Abstract
Call lights are prevalent in inpatient healthcare facilities across the nation. While call light use directly influences the delivery of nursing care, there remain significant gaps both in research and technology that can impact the quality of care and patient satisfaction. This study examines the perception of nurses and patients on the use of a new call communication solution, Eloquence™, in the acute care inpatient setting. Eighteen patients were recruited for the study and participated in individual semi-structured interviews during their hospital stay. Eighteen nurses were recruited and participated in focus groups for this study. Qualitative descriptive methods were used to analyze the data. Results revealed themes of usability, improved communication, and suggestions for improvement to the alpha prototype design. After a demonstration of the use and capability of Eloquence™, nurse and patient participants found Eloquence™ as a welcomed advancement in nurse call technology that has the potential to improve workflow and patient outcomes. In addition, the participants also proposed ideas on how to further develop the technology to improve its use.
Keywords: call lights, nurse call systems, health information technology, communication technology, patient communication, nurse communication
Introduction
Most inpatient healthcare facilities are equipped with call light technology as a way for patients to communicate with their care providers. Only recently were studies undertaken to demonstrate how this technology affects patient care. Using ethnographic methods, Deitrick et al.1 revealed concerns regarding call light use and found that staff were unclear on whose job it was to answer the call light with some staff members viewing call lights as an interruption to their work flow and delivery of patient care. Patients' comments revealed issues concerning long wait times in getting their calls answered, inconsistencies with the response time, lack of follow through with requests, and differing lengths of time to fulfill their requests. These findings are concerning given that call light use is important in providing patient-centered care and it is one way patients can exercise control over their care.1,2
Call light technology serve as a means of communication for patients to their care providers that are outside of the patient's room. This technology is a direct link to getting their needs met and the care provided by nurses. Management of call light activity is largely driven by the nursing staff.2 However, a study in four U.S. hospitals revealed varied opinions among staff regarding patient's use of call lights.3 While 49% of the nurses viewed call lights as a patient-safety issue, 53% viewed answering call lights as an interruption to critical aspects of their role, and only 52% thought that these calls required nursing care by nurses as opposed to support staff. The discordance between the patient expectations and staff expectations on call light use is important as call light response times have been shown to be a good predictor of key elements of patient satisfaction4-6 . In addition, the timeliness of answered call lights may impact patient safety and quality of patient care.
Nurse's timeliness in responding to call lights, for example, has been correlated to lower nosocomial pressure ulcers7 . Studies have shown a correlation between call light response times and patient falls in acute care settings. A more recent multihospital study by Tzeng et al.8 showed a relationship between faster call light response time and decreased fall rates and injurious fall rates. Extrinsic fall risk factors related to call lights include lack of clarity in setting priorities in patient care, staff perception of call light usage, and delayed response times in answering call lights9 . More in-depth studies are needed to capture the specific problems with nurse call light technology as it relates to patient safety, quality of care, and patient satisfaction on patient quality and safety outcomes.
Given the implication that nurses' responsiveness to call lights impacts patient care quality and patient safety, changes in practice regarding call light use such as hourly rounding have been used to optimize call light response times.10,11 However, these measures can be a costly and an inefficient way of addressing patients' needs. To this extent, there has been an increased impetus to advance nurse call light systems to keep up with the advances in commercial communications technology and health information technology. Recent advances in call light systems include the Vocera Communications System, which provides caregivers the capability of remote, hands-free verbal communication with patients and other staff. Evaluation of this device shows more efficient workflow, time savings, and staff satisfaction by bypassing overhead pagers and attendants who would then forward calls to caregivers.12, 13 In its report The Future of Nursing Leading Change, Advancing Health, the Institute of Medicine suggested engaging nurses in the development of medical and health devices.14 In a survey, front line staff using the Vocera Communication System found it to be an improvement in their provision of care.12
A new advancement in call light technology is the Eloquence™ call light system (Eloquence Communications; Ann Arbor, Michigan). Unlike other call light technology that uses Voice over Internet Protocol (VoIP), which is limited in use for patients who have language barriers (e.g. postoperative laryngectomy patients, patients with weak voices, patients with limited English proficiency), Eloquence™ uses icons and phrases to allow patients to specify their needs when making a nurse call request, thus informing the nursing staff the reason for their call upon the initiation of the call light request. Eloquence™ uses three main components: a touch screen device at the patient's bedside (Figure 1, 2); a hand held device for nursing personnel; and a gateway display at each nursing station that displays which patient rooms have an activated call light (Figure 3), the amount of time that has lapsed since the initiation of the call light, the personnel that has been assigned to the request. Eloquence™ also has an automated routing algorithm that routes each request with an assigned priority ranking and subsequent escalation routing to the post appropriate personnel. For instance, a request for water would be routed to unlicensed personnel, while a request for medication would be routed to a registered nurse.
