Abstract
Background
Debate exists regarding which endpoints most sensitively reflect day-to-day variation in chronic obstructive pulmonary disease (COPD) symptoms and are most useful in clinical practice to predict COPD exacerbations. We hypothesized that short-acting β2-agonist (SABA) reliever use would predict short- and long-term exacerbation risk in COPD patients.
Methods
We performed a retrospective analysis of data from a study (ClinicalTrials.gov registration: NCT00419744) comparing budesonide/formoterol 320/9 μg with formoterol 9 μg (both twice daily) in patients with moderate-to-very-severe COPD; reliever salbutamol 90 μg was provided. First occurrence of reliever use >4 (low), >10 (medium), and >20 (high) inhalations/day was assessed as a predictor of short-term (3-week) exacerbation risk. Mean daily reliever use in the week preceding the 2-month visit was investigated as a predictor of the long-term (10-month) exacerbation risk, using intervals of 2–5, 6–9, and ≥10 inhalations/day.
Results
Overall, 810 patients were included (61 % male; mean age 63.2 years; post-bronchodilator forced expiratory volume in 1 s 37.7 % of predicted). First occurrence of low, medium, or high reliever use was predictive of an exacerbation within the following 3 weeks; exacerbation risk increased significantly with increasing reliever use. Mean reliever use over 1 week was predictive of long-term exacerbation risk. Patients with mean use of 2–5, 6–9, and ≥10 inhalations/day exhibited 21 %, 67 %, and 135 % higher exacerbation rates, respectively, in the following 10 months, compared with <2 inhalations/day. Budesonide/formoterol was associated with lower short- and long-term exacerbation risk than formoterol in all reliever-use groups.
Conclusions
SABA reliever use is a predictor of short- and long-term exacerbation risk in moderate-to-very-severe COPD patients with a history of exacerbations receiving budesonide/formoterol or formoterol.
Keywords: COPD, Budesonide/formoterol, Exacerbation, Reliever medication, Predictor
Background
The global burden of symptoms in patients with chronic obstructive pulmonary disease (COPD) is high [1]. Under-recognition and under-treatment of COPD can have a significant impact on day-to-day activities and quality of life for patients, resulting in avoidable disease burden, activity impairment [1], and hospitalization risk [2].
It remains unclear which endpoints most sensitively reflect the day-to-day variation in symptoms in patients with COPD. Ideally, outcomes in COPD trials should reflect the real-world behavior of patients as well as the potential of treatment to influence both current disease state and future risk [3]. The forced expiratory volume in 1 s (FEV1) is a reproducible and responsive measurement that reflects aspects of the pathophysiology characterizing COPD. However, FEV1 impairment is only weakly related to overall patient well-being [4, 5], and other endpoints are needed that are easier to obtain in routine clinical practice and that reflect the day-to-day impact of COPD on the patient, in order to guide treatment decisions [6, 7]. New symptom-based questionnaires address this need, but they may neglect the important information patients report during routine office visits or in surveys accompanied by objective measures of symptom impact [8]. An example of this type of information is the frequency with which patients use reliever medication to control symptoms experienced in the real world.
In asthma trials, the use of short-acting β2-agonists (SABA) as reliever medication to decrease symptoms has been accepted as a measure of day-to-day asthma control [9]. This outcome is included in widely used asthma control questionnaires as a surrogate measure of symptom frequency and a reflection of treatment efficacy [10, 11]. Until relatively recently, SABAs were prescribed to COPD patients as background maintenance therapy 1–4 times per day and, traditionally, their frequency of use has not been considered to reflect the variability of symptoms and patients’ responses. With the widespread use of long-acting inhaled bronchodilators as first-line maintenance medication in COPD [12], SABAs are now seen as reliever medication in COPD [13]. Thus, by analogy with asthma, reliever use in COPD may be a sensitive marker of symptom variability [14] and of the extent to which an intervention improves symptom control. Conversely, since increased reliever use is an indicator of sub-optimal control in asthma, it could have a similar significance in COPD, reflecting worsening symptom control or an impending exacerbation. Evidence already exists to show that, compared with as-needed SABA use, regular SABA use is not associated with additional benefit across a range of clinical and functional outcomes in COPD [15].
We hypothesized that more SABA taken as reliever medication would predict increased short- and long-term risk of exacerbations in patients with COPD, and tested our hypothesis retrospectively by analyzing reliever use collected by electronic diary recording in patients who participated in a clinical trial of budesonide/formoterol (BUD/FORM) or formoterol (FORM) [16].
