Abstract
Objective
Epidemiological data on neonatal hypothermia in low-resource community settings are lacking. We quantified incidence, age distribution, and seasonality of neonatal hypothermia among a large population cohort.
Design
Longitudinal cohort study
Setting
Sarlahi, Nepal
Participants
23,240 newborns born between September 2002 and January 2006
Main Exposures
Community-based workers recorded axillary temperature on days 1–4, 6, 8, 10, 12, 14, 21, 28 (total measures: 213,636).
Main Outcome Measures
Regression smoothing was used to describe axillary temperature patterns over the newborn period. Hypothermia incidence in the first day, week, and month were estimated using standard cutoffs. Ambient temperatures allowed comparison of mild (36.0°C – 36.5°C) moderate/severe hypothermia (<36.0°C) incidence over mean ambient temperature quintiles.
Results
Measures <36.5 °C were observed in 21,459 (92.3%) babies; half (48.5%) had moderate or severe hypothermia, and risk peaked in the first 24–72 hours of life. Risk of moderate/severe hypothermia increased by 41.3% (95% CI: 40.0% – 42.7%) for every 5 °C decrease in average ambient temperature. Relative to the highest quintile, risk was 4.03 (3.77 – 4.30) times higher among babies exposed to the lowest quintile of average ambient temperature. In the hot season, one fifth (18.2%) were observed below the moderate hypothermia cutoff.
Conclusions
Mild or moderate hypothermia was near universal, with substantially higher risk in the cold season. However, incidence in the hot season was also high; thus year-round thermal care promotion is required. Research on community, household, and care-taker practices associated with hypothermia can guide behavioral interventions to reduce risk.
Keywords: neonatal, hypothermia, Nepal, seasonality, community health
Introduction
Neonatal hypothermia has been recognized as a contributing cause of mortality and morbidity among both low birth weight and normal weight babies, even in warm tropical environments1–3. The prevention of neonatal hypothermia is included in essential newborn care, a basic package of interventions that should be provided to all newborns4, 5. Strategies to prevent and effectively manage hypothermia have been extensively studied in developed countries and subsequent improvements in thermal care of the newborn have largely been limited to these settings6.
More than 98% of the 4 million annual neonatal deaths occur in developing countries where specific data on hypothermia are scarce7, 8 and largely limited to hospital-based data. A number of hospital-based studies in such settings have demonstrated that thermal stress is common9, 10, and more than one-half of newborns experience hypothermic episodes1, 2, 10–12. Some hospital-based studies have observed higher mortality risk among admitted babies with hypothermia broadly defined as any measure <36.0°C3 or 36.5°3, 13, 14. While these studies indicate that hypothermia may be an important contributor to neonatal mortality, they are limited by lack of adjustment for age of infants at measurement and are predominately focused on sick infants presenting to tertiary care units. In a retrospective cohort study from Guinea-Bissau, hypothermia (<34.5°C) measured within 12 hours of birth in a maternity ward in Guinea-Bissau was associated with almost 5 times higher mortality in the first week of life15.
The majority of high-risk babies are born in the home in low-resource communities where the burden, health impact, and associations of hypothermia with newborn care practices and health outcomes have been insufficiently documented8. Smaller studies in both urban slums16 and the rural community17 in India have reported on the incidence of hypothermia, but large population-based investigations of the timing of episodes, cumulative incidence of neonatal hypothermia, and seasonality of risk among babies born at home have not been conducted. Such information is needed to further guide community-based neonatal health promotion packages, and refine messages related to thermal care of the newborn throughout the newborn period. Our previous community-based trials of chlorhexidine cleansing interventions in southern Nepal between 2002 and 200618, 19 included repeated visits by project workers to more than 23,000 babies, producing more than 213,000 axillary temperature measures. In this manuscript we present analyses of these existing data to provide an overview of the pattern, incidence, age distribution, and seasonality of neonatal hypothermia, both overall and within sub-categories of severity using current World Health Organization (WHO) temperature cut-offs1. Future analyses will build on data presented here to examine the relationship between neonatal hypothermia and mortality and how hypothermia incidence varies across potential risk factors including household care practices and infant, maternal/paternal, household, demographic, and socioeconomic characteristics.
Methods
Data Collection
Data for this analysis were collected during a large, community-based, placebo controlled, randomized trial of the impact of two chlorhexidine interventions (newborn skin and umbilical cord cleansing) on neonatal mortality and morbidity. Details of implementation and results of these trials have been published previously18, 19. Briefly, between August 2002 and January 2006, 23,662 live born babies in the Nepal Nutrition Intervention Project area of Sarlahi District, Nepal were eligible to participate in either a comparative phase or post-trial scale-up phase of the study. Identification, follow-up and data collection activities remained identical in both phases. Pregnancies were identified at approximately mid-pregnancy, study procedures were explained and oral informed consent obtained. Women received iron-folic acid supplements, deworming with albendazole, weekly vitamin A supplementation, a clean birthing kit and basic counseling on nutrition and antenatal and postnatal newborn care. Notification of live-born babies to study workers was facilitated by local female staff, and babies were visited as soon as possible after birth and then followed up during the neonatal period on a standard schedule (days 1–4, 6, 8, 10, 12, 14, 21, 28). These project workers had completed secondary school education and approximately 7–12 years experience as data collectors in field trials in this setting.
