Abstract
Purpose of review
To review commonly encountered adverse ocular effects of illicit drug use.
Recent findings
Drug and alcohol abuse can produce a variety of ocular and neuro-ophthalmic side effects. Novel, so-called “designer,” drugs of abuse can lead to unusual ocular disorders. Legal substances, when used in manners for which they have not been prescribed, can also have devastating ophthalmic consequences.
Summary
In this review we will systematically evaluate each part of the visual pathways and discuss how individual drugs may affect them.
Keywords: drug abuse, alcohol abuse, fetal alcohol syndrome, endophthalmitis, drug induced ocular manifestations
Introduction
Drugs of abuse are substances which are either illicit, and are used by individuals recreationally, or are legal substances which are used in a manner for which they were not prescribed. Effects of these substances on the visual system can range from mild keratopathy, to severe vision loss from endophthalmitis or occipital lesions. The effects of drugs of abuse on the visual system is best addressed anatomically. Routes of administration include, but are not limited to, oral ingestion, nasal inhalation, intravenous injection, smoking, topical application, or application to other mucosal surfaces. The development of novel substances of abuse and novel routes of administration may surprise even the most astute clinician if substance abuse is not suspected.
Pre-corneal tear film
Abnormalities of the tear film can induce severe visual dysfunction due to the creation of an irregular refracting surface.
Smoking has been associated with an increased incidence of dry eye.[1] The Beaver Dam Eye Study found that dry eye symptoms were related to a history of heavy alcohol consumption, but not current alcohol consumption.[2]
A recent investigation of patients following ethanol ingestion described detection of ethanol in the tears, along with a decreased tear breakup time. The proposed mechanisms for the altered tear function were that ethanol increased tear osmolarity, acted as a solvent, and could disturb cytokine production.[3*] In this manner, ethanol could exacerbate the signs and symptoms of dry eye syndrome. A comparative case-control study between men who drank heavily (≥4 drinks per day) and non-drinkers showed that heavy ethanol ingestion was associated with a decreased tear break up time, lower Schirmer I test, as well as altered conjunctival impression cytology in comparison to non-drinkers.[4]
Conjunctiva
Conjunctival and ciliary injection is associated with use of marijuana [5] and with heroin use.
One of the more creative routes of use for heroin was recently described in a case report from Iran in which an individual presented with an unusual chronic conjunctival lesion.[6] Conjunctival biopsy revealed chronic inflammatory changes secondary to repeated topical applications of crystallized heroin into the inferior fornices.
Cornea
The cornea contains the highest concentration of nerve endings in the entire body. Both prescribed and illicit drugs of abuse topically-applied may anesthetize the cornea, leading to injuries of the ocular surface and predisposition to infectious corneal ulcers. Agents often implicated in these injuries include cocaine, crack cocaine,[7] and topical anesthetics.
Poulsen et al. described a case series of presumed methamphetamine-related corneal ulceration with devastating keratitis that resulted in perforation requiring penetrating keratoplasties.[8]
Self-prescription of topical anesthetics is well known to induce severe corneal damage. A series of 19 patients from Turkey described individuals who had suffered occupational injuries such as metallic foreign bodies, welding flash, or chemical injury. These patients either self medicated with proparacaine hydrochloride (available over the counter in Turkey) prior to hospitalization for corneal disease, or self medicated while hospitalized. Despite warnings of the devastating ocular consequences of anesthetic abuse, 12 of these patients continued to abuse their topical anesthetic. These patients were followed for at least one year, with 15.4% of the patients becoming legally blind.[9] A psychiatric evaluation may be indicated for patients with topical anesthetic abuse if they exhibit signs of Munchausen’s syndrome.[10] Finally, an orally ingested anti-tussive agent, benzonatate, has been reported to be abused as a topical anesthetic by breaking the capsules and directly applying the contained gel.[11]
Iris
Multiple drugs of abuse affect pupil size and reaction. Use of opiates, both legally and illicitly, leads to pupillary miosis.[5**] Cocaine’s inhibition of reuptake of norepinephrine causes pupillary mydriasis (useful in clinical practice in determining the presence of a Horner syndrome). Methamphetamine also causes pupillary mydriasis. Increasing use of a newer designer drug, “bath salts,” comprised of a variety of molecules in a class of chemicals called phenethylamines (which includes methamphetamine, 3,4-methylenedioxy-N-methylamphetamine (MDMA), and methcathinone) has led to a substantial number of poison control calls in the United States.[12] Route of administration of bath salts includes inhalation, oral ingestion, and injection.[12] Sale of 31 specific “bath salt” compounds in the United States was banned in July 2012. In an analysis of 1,633 emergency department visits for acute “bath salt” intoxication, 7.1% of patients had mydriasis, although co-ingestion of other intoxicants occurred at a rate of 26%.12 The ocular side effects of this class of drug of abuse will need to be further clarified if, despite their illegality, these drugs continue to increase in popularity.