Methods
This retrospective analysis was undertaken on data collected in a study (ClinicalTrials.gov registration: NCT00419744) comparing fixed-dose combination BUD/FORM with FORM monotherapy, in which electronic diaries were used to record as-needed SABA reliever use administered using a pressurized metered-dose inhaler (pMDI) [16]. The study evaluated the effect of maintenance treatment with BUD/FORM or FORM on COPD exacerbations, defined as COPD worsening leading to oral corticosteroid therapy and/or hospitalization, in patients with moderate-to-very-severe COPD [12] who had a history of one or more exacerbations in the previous year. The study protocol was approved by an institutional review board for each of the clinical sites and written informed consent was obtained from patients or guardians before any study procedures were initiated. The study was conducted in accordance with the Declaration of Helsinki, Good Clinical Practice and applicable local regulations.
Study design and methods
The full methodology of this trial has been published previously [16]. Following a 2-week run-in period, current COPD medications were discontinued and eligible patients who met inclusion criteria were randomized to twice-daily BUD/FORM pMDI 160/4.5 μg × 2 inhalations (320/9 μg), BUD/FORM pMDI 80/4.5 μg × 2 inhalations (160/9 μg), or formoterol dry powder inhaler (DPI) 4.5 μg × 2 inhalations (9 μg). Patients were provided with the SABA salbutamol (albuterol) 90 μg × 2 inhalations via a pMDI to administer as reliever medication throughout the study. Medications were not escalated during the trial; however, medications allowed during a COPD exacerbation were oral corticosteroids, single injection parenteral corticosteroids (not depot formulations), xanthines, and inhaled or nebulized ipratropium or β2-agonists. Symptoms, and morning and evening peak expiratory flow, were measured daily prior to the administration of the morning and evening dose of study medication. Use of reliever medication was recorded in the morning and evening as number of inhalations.
Patients receiving twice-daily BUD/FORM pMDI 160/4.5 μg × 2 inhalations (320/9 μg) and formoterol dry powder inhaler (DPI) 4.5 μg × 2 inhalations (9 μg) were included in the present analysis. Patients receiving the lower dose of BUD/FORM were excluded from the present analysis as it is not a registered product.
Statistical analysis
We assessed two risk profiles for SABA use and exacerbations.
Short-term exacerbation risk (21 days)
The short-term exacerbation risk was evaluated as the relationship between a patient reaching a certain threshold of reliever use in a single day and the probability of having an exacerbation in the next 21 days. This short-term risk was described by analysis of time to first exacerbation after the first time a patient used more than the specified number of SABA inhalations. This was presented descriptively using Kaplan-Meier graphs for reliever use thresholds of >4 (low use), >10 (medium use), and >20 (high use) inhalations in a single day for both treatment groups, with ≥0 inhalations (i.e. all patients) as a reference group. Both the reliever use thresholds and 21-day time period were defined empirically; the reliever use thresholds broadly reflected use in clinical practice based on the authors’ clinical expertise, and the time period considered both the longest period of time following deviation from daily reliever use and the known evolution of COPD exacerbations [17]. The data were analyzed using a log-rank test; p-values were calculated for the comparisons of all groups and then individually against the reference group.
Long-term exacerbation risk (months 3–12)
The long-term exacerbation risk was evaluated as the relationship between mean reliever use during stable treatment in the week before the 2-month study visit and probability of an exacerbation occurring in months 3–12 of the study. This risk was described by analysis of the number of exacerbations for mean reliever use intervals (2–5, 6–9, and ≥10 inhalations/day: low, medium, and high reliever use, respectively), compared with mean reliever use <2 inhalations per day (infrequent). The long-term mean reliever use intervals were defined empirically to broadly reflect mean reliever use over a week in clinical practice based on the authors’ clinical expertise, and a 10-month time period was chosen to allow the longest time period between the 2-month visit and study end. We also determined long-term 10-month risk by analyzing the exacerbation rates by treatment in patients: i) reaching mean reliever use thresholds of ≥2, ≥6, and ≥10 inhalations per day; and ii) with mean number of inhalations (< or ≥) in a range from zero to 12 inhalations/day.
The analyses were performed using a Poisson regression analysis, adjusted for over-dispersion, with treatment as factor included for the first analysis. The analyses were not adjusted for additional covariates. Both analyses were presented with rates and ratios with 95 % confidence intervals (CI) and p-values.
The distribution of the frequency of patients’ reliever use on each of the study treatments was analyzed using Fisher’s exact test.
Results
In total, 810 patients with moderate-to-very-severe COPD were included: 61 % male; mean age (range) 63.2 (40–87) years; mean (±SD) post-bronchodilator FEV1 37.7 (12.1) % of predicted; 27.8 % of patients received inhaled corticosteroids before study run-in (BUD/FORM: 26.5 %, FORM: 29.0 %). Demographic and baseline clinical characteristics of patients included in this post-hoc analysis generally were similar across treatment groups (Table 1) [16]. Data were available for 807 patients in the short-term exacerbation risk analysis: 692, 351, and 91 patients reached the low (>4 inhalations/day), medium (>10 inhalations/day), and high (>20 inhalations/day) reliever use thresholds, respectively (patient n values are cumulative, i.e. all patients in the >20 subgroup are also in the >4 and >10 subgroups). In addition, data were available for 674 patients in the long-term exacerbation risk analysis: 234, 155, and 92 patients reached the mean number of inhalations/day for inclusion in the low (2–5 inhalations/day), medium (6–9 inhalations/day), and high (>10 inhalations/day) reliever use subgroups, respectively.