Figure 1.
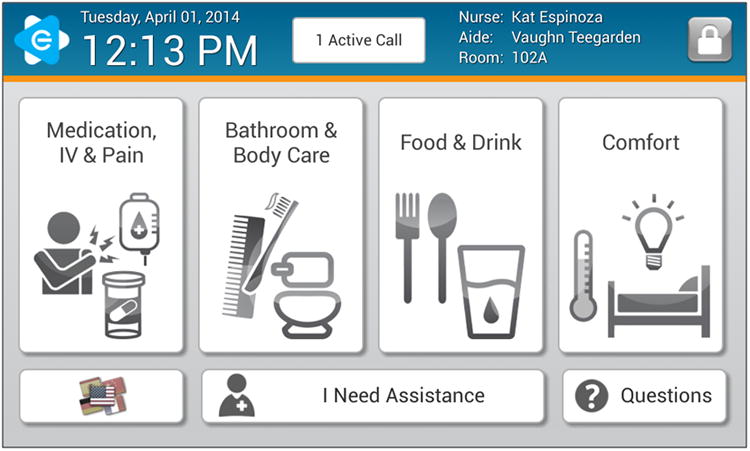
Eloquence Bedside Patient Tablet Interface, example 1.
Figure 2.
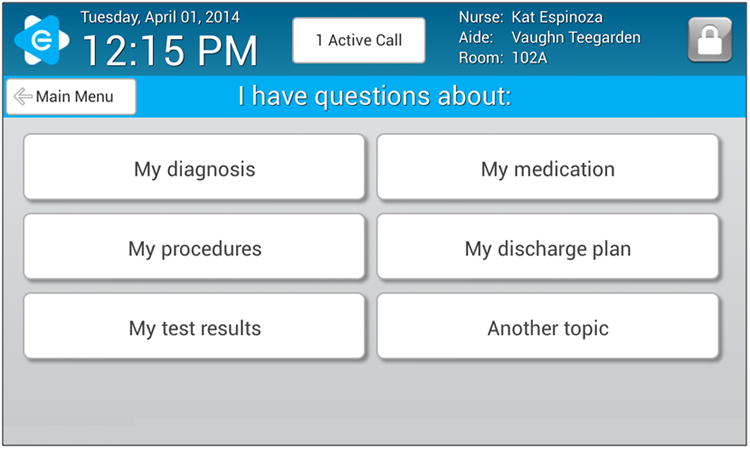
Eloquence Bedside Patient Tablet Interface, example 2.
Figure 3.
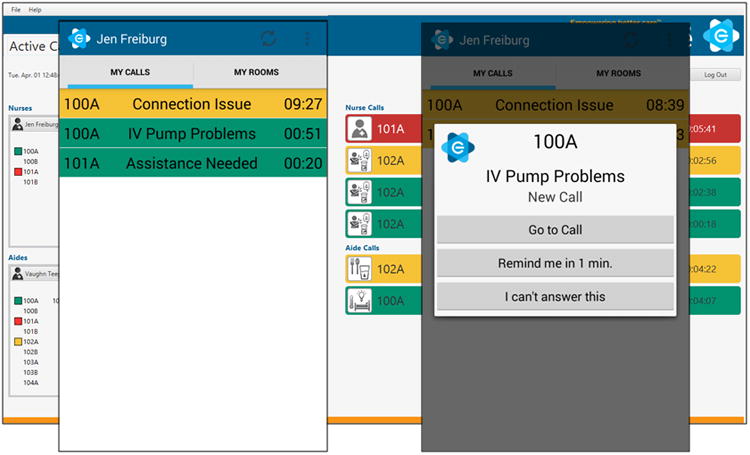
Eloquence Gateway Display for Nursing Station.
