Abstract
Epidemiological studies have shown that cigarette smoking is associated with an increased risk of midlife hot flashes; however, the effect of quitting smoking on this risk is unclear. The purpose of this study was to examine the effect of quitting smoking on hot flashes using data from 761 women aged 45 to 54 years of age at baseline followed for 1 to 7 years. Results showed that women who quit smoking were less likely to suffer from hot flashes, less likely to have severe hot flashes, and less likely to have frequent hot flashes than women who continued to smoke (OR = 0.55, 0.80, 0.76), but were more likely to suffer from any hot flashes, more severe hot flashes, and more frequent hot flashes than women who never smoked (OR = 2.55, 1.68, 1.46). Subset analysis of the 353 women who had ever smoked found that women who had quit smoking for longer than 5 years had significantly lower odds, severity, and frequency of hot flashes than women who had continued smoking (OR = 0.36, 0.62, 0.63) or women who had quit in the previous 5 years (OR = 0.66, 0.77, 0.69). These findings suggest that that early smoking cessation programs may improve women’s well-being during the menopausal transition.
Keywords: menopause, hot flashes, smoking, smoking cessation
1. Introduction
Approximately 75% of perimenopausal women will experience vasomotor symptoms, which include hot flashes [1]. The economic cost of hot flashes is significant, as experiencing this symptom can lead to medical treatment, physician visits, laboratory testing, and loss of productivity [2]. Women experiencing hot flashes also report a decrease in quality of life [3] and level of self-worth [4].
The risk and severity of hot flashes has been shown to vary with exercise [4], ethnicity [5], and body mass index (BMI) [6]. One factor that has consistently been shown to be associated with and increased risk of midlife hot flashes is history of cigarette smoking [5–12]. Cohort studies have found that current smokers had increased risk of hot flashes [5–7,12], severe hot flashes [7], and discomfort due to symptom [8]. A cross-sectional survey of perimenopausal women found that current smokers were at an increased risk for moderate to severe hot flashes and daily hot flashes, and that the risk for hot flashes increased with the amount smoked [10]. Similarly, a cross-sectional study of perimenopausal women found that current and former smokers, when compared to non-smokers, had higher odds of experiencing hot flashes and of severe hot flashes [11]. The mechanism by which smoking is associated with hot flashes is not clear, but several studies suggest that cigarette smoking may decrease levels of bioavailable estrogen [13–16] through increased hepatic metabolism [17], and low estrogen levels could explain the increased risk of hot flashes. However, the effect of quitting smoking on hot flashes has never been specifically studied, and no studies of former smokers have considered the amount of time since quitting. As quitting smoking is one of the personal modifications a woman can make to alter her health [18], it is important to precisely determine the benefit to be gained by quitting smoking.
Thus, the goal of this study was to explicitly calculate the effect of quitting smoking on the risk, severity, and frequency of hot flashes. Specifically, we established the time-dependent effect of quitting smoking on hot flashes, to determine the benefit associated with quitting over time.
2. Materials and Methods
The study design for the parent study is described in detail elsewhere [6]. Briefly, a cohort study of hot flashes among women 45–54 years of age was conducted starting in 2006 among residents of Baltimore and its surrounding counties. Women were recruited by mail, and were included if they were in the target age range, had intact ovaries and uteri, and were pre- or perimenopausal. Exclusion criteria consisted of pregnancy, a history of cancer, exogenous female hormone or herbal/plant substance, and no menstrual periods within the past year. Participants made a baseline clinic visit, which included measurement of height and weight to calculate body mass index (BMI) and completion of a detailed 26-page baseline survey. Participants were asked to complete a brief questionnaire during a clinic visit 3 weeks after the baseline visit, then annually after that. This questionnaire repeated all previous questions about hot flashes and smoking, and BMI was calculated during the visit. Menopausal status was defined as follows: premenopausal women were those who experienced their last menstrual period within the past 3 months and reported 11 or more periods within the past year; perimenopausal women were those who experienced 1) their last menstrual period within the past year, but not within the past 3 months, or 2) their last menstrual period within the past 3 months and experienced 10 or fewer periods within the past year; postmenopausal women were those women who had not experienced a menstrual period within the past year. Follow-up was discontinued for women if they reported hormone therapy, an oophorectomy, or a cancer diagnosis. At the year 4 visit, follow-up was discontinued for women determined to be postmenopausal. This analysis included all participants enrolled as of February 2015, and consisted of the information gathered in the baseline survey and in the annual follow-up surveys.
For this analysis, history of hot flashes consisted of 3 variables collected in the survey. Participants were asked if they had, ever (at baseline) or in the last year (for follow-ups), had hot flashes (yes/no/don’t know); the response to this was the dependent variable for a logistic regression analysis. Participants were