in the respective comparison groups. We also found that patients reporting cost as a barrier to seeing a physician in the last 12 months to be significantly associated with decreased odds of influenza vaccination. Most studies focus on income or combined indicators of socio-economic status when assessing associations with vaccine coverage [11, 17] which does not provide a direct comparison with the findings of our study. However, cost as a barrier is most likely associated with socio-economic status. It may be of interest to further investigate whether cost is an equal barrier among the insured and uninsured as not all insurance covers seasonal influenza vaccination, especially as health care reform is implemented differently, state by state.
While a significantly greater proportion of white respondents had more than 5 years of cancer survivorship compared to black respondents, we did not find years of survivorship to significantly modify or confound the effect of race on vaccine coverage. Respondents in their first 5 years of survival actually had slightly lower vaccine prevalence. Coordination between cancer specialists and primary care providers to ensure all health needs are met by cancer survivors (including preventive services such as immunizations, medical screening, and cancer screening) is an essential component of survivorship care. The relatively low vaccine coverage overall regardless of survival time however, may be related to the need for survivor care plans to focus on general and preventive health in addition to cancer-related care and follow-up [32]. In addition, as cancer survivorship length increases and cancer survivors receive more of their health care from primary care providers, ensuring that influenza vaccination is offered at these visits will become increasingly important.
Our study is subject to some limitations. As a household-based survey, BRFSS excludes institutionalized and non-civilian individuals, therefore cancer survivors that were hospitalized, residing in a long-term care facility or in hospice care, were not represented in the study sample. However, with the emphasis on preventive care for infectious illnesses such as influenza in long term care facilities, this would most likely lead to an underestimate in our sample rather than overestimate of actual vaccine prevalence in the population. BRFSS is also self-report data which can often be subject to recall bias. However, studies have validated self-report data with regards to vaccination, including influenza vaccination [33, 34]. As we used the most recent cancer diagnosis to define our study sample, we may have missed some patients whose first cancer diagnosis was not a non-melanoma skin cancer. Our study has a number of strengths. The large representative nature of BRFSS makes this study generalizable to the non-institutionalized population of cancer survivors over the age of 18. Our sample is also larger than similar studies in the present literature. Additionally, few studies have looked at racial disparities in influenza vaccination specifically among cancer survivors.
Implications for cancer survivors
Influenza vaccine coverage remains much lower than desirable among cancer survivors. Vaccine prevalence exceeded 70 % only in those aged 65 or older and was 64 % overall. Black respondents had only 50 % vaccine prevalence overall. Now that the recommendations for seasonal influenza vaccination have been expanded to include all individuals ≥6 months of age, it would be useful to review high-risk population respondents in subsequent years, as well as other studies that collect preventive health care service utilization information. As a nationally representative survey with a large sample size, our study provides a representative picture of self-reported vaccine coverage among cancer survivors in the USA and the disparity that exists between blacks and whites in this population. This information can be used to help better target preventive health care messages and services to this high-risk population. Our study demonstrates that individuals with lower educational achievement, less than yearly routine check-ups, who are divorced, and those who identify cost as a barrier to seeing a physician have significantly lower odds of receiving influenza vaccination. Most significantly, our study demonstrates that racial disparities in vaccine coverage persist among cancer survivors even when predictors significantly associated with increased vaccination are controlled for. Care teams can use these findings to better target follow-up care for cancer survivors.
Acknowledgments
Grant support The work reported in this paper was supported by the Baltimore VA Medical Center Geriatric Research, Educational and Clinical Center, the Claude D. Pepper Older Americans Independence Center 5 P30 AG028747 07, and the Clinical Research Curriculum Award 8 K30 TR000106 08 (Sorkin).
Footnotes
Conflicts of interest The authors declare they have no conflict of interest.
Contributor Information
Kristen A. Stafford, Department of Epidemiology and Public Health, University of Maryland School of Medicine, 660 West Redwood Street, Suite 100 Howard Hall, Baltimore, MD 21201, USA
John D. Sorkin, Department of Veterans Affairs, Geriatric Research, Education, and Clinical Center, Baltimore VA Medical Center, Baltimore, MD 21201, USA; Department of Medicine, Division of Gerontology and Geriatric Medicine, University of Maryland School of Medicine, Baltimore, MD 21201, USA
Eileen K. Steinberger, Email: estein@epi.umaryland.edu, Department of Epidemiology and Public Health, University of Maryland School of Medicine, 660 West Redwood Street, Suite 100 Howard Hall, Baltimore, MD 21201, USA.