Given the rise of new information and technology with regards to call lights, this study evaluates the perceptions of patients on a new innovation in call light systems using a prototype of Eloquence™. At the time of this study, Eloquence™ has not been installed or used in any health care setting. Research reported in this study is supported by National Institutes of Health, Minorities, and Health Disparities of the National Institutes of Health under grant number 1R41MD006149-01. The purpose of this study was to examine the usefulness, effectiveness, and appropriateness of Eloquence™ in acute inpatient noncritical care units as perceived by patients and nurses.
Methods
Qualitative data were collected from semi-structured focus groups of registered nurses (RNs), and individual patient interviews from six adult acute care inpatient units in a large academic medical center in Michigan (Table 1) from October 2011 to January 2012. Approval from the institutional review board at the study site was obtained. Eligible nurse participants were approached with the assistance of nurse managers from each study unit, who provided a list of eligible nurses who met the inclusion criteria (Table 2). Potential nurse participants were invited via e-mail to join the focus groups, and were assured that collected data would be kept confidential and not affect their employment evaluation. Nurse participants were assured confidentiality and anonymity. Once a mutually agreed upon time was established, nurse focus groups were conducted, separate from patient participant interviews. The focus groups were audio taped for accuracy and the recording was transcribed. Informed consent was obtained from all the nurse participants.
Table 1. Participating Inpatient Units.
| Specialty | No. of beds | No. of licensed nursing personnel |
|---|---|---|
| Neurology and Neurosurgical | 26 | 79 Registered Nurses |
| Cardio and thoracic intermediate | 44 | 85 Registered Nurses |
| Orthopedic trauma | 32 | 48 Registered Nurses |
| Rehabilitation | 32 | 57 Registered Nurses |
| General Medicine | 32 | 49 Registered Nurses |
| Oncology and gynecology | 32 | 57 Registered Nurses |
Table 2. Participant Inclusion and Exclusion Criteria.
| Participant Group | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| RN |
|
1. Works as a contingent or travel nurse |
| Patients |
|
|
Potential patient participants, identified by the nurse manager based on established exclusion and inclusion criteria, were approached in-person by study personnel on study unit floors for their willingness to participate via assistance from nurse managers. Likewise, all patient participants were assured confidentiality and that their participation would not affect their care in any capacity. Patient participant interviews were conducted individually and lasted for approximately one hour. Similar to the nurse focus groups, interviews were audio taped for accuracy and were transcribed. Informed consent was obtained from all patient participants. Each of the nurse and patient participants received a gift card as a token of appreciation for their time and participation. Qualitative data analysis utilized a descriptive approach.
Qualitative data analysis was conducted via a descriptive approach15 to explore nurse and patient participants' perspectives with regards to the prototype Eloquence™. A brief video demonstrating the technology capabilities was shown prior to providing an opportunity for participants to simulate the use of the device as they would use it in their health care settings using various scenarios. Opportunities were also given to ask any questions they might have about the device. Interview guides were then used to elicit information about the participants' perceptions of Eloquence ™. All participants were then asked to respond to the following questions:
Please share with us your first reaction to Eloquence ™
What do you like about Eloquence ™?
What do you not like about Eloquence ™?
Would you make any changes to Eloquence ™? If so what would they be?
For each of you, how well would this system work for you? Why or why not?
Data obtained from focus groups and individual interviews were transcribed and coded using a constant comparative method15 . A constant comparative method is an iterative process that is used to derive a coding process that in turn provides a framework that is used to develop minor and major themes. Coding was independently identified and was then compared until common themes emerged. Deduction was utilized as a collaborative process in the final decisions of major and minor themes and is reflected in the data analysis. Three independent research team members further determined credibility of the data and its analysis. Research team members responsible for data collection and analysis didnot have any financial interests in the development or marketing of the Eloquence™ call light system.
Results
Eighteen nurses and eighteen patients participated for this study from six units (Nurse participant and patient participant demographics are found in Table 3 and 4, respectively). Qualitative data analysis resulted in five major themes from the nurse focus groups: Nurse Perspectives, Usability, Communication, Technological Concerns, and Suggestions for Future Use. These themes are described in the following sections.