At each home visit, the project worker measured the axillary temperature of the newborn using a locally purchased lithium battery-operated digital thermometer. Workers were trained by supervisory staff using a standard written protocol and directly observed throughout the course of the study for adherence to the protocol. The baby was measured either in the lap/arms of the mother or other caretaker, on a blanket/mat placed on the floor, or on a bed. Measurement involved placing the tip of the thermometer in the middle of the axilla and holding the newborn’s arm in place until an automatic audible notification was heard. Data were recorded on forms as displayed on the thermometers on the Fahrenheit scale, and converted to Celsius during analysis.
Analytic Dataset
All babies with one or more measures of axillary temperature recorded during the home visit schedule were included in the analysis. For the main parent trial, mortality during the neonatal period was the primary outcome, thus flexibility on timing of the 28-day home visit was granted during field implementation. Therefore, for the purposes of this analysis, axillary temperatures recorded on the day 28 visit were included if collected within 7 days of the end of the neonatal period. Daily maximum and minimum environmental temperature recordings (in Celsius) at Simara (27°09’34’’N, 84°58’47” E, 137 meters above sea level) and Janakpur (26°42’39” N, 85°55’27’’ E, 78 meters above sea level) airports, were obtained from the Government of Nepal, Department of Hydrology and Meteorology, Ministry of Environment, Science, and Technology. These airports are located approximately 52 km east and 60 km west, respectively, of the geographical center of the study area, and the entire region is at or near sea level with little to no topographical variability.
Analysis
Descriptive analysis included examination of mean, median, maximum/minimum, and inter-quartile range of axillary temperatures by age at the time of the measurement. Locally weighted regression smoothing illustrating the pattern of axillary temperature measures over time were restricted to the first 10 days of life where most of the temperature variability occurred. The numbers and proportion of infants meeting WHO definitions1 for hypothermia (mild: [36.0 °C – 36.5 °C); moderate: [32.0 °C – 36.0 °C), severe: < 32.0 °C) were estimated, by 24-hour age interval. Given the small number of newborn babies meeting the criteria for severe hypothermia (n=3), this category was combined with moderate for the remaining analyses. Incidence of hypothermia (any or moderate/severe) was estimated for the first week of life and the entire neonatal period, and expressed in two separate ways: First, incidence was estimated as the proportion of newborn babies meeting the specified cutoff for mild or moderate/severe hypothermia at any one of his/her measures throughout the newborn period. This is can be considered an estimate of cumulative incidence. Second, incidence was estimated as the proportion of total measurements for which a newborn was found to meet the specified cutoff. This estimate, or the proportion of prevalent days, was adjusted for multiple measures per child using generalized estimating equations with exchangeable correlation structure.
The average ambient minimum temperature was estimated for each day during the study period as the mean of the minimum temperature from Simara and Janakpur if both measurements were available; the recording from a single airport was used if only one was available. Seasonality of hypothermia was examined by 1) creating locally weighted regression smoothing curves of a) the daily proportion of measures meeting the cutoff for hypothermia and b) the daily minimum ambient temperature, and 2) plotting these curves over the period from 3rd September 2002 to 1st February 2006. For each infant, the mean of the minimum ambient temperatures recorded throughout the first week of life was estimated; the cumulative incidence (proportion of newborn babies) of moderate/severe hypothermia was compared across quintiles of this average temperature. Separately, prevalent days of any (<36.5°C) or moderate (<36.0°C) hypothermia during the first week of life were estimated and compared by quintiles of minimum ambient temperature.
Analyses were conducted using Stata 9.2 (Stata Corp, College Station, TX). The Nepal Health Research Council (Kathmandu, Nepal) and the Committee on Human Research of the Johns Hopkins Bloomberg School of Public Health (Baltimore, USA) approved the protocol. The parent trial is registered at Clinicaltrials.gov (NCT00109616)
Results
Between September 2002 and January 2006, there were 23,662 live born infants in the study area eligible for inclusion. Of these, 23,257 (98.2%) were met alive at one or more home visits during the neonatal period; 17 of these babies did not have any axillary temperatures measures, while the remaining 23,240 contributed to the analytic dataset. Among these babies, the mean (standard deviation) and median (range) number of temperature recordings collected was 9.2 (2.1) and 10 (1 – 11), respectively. The maximum number of measures (n=11) was provided by 7,910 (34%) newborn babies, while 20,689 (89%) contributed 7 or more measures. The 23,240 babies contributed a total of 213,636 axillary temperature measures throughout the neonatal period, of which more than three-quarters were collected during the first two weeks of life (n=167,607 measures, 78.5%).