Angle and Ciliary Body
Inhalation of marijuana leads to an acute short-term decrease in intraocular pressure,[13] suggesting the possible use of marijuana or its derivatives for the treatment of glaucoma. However, due to its short duration of action, lack of long-term studies, and the other deleterious effects of marijuana including decreasing blood pressure (and possible optic nerve head perfusion), the American Glaucoma Society issued a position statement that use of marijuana in the treatment of glaucoma is not recommended.[14] A single case of recurrent bilateral angle-closure glaucoma following the use of marijuana and MDMA was reported, with resolution of symptoms after cessation of MDMA use.[15]
The consumption of alcohol has been associated with elevated intraocular pressure and glaucoma in several studies.[16]
Lens
Drugs of abuse rarely directly affect the crystalline lens. However, multiple case reports of cataracts associated with fetal alcohol syndrome have been published.[17] A single case of bilateral congenital triangular cataracts in an infant of a methamphetamine-abusing mother was reported, but definite causation was not established.[18] Many studies have examined the association of alcohol consumption with cataract formation. These studies were summarized and analyzed by Wang, et al., who found that current evidence supports a mild protective effect of moderate alcohol consumption on cataract formation, and an increased prevalence of cataracts among heavy alcohol consumers.[16] The Beaver Dam Eye Study found that smoking cigarettes had a dose response relationship with the formation of cataracts.[19,20] Further studies have confirmed the association of cigarette smoking with cataract formation.[1,20]
Retina
Retinal pathology from illicit drug use includes embolic phenomena resulting from intravenous drug delivery. Talc retinopathy (embolic phenomena resulting from drug impurities delivered intravenously) was first described in patients who self-injected methylphenidate hydrochloride.[21] Refractile particles in the perifoveal arterioles, with possible retinal ischemia, is seen in patients with talc retinopathy. It is well documented in the ophthalmic literature to occur with other intravenously injected drugs as well.[22] Talc retinopathy may actually represent the accumulation of microemboli, rather than single embolic particles.[23] Localization of talc retinopathy to the inner retinal layers is now possible by demonstrating hyperreflective areas on ocular coherence tomography, corresponding to refractile bodies seen on funduscopy.[24] A recent publication described crystalline retinopathy as a result of intranasal methamphetamine use.[25] The mechanisms proposed included uptake by lymphoid tissue, and diffusion into pulmonary capillaries.
The use of intranasal cocaine was associated with the development of a bilateral, symmetric maculopathy, presenting as decreased color sensitivity, possibly from an adulterant.[26] A class of designer drugs, the alkyl nitrites, including isopropyl nitrite and isobutyl nitrite, has been implicated in “poppers maculopathy.”[27,28,29] The offending agent is inhaled. Symptoms include decreased central visual acuity, central scotoma, phosphenes, and metamorphopsia. These chemicals may lead to bilateral vision loss and altered structure of the macula, specifically altered structure at the inner segment/outer segment (IS/OS) retinal junction, as demonstrated on spectral-domain optical coherence tomography, and visible on funduscopy as a yellow spot at the fovea.[27,28] [Figure 1] The mechanism of deleterious action on the retina is unclear, but may include nitric oxide toxicity.[27,28,29]
Figure 1.
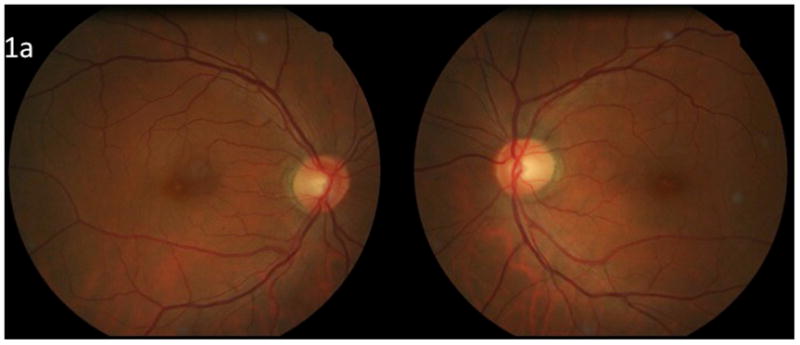
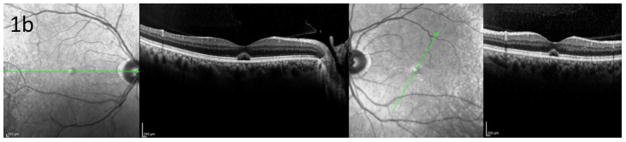
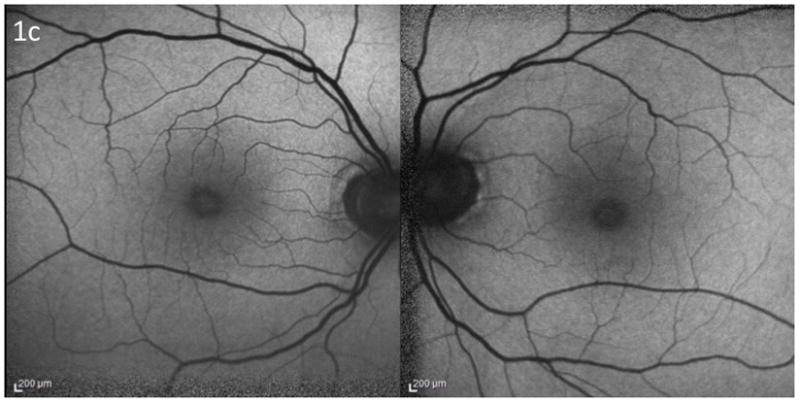
Poppers maculopathy: a) Fundus photographs demonstrating bilateral foveal yellow spots b) Ocular coherence tomography of the macula demonstrating bilateral damage to the foveal photoreceptors c) Fundus autofluorescence photographs demonstrating central hyperautofluorescence. Courtesy of Dr. Catherine Vignal and Pr. Michel Paques, Paris, France.