References
- 1.Centers for Disease Control and Prevention. Seasonal influenza. [Accessed 11, 2012]; http://www.cdc.gov/flu/about/qa/disease.htm.
- 2.Centers for Disease Control and Prevention (CDC) Updated estimates of mortality associated with seasonal influenza through the 2006–2007 influenza season. MMWR Morb Mortal Wkly Rep. 2010;59(33):1057–62. [PubMed] [Google Scholar]
- 3.Molinari N, Ortegasanchez I, Messonnier M, Thompson W, Wortley P, Weintraub E, et al. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine. 2007;25(27):5086–96. doi: 10.1016/j.vaccine.2007.03.046. [DOI] [PubMed] [Google Scholar]
- 4.Tosh PK, Jacobson RM, Poland GA. Influenza vaccines: from surveillance through production to protection. Mayo Clin Proc. 2010;85(3):257–73. doi: 10.4065/mcp.2009.0615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Glezen WPGS, Atmar RL, Piedra PA, Couch RB. Impact of respiratory virus infections on persons with chronic underlying conditions. JAMA. 2000;283:499–505. doi: 10.1001/jama.283.4.499. [DOI] [PubMed] [Google Scholar]
- 6.Altekruse SF, Kosary CL, Krapcho M, Neyman N, Aminou R, Waldron W, Ruhl J, Howlader N, Tatalovich Z, Cho H, Mariotto A, Eisner MP, Lewis DR, Cronin K, Chen HS, Feuer EJ, Stinchcomb DG, Edwards BK, editors. SEER cancer statistics review, 1975–2007. Bethesda: National Cancer Institute; [Accessed 11 Sep 2012]. http://seer.cancer.gov/csr/1975_2007/, based on November 2009 SEER data submission, posted to the SEER web site, 2010. [Google Scholar]
- 7.Warren JL, Mariotto AB, Meekins A, Topor M, Brown ML. Current and future utilization of services from medical oncologists. J Clin Oncol. 2008;26(19):3242–7. doi: 10.1200/jco.2007.14.6357. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (CDC) Cancer survivors - United States, 2007. MMWR Morb Mortal Wkly Rep. 2011;60(9):269–96. [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Cancer, the flu, and you. [Accessed 11, 2012]; http://www.cdc.gov/cancer/flu/
- 10.McBean A. The use of preventive health services among elderly uterine cancer survivors. Am J Obstet Gynecol. 2008;198(1):86.e1–e8. doi: 10.1016/j.ajog.2007.05.036. [DOI] [PubMed] [Google Scholar]
- 11.Fairley TL, Hawk H, Pierre S. Health behaviors and quality of life of cancer survivors in Massachusetts, 2006: data for comprehensive cancer control. [Accessed 11, 2012];Prev Chronic Dis. 2010 7(1):A09. http://www.cdc.gov/pcd/issues/2010/jan/09_0062.htm. [PMC free article] [PubMed] [Google Scholar]
- 12.Snyder CF, Frick KD, Peairs KS, Kantsiper ME, Herbert RJ, Blackford AL, et al. Comparing care for breast cancer survivors to non-cancer controls: a five-year longitudinal study. J Gen Intern Med. 2009;24(4):469–74. doi: 10.1007/s11606-009-0903-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Institute NC. Incidence and mortality rates by age. 2007 [Google Scholar]
- 14.U.S. Department of Health and Human Services. Healthy people 2020. [Accessed 11, 2012]; http://www.healthypeople.gov/2020/about/DisparitiesAbout.aspx.
- 15.U.S. Department of Health and Human Services. Healthy people 2020. [Accessed 11, 2012]; http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=23.