Hypothermia patterns during the neonatal period
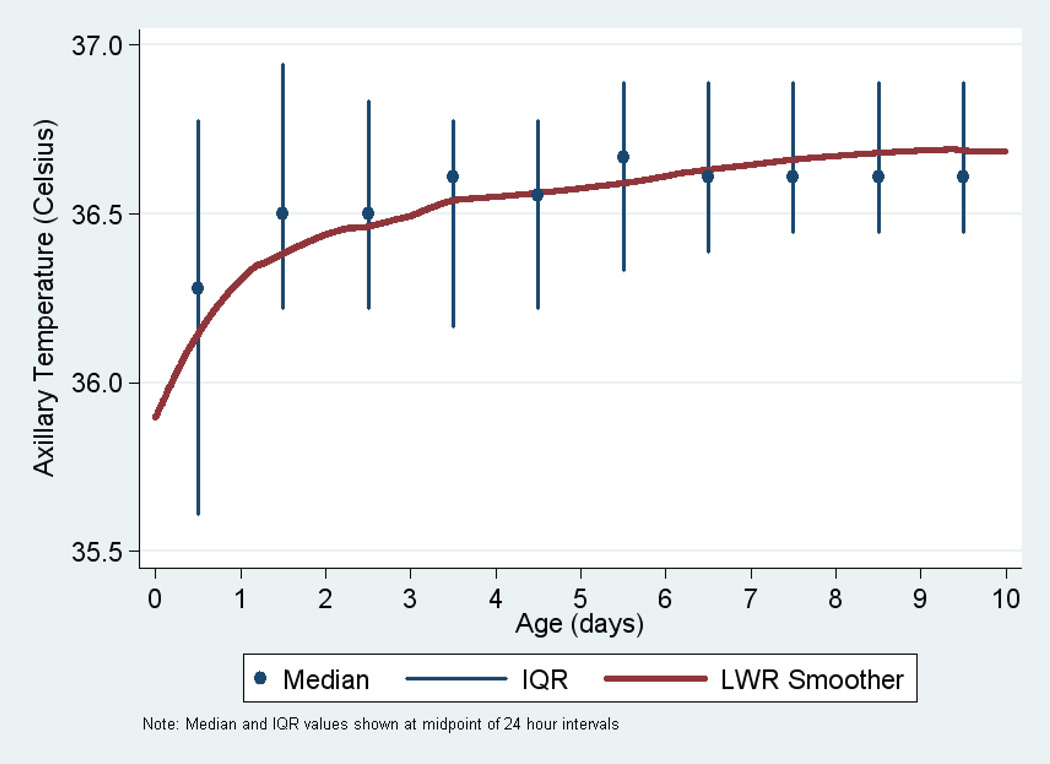
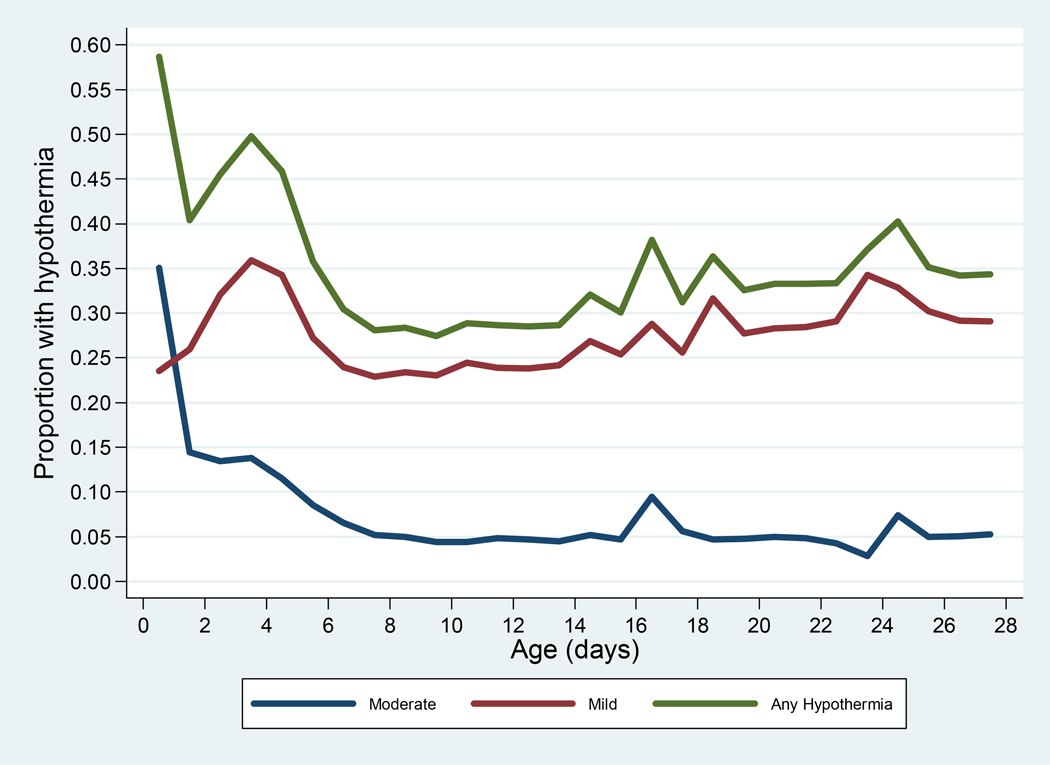
The mean axillary temperature was lowest during the first 24 hours (mean=36.1 °C); measures were also most variable (SD=1.0°C; range: 30.3 °C – 40.3 °C) during this period. The mean and interquartile range of axillary temperature measures during the first 10 days of life, and a smoothed locally weighted regression of temperature on age during this period is shown in Figure 1. Almost 60% of the babies measured within 24 hours (n=8,606 of 14,588, 59.0%) were hypothermic (axillary temperature less than 36.5 °C) at first measure; only one of these babies had severe hypothermia (<32.0 °C), while 35.4% (n=5,169) and 23.6% (n=3,436) had moderate or mild hypothermia. The proportions of babies meeting the criteria for mild, moderate/severe (combined), or any hypothermia, by 24-hour age intervals, is shown in Figure 2. The prevalence of both moderate and mild hypothermia peaked in the first 24 hours. While the proportion with axillary temperatures below 36 °C decreased to a range of approximately 4% to 8% after the first week of life, the proportion of babies with any hypothermia (<36.5 °C) never went below 25% for any 24-hour interval, and was lowest during the second week of life, before trending upward in the final two weeks of the neonatal period.