One of the most devastating consequences of intravenous drug abuse is the development of endophthalmitis. Contaminated instruments of drug injection are often implicated in the injection of offending organisms into the bloodstream, which then travel to the eye.[30] A variety of organisms have been demonstrated, most frequently candida, aspergillus, bacillus, staphylococcus, and pseudomonas, among many others.[30]
Retinal vascular occlusive disease is known to occur with many drugs of abuse, including cocaine and methamphetamine.[31,32,33] Additionally, two cases of branch retinal vein occlusions in young men using anabolic steroids for enhanced muscle development have been reported, with proposed etiologic factors of increased blood viscosity, abnormal vascular walls, and hypertension.[34] In a study comparing African-American patients who used cocaine with those who did not use cocaine, investigators found a wider retinal venular caliber and increased arterial branching, and proposed this may reflect more generalized central nervous system (CNS) microvascular disease.[35]
Age-related macular degeneration (ARMD) is associated with alcohol and tobacco use. Smoking has been found to be related to the incidence and progression of ARMD in several population-based studies.[36] In addition, polymorphisms in several genetic loci, including complement factor H, have been found to contribute to the additional risk of developing ARMD in smokers.[20] Several studies, both cross-sectional and prospective, have examined the effects of alcohol on the development of ARMD, but with no definite consensus.[1] There is a possible protective effect of moderate alcohol consumption, and possible adverse effect of heavy alcohol consumption on the development of ARMD.[16] A meta-analysis of published studies found that heavy drinking was associated with an increased risk of early ARMD.[37] The Beijing Eye Study found no association of moderate alcohol consumption on the development of ARMD.[38] However, the Melbourne Collaborative Cohort Study found an increased risk of both early and late age-related ARMD in individuals who consumed more than 20g of alcohol per day.[39]
Optic Nerve
The use of alcohol during fetal development can have the devastating consequential association of congenital abnormalities known as fetal alcohol syndrome. Optic nerve hypoplasia, although not a part of the diagnostic criteria described by the Centers for Disease Control and Prevention, is found in 61% of patients with fetal alcohol syndrome.[17] Interestingly, a recent investigation of children who were exposed to high levels of alcohol in utero in comparison to unexposed children revealed no increase in risk of developing ocular defects. This study suggests that ophthalmic screening should not be used to determine the presence of fetal alcohol syndrome, but that children who meet the criteria for fetal alcohol syndrome should have systematic eye examinations.[40]
Methanol ingestion most often occurs due to accidental consumption, and may induce a severe irreversible bliateral toxic optic neuropathy. The optic disc may become hyperemic with edema, followed by pallor and cupping. [Figure 2] The insult appears to be demyelinating early, and necrotic late. In a retrospective case series describing visual outcomes of methanol poisoning in which 37 patients with visual disturbances at presentation were followed, 62% of patients had complete recovery, 14% had partial recovery, 14% had complete blindness, and 11% had initial partial recovery followed by deterioration and complete blindness.[41] Treatments include ethanol (which competes with methanol metabolism) and hemodialysis.
Figure 2.
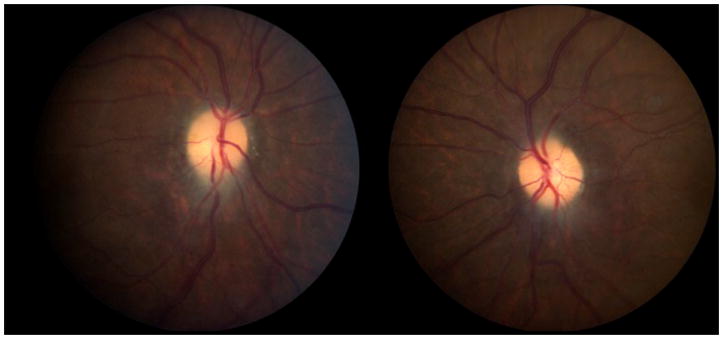
Fundus photographs of a patient with bilateral optic neuropathies secondary to methanol ingestion. Photographs show bilateral disc atrophy following disc edema. The patient’s vision was light perception in each eye.
Visual evoked potentials (VEP) can be used to measure the integrity of the visual pathways, specifically optic nerve function. A study in children who had in utero exposure to methadone and other drugs of abuse had abnormal visual evoked potentials in 60%, suggesting a very high rate of optic nerve toxicity.[42]
Several patients with Wernicke’s encephalopathy (ataxia, ophthalmplegia, and confusion) have been reported with disc edema and visual loss from optic neuropathies.[43–36] Li et al. described a patient with Wernicke’s encephalopathy with optic neuropathies in whom they found a mitochondrial DNA mutation that causes Leber hereditary optic neuropathy (LHON).[43] They propose that when there is vision loss in cases of Wernicke’s encephalopathy, an underlying genetic predisposition for LHON should be investigated.