Table 1.
Baseline characteristics of patients included in this post-hoc analysis of the Sharafkhaneh et al. study [16]
| BUD/FORM | FORM | Total | |
|---|---|---|---|
| (n = 407) | (n = 403) | (n = 810) | |
| Male, n (%) | 262 (64.4) | 229 (56.8) | 491 (60.6) |
| Age, years (range) | 63.8 (40–86) | 62.5 (40–87) | 63.2 (40–87) |
| Pre-BD FEV1, % predicted | 33.0 (10.5) | 32.4 (10.1) | 32.7 (10.3) |
| Post-BD FEV1, % predicted | 37.9 (11.8) | 37.5 (12.4) | 37.7 (12.1) |
| Pre-BD FEV1/FVC ratio, % | 45.9 (11.3) | 46.1 (11.1) | 46.0 (11.2) |
| Smoking history | |||
| Current smokers, n (%) | 138 (33.9) | 154 (38.2) | 292 (36.0) |
| Pack-years (range) | 52.6 (10–200) | 52.2 (10–258) | 52.4 (10–258) |
| Most common COPD medications before run-in, n (%) | |||
| β2-adrenergic agonists (SABA/LABA) | 320 (78.6) | 321 (79.7) | 641 (79.1) |
| Adrenergics/other drugs for obstructive airway diseases | 198 (48.6) | 196 (48.6) | 394 (48.6) |
| Long-acting muscarinic antagonist | 123 (30.2) | 109 (27.0) | 232 (28.6) |
| Inhaled corticosteroids | 108 (26.5) | 117 (29.0) | 225 (27.8) |
| No. of exacerbations in the past 12 months, n (%) | |||
| 1 | 244 (60.0) | 234 (58.1) | 478 (59.0) |
| 2 | 95 (23.3) | 99 (24.6) | 194 (24.0) |
| 3 | 36 (8.8) | 38 (9.4) | 74 (9.1) |
| 4 | 22 (5.4) | 19 (4.7) | 41 (5.1) |
| ≥ 5 | 10 (2.5) | 13 (3.2) | 23 (2.8) |
| Mean reliever use, inhalations/daya | 5.8 (4.6) | 6.0 (4.5) | 5.9 (4.6) |
| Patients taking ICS at baseline, n % | 108 (26.5) | 117 (29.0) | 225 (2.8) |
Data shown as mean (±SD), unless otherwise stated. Current smokers include habitual and occasional smokers
BD bronchodilator, BUD budesonide, FEV 1 forced expiratory volume in 1 s, FORM formoterol, FVC forced vital capacity, ICS inhaled corticosteroid, LABA long-acting β2-agonists, SABA short-acting β2-agonists, SD standard deviation
aBaseline: 2-week run-in period
Short-term exacerbation risk (21 days)
The first occurrence of reliever use beyond a certain threshold, i.e. low, medium, or high reliever use in a single day, was predictive of an exacerbation within the following 3 weeks (Fig. 1). The time to first exacerbation differed between the reliever use groups for both BUD/FORM and FORM (p < 0.001; Fig. 1). In addition, there was a significant increase in the risk of an exacerbation for patients who had medium and high reliever use compared with the reference group (≥0 inhalations/day) for both the BUD/FORM (p = 0.002 and <0.0001, respectively) and FORM (p = 0.02 and <0.0001, respectively) groups.
Fig. 1.