Figure 1.
Locally weighted regression smoother (LWS) and median/IQR of axillary temperatures during the first 10 days of life
Figure 2.
Proportion of infants meeting WHO definitions for mild, moderate, or any hypothermia, by age*
*Estimates are located at the mid-point of each 24-hour interval
Cumulative Incidence
Cumulative incidence of hypothermia (proportion of babies meeting criteria on one or more days) and total prevalent days of severe, moderate, mild, and any hypothermia are shown in Table 1. One or more axillary temperature measures less than the WHO cut-off for any hypothermia (<36.5°C) were observed in 92.3% of all newborn babies. Among these hypothermic babies, the minimum temperature observed was in the mild range (36.0 – 36.4°C) for 47.4% of babies, and in the upper half (34.0°C – 35.9°C) of the WHO-defined range for moderate hypothermia for 48.7% of babies. Only 833 (3.9%) babies had measures below 34.0°C and only 23 (0.1%) had one or more measures in the severe (<32.0°C) range.
Table 1.
Incidence of hypothermia (cumulative proportion of newborn babies and proportion of all measures): Entire neonatal period and first week of life
| Proportion of all newborn babies (N=23,240) | ||||
| Hypothermia | Neonatal (N=23,240, 100%) | First Week (N=22,114, 95.2%) | ||
| Babies | Percent (95%CI) | Babies | Percent (95%CI) | |
| Severe | 23 | 0.1 (0.1 – 0.1) | 13 | 0.1 (0.0 – 0.1) |
| Moderate | 11,277 | 48.5 (47.9 – 49.2) | 9161 | 41.4 (40.8 – 42.1) |
| Mild | 20,516 | 88.3 (87.9 – 88.7) | 15,621 | 70.6 (70.0 – 71.2) |
| Any | 21,459 | 92.3 (92.0 – 92.7) | 17,958 | 81.2 (80.6 – 81.7) |
| Proportion of all axillary measures (N=213,636) | ||||
| Hypothermia | Neonatal (N=213,636, 100%) | First Week (N=94,571) | ||
| Prevalent Days | Percent (95%CI)* | Prevalent Days | Percent (95%CI)* | |
| Sev/Moderate | 20,689 | 9.7 (9.5 – 9.8) | 14,889 | 15.8 (15.5 – 16.1) |
| Mild | 57,864 | 27.1 (26.8 – 27.3) | 27,476 | 29.1 (28.8 – 29.4) |
| Any | 78,553 | 36.7 (36.4 – 37.0) | 42,375 | 44.8 (44.4 – 45.3) |
Confidence intervals adjusted for multiple measures per infant
Almost half (48.6%) of all babies had one or more measures in the moderate or severe range. This proportion was higher (54.5%) among those babies whose first measure was collected within 24 hours of birth (14,588 babies, or 62.8%), compared to the burden (38.7%) among those first measured after 24 hours (Risk Ratio [RR] = 1.41 [1.37 – 1.45]). More than 95% of babies had data recorded within the first week of life; among these babies 41.4% met the criteria for moderate/severe hypothermia. Of all axillary measures within the first week of life, 15.8% (15.5 – 16.1) were in the moderate/severe range. More than one third of all measures (78,553 of 213,636) fit the WHO cut-off for any hypothermia.
Seasonality of Hypothermia
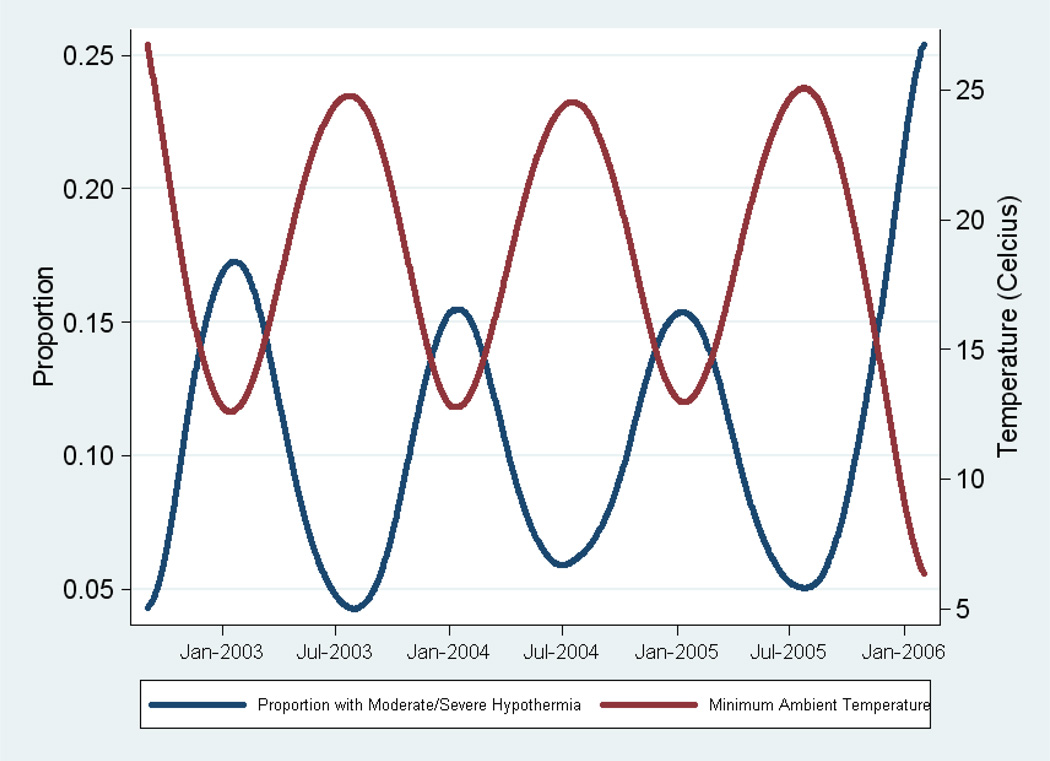
Axillary temperature was strongly correlated with ambient temperature. Scatter plots of ambient temperature (Figure 3) peaked in July/August of each calendar year, and these correspond with the lowest proportion of axillary measures <36.0°C, while the coldest days of the year (January) corresponded with the highest prevalence of measures <36.0°C. Cumulative incidence during the first week of life was substantially higher among babies born in cooler temperatures. For every 1° difference in minimum ambient temperature (averaged over the first week of life), the risk of moderate or severe hypothermia were approximately 7% higher; for each incremental reduction in ambient temperature of 5° and 10°, the risk of hypothermia increased by a factor of 1.41 (1.40 – 1.43) and 2.00 (1.96 – 2.04). Babies exposed to the lowest quintile of average minimum ambient temperatures had 4.03 (3.77 – 4.30) times the risk of moderate/severe hypothermia than those in the highest quintile.