Table 3. Nurse Participant Demographics.
| Characteristic | Total (n=18) | Percentage |
|---|---|---|
| Age | ||
| 21-45 Years of age | 12 | 66.7% |
| 46-60 Years of age | 6 | 33.3% |
| Sex | ||
| Female | 17 | 94.4% |
| Male | 1 | 5.6% |
| Ethnicity | ||
| White/Non-Hispanic | 14 | 77.8% |
| Black | 1 | 5.6% |
| Asian | 3 | 16.7% |
| Average Years Working as a Nurse | 8.43 (SD 9.6) |
Table 4. Patient Participant Demographics.
| Characteristic | Total (n=18) | Percentage |
|---|---|---|
| Age | ||
| 21-55 Years of age | 5 | 27.8% |
| 56-75 Years of age | 12 | 66.7% |
| >75 Years of age | 1 | 5.6% |
| Sex | ||
| Female | 8 | 44.4% |
| Male | 10 | 55.6% |
| Ethnicity | 49 Registered Nurses | |
| White/Non-Hispanic | 14 | 77.8% |
| Black | 1 | 5.6% |
| Average Length of Stay | 6.06 (days) |
Nurse Perspectives
Nurse's initial impressions of the new prototype Eloquence™ nurse call solution were positive. Nurses stated that they felt that Eloquence™ would enhance efficiency, including time management, addressing patient needs, and communication. The nurse participants also added that this enhanced efficiency would benefit patient care because patient needs could be clearly defined and addressed appropriately (“…I thought the idea was great to cut down the running back and forth because you already have an idea of what's needed”). In addition, nurses remarked that the increase in technology was welcomed:
“High technology…I liked it“
“…It is very comprehensive”
“…easy to learn” and “user friendly”
In particular, nurses discussed the device's usability, communication, prioritization, and patient needs. Usability of the device for example, proved to be an important aspect of Eloquence™ from the nursing perspective.
Usability
The usability of the Eloquence™ device, defined as how capable the device could be used in the clinical setting, was important to nurses and proved to be an important aspect of the Eloquence™ nurse call solution. Nurses commented that they appreciated the user friendliness of the system:
“I love how its user friendly”
“It is a great system, easy and embraces new technology.”
“Portability…able to speak to your patients without going to the room.”
Nurses found that its portability along with the use of the latest technology contributed to the user-friendliness of the device. They found it easy to use and applicable to the care that they provide.
In addition, the usability of Eloquence™ lent itself to anticipated improved communication between nurses as care providers and patients.
Communication
Communication between nurses and their patients is important, and aids in the delivery of patient care and fulfillment of their needs. Improved communication from Eloquence™ technology was two -fold: communication between nurses, and communication between nurses and patients. Nurses stated that they appreciated the ability to communicate and call other nurses from their handheld device, “I like that nurses can call each other and call patients.” Nurses thought that the Eloquence™ device would also aid in patient communication, “Being able to communicate quickly with patients” and “the better communication…I try to anticipate patient needs now.” The ability to communicate more effectively contributed to the ability to prioritize not only nursing care and patient requests, but also addressed time management.
Nurses' thought that the Eloquence™ system could provide prioritization in their clinical practice with better time management. Nurses for example, commented:
“I like that we can prioritize the tasks”
“Improve time management of staff members”
In addition, nurses liked that Eloquence™ could program which care provider type and specific nursing personnel should receive each patient request, “Eloquence™ chooses whether an RN or tech should get the call.” Eloquence™ not only helped with time management and allocation of tasks, but also allowed nurses to prioritize patient care:
“Helps me to prioritize…I like the color coordination and prioritizing”
“Nurses will be able to prioritize workload with patients and go to the patents who need help first.”
Prioritizing also led to anticipating patient needs:
“I can know what my patient needs before I enter the room”
“Triage the calls; know exactly what each patient wants.”
Thus, time management and prioritization of calls emerged as a much needed of the call light technolgy. Addressing patient needs also contributed to the appeal of Eloquence™.