So called “tobacco-alcohol amblyopia,” in which an optic neuropathy is attributed to the toxic effects of combined tobacco and alcohol use, should be eliminated from the medical lexicon.[47] This is not to say that tobacco does not contribute to the exacerbation of optic neuropathies. However, the contribution of alcohol use to the development of an optic neuropathy is likely due to malnutrition, and not the direct toxic effects of ethanol use. The Cuban optic neuropathy epidemic associated the use of tobacco, especially cigars, and malnutrition, to vision loss from an optic neuropathy.[48] Susceptible individuals who harbor the mitochondrial DNA mutations associated with LHON should be counseled to avoid smoking. Kirkman et al. found that smoking significantly increased the risk of vision loss in patients harboring mutations for LHON.[49] While not statistically significant, these individuals also had a trend toward visual loss with heavy alcohol intake.[49]
Orbit
Intranasal cocaine abuse can have devastating consequences for the orbit due to local ischemic damage leading to bony destruction, sometimes with pneumocele.[50] Intranasal cocaine abuse has led to severe sinusitis extending into the orbit causing an optic neuropathy and orbital apex syndrome.[51,52] In one case of orbital cellulitis, superior ophthalmic vein thrombosis resulted from direct intraorbital injection of heroin.[53]
Eye Movements (strabismus, cranial neuropathies and nystagmus)
Eye movement abnormalities may occur with numerous drugs of abuse, including phencyclidine, lysergic acid diethylamide (LSD), and opioids.[54] Cocaine may induce or exacerbate myasthenia gravis.[55] Previous cases of acute esotropia following heroin withdrawal have been described.[56] Heroin detoxification was found to lead to a trend toward an esodeviation at distance in a prospective study of patients undergoing detoxification.[57]
Fetal alcohol syndrome is also associated with strabismus, as well as with prolonged saccadic reaction times, saccadic direction errors, and decreased saccadic velocity, suggestive of frontal lobe dysfunction.[17,58] Strabismus is common with infantile exposure to other drugs of abuse as well, and has been reported in 14% of infants of opiate-dependent mothers, more than 10 times that of the general population.[59]
Severe malnutrition leading to thiamine deficiency, seen in some chronic alcoholics and post-bariatric surgery patients, can lead to Wernicke’s encephalopathy. The classic clinical triad of Wernicke’s encephalopathy is ophthalmoplegia, ataxia, and confusion, but this triad is rarely complete in patients with Wernicke’s. MRI findings include symmetric T2 hyperintensities and contrast enhancement in the mammillary bodies, dorsal medial thalamic nuclei, tectal plate, and periaqueductal grey areas. [Figure 3] Wernicke’s can lead to extraocular motility disturbances including cranial nerve palsies, vertical gaze palsies, and nystagmus.[60]
Figure 3.
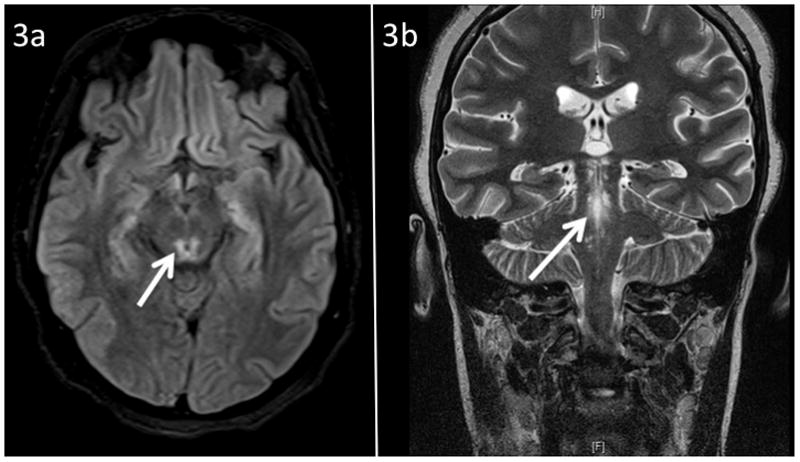
MRI findings in Wernicke syndrome, a) FLAIR axial imaging demonstrating hyperintensity of periaqueductal grey area (arrow), b) T2 coronal imaging demonstrating hyperintensity of periaqueductal grey area (arrow).
The cranial nerves themselves are rarely affected in isolation by substance abuse. A case of isolated bilateral sixth nerve palsy presumed to be from MDMA abuse was attributed to the interaction of the drug with serotonin receptors in the sixth nerves.[61] Sixth nerve palsy may accompany papilledema following the intake of any drug which raises intracranial pressure, as seen, for example, in a case of of ethylene glycol ingestion.[62]
Nystagmus is common with many drugs of abuse, including phencyclidine, opiates, marijuana, and barbituates. In utero exposure of the developing fetus to benzodiazepines and opiates can lead to a fine horizontal pendular nystagmus. The nystagmus can be associated with the development of a neonatal abstinence syndrome that is severe enough to require treatment.[42,63]
Central nervous system
Hallucinations are often a desired effect of numerous drugs of abuse, such as lysergic acid diethylamide (LSD), psilocybin, alcohol, barbituates, phencyclidine, MDMA, and marijuana. So-called flashbacks, or recurrent hallucinations, can occur years, or even decades, following even a single prior use of LSD.[64–66] An unusual side effect of LSD is palinopsia, prolonged or persistent afterimages.[64]
Similar to the effects of sympathomimetics causing vascular occlusive and hemorrhagic disease within the eye, these substances can affect the brain. Cocaine and methamphetamine use are a classic cause of ischemic stroke, intracerebral hemorrhage, and subarachnoid hemorrhage.[67,68] Small vessel vasculopathy affecting the central nervous system can be induced by amphetamines.[68] Therefore, any young adult presenting with an acute hemorrhagic or ischemic stroke should be screened for substance abuse. Cardiogenic emboli in patients with a history of intravenous drug use may be infectious (endocarditis) and result in strokes and associated visual symptoms. [Figure 4]
Figure 4.