Figure 3.
Seasonality of hypothermia: Locally weighted regression curves for daily proportion of axillary temperatures measures <36.0° and minimum ambient temperature throughout the study period
* Predictions at the extreme end of the curves are skewed due to progressively fewer estimates contributing to the regression estimate at those points.
On days with minimum ambient temperatures in the lowest quintile (range: 3.8°C – 11.7°C), the proportion of axillary measures during the first week of life meeting the cutoff was 31.7% (5,765 of 18,213 total measures in the first week), while on days in the highest quintile (range: 25.6°C – 29.3°C), the proportion was 4.3% (816 of 19,164). Adjusting for age of the infant, the prevalence rate ratio was 7.70 (95% CI: 7.13 – 8.33) times higher on the coldest (per quintile) days compared to the warmest days (Table 3). The correlation between ambient temperature quintiles and likelihood of hypothermic axillary measures was relatively stable whether further restricted to first day of life or expanded to the entire neonatal period (data not shown).
Table 3.
Cumulative Incidence and Proportion of Newborn Babies With Hypothermia Within the First Week of Life by Quintile of Minimum Ambient Temperature
| Minimum Ambient Temperature, Quintile (Range) |
Babies, No. |
Hypothermia Cases, No. (%) |
RR (98% CI) |
|---|---|---|---|
| 1 (3.8°C–11.7°C) | 4426 | 3245 (73.2) | 4.03 (3.77–4.30) |
| 2 (11.8°C–16.7°C) | 4440 | 2357 (53.1) | 2.92 (2.72–3.12) |
| 3 (16.8°C–22.7°C) | 4408 | 1606 (36.4) | 2.00 (1.86–2.15) |
| 4 (22.8°C–25.5°C) | 4418 | 1156 (26.2) | 1.44 (1.32–1.56) |
| 5 (25.6°C–29.3°C) | 4422 | 805 (18.2) | 1 [Reference] |
Abbreviation: CI, confidence interval; RR, risk ratio.
Discussion
These data indicate that among newborns in rural Sarlahi, Nepal, axillary temperatures at or below the current WHO cutoffs for mild and moderate hypothermia are common, with more than 90% of babies having one or more measures <36.5°C in the first 28 days. Furthermore, there is a strong association between season and hypothermia, with incidence rates peaking in the coldest months of the year (December – February) and the risk of moderate/severe hypothermia more than 4 times higher among babies in the lowest quintile of mean ambient temperature exposure. However, even among babies in the highest ambient temperature exposure quintile, the proportion with hypothermia in the first week of life was almost one in five (18.2%), suggesting the continuing importance and relevance of hypothermia risk even in the hot season of a tropical climate.
These estimates in the community confirm hospital reports that the burden of neonatal hypothermia is high in Nepal and other developing countries where exposure to cold stress is extremely common. In a maternity hospital in Katmandu, 85% and 50% of newborns were hypothermic at 2 and 24 hours after birth, respectively11. Similarly, 79%, 85%, and 62% of newborns in urban hospitals of Uganda10, Zimbabwe12, and Nigeria14, respectively, were hypothermic. In a community study of 763 newborns, 17% were observed with axillary measures <35°C; this proportion was higher in “winter” months (21.5%) compared with “summer” months (13.9%)17, and hypothermia was associated with approximately three times higher mortality risk20. In these studies, including the community-based study in India, observations were collected close to the time of birth (generally within hours). The estimate of hypothermia depends substantially on the distribution of ages at which babies are measured. For example in our study, babies whose serial measures began within the first day of life had significantly higher risk of meeting the criteria for moderate hypothermia compared with those whose measures were initiated later.