Nurses' discussed the importance of addressing patients' needs, and commented on how it compared to the current call light system currently in use in their institution, which at the time of our study was conducted was the Rauland IV Responder (Rauland-Borg; Mount Prospect, Illinois). With Eloquence™, nurses stated that they liked that they could see patient requests:
“I like that one can see patient requests before I enter the room to prioritize tasks”
“That you can see what the patient may need, medications versus water, internet use…”
The ability to visually see patient requests led to “knowing exactly what their [patient] needs are” thus, further contributing to better time management and prioritization of patient needs. Usability, communication, the ability to prioritize tasks, time management and addressing patient needs, all led nurses to conclude that Eloquence™ could be a more efficient call light system:
“…At least with this system you have a checklist of to do's”
“ I know which light to go to firstand I could transfer or ask for help in a few clicks”
“I love how much it will improve service, response time, time management, and setting priorities”
Nurses however, reported technological concerns as well.
Technological Concerns
Nurses reported concerns with regards to the technological aspects of Eloquence™. For example, nurses wondered about the ability for people with limited technology skills to understand how to use Eloquence™:
“…I wonder if this will be difficult for some non-tech savvy nurse to master”
“[I'm] concerned about elderly patients [or] older nurses [with using the device]”).
Nurses reported concerns about the Eloquence™ user interface. Some nurses for example, thought the size of the Eloquence™ device was too large and that perhaps, there were too many options:
“Large box…screen not easy to use”
“…Large, needs to be mounted”
“I dislike that the patients are given options regarding dressing changes that might be too detailed an option”
“…It's an ‘I want box’ and people are going to ask for more now”
User interface was also discussed in terms of the physical device of Eloquence™:
“Touch screens are very finicky”
“…protective shield for phone and clip and able to get replacements right away if needed.”
Nurses were also concerned with the user interface in terms of user abilities; citing concerns regarding potential difficulty for vulnerable populations, nurses reported:
“[Eloquence™] is high tech, would' need a tutorial especially for the elderly”
“Technology can be a negative factor…especially the elderly who are not technology savvy, hearing impaired, [or] with neurologic problems…”
“[I'm] concerned how it will accommodate the elderly, paraplegics, people with handicaps/disabilities”
“It would work well for me, but not for all of our population on a rehab floor, many spinal cord patients…”
“Too high tech for elderly or mentally delayed”
Despite technological and user interface concerns, nurses also provided suggestions for logistical additions to the Eloquence™ nurse call solution.
Suggestions for Future Use
Nurses discussed logistical additions to the Eloquence™ call light system from two different perspectives: professional nursing perspective, and from the patient perspective. From their professional nursing experiences, nurses suggested the following:
“A direct connect to charge nurse and other staff”
“Ability to page MD”
“Need to be able to see home screen and the whole unit's needs so we can see requests of other patients”
Nurses also provided suggestions advocating for patients' usage of the Eloquence™ device as well. In their professional nursing experience with patient care, nurses suggested the following:
“Add option for patients to order snacks directly to dietary”
“Attach [Eloquence™ device] to bed, add other languages, head phone attachments, tutorial…”
“[Patient] Ability to change languages”
“Information is stored and protected…Have a personal pin so others can't view personal information without patients knowledge”
“And music for patients – several stations”
Thus, nurses' suggestions from their professional perspective and advocating for patient use, reflected concern for the implementation of Eloquence™ and providing feedback on how to improve Eloquence™. In turn, these reflections provided worthy suggestions for improvement of its use. Nurses stated confidently that with trial and error, Eloquence™ could become a critical tool in patient care.
Qualitative data analysis revealed four major themes from the patient participant interviews: Patient Participant Perspectives, Patient Usability, Patient Communication, and Suggestions for Future Eloquence™ Use. These themes are described in the following sections.
Patient Participant Perspectives
Parallel to the nurses' first impressions of the Eloquence™ nurse call solution, patient participants also found the Eloquence™ bedside tablet impressive. Patients stated:
“I was very impressed…It makes such sense to be specific in ones needs while a patient”
“I thought the idea is very solid, first reaction was very positive”
“It is perfect and simple to use, saves time for everyone”
Patients also reported positive experiences regarding the usability of the Eloquence™ device.