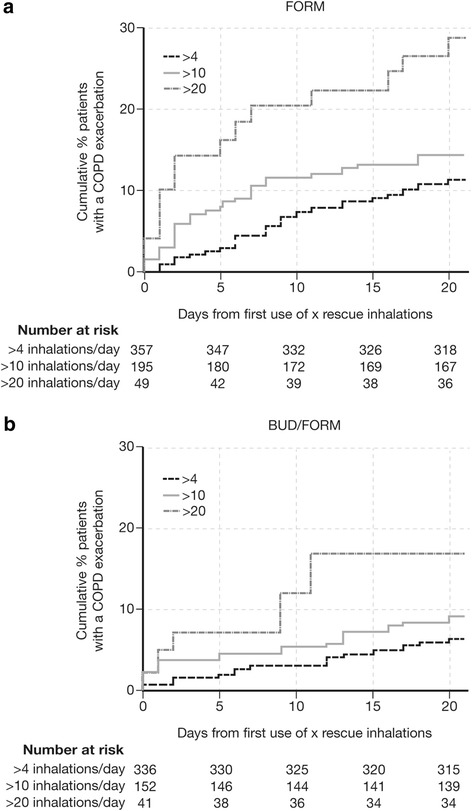
Short-term (days 0–21) exacerbation risk. Kaplan-Meier plot of patients with occurrence of an exacerbation after they used for the first time >4, >10, or >20 inhalations of salbutamol per day in a) FORM and b) BUD/FORM treatment groups. Data for 16 patients are missing from baseline to day 0. BUD budesonide, COPD chronic obstructive pulmonary disease, FORM formoterol
Long-term exacerbation risk (months 3–12)
Mean daily reliever use over 1 week preceding the 2-month visit was identified as a predictor of the long-term 10-month (i.e. months 3–12) probability of an exacerbation. Patients with a mean use of 2–5, 6–9, and ≥10 inhalations exhibited 21 %, 67 %, and 135 %, respectively, greater exacerbation rates in the following 10 months relative to patients with a mean use of <2 inhalations/day; the difference being significant for the 6–9 and ≥10 groups (Table 2). For both treatments, long-term 10-month exacerbation rates were greater whenever mean reliever use exceeded thresholds, in the range from 0–12 inhalations/day in the week preceding the 2-month visit (Fig. 2). In addition, there were more infrequent reliever users in the BUD/FORM group than FORM group and, consequently, fewer patients with ≥2, ≥6, or ≥10 inhalations of reliever medication per day; this was most apparent at higher reliever use (Table 3). Patients randomized to BUD/FORM had a lower risk of exacerbations than the FORM group (Fig. 3). Patients with higher mean daily reliever use in the week preceding the 2-month visit had a higher rate of exacerbations during months 3–12 than those with lower mean daily reliever use, over a range of cut-points (Table 2 and Fig. 3). This was true for both BUD/FORM and FORM recipients.
Table 2.
Long-term exacerbation rate. Long-term (months 3–12) exacerbation rate in all patients, based on cut-points of ≥2, ≥6, and ≥10 reliever inhalations/day in the week preceding the 2-month visit
| Mean reliever use (inhalations/day) | Exacerbation ratea or ratio | 95 % CI | P-value |
|---|---|---|---|
| <2 | 0.596 | (0.470, 0.756) | |
| 2–5 | 0.724 | (0.594, 0.882) | |
| 6–9 | 0.996 | (0.806, 1.230) | |
| ≥10 | 1.403 | (1.115, 1.766) | |
| 2–5 versus <2 | 1.214 | (0.891, 1.654) | 0.22 |
| 6–9 versus <2 | 1.670 | (1.215, 2.296) | 0.0016 |
| ≥10 versus <2 | 2.353 | (1.687, 3.282) | <0.001 |
CI confidence interval
aRates are normalized for 10 months and expressed as events per year. Analysis adjusted for treatment effects
Fig. 2.
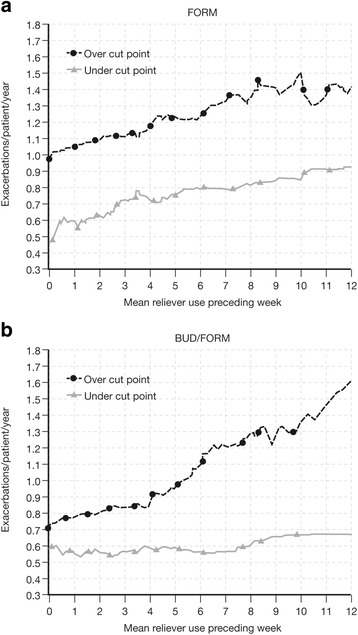
Long-term (months 3–12) exacerbation rate by reliever use thresholds. Long-term (months 3–12) exacerbation rates for patients receiving a) FORM and b) BUD/FORM with a mean number of inhalations less than, and greater than or equal to, reliever use in the range from zero to 12 inhalations/day in the week preceding the 2-month visit. BUD budesonide, FORM formoterol
Table 3.
Number of patients reporting <2, ≥2, ≥6, or ≥10 inhalations/day in the week preceding the 2-month visit by treatment group
| Mean reliever use (inhalations/day) | BUD/FORM (n = 349) | FORM (n = 325) | P valuea |
|---|---|---|---|
| Patients with cut-point inhalations/day, n (%) | |||
| <2 | 114 (32.7) | 79 (24.3) | 0.017 |
| ≥2 | 235 (67.3) | 246 (75.7) | 0.017 |
| ≥6 | 111 (31.8) | 136 (41.8) | 0.007 |
| ≥10 | 27 (7.7) | 65 (20.0) | <0.001 |
Patient n values are cumulative (i.e. all patients in the ≥10 group are also in the ≥2 and ≥6 groups) and represent the number of patients remaining in the analysis for the week before the 2-month visit
BUD budesonide, FORM formoterol
aP-values are for the analysis of BUD/FORM versus FORM
Fig. 3.