The large number of newborn (>22,000) and the repeated measures (maximum 11) throughout the newborn period allowed for examination of the pattern of hypothermia across the newborn period and precise estimates of incidence in the first 24 hours, first week, and first month of life. Ambient temperatures available for every day between September 2002 and February 2006 allowed for estimates over three full calendar years. Given that this was a community-based study of newborns in the home, continuous monitoring of temperature as done in hospital-based studies of neonatal hypothermia9, 21 was not attempted due to the logistical challenges. This may lead to an underestimate of hypothermia burden as the largest variation in temperatures occur during the first 24–48 hours of life and axillary measures were not collected for all babies in this early timeframe; this observation-time dependency was demonstrated by the 41% higher likelihood of observing one or more measures in the moderate to severe range among babies first measured within 24 hours.
Any underestimate of the population-level burden of hypothermia might be offset by the choice of digital thermometers and the axilla, as the method and location of measurement, respectively. Digital thermometers with an automatic audible notification system are inexpensive, locally available, and substantially easier to use than mercury-in-glass thermometers, given the shorter placement time, which is important for neonates, and the ease of reading in low-light settings such as rural homes. These may slightly over22, 23 or underestimate23–25 temperature relative to mercury-in-glass thermometers, leading to upward and/or downward bias in the estimates of hypothermia burden. Recording at the axilla, rather than rectum, was chosen given the repetitive collection outside of a clinical setting, the ease and safety of placement, and greater likelihood of compliance from parents. However, in a systematic review26 of 10 studies comparing rectal versus axilla temperatures among neonates, the pooled mean difference (rectal minus axilla) was 0.17° (−0.15 – 0.50). Adjusting upward all measures in this dataset by 0.17°C would result in decreases in the proportion of babies with one or more measures meeting cutoffs for moderate/severe hypothermia (37.9% [adjusted] vs. 48.6% [observed], 22% reduction) or any hypothermia (82.2% [adjusted] vs. 92.3% [observed], 11% reduction).
All infants in this study were participants in the parent chlorhexidine trials which included a one-time, full-body cleanse of the infant immediately after birth with either chlorhexidine or water-based placebo soaked baby wipes. We do not believe this procedure contributed to the incidence of hypothermia in this setting or the conclusions drawn from these analyses. In a pilot study27 of the feasibility, safety, and acceptability of in-home full-body cleansing of newborns conducted prior to the main trial, there was decrease in body temperature of 0.4°C; the time between the procedure and return to mean baseline temperature was about 15 minutes in a study of 286 newborns undergoing the procedure at a tertiary care hospital in Kathmandu28. All workers were instructed minimize the time of the procedure, wrap the baby warmly in a baby blanket provided to all families at the time of the intervention, and reiterate the basic messages on the importance of keeping the baby dry and warm. While there was not a group of babies that did not receive a wipe, a previous study29 conducted by our group in the same area immediately prior to this trial, measured axillary temperature of ~4000 newborns throughout the neonatal period in an identical manner, allowing comparison between the two studies. Adjusted for month of birth, there was a 9.9% (95% CI: 5.0% – 15.0%) increased risk of mild hypothermia and a 14.5% (95% CI: 5.6% – 20.8%) decreased risk of moderate / severe hypothermia in the skin cleansing trial compared with the previous study. These data suggest that, rather than the cleansing intervention increasing hypothermia risk, there might have been a slight shift upward in the axillary temperature distribution, potentially a result of increased awareness and messages about hypothermia given in the context of the intervention.
Comment
In this community, further efforts are required to reduce the exposure of newborn babies to thermal stress. Thermal care is considered important by caretakers in this community: warming of the room in which newborns are cared for (82.2%) and provision of a hat (82.5%) for the baby are relatively common30, and mustard oil massage is nearly universal with 40% of mothers reporting that massage to keep the baby warm31. However, newborns are often not dried (18.0%) and wrapped (22.2%) until after the placenta has been delivered32, 33, more than 95% of babies are bathed within the first 12 hours after birth31, skin-to skin contact (4.4%) is uncommon30, and initiation of breastfeeding within the first hour (3.3%) hours is rare34, all practices that might be associated with hypothermia in the first week of life and beyond and could be improved through behavioral change communications. Further analyses are needed to identify specific factors that are associated with increased risk of hypothermia and risk of mortality and morbidity subsequent to hypothermia. Context-specific and culturally appropriate measures might then be defined to reduce exposure to thermal stress, evaluated for impact, and ultimately, scaled up within integrated neonatal health promotion programs.
Table 2.