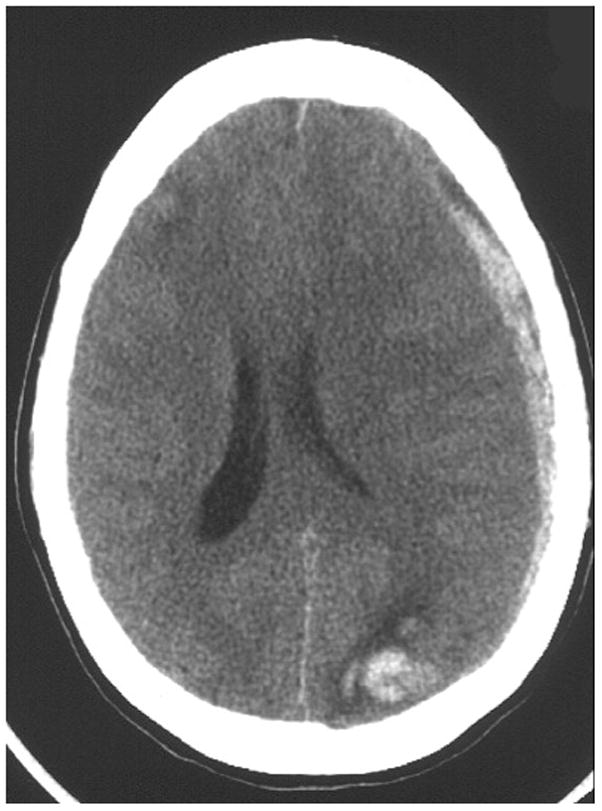
Axial CT scan of the brain without contrast demonstrating a left empyema with left hemorrhagic parietal-occipital infarction. Underlying etiology was an embolus in a patient with infectious endocarditis from intravenous heroin use. The brain lesion resulted in a right homonymous hemianopia.
Trauma
The use of alcohol and other substances of abuse is associated with a higher risk of penetrating ocular trauma and traumatic brain injury. Rates of drug and alcohol use among open globe injury patients range from 24–73%.[69]
The production of illicit drugs, in addition to the consumption, has proven hazardous to ocular health. A case series of four patients reported thermal and alkali burns from a “shake and bake” methamphetamine laboratory explosion.[70] A case series from the University of Iowa described the ocular thermal and alkalki injuries suffered by eight patients who presented to their burn care unit after methamphetamine production accidents.[71]
Conclusion
Drugs of abuse are an increasing cause of morbidity and mortality within our society, despite efforts to eliminate them from distribution and use. Novel materials are being used in the drug abuser’s arsenal of self-inflicted damage, and we must be able to recognize the effects of these compounds on the visual system. For patients with unusual presentations, maintaining a high suspicion of drug abuse is prudent.
Table.
Commonly abused drugs and frequent ophthalmic or visual manifestations
| Drug | Ocular/visual manifestation | |
|---|---|---|
|
| ||
| Alcohol | Dry Eye | |
| Fetal Alcohol Syndrome | ||
| Ocular Trauma | ||
| Diplopia | ||
| Wernicke’s Encephalopathy | ||
| Methanol | Toxic optic neuropathy | |
| Cocaine | Corneal anesthesia | |
| Keratitis | ||
| Corneal ulceration | ||
| Mydriasis | ||
| Retinal emboli | ||
| Retinal venous occlusion | ||
| Orbital disease | ||
| Stroke | ||
| Hallucinations | ||
| Methamphetamine | Keratitis | |
| Corneal ulceration | ||
| Mydriasis | ||
| Retinal venous occlusion | ||
| Intraretinal hemorrhage | ||
| Talc retinopathy | ||
| Stroke | ||
| Hallucinations | ||
| Heroin/Methadone | Talc retinopathy | |
| Endophthalmitis | ||
| Miosis | ||
| Marijuana | Conjunctival injection | |
| Decreased intraocular pressure | ||
| Nystagmus | ||
| Hallucinations | ||
| LSD | Mydriasis | |
| Hallucinations | ||
| Palinopsia | ||
| Phencyclidine | Decreased corneal reflex | |
| Diplopia | ||
| Nystagmus | ||
| “Bath Salts” | Mydriasis | |
| Alkyl nitrites | Maculopathy | |
| Barbiturates | Ptosis | |
| Diplopia | ||
| Nystagmus | ||
Key Points.
The abuse of drugs and alcohol can have serious consequences for the visual system.
Novel routes of administration and use of novel drugs of abuse can have consequences for the visual system that surprise the most astute clinicians if drug abuse is not suspected.
For patients who have unusual presentations, suspicion of drug abuse may be warranted.
Acknowledgments
This study was supported in part by a departmental grant (Department of Ophthalmology) from Research to Prevent Blindness, Inc., New York, by core grant P30-EY06360 (Department of Ophthalmology). Dr. Newman is a recipient of the Research to Prevent Blindness Lew R. Wasserman Merit Award.
Footnotes
The authors report no conflicts of interest.