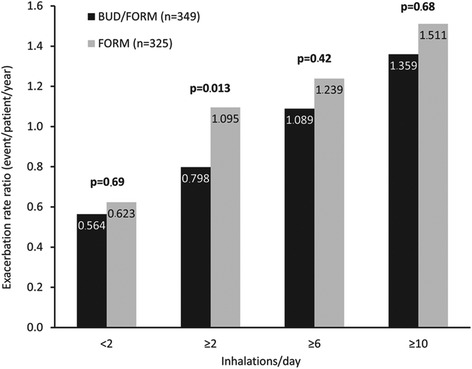
Long-term (months 3–12) exacerbation rate by treatment group. Long-term (months 3–12) exacerbation rate by treatment group, for patients reporting <2, ≥2, ≥6, or ≥10 inhalations/day in the week preceding the 2-month visit. P-values are for the analysis of BUD/FORM versus FORM. BUD budesonide, FORM formoterol
Discussion
In this analysis, the daily number of inhalations of SABA needed for relief of symptoms was a predictor for future exacerbations in patients with COPD and a history of exacerbations in a study of combination BUD/FORM as maintenance therapy. SABA use predicted both short- and long-term risk of exacerbations. High SABA use in a single day was a predictor of the short-term probability of exacerbation in the following 21 days, whereas the average daily SABA use over 1 week of stable maintenance treatment was a strong predictor of an exacerbation in the following 10 months. This was true for patients taking BUD/FORM and FORM alone; however, patients treated with BUD/FORM had a lower short- and long-term risk of exacerbation compared with FORM monotherapy.
Although a relationship between as-needed SABA use and exacerbations in patients with COPD has long been suspected by clinicians, to our knowledge this is the first systematic investigation demonstrating this relationship. Indeed, although an increasing number of studies testing the efficacy of long-acting bronchodilators have used this index as an objective measure of the impact of treatment and a surrogate marker for breakthrough symptoms [18–21], none have specifically analyzed the data in relation to the predictive capacity of as-needed SABA use in this context. In this analysis of data from a randomized, controlled study, we showed that as-needed SABA use in COPD patients can predict exacerbation risk over the short (≤21 days) and long (≤10 months) term, if patients are taking appropriate doses of long-acting β2-agonist either alone or in combination with an inhaled corticosteroid. Our data suggest that for COPD, as in asthma [22], reliever use may be implemented as an important parameter for disease stability and future exacerbation risk. If our results are confirmed in other studies, it may be useful for clinicians to monitor patterns of reliever medication use so that they can identify patients at risk for an exacerbation, take steps to prevent the occurrence of a COPD exacerbation and ensure that when these events do occur, they are more rapidly identified and effectively treated. Similarly, patients may be educated to recognize increasing reliever use as a warning sign for an exacerbation and to take steps early to prevent further deterioration.
While we consider these findings to be robust for this group of patients with moderate-to-very-severe COPD and a history of exacerbations, further studies in patients with milder disease are needed before the predictive capacity of the use of SABA as a reliever can be generalized to all symptomatic patients with COPD. Ideally, for implementation in clinical trials, the findings should be confirmed in other large datasets in which similar instructions have been given to participants, with records of SABA use kept in a comparable way throughout the study. In addition, further studies would enable assessment of the degree of individual variability and clarify the ideal reliever use cut-points in predicting COPD exacerbations. We wished to validate our findings in a larger study population receiving similar BUD/FORM and FORM doses and recording reliever use, using data from five randomized controlled trials of BUD/FORM [17, 23–26], including the use of BUD/FORM in combination with a long-acting muscarinic antagonist [17]. However, methodological differences between the studies, specifically a mix of methodology (paper versus electronic diaries, different study duration and devices), meant that this analysis could not be undertaken in a suitably rigorous manner.
The reliever use categories in the present analysis were defined empirically to broadly reflect use in clinical practice based on the authors’ clinical expertise, and future analyses should validate reliever use categories to identify specific thresholds that may predict future exacerbations. However, even in the absence of further validation, measures of SABA reliever use could be incorporated into risk prediction tools for exacerbations to initiate early treatment and potentially mitigate an upcoming exacerbation. We have previously developed a risk prediction tool (SCOPEX) based on a range of demographic and baseline parameters from a pooled database of BUD/FORM COPD studies; data from this tool showed that higher mean daily reliever use was a dominant predictor of a COPD exacerbation in the next 6 months [27]. In agreement with the current analysis, the risk prediction tool showed that FORM was associated with a higher exacerbation risk than BUD/FORM.
As with the original study [16], it is unclear whether discontinuation of inhaled corticosteroids in those patients who received FORM alone contributed to worse exacerbation outcomes compared with those receiving BUD/FORM. Long-acting β2-agonist monotherapy is not recommended in patients with severe-to-very-severe COPD, limiting the interpretability of our data in the FORM only group. We note, however, a trend to undertake studies assessing bronchodilators alone even in severe/Group D patients, so the issue of a non-inhaled corticosteroid approach to Group D – especially those who do not exacerbate frequently – is still being discussed. In addition, we cannot verify whether the number of daily inhalations or occasions of SABA use as reliever medication was exactly as patients recorded in their electronic diaries. However, reliever use was recorded twice daily and entries were permitted only in specific time windows (morning and evening), which prevented retrospective recordings. It is well known that paper diaries may permit retrospective and fictitious entries, and even electronic diaries may suffer from recall errors [28, 29]. Optimally, electronic inhaler adherence monitoring should be used to confirm these records, but the data we analyzed were taken from a study in which this was not undertaken.