Cumulative incidence and proportion of axillary measures <36.0°C within the first week of life by quintile of minimum ambient temperature measure
|
Quintile (Range) Ambient Temp |
Number of Babies | Cases (%) | RR | 95% CI† |
| 1 (3.8°C – 11.7°C) | 4,426 | 3,245 (73.2) | 4.03 | 3.77 – 4.30 |
| 2 (11.8°C – 16.7°C) | 4,440 | 2,357 (53.1) | 2.92 | 2.72 – 3.12 |
| 3 (16.8°C – 22.7°C) | 4,408 | 1,606 (36.4) | 2.00 | 1.86 – 2.15 |
| 4 (22.8°C – 25.5°C) | 4,418 | 1,156 (26.2) | 1.44 | 1.32 – 1.56 |
| 5 (25.6°C – 29.3°C) | 4,422 | 805 (18.2) | 1.00 | |
|
Quintile (Range) Ambient Temp |
Number of Axillary Measures |
Number (%) <36.0°C |
PRR* | 95% CI† |
| 1 (3.8°C – 11.7°C) | 18,213 | 5,765 (31.7) | 7.70 | (7.13 – 8.33) |
| 2 (11.8°C – 16.7°C) | 18,133 | 4,219 (23.3) | 5.93 | (5.74 – 6.42) |
| 3 (16.8°C – 22.7°C) | 18,783 | 2,511 (13.4) | 3.36 | (3.09 – 3.65) |
| 4 (22.8°C – 25.5°C) | 20,278 | 1,588 (7.8) | 1.87 | (1.72 – 2.04) |
| 5 (25.6°C – 29.3°C) | 19,164 | 816 (4.3) | 1.00 | |
PRR: Prevalence Rate Ratio, adjusted for age of infant
Confidence Intervals adjusted for multiple measures per infant, using GEE
Acknowledgements
This study was supported by grants from the National Institutes of Health, Bethesda, Maryland (HD 553466, HD 44004, HD 38753), the Bill and Melinda Gates Foundation, Seattle, Washington (810-2054), and Cooperative Agreements between JHU and the Office of Health and Nutrition, US Agency for International Development, Washington DC (HRN-A-00-97-00015-00, GHS-A-00-03-000019-00). The lead author had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Abbreviations
- WHO
World Health Organization
- RR
Risk Ratio
- SD
Standard Deviation
Footnotes
Disclosure: The authors have no financial relationships relevant to this manuscript
REFERENCES
- 1.World Health Organization. Thermal protection of the newborn: A practical guide. Geneva: World Health Organization; 1997. WHO/RHT/MSM/97.2. [Google Scholar]
- 2.Tafari N, Olsson EE. Neonatal cold injury in the tropics. Ethiop Med J. 1973;11(1):57–65. [PubMed] [Google Scholar]
- 3.Christensson K, Bhat GJ, Eriksson B, Shilalukey-Ngoma MP, Sterky G. The effect of routine hospital care on the health of hypothermic newborn infants in Zambia. J Trop Pediatr. 1995;41(4):210–214. doi: 10.1093/tropej/41.4.210. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Essential newborn care. 1996 WHO/FRH/MSM/96.13.
- 5.World Health Organization. Mother-baby package: Implementing safe motherhood in countries. 1994 WHO/FHE/MSM/94.11.
- 6.Sauer PJ. Neonatal thermoregulation. In: Cowett RM, editor. Principles of Perinatal-Neonatal Metabolism. New York: Springer-Verlag; 1991. [Google Scholar]
- 7.Lawn JE, Cousens S, Zupan J. Lancet Neonatal Survival Steering Team. 4 million neonatal deaths: When? Where? Why? Lancet. 2005;365(9462):891–900. doi: 10.1016/S0140-6736(05)71048-5. [DOI] [PubMed] [Google Scholar]
- 8.Bhutta ZA, Darmstadt GL, Hasan BS, Haws RA. Community-based interventions for improving perinatal and neonatal health outcomes in developing countries: A review of the evidence. Pediatrics. 2005;115(2 Suppl):519–617. doi: 10.1542/peds.2004-1441. [DOI] [PubMed] [Google Scholar]
- 9.Ellis M, Manandhar N, Shakya U, Manandhar DS, Fawdry A, Costello AM. Postnatal hypothermia and cold stress among newborn infants in Nepal monitored by continuous ambulatory recording. Arch Dis Child Fetal Neonatal Ed. 1996;75(1):F42–F45. doi: 10.1136/fn.75.1.f42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Byaruhanga R, Bergstrom A, Okong P. Neonatal hypothermia in Uganda: Prevalence and risk factors. J Trop Pediatr. 2005;51(4):212–215. doi: 10.1093/tropej/fmh098. [DOI] [PubMed] [Google Scholar]
- 11.Johanson RB, Spencer SA, Rolfe P, Jones P, Malla DS. Effect of post-delivery care on neonatal body temperature. Acta Paediatr. 1992;81(11):859–863. doi: 10.1111/j.1651-2227.1992.tb12123.x. [DOI] [PubMed] [Google Scholar]
- 12.Kambarami R, Chidede O. Neonatal hypothermia levels and risk factors for mortality in a tropical country. Cent Afr J Med. 2003;49(9–10):103–106. [PubMed] [Google Scholar]
- 13.Manji KP, Kisenge R. Neonatal hypothermia on admission to a special care unit in Dar-es-Salaam, Tanzania: A cause for concern. Cent Afr J Med. 2003;49(3–4):23–27. [PubMed] [Google Scholar]
- 14.Ogunlesi TA, Ogunfowora OB, Adekanmbi FA, Fetuga BM, Olanrewaju DM. Point-of-admission hypothermia among high-risk Nigerian newborns. BMC Pediatr. 2008;8:40. doi: 10.1186/1471-2431-8-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sodemann M, Nielsen J, Veirum J, Jakobsen MS, Biai S, Aaby P. Hypothermia of newborns is associated with excess mortality in the first 2 months of life in Guinea-Bissau, West Africa. Trop Med Int Health. 2008;13(8):980–986. doi: 10.1111/j.1365-3156.2008.02113.x. [DOI] [PubMed] [Google Scholar]