References
- 1.Klein BE, Klein R. Lifestyle exposures and eye diseases in adults. Am J Ophthalmol. 2007;144:961–969. doi: 10.1016/j.ajo.2007.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moss SE, Klein R, Klein BEK. Prevalence of and risk factors for dry eye syndrome. Arch Ophthalmol. 2000;118:1264–1268. doi: 10.1001/archopht.118.9.1264. [DOI] [PubMed] [Google Scholar]
- 3**.Kim JH, Kim JH, Nam WH, et al. Oral alcohol administration disturbs tear film and ocular surface. Ophthalmology. 2012;119:965–971. doi: 10.1016/j.ophtha.2011.11.015. A case-control study of 35 heavy consumers of alcohol demonstrating altered tear film function and altered ocular surface structure compared to normal subjects. [DOI] [PubMed] [Google Scholar]
- 4.Cumurcu T, Gunduz A, Cumurcu BE, et al. The changes in tear film parameters and impression cytology in heavily drinking men. Cornea. 2013;32:237–241. doi: 10.1097/ICO.0b013e31825239d1. [DOI] [PubMed] [Google Scholar]
- 5.McLane NJ, Carroll DM. Ocular manifestations of drug abuse. Surv Ophthalmol. 1986;30:298–313. doi: 10.1016/0039-6257(86)90062-7. [DOI] [PubMed] [Google Scholar]
- 6.Alipour F, Hashemi H, Pirim N, Asghari H. Ocular manifestations of transconjunctival heroin abuse: A case report of an unusual route of substance abuse. Cornea. 2010;29:110–112. doi: 10.1097/ICO.0b013e3181a0a220. [DOI] [PubMed] [Google Scholar]
- 7.Poulsen EJ, Mannis MJ, Chang SD. Keratitis in methamphetamine abusers. Cornea. 1996;15:477–482. [PubMed] [Google Scholar]
- 8.Ghosheh FR, Ehlers JP, Ayres BD, et al. Corneal ulcers associated with aerosolized crack cocaine use. Cornea. 2007;26:966–969. doi: 10.1097/ICO.0b013e3180cfe716. [DOI] [PubMed] [Google Scholar]
- 9.Yagci A, Bozkurt B, Egrilmez S, et al. Topical anesthetic abuse keratopathy: A commonly overlooked health care problem. Cornea. 2011;30:571–575. doi: 10.1097/ico.0b013e3182000af9. [DOI] [PubMed] [Google Scholar]
- 10.Ansari H, Garibaldi DC, Jun AS. Anaesthetic abuse keratopathy as a manifestation of ocular Munchausen’s syndrome. Clin Exp Ophthalmol. 2006;34:81–92. doi: 10.1111/j.1442-9071.2006.01152.x. [DOI] [PubMed] [Google Scholar]
- 11.Hendershot AJ, Colling L, Mauger TF. Corneal anesthetic abuse from the use of topical benzonatate (Tessalon Perle) Cornea. 2011;30:1518–1519. doi: 10.1097/ICO.0b013e318207f229. [DOI] [PubMed] [Google Scholar]
- 12.Warrick BJ, Hill M, Hekman K, et al. A 9-state analysis of designer stimulant, “bath salt,” hospital visits reported to poison control centers. Ann Emerg Med. 2013 doi: 10.1016/j.annemergmed.2012.12.017. In press. [DOI] [PubMed] [Google Scholar]
- 13.Zhan G, Camras CB, Palmberg PF. Effects of marijuana on aqueous humor dynamics in a glaucoma patient. J Glaucoma. 2005;14:175–177. doi: 10.1097/01.ijg.0000151882.07232.1d. [DOI] [PubMed] [Google Scholar]
- 14.Jampel H. American Glaucoma Society position statement: Marijuana and the treatment of glaucoma. J Glaucoma. 2010;19:75–76. doi: 10.1097/IJG.0b013e3181d12e39. [DOI] [PubMed] [Google Scholar]
- 15.Trittibach P, Frueh BE, Goldblum D. Bilateral angle-closure glaucoma after combined consumption of “ecstasy” and marijuana. Am J Emerg Med. 2005;23:813–814. doi: 10.1016/j.ajem.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 16.Wang S, Wang JJ, Wong TY. Alcohol and eye diseases. Surv Ophthalmol. 2008;53:512–525. doi: 10.1016/j.survophthal.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 17.Bruce BB, Dean AL, Newman NJ, Biousse V. Neurologic and Ophthalmic Manifestations of Fetal Alcohol Syndrome. Rev Neurol Dis. 2009;6:13–20. [PubMed] [Google Scholar]
- 18.Clarke ME, Schloff S, Bothun ED. Triangular congenital cataract morphology associated with prenatal methamphetamine exposure. J AAPOS. 2009;13:408–409. doi: 10.1016/j.jaapos.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 19.Klein BE, Klein R, Linton KL, et al. Cigarette smoking and lens opacities: the Beaver Dam Eye Study. Am J Prev Med. 1993;9:27–30. [PubMed] [Google Scholar]
- 20.Galor A, Lee DJ. Effects of smoking on ocular health. Curr Opin Ophthalmol. 2011;22:477–482. doi: 10.1097/ICU.0b013e32834bbe7a. [DOI] [PubMed] [Google Scholar]
- 21.Atlee WE. Talc and cornstarch emboli in eyes of drug abusers. JAMA. 1972;219:49–51. [PubMed] [Google Scholar]
- 22.Kim RW, Juzych MS, Eliott D. Ocular manifestations of injection drug use. Infect Dis Clin N Am. 2002;16:607–622. doi: 10.1016/s0891-5520(02)00013-2. [DOI] [PubMed] [Google Scholar]
- 23.Zoumalan CI, Marmor MF. Revisiting talc retinopathy. Arch Ophthalmol. 2007;125:988. doi: 10.1001/archopht.125.7.988. [DOI] [PubMed] [Google Scholar]
- 24.Shah VA, Cassell M, Poulouse A, et al. Talc retinopathy. Ophthalmology. 2008;115:755–755. e2. doi: 10.1016/j.ophtha.2007.10.043. [DOI] [PubMed] [Google Scholar]
- 25.Kumar RL, Kaiser PK, Lee MS. Crystalline retinopathy from nasal ingestion of methamphetamine. Retina. 2005;26:823–824. doi: 10.1097/01.iae.0000244275.03588.ad. [DOI] [PubMed] [Google Scholar]