Conclusions
SABA reliever use was a predictor of short- (≤21 days) and long-term (≤10 months) risk of exacerbations in patients with moderate-to-very-severe COPD and a history of exacerbations receiving combination BUD/FORM or FORM monotherapy. Mean reliever use over 1 week predicted exacerbation risk, and this risk increased further with a higher number of inhalations of reliever/day. These data suggest that SABA use is an important and practical outcome for assessing both current control and future risk in patients with COPD. Additional clinical trials and effectiveness studies of COPD patients with different disease severity and exacerbation history are needed to validate SABA use as a predictor of exacerbations in both clinical trials and in clinical practice.
Acknowledgements
AstraZeneca funded the analysis and were responsible for data collection and analysis of this post-hoc analysis. The authors thank Malin Fagerås and Magnus Lindberg of AstraZeneca R&D, Mölndal, Sweden, and Thomas Similowski of Service de Pneumologie et Réanimation Médicale, Paris, France, for their assistance with the development of this manuscript. Anna Mett and Shaun Foley of inScience Communications, Springer Healthcare, provided medical writing assistance, funded by AstraZeneca.
Abbreviations
- BUD/FORM
Budesonide/formoterol
- CI
Confidence interval
- COPD
Chronic obstructive pulmonary disease
- DPI
Dry powder inhaler
- FEV1
Forced expiratory volume in 1 s
- FORM
Formoterol
- pMDI
Pressurized metered-dose inhaler
- SABA
Short-acting β2-agonist
- SD
Standard deviation
Footnotes
Competing interests
CRJ is an advisory board member for AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Merck Limited, and Novartis, and a consultant for AstraZeneca, Chiesi, GlaxoSmithKline, and Pieris. Educational presentations have been developed for AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, and Novartis, with honoraria paid to CRJ or her institution. Lectures have been presented on behalf of AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Hunter Immunology, and Novartis. Support for travel to meetings has been provided by AstraZeneca and Boehringer Ingelheim.
The University of Groningen has received honoraria for DSP advising on the conduct and analysis of clinical trial data from AstraZeneca, Nycomed, and Teva, as well as for lectures at meetings supported by AstraZeneca, Chiesi, GlaxoSmithKline, Nycomed, and Teva. The University of Groningen has received money for research by unrestricted educational grants from AstraZeneca and Chiesi. AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, and Nycomed have provided support for travel to meetings.
ARA is a consultant and speaker for AstraZeneca, Bayer Pharma, Boehringer Ingelheim, Dey Pharma, GlaxoSmithKline, and Pfizer, and has received honoraria from these companies. Educational presentations have been developed for AstraZeneca, Bayer Pharma, Boehringer Ingelheim, Dey Pharma, GSK, and Pfizer. The University of Texas Health Science Center at San Antonio has received money for research to perform clinical trials. Support for travel to meetings has also been provided by AstraZeneca.
BJM is an advisory board member for Aerocrine, AstraZeneca, Forest, Boehringer Ingelheim, CSL Bering, Forest, Novartis, and Theravance and a consultant for Astellas, Forest, and Chiesi. Clinical trial data have been reviewed for Spiration, with grants received and controlled by National Jewish Health from AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Forest, MedImmune, Nabi, National Institutes of Health, Pfizer, and Sunovian. Lectures have been presented on behalf of Boehringer Ingelheim and GlaxoSmithKline. Educational presentations and programs have been developed (Carden Jennings, Cleveland Clinic, Consensus Medical, Foundation for Improving Patient Outcomes, Hybrid Communications, Integrity, Intellisphere, Medscape, National Jewish Health, Projects in Knowledge, SPIRE, Synapse, and WebMD). Royalties have been received from Up-To-Date. BJM has been a speaker for educational programs at Abbott, the American Academy of Family Practice, the American College of Chest Physicians, and the American Thoracic Society. Support for travel to meetings has also been provided by AstraZeneca.
GSE is an ex-employee of AstraZeneca. He is a consultant for Novartis, ALK, and MVIC and has been a consultant for Almirall.
SP is an ex-employee of AstraZeneca and own stocks within the company.
PMC is a board member for Boehringer Ingelheim, the Department of Health Respiratory Programme Board, GlaxoSmithKline, and Nycomed. He has been a consultant for Novartis and provided expert testimony for Forest. PMC has received honoraria for advising on the conduct and analysis of clinical trial data from AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Novartis, and Nycomed. He has also spoken at meetings supported by these companies. Support for travel to meetings has been provided by AstraZeneca.