Patient Usability
Patients reported experiences with regards to the usability of the Eloquence™ system. Patients remarked that Eloquence™:
“…would work very well, system appears to be easy to learn and use”
“It is perfect and simple to use”
“Very easy to use…Pictures for choices, simple buttons…”
Usability of the Eloquence™ device was important for patients, and led to further discussion regarding the communication to providers by the bedside tablet.
Patient Communication
Patients described communication through the Eloquence™ bedside tablet as appropriate and easy, and this was especially true in regards to their communication with their care providers. For example, patients described that the communication Eloquence™ enabled for their care providers was positive:
“Being able to tell nursing/doctor staff exactly what I need,”
“ The ability to give info to nurses before they get to you”
“The fact that one can be specific on needs is really nice. I like that the staff can come to the room prepared with what the patient needs/wants. It saves a lot of time”
“It allows me to identify exactly what I need”
Communication proved to be important for patients; affirming that clear communication by patients with their assigned nursing personnel is both desired and needed. In addition, patients offered suggestions for future Eloquence™ programming.
Patient Suggestions for Future Eloquence™ Use
The majority of patients had no suggestions for future Eloquence™ design and engineering. However, some patients made some suggestions regarding the size of the bedside tablet; voicing common concerns parallel to that of the nurse participants. For example, some patients were concerned with the size of Eloquence™ bedside tablet:
“Make sure the final product is a correct size and easy to find in the middle of the night” “[Make] the urgent button larger and more prominent”
“[Be] careful in the final design, letter size, sensitivity…”
“Maybe a little smaller in size”
Thus patients' comments regarding the size of the bedside tablet were consistent, questioning the accessibility of the device for its future use.
Discussion
Assessing nurse call light technology and how it impacts both communication between patients and their caregivers is important because it is a direct communicative link to patient needs and patient care provided by nurses.1 Current literature regarding call light communication presents discordance between patient perceptions and staff expectations for care responsibilities.3 In accordance with the Institute of Medicine12 suggestion for the development of innovative health technologies such as call light systems in collaboration with nurses, this study evaluated an alpha-prototype of Eloquence™ from a nurse and patient perspective.
Nurses and patients initial impressions to the Eloquence™ alpha-bedside tablet and nurse call system were positive, similar to the positive response of front-line staff to another advancement to call light technology.12 Both patients and nurses appreciated the “usability” of the prototype of Eloquence™ that was demonstrated; but defined the term differently. According to nurses, usability lent itself to the effectiveness of anticipated effective communication between nurses, and between nurses and patients. Usability from the patients' perspective was derived from more physical aspects of the prototype itself (i.e., easy to learn, pictures for choices, simple buttons for use, and the content displayed on the bedside tablet). Usability of the nurse call system for patients, specifically the bedside device, however, is very important as the bedside device (a tablet for Eloquence™) allows patients to initiate the nurse-patient interaction and is key to their perception of feeling safe and having control of getting their needs met.1,2 Parallel to the usability of the device, both nurses and patients commented on the potential improvement of communication via the Eloquence™ prototype.
Both nurses and patients commented positively on the potential improvement of communication between themselves via the Eloquence™ prototype. For nurses, communication could be enhanced via Eloquence™ for two main reasons: 1) Eloquence™ could provide opportunities to communicate quickly with patients, and that this communication would lead to anticipating patient needs; and 2) that nurses could communicate with other nurse's directly through Eloquence™ and that this communication would also be beneficial because it could bolster efficient time management. Indeed, the nurses' perceptions of the usability and helpfulness of the Eloquence™ nurse call solution is important as they are accountable for addressing needs of their patients w.2 The advancement of nurse call systems is particularly important given the correlation of nursing care to patient outcomes, such as pressure ulcers7 and patient falls8 , to the responsiveness of the nurses to call lights. Engaging nurses in the development of health technology, as the IOM recommends14 , might lead to improvement of the development and commercialization of evidence-based solutions that effectively improve the delivery of patient care and, in turn, patient outcomes. In addition, such technology, when incorporating the feedback and evaluation by nurses using an iterative design process can lead in better implementation and end-user acceptance of new technology.