- 16.Green DA, Kumar A, Khanna R. Neonatal hypothermia detection by ThermoSpot in Indian urban slum dwellings. Arch Dis Child Fetal Neonatal Ed. 2006;91(2):F96–F98. doi: 10.1136/adc.2005.078410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bang AT, Reddy HM, Baitule SB, Deshmukh MD, Bang RA. The incidence of morbidities in a cohort of neonates in rural Gadchiroli, India: Seasonal and temporal variation and a hypothesis about prevention. J Perinatol. 2005;25(Suppl 1):S18–S28. doi: 10.1038/sj.jp.7211271. [DOI] [PubMed] [Google Scholar]
- 18.Mullany LC, Darmstadt GL, Khatry SK, et al. Topical applications of chlorhexidine to the umbilical cord for prevention of omphalitis and neonatal mortality in southern Nepal: A community-based, cluster-randomised trial. Lancet. 2006;367(9514):910–918. doi: 10.1016/S0140-6736(06)68381-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tielsch JM, Darmstadt GL, Mullany LC, et al. Impact of newborn skin-cleansing with chlorhexidine on neonatal mortality in southern Nepal: A community-based, cluster-randomized trial. Pediatrics. 2007;119(2):e330–e340. doi: 10.1542/peds.2006-1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reddy MH, Bang AT. How to identify neonates at risk of death in rural India: Clinical criteria for the risk approach. J Perinatol. 2005;25(Suppl 1):S44–S50. doi: 10.1038/sj.jp.7211272. [DOI] [PubMed] [Google Scholar]
- 21.Robertson NJ, Nakakeeto M, Hagmann C, et al. Therapeutic hypothermia for birth asphyxia in low-resource settings: A pilot randomised controlled trial. Lancet. 2008;372(9641):801–803. doi: 10.1016/S0140-6736(08)61329-X. [DOI] [PubMed] [Google Scholar]
- 22.Jones HL, Kleber CB, Eckert GJ, Mahon BE. Comparison of rectal temperature measured by digital vs. mercury glass thermometer in infants under two months old. Clin Pediatr (Phila) 2003;42(4):357–359. doi: 10.1177/000992280304200409. [DOI] [PubMed] [Google Scholar]
- 23.Latman NS, Hans P, Nicholson L, DeLee Zint S, Lewis K, Shirey A. Evaluation of clinical thermometers for accuracy and reliability. Biomed Instrum Technol. 2001;35(4):259–265. [PubMed] [Google Scholar]
- 24.Sganga A, Wallace R, Kiehl E, Irving T, Witter L. A comparison of four methods of normal newborn temperature measurement. MCN Am J Matern Child Nurs. 2000;25(2):76–79. doi: 10.1097/00005721-200003000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Smith J. Are electronic thermometry techniques suitable alternatives to traditional mercury in glass thermometry techniques in the paediatric setting? J Adv Nurs. 1998;28(5):1030–1039. doi: 10.1046/j.1365-2648.1998.00745.x. [DOI] [PubMed] [Google Scholar]
- 26.Craig JV, Lancaster GA, Williamson PR, Smyth RL. Temperature measured at the axilla compared with rectum in children and young people: Systematic review. BMJ. 2000;320(7243):1174–1178. doi: 10.1136/bmj.320.7243.1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mullany LC, Darmstadt GL, Khatry SK, LeClerq SC, Tielsch JM. Safety of neonatal skin cleansing in rural Nepal. Indian Pediatr. 2006;43(2):117–124. [PMC free article] [PubMed] [Google Scholar]
- 28.Mullany LC, Khatry SK, Sherchand JB, et al. A randomized controlled trial of the impact of chlorhexidine skin cleansing on bacterial colonization of hospital-born infants in Nepal. Pediatr Infect Dis J. 2008 doi: 10.1097/INF.0b013e31816791a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Christian P, Khatry SK, Katz J, et al. Effects of alternative maternal micronutrient supplements on low birth weight in rural Nepal: Double blind randomised community trial. BMJ. 2003;326(7389):571. doi: 10.1136/bmj.326.7389.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mullany LC, Darmstadt GL, Katz J, et al. Risk factors for umbilical cord infection among newborns of southern Nepal. Am J Epidemiol. 2007;165(2):203–211. doi: 10.1093/aje/kwj356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mullany LC, Darmstadt GL, Khatry SK, Tielsch JM. Traditional massage of newborns in Nepal: Implications for trials of improved practice. J Trop Pediatr. 2005;51(2):82–86. doi: 10.1093/tropej/fmh083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Falle T, Mullany LC, Thatte N, et al. Role of traditional birth attendants in neonatal health care in communities: A survey of practices in rural Nepal. J Pop Health Nutr. 2009;27(1):53–61. doi: 10.3329/jhpn.v27i1.3317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thatte N, Mullany LC, Khatry SK, Katz J, Tielsch J, Darmstadt GL. Knowledge, attitudes, and practices of delivery and newborn care: A qualitative study of traditional birth attendants in rural Nepal. Global Public Health. 2009;5(2):1–17. doi: 10.1080/17441690802472406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mullany LC, Katz J, Li YM, et al. Breast-feeding patterns, time to initiation, and mortality risk among newborns in southern Nepal. J Nutr. 2008;138(3):599–603. doi: 10.1093/jn/138.3.599. [DOI] [PMC free article] [PubMed] [Google Scholar]