- 26.Ascaso FJ, Cruz N, Del Buey MA, Cristóbal JA. An unusual case of cocaine-induced maculopathy. Eur J Ophthalmol. 2009;19:880–882. doi: 10.1177/112067210901900533. [DOI] [PubMed] [Google Scholar]
- 27**.Davies AJ, Kelly SP, Naylor SG, et al. Adverse ophthalmic reaction in poppers users: case series of ‘poppers maculopathy’. Eye. 2012;26:1479–1486. doi: 10.1038/eye.2012.191. A case series of seven patients with maculopathy following poppers use is presented. In this paper it is stressed that thorough investigation of drug use history with foveal damage is necessary. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vignal-Clermont C, Audo I, Sahel JA, Paques M. Poppers-associated retinal toxicity. N Engl J Med. 2010;363:1583–1584. doi: 10.1056/NEJMc1005118. [DOI] [PubMed] [Google Scholar]
- 29.Audo I, Sanharawi ME, Vignal-Clermont C, et al. Foveal damage in habitual poppers users. Arch Ophthalmol. 2011;129:703–708. doi: 10.1001/archophthalmol.2011.6. [DOI] [PubMed] [Google Scholar]
- 30.Kim RW, Juzych SM, Eliott D. Ocular manifestations of injection drug use. Infect Dis Clin N Am. 2002;16:607–622. doi: 10.1016/s0891-5520(02)00013-2. [DOI] [PubMed] [Google Scholar]
- 31.Hazin R, Cadet JL, Kahook MY, Saed D. Ocular manifestations of crystal methamphetamine use. Neurotox Res. 2009;15:187–191. doi: 10.1007/s12640-009-9019-z. [DOI] [PubMed] [Google Scholar]
- 32.Kannan B, Balaji V, Kummararaj S, Govindarajan K. Cilioretinal artery occlusion following intranasal cocaine insufflations. Indian J Ophthalmol. 2011;59:388–389. doi: 10.4103/0301-4738.83619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rahman W, Thomas S, Wiselka M, Bibby K. Cocaine-induced chorioretinal infarction. Br J Ophthalmol. 2008;92:150–151. doi: 10.1136/bjo.2007.119248. [DOI] [PubMed] [Google Scholar]
- 34.Damasceno EF, Neto AM, Damasceno NAP, et al. Branch retinal vein occlusion and anabolic steroids abuse in young bodybuilders. Acta Ophthalmol. 2009;87:580–581. doi: 10.1111/j.1755-3768.2008.01238.x. [DOI] [PubMed] [Google Scholar]
- 35.Leung IY, Lai S, Ren S, et al. Early retinal vascular abnormalities in African-American cocaine users. Am J Ophthalmol. 2008;146:612–619. doi: 10.1016/j.ajo.2008.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cong R, Zhou B, Sun Q, et al. Smoking and risk of age-related macular degeneration: a meta-analysis. Ann Epidemiol. 2008;18:647–656. doi: 10.1016/j.annepidem.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 37.Chong EW, Kreis AJ, Wong TY, et al. Alcohol consumption and the risk of age-related macular degeneration: a systematic review and meta-analysis. Am J Ophthalmol. 2008;145:707–715. doi: 10.1016/j.ajo.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 38.Xu L, You QS, Jonas JB. Prevalence of alcohol consumption and risk of ocular diseases in a general population: the Beijing Eye Study. Ophthalmology. 2009;116:1872–1879. doi: 10.1016/j.ophtha.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 39.Adams MK, Chong EW, Williamson E, et al. 20/20 – Alcohol and age-related macular degeneration: the Melbourne Collaborative Cohort Study. Am J Epidemiol. 2012;176:289–298. doi: 10.1093/aje/kws004. [DOI] [PubMed] [Google Scholar]
- 40.Flanigan EY, Aros S, Bueno MF, et al. Eye malformations in children with heavy alcohol exposure in utero. J Pediatr. 2008;153:391–395. doi: 10.1016/j.jpeds.2008.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sanaei-Zadeh H, Zamani N, Shadnia S. Outcomes of visual disturbances after methanol poisoning. Clin Toxicol. 2011;49:102–107. doi: 10.3109/15563650.2011.556642. [DOI] [PubMed] [Google Scholar]
- 42.Hamilton R, McGlone L, MacKinnon JR, et al. Ophthalmic, clinical and visual electrophysiological findings in children born to mothers prescribed substitute methadone in pregnancy. Br J Ophthalmol. 2010;94:696–700. doi: 10.1136/bjo.2009.169284. [DOI] [PubMed] [Google Scholar]
- 43.Li JM, Rucker JC. Irreversible Optic Neuropathy in Wernicke encephalopathy and Leber hereditary optic neuropathy. J Neuro-ophthalmol. 2010;30:49–53. doi: 10.1097/WNO.0b013e3181ce80c6. [DOI] [PubMed] [Google Scholar]
- 44.Kulkarni S, Lee AG, Holstein SA, Warner JE. You are what you eat. Surv Ophthalmol. 2005;50:389–393. doi: 10.1016/j.survophthal.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 45.Longmuir R, Lee AG, Rouleau J. Visual loss due to Wernicke syndrome following gastric bypass. Semin Ophthalmol. 2007;22:13–19. doi: 10.1080/08820530601182733. [DOI] [PubMed] [Google Scholar]
- 46.Cooke CA, Hicks E, Page AB, et al. An atypical presentation of Wernicke’s encephalopathy in an 11-year-old child. Eye. 2006;20:1418–1420. doi: 10.1038/sj.eye.6702275. [DOI] [PubMed] [Google Scholar]
- 47.Phillips PH. Toxic and Deficiency Optic Neuropathies. In: Miller NR, Newman NJ, editors. Clinical Neuro-ophthalmology. 6. Philadelphia: Lippincott Williams & Wilkins; 2005. pp. 458–459. [Google Scholar]