- 16.Ompad D, Galea S, Vlahov D. Distribution of influenza vaccine to high-risk groups. Epidemiol Rev. 2006;28:54–70. doi: 10.1093/epirev/mxj004. [DOI] [PubMed] [Google Scholar]
- 17.Linn ST, Guralnik JM, Patel KV. Disparities in influenza vaccine coverage in the United States, 2008. J Am Geriatr Soc. 2010;58(7):1333–40. doi: 10.1111/j.1532-5415.2010.02904.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Findley P, Sambamoorthi U. Preventive health services and lifestyle practices in cancer survivors: a population health investigation. J Cancer Surviv. 2009;3(1):43–58. doi: 10.1007/s11764-008-0074-x. [DOI] [PubMed] [Google Scholar]
- 19.Shih YCT, Pan IW. Influenza vaccination among individuals with cancer and their family members. Am J Prev Med. 2010;38(1):61–9. doi: 10.1016/j.amepre.2009.09.032. [DOI] [PubMed] [Google Scholar]
- 20.Snyder CF, Earle CC, Herbert RJ, Neville BA, Blackford AL, Frick KD. Trends in follow-up and preventive care for colorectal cancer survivors. J Gen Intern Med. 2008;23(3):254–9. doi: 10.1007/s11606-007-0497-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fiscella K. Commentary - anatomy of racial disparity in influenza vaccination. Health Serv Res. 2005;40(2):539–50. doi: 10.1111/j.1475-6773.2005.00371.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Behavioral risk factor surveillance system 2009 survey overview. [Accessed 11, 2012]; http://www.cdc.gov//brfss/technical_infodata/surveydata/2009.htm.
- 23.Centers for Disease Control and Prevention. Behavioral risk factor surveillance survey 2009 summary data quality report. [Accessed 11, 2012]; http://www.cdc.gov/BRFSS/technical_infodata/quality.htm.
- 24.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System 2009 Summary Data Quality Report. [Accessed 11, 2012]; http://www.cdc.gov/BRFSS/technical_infodata/quality.htm.
- 25.Centers for Disease Control and Prevention (CDC) Racial/ethnic disparities in influenza and pneumococcal vaccination levels among persons aged ≥65 years - United States, 1989–2001. MMWR Morb Mortal Wkly Rep. 2003;52(40):958–62. [PubMed] [Google Scholar]
- 26.Gornick ME, Eggers PW, Reilly TW, Mentnech RM, Fitterman LK, Kucken LE, et al. Effects of race and income on mortality and use of services among Medicare beneficiaries. N Engl J Med. 1996;335(11):791–9. doi: 10.1056/NEJM199609123351106. [DOI] [PubMed] [Google Scholar]
- 27.Fiscella K, Dressler R, Meldrum S. Impact of influenza vaccination disparities on elderly mortality in the United States. Prev Med. 2007;45:83–7. doi: 10.1016/j.ypmed.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 28.Hebert P, Frick K, Kane R, McBean A. The causes of racial and ethnic differences in influenza vaccination rates among elderly Medicare beneficiaries. Health Serv Res. 2005;40(2):517–37. doi: 10.1111/j.1475-6773.2005.00370.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Setse RW, Euler GL, Gonzalez-Feliciano AG, Bryan LN, Furlow C, et al. Influenza vaccination coverage - United States, 2000– 2010. MMWR Surveill Summ. 2011;60(Suppl):38–41. [PubMed] [Google Scholar]
- 30.Centers for Medicare and Medicaid Services. Immunizations. [Accessed 11, 2012]; https://www.cms.gov/AdultImmunizations/02_Providerresources.asp.
- 31.Winston CA, Wortley PM, Lees KA. Factors associated with vaccination of Medicare beneficiaries in five U.S. communities: results from the racial and ethnic adult disparities in Immunization Initiative survey, 2003. J Am Geriatr Soc. 2006;54(2):303–10. doi: 10.1111/j.1532-5415.2005.00585.x. [DOI] [PubMed] [Google Scholar]
- 32.Hewitt M, Greenfield S, Stovall E, editors. From cancer patient to cancer survivor: lost in transition. Washington, DC: Institute of Medicine and National Research Council; 2006. [Google Scholar]
- 33.Shenson D, DiMartino D, Bolen J, Campbell M, Lu PJ, Singleton JA. Validation of self-reported pneumococcal vaccination in behavioral risk factor surveillance surveys: experience from the sickness prevention achieved through regional collaboration (SPARC) program. Vaccine. 2005;23(8):1015–20. doi: 10.1016/j.vaccine.2004.07.039. [DOI] [PubMed] [Google Scholar]
- 34.Zimmerman RK, Raymund M, Janosky JE, Nowalk MP, Fine MJ. Sensitivity and specificity of patient self-report of influenza and pneumococcal polysaccharide vaccinations among elderly outpatients in diverse patient care strata. Vaccine. 2003;21(13–14):1486–91. doi: 10.1016/s0264-410x(02)00700-4. [DOI] [PubMed] [Google Scholar]