This study and the analysis performed for this manuscript were funded by AstraZeneca.
Authors’ contributions
CRJ, DSP, ARA, BJM, SP, GSE, and PMC all contributed to data-interpretation, and conceiving, writing, and revising the manuscript. SP was responsible for statistical analyses. CRJ, the corresponding author, had full access to all the data in the study and had final responsibility for the decision to submit for publication. All authors approved the final draft of the manuscript.
Contributor Information
Christine R. Jenkins, Phone: +61-2-9767 6712, Email: christine.jenkins@sydney.edu.au
Dirkje S. Postma, Email: d.s.postma@umcg.nl
Antonio R. Anzueto, Email: anzueto@uthscsa.edu
Barry J. Make, Email: makeb@njhealth.org
Stefan Peterson, Email: stefan.peterson@statmind.se.
Göran Eriksson, Email: goran.eriksson@med.lu.se.
Peter M. Calverley, Email: pmacal@liverpool.ac.uk
References
- 1.Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yeatts KB, Lippmann SJ, Waller AE, Hassmiller Lich K, Travers D, Weinberger M, et al. Population-based burden of COPD-related visits in the ED: return ED visits, hospital admissions, and comorbidity risks. Chest. 2013;144(3):784–793. doi: 10.1378/chest.12-1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Postma D, Anzueto A, Calverley P, Jenkins C, Make BJ, Sciurba FC, et al. A new perspective on optimal care for patients with COPD. Prim Care Respir J. 2011;20(2):205–209. doi: 10.4104/pcrj.2011.00041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jones PW. Health status measurement in chronic obstructive pulmonary disease. Thorax. 2001;56(11):880–887. doi: 10.1136/thorax.56.11.880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Westwood M, Bourbeau J, Jones PW, Cerulli A, Capkun-Niggli G, Worthy G. Relationship between FEV1 change and patient-reported outcomes in randomised trials of inhaled bronchodilators for stable COPD: a systematic review. Respir Res. 2011;12:40. doi: 10.1186/1465-9921-12-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A self-complete measure of health status for chronic airflow limitation. The St. George’s Respiratory Questionnaire. Am Rev Respir Dis. 1992;145(6):1321–1327. doi: 10.1164/ajrccm/145.6.1321. [DOI] [PubMed] [Google Scholar]
- 7.Cazzola M, MacNee W, Martinez FJ, Rabe KF, Franciosi LG, Barnes PJ, et al. Outcomes for COPD pharmacological trials: from lung function to biomarkers. Eur Respir J. 2008;31(2):416–469. doi: 10.1183/09031936.00099306. [DOI] [PubMed] [Google Scholar]
- 8.Landis SH, Muellerova H, Mannino DM, Menezes AM, Han MK, van der Molen T, et al. Continuing to confront COPD international patient survey: methods, COPD prevalence, and disease burden in 2012–2013. Int J Chron Obstruct Pulmon Dis. 2014;9:597–611. doi: 10.2147/COPD.S61854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bateman ED, Reddel HK, Eriksson G, Peterson S, Ostlund O, Sears MR, Jenkins C, Humbert M, Buhl R, Harrison TW. Overall asthma control: the relationship between current control and future risk. J Allergy Clin Immunol. 2010;125(3):600–8. doi: 10.1016/j.jaci.2009.11.033. [DOI] [PubMed] [Google Scholar]
- 10.Melosini L, Dente FL, Bacci E, Bartoli ML, Cianchetti S, Costa F, et al. Asthma control test (ACT): comparison with clinical, functional, and biological markers of asthma control. J Asthma. 2012;49(3):317–323. doi: 10.3109/02770903.2012.661008. [DOI] [PubMed] [Google Scholar]
- 11.Revicki D, Weiss KB. Clinical assessment of asthma symptom control: review of current assessment instruments. J Asthma. 2006;43(7):481–487. doi: 10.1080/02770900600619618. [DOI] [PubMed] [Google Scholar]
- 12.Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease. Updated 2014 [http://www.goldcopd.com/]
- 13.Vestbo J, Hurd SS, Agusti AG, Jones PW, Vogelmeier C, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347–365. doi: 10.1164/rccm.201204-0596PP. [DOI] [PubMed] [Google Scholar]
- 14.Kessler R, Partridge MR, Miravitlles M, Cazzola M, Vogelmeier C, Leynaud D, et al. Symptom variability in patients with severe COPD: a pan-European cross-sectional study. Eur Respir J. 2011;37(2):264–272. doi: 10.1183/09031936.00051110. [DOI] [PubMed] [Google Scholar]
- 15.Cook D, Guyatt G, Wong E, Goldstein R, Bedard M, Austin P, et al. Regular versus as-needed short-acting inhaled beta-agonist therapy for chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;163(1):85–90. doi: 10.1164/ajrccm.163.1.2004214. [DOI] [PubMed] [Google Scholar]