- 48.The Cuba Neuropathy Field Investigation Team. Epidemic optic neuropathy in Cuba: Clinical characterization and risk factors. N Engl J Med. 1995;333:1176–1182. doi: 10.1056/NEJM199511023331803. [DOI] [PubMed] [Google Scholar]
- 49.Kirkman MA, Yu-Wai-Man P, Korsten A, et al. Gene-environment interactions in Leber hereditary optic neuropathy. Brain. 2009;132:2317–2326. doi: 10.1093/brain/awp158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ayala C, Watkins L, Deschler DG. Tension orbital pneumocele secondary to nasal obstruction from cocaine abuse: a case report. Otolaryngol Head Neck Surg. 2002;127:572–574. doi: 10.1067/mhn.2002.129810. [DOI] [PubMed] [Google Scholar]
- 51.Leibovitch I, Khoramian D, Goldberg RA. Severe destructive sinusitis and orbital apex syndrome as a complication of intranasal cocaine abuse. Am J Emerg Med. 2006;24:499–501. doi: 10.1016/j.ajem.2005.11.019. [DOI] [PubMed] [Google Scholar]
- 52.Shen CC, Silver AL, O’Donnell TJ, et al. Optic neuropathy caused by naso-orbital mass in chronic intranasal cocaine abuse. J Neuro-ophthalmol. 2009;29:50–53. doi: 10.1097/WNO.0b013e3181989adb. [DOI] [PubMed] [Google Scholar]
- 53.Ghosheh FR, Kathuria SS. Intraorbital heroin injection resulting in orbital cellulitis and superior ophthalmic vein thrombosis. Ophthal Plast Reconstr Surg. 2006;22:473–475. doi: 10.1097/01.iop.0000248991.71690.eb. [DOI] [PubMed] [Google Scholar]
- 54.Firth A. Ocular effects of criminal drug use. Can J Ophthalmol. 2006;41:140–143. doi: 10.1139/i06-902. [DOI] [PubMed] [Google Scholar]
- 55.Valmaggia C, Gottlob I. Cocaine abuse, generalized myasthenia, complete external ophthalmoplegia, and pseudotonic pupil. Strabismus. 2001;9:9–12. doi: 10.1076/stra.9.1.9.706. [DOI] [PubMed] [Google Scholar]
- 56.Firth AY. Heroin and diplopia. Addiction. 2005;100:46–50. doi: 10.1111/j.1360-0443.2005.00915.x. [DOI] [PubMed] [Google Scholar]
- 57.Firth AY, Pulling S, Carr MP, Beaini AY. Orthoptic status before and immediately after heroin detoxification. Br J Ophhtalmol. 2004;88:1186–1190. doi: 10.1136/bjo.2003.032334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Green CR, Munoz DP, Nikkel SM, Reynolds JN. Deficits in eye movement control in children with fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2007;31:500–511. doi: 10.1111/j.1530-0277.2006.00335.x. [DOI] [PubMed] [Google Scholar]
- 59.Gill AC, Oei J, Lewis NL, et al. Strabismus in infants of opiate-dependent mothers. Acta Paediatr. 2003;92:379–385. [PubMed] [Google Scholar]
- 60.Kumar N. Acute and Subacute Encephalopathies: Deficiency States (Nutritional) Semin Neurol. 2011;31:169–183. doi: 10.1055/s-0031-1277986. [DOI] [PubMed] [Google Scholar]
- 61.Schroeder B, Brieden S. Bilateral sixth nerve palsy associated with MDMA (“Ecstasy”) abuse. Am J Ophthalmol. 2000;129:408–409. doi: 10.1016/s0002-9394(99)00354-2. [DOI] [PubMed] [Google Scholar]
- 62.Delany C, Jay WM. Papilledema and abducens nerve palsy following ethylene glycol ingestion. Semin Ophthalmol. 2004;19:72–74. doi: 10.1080/08820530490882733. [DOI] [PubMed] [Google Scholar]
- 63.Mulvihill AO, Cackett PD, George ND, Fleck BW. Nystagmus secondary to drug exposure in utero. Br J Ophthalmol. 2007;91:613–615. doi: 10.1136/bjo.2006.105569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sunness JS. Persistent afterimages (palinopsia) and photophobia in a patient with a history of LSD use. Retina. 2004;24:805. doi: 10.1097/00006982-200410000-00022. [DOI] [PubMed] [Google Scholar]
- 65.Kawasaki A, Purvin V. Persistent palinopsia following ingestion of lysergic acid diethylamide (LSD) Arch Ophthalmol. 1996;114:47–50. doi: 10.1001/archopht.1996.01100130045007. [DOI] [PubMed] [Google Scholar]
- 66.Levi L, Miller NR. Visual illusions associated with previous drug abuse. J Clin Neuro-ophthalmol. 1990;10:103–110. [PubMed] [Google Scholar]
- 67.Toossi S, Hess CP, Hills NK, Josephson SA. Neurovascular complications of cocaine use and a tertiary stroke center. J Stroke Cerebrovasc Dis. 2010;19:273–278. doi: 10.1016/j.jstrokecerebrovasdis.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 68.Ho EL, Josephson SA, Lee HS, Smith WS. Cerebrovascular complications of methamphetamine abuse. Neurocrit Care. 2009;10:295–305. doi: 10.1007/s12028-008-9177-5. [DOI] [PubMed] [Google Scholar]
- 69.Rahman I, Maino A, Devadason D, Leatherbarrow B. Open globe injuries: factors predictive of poor outcome. Eye. 2006;20:1336–1341. doi: 10.1038/sj.eye.6702099. [DOI] [PubMed] [Google Scholar]
- 70.Chan AY, Storck SA, Stone DU. Ocular injuries from shake and bake methamphetamine labs. J Okla State Med Assoc. 2011;104:409–412. [PubMed] [Google Scholar]
- 71.Charukamnoetkanok P, Wagoner MD. Facial and ocular injuries associated with methamphetamine production accidents. Am J Ophthalmol. 2004;138:875–876. doi: 10.1016/j.ajo.2004.05.056. [DOI] [PubMed] [Google Scholar]