For patients, Eloquence™ could be an appropriate tool to facilitate communication primarily for two reasons: First, the ability to inform nurses and other health care staff “specific” requests would be helpful, which could better enhance the sense of control the patients perceive with their call light use.2 Second, nurses and other healthcare staff could arrive to patient rooms prepared to address their patient needs. The perceived improvement on delineating specific nursing personnel to specific call requests could abate previous concerns on the ambiguity on whose responsibility it is to answer the call light3 and the patient dissatisfaction from responsiveness to call lights1, 4-6 . Asking patients about their concerns regarding hospital technology is important in the provision of both the delivery of patient-centered care and ensuring the technology meets the end users' needs both in design and functionality. The nurses and patients also discussed different perspectives with regards to technological aspects of the Eloquence™ prototype.
Nurses expressed some concern in regards to different aspects of the use of advanced technology such as the Eloquence™ prototype that was demonstrated. For example, nurses commented that for personnel and older patients with limited technological skills, there could be some discomfort with their ability to easily learn and the use of Eloquence™'s technology. In addition, some nurses were not in agreement with some of the user interface features of Eloquence™; citing that the bedside tablet may be too large, there were too many options for patients, and that replacement parts would need to be available immediately, if warranted. In contrast, some patients commented that they thought the bedside device may need to be smaller, letter size and sensitivity of the tablet's touch screen should be evaluated, and that perhaps the “urgent” button should be larger and more prominent. Lastly, nurses suggested future logistical additions for the Eloquence™ system.
Nurses suggested future logistical additions for Eloquence™ from both a professional nursing perspective, and from a patient-centered perspective. From a nursing perspective, nurses felt that direct connections to charge nurses, the ability to page physicians, and the ability to view the home screen for the entire unit's needs would be beneficial. From a patient-centered perspective, nurses suggested that ordering food/snacks directly from dietary, a headphone attachment, the addition of music, and a tutorial on how to use the Eloquence™ bedside tablet, should be included in future programming for the Eloquence™ system for patient use. Thus, nurses provided worthy suggestions for not only their professional use; but also advocated on behalf of patients' use of Eloquence™ through suggestions for future Eloquence™ programming. Patients also provided their thoughts on the Eloquence™ system, often paralleling that of the nurses' perspectives. The majority of patients, however, had no new suggestions for future iterations of Eloquence™. From both the nurses' and patients' perspectives, the importance of more effective communication between caregivers and patients is prudent; an appropriate call light system is warranted. Eloquence™, in accordance with the perspectives from nurses and patients, not only solicited appropriate usability, but also contributed to improving communication between patients and their nurses.
Study Implications
Nurse call systems serve as critical component of patient care delivery and the ability for patients to communicate with their nursing personnel. The importance implementing an appropriate call light system that is multifunctional, addresses the needs of both patients, healthcare providers, and administrators, and, supports effective communication, cannot be undermined. Our study adds to the limited inquiry on the impact of call light use and work flow to patient care. The results from the nurse focus groups and patient interviews provide insight on the phenomenon surrounding call light use that can be used to develop further research and technology development. Particularly, their comments on improvements to nurse call systems could guide health informaticians, administrators, and clinicians on developing and implementing new call light technologies to better serve patients and nursing staff. Further research is needed to examine impact of nurse call light use on patient care and nurse-sensitive patient outcomes. For instance, a study could be undertaken to see if there is a difference between call light response times in private and shared patient rooms, and if the difference correlates with patient outcomes.
This study addressing the usefulness, effectiveness, and appropriateness of an alpha-prototype of the Eloquence™ system in acute inpatient noncritical care units as perceived by nurses and patients was limited in the number of participants included. Further, Eloquence™ was not used in a real patient care setting for the purposes of this study. A more in depth study could be conducted after the implementation of Eloquence™ in an inpatient unit. Nonetheless, nurse and patient suggestions should be used in future design and engineering of Eloquence™ and before final implementation of the Eloquence™ system since nurses and patients are the primary users of Eloquence™.
In conclusion, findings from this study demonstrate that Eloquence™ is a favorable call light system and device, but further research with more participation from users is required for a more robust evaluation.