- 16.Sharafkhaneh A, Southard JG, Goldman M, Uryniak T, Martin UJ. Effect of budesonide/formoterol pMDI on COPD exacerbations: a double-blind, randomized study. Respir Med. 2012;106(2):257–268. doi: 10.1016/j.rmed.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 17.Welte T, Miravitlles M, Hernandez P, Eriksson G, Peterson S, Polanowski T, et al. Efficacy and tolerability of budesonide/formoterol added to tiotropium in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2009;180(8):741–750. doi: 10.1164/rccm.200904-0492OC. [DOI] [PubMed] [Google Scholar]
- 18.Donohue JF, Fogarty C, Lotvall J, Mahler DA, Worth H, Yorgancioglu A, et al. Once-daily bronchodilators for chronic obstructive pulmonary disease: indacaterol versus tiotropium. Am J Respir Crit Care Med. 2010;182(2):155–162. doi: 10.1164/rccm.200910-1500OC. [DOI] [PubMed] [Google Scholar]
- 19.D’Urzo A, Ferguson GT, van Noord JA, Hirata K, Martin C, Horton R, et al. Efficacy and safety of once-daily NVA237 in patients with moderate-to-severe COPD: the GLOW1 trial. Respir Res. 2011;12:156. doi: 10.1186/1465-9921-12-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fuhr R, Magnussen H, Sarem K, Llovera AR, Kirsten AM, Falques M, et al. Efficacy of aclidinium bromide 400 mug twice daily compared with placebo and tiotropium in patients with moderate to severe COPD. Chest. 2012;141(3):745–752. doi: 10.1378/chest.11-0406. [DOI] [PubMed] [Google Scholar]
- 21.Vogelmeier C, Hederer B, Glaab T, Schmidt H, Rutten-van Molken MP, Beeh KM, et al. Tiotropium versus salmeterol for the prevention of exacerbations of COPD. N Engl J Med. 2011;364(12):1093–1103. doi: 10.1056/NEJMoa1008378. [DOI] [PubMed] [Google Scholar]
- 22.Buhl R, Kuna P, Peters MJ, Andersson TL, Naya IP, Peterson S, et al. The effect of budesonide/formoterol maintenance and reliever therapy on the risk of severe asthma exacerbations following episodes of high reliever use: an exploratory analysis of two randomised, controlled studies with comparisons to standard therapy. Respir Res. 2012;13:59. doi: 10.1186/1465-9921-13-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tashkin DP, Rennard SI, Martin P, Ramachandran S, Martin UJ, Silkoff PE, et al. Efficacy and safety of budesonide and formoterol in one pressurized metered-dose inhaler in patients with moderate to very severe chronic obstructive pulmonary disease: results of a 6-month randomized clinical trial. Drugs. 2008;68(14):1975–2000. doi: 10.2165/00003495-200868140-00004. [DOI] [PubMed] [Google Scholar]
- 24.Rennard SI, Tashkin DP, McElhattan J, Goldman M, Ramachandran S, Martin UJ, et al. Efficacy and tolerability of budesonide/formoterol in one hydrofluoroalkane pressurized metered-dose inhaler in patients with chronic obstructive pulmonary disease: results from a 1-year randomized controlled clinical trial. Drugs. 2009;69(5):549–565. doi: 10.2165/00003495-200969050-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Calverley PM, Boonsawat W, Cseke Z, Zhong N, Peterson S, Olsson H. Maintenance therapy with budesonide and formoterol in chronic obstructive pulmonary disease. Eur Respir J. 2003;22(6):912–919. doi: 10.1183/09031936.03.00027003. [DOI] [PubMed] [Google Scholar]
- 26.Szafranski W, Cukier A, Ramirez A, Menga G, Sansores R, Nahabedian S, et al. Efficacy and safety of budesonide/formoterol in the management of chronic obstructive pulmonary disease. Eur Respir J. 2003;21(1):74–81. doi: 10.1183/09031936.03.00031402. [DOI] [PubMed] [Google Scholar]
- 27.Make BJ, Eriksson GS, Calverley PM, Jenkins C, Postma DS, Peterson S, et al. A score to predict short-term risk of COPD exacerbations (SCOPEX) Int J Chron Obstruct Pulmon Dis. 2015;10:201–209. doi: 10.2147/COPD.S69589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Juniper EF, Bousquet J, Abetz L, Bateman ED. Identifying’well-controlled’ and ’not well-controlled’ asthma using the Asthma Control Questionnaire. Respir Med. 2006;100(4):616–21. [DOI] [PubMed]
- 29.Juniper EF, Langlands JM, Juniper BA. Patients may respond differently to paper and electronic versions of the same questionnaires. Respir Med. 2009;103(6):932–934. doi: 10.1016/j.rmed.2008.10.019. [DOI] [PubMed] [Google Scholar]