Acknowledgments
This research was supported by National Center on Minority Health and Health Disprities of the National Institutes of Health (NIH) under award number 1R41MD006149-01. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
References
- 1.Deitrick L, Bokovoy J, Stern G, Panik A. Dance of the call bells: using ethnography to evaluate patient satisfaction with quality of care. Journal of nursing care quality. 2006 Oct-Dec;21(4):316–324. doi: 10.1097/00001786-200610000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Lasiter S. “The button”: initiating the patient-nurse interaction. Clin Nurs Res. 2014 Apr;23(2):188–200. doi: 10.1177/1054773813479794. [DOI] [PubMed] [Google Scholar]
- 3.Tzeng HM. Perspectives of staff nurses of the reasons for and the nature of patient-initiated call lights: an exploratory survey study in four USA hospitals. BMC Health Serv Res. 2010 Feb;10:52. doi: 10.1186/1472-6963-10-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tzeng HM, Ronis DL, Yin CY. Relationship of actual response time to call lights and patient satisfaction at 4 US hospitals. J Nurs Care Qual. 2012 Apr-Jun;27(2):E1–8. doi: 10.1097/NCQ.0b013e31823e827a. [DOI] [PubMed] [Google Scholar]
- 5.Tzeng HM, Yin CY. Predicting patient satisfaction with nurses' call light responsiveness in 4 US hospitals. J Nurs Adm. 2010 Oct;40(10):440–7. doi: 10.1097/NNA.0b013e3181f2eb29. [DOI] [PubMed] [Google Scholar]
- 6.Roszell S, Jones CB, Lynn MR. Call bell requests, call bell response time, and patient satisfaction. J Nurs Care Qual. 2009 Jan-Mar;24(1):69–75. doi: 10.1097/01.NCQ.0000342938.99036.9f. [DOI] [PubMed] [Google Scholar]
- 7.Tzeng HM, Grandy GA, Yin CY. Staff response time to call lights and unit-acquired pressure ulcer rates in adult in-patient acute care units. Contemp Nurse. 2013 Oct;45(2):182–7. doi: 10.5172/conu.2013.45.2.182. [DOI] [PubMed] [Google Scholar]
- 8.Tzeng HM, Titler MG, Ronis DL, Yin CY. The contribution of staff call light response time to fall and injurious fall rates: an exploratory study in four US hospitals using archived hospital data. BMC Health Serv Res. 2012 Mar;12:84. doi: 10.1186/1472-6963-12-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tzeng HM, Yin CY. The extrinsic risk factors for inpatient falls in hospital patient rooms. J Nurs Care Qual. 2008 Jul-Sep;23(3):233–41. doi: 10.1097/01.NCQ.0000324588.91837.84. [DOI] [PubMed] [Google Scholar]
- 10.Meade CM, Bursell AL, Ketelsen L. Effects of nursing rounds on patients' call light use, satisfaction, and safety. AJN. 2006 Sep;106(9):58–71. doi: 10.1097/00000446-200609000-00029. [DOI] [PubMed] [Google Scholar]
- 11.Murray T, Spence J, Bena JF, Morrison S, Albert NM. Perceptions of reasons call lights are activated pre- and postintervention to decrease call light use. J Nurs Care Qual. 2010 Oct-Dec;25(4):366–72. doi: 10.1097/NCQ.0b013e3181e0cf08. [DOI] [PubMed] [Google Scholar]
- 12.Breslin S, Greskovich W, Turisco F. Wireless technology improves nursing workflow and communications. Comput Inform Nurs. 2004 Sep-Oct;22(5):275–81. doi: 10.1097/00024665-200409000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Kuruzovich J, Angst CM, Faraj S, Agarwal R. Wireless communication role in patient response time: a study of vocera integration with a nurse call system. Comput Inform Nurs. 2008;26(3):159–66. doi: 10.1097/01.NCN.0000304780.27070.ee. [DOI] [PubMed] [Google Scholar]
- 14.Institute of Medicine 2010. The future of nursing: Leading change, advancing health. Washington, DC: National Academies Press; 2010. [PubMed] [Google Scholar]
- 15.Glaser BG, Strauss A. The Discovery of Grounded Theory. Chicago: Aldine Publishing; 1967. [Google Scholar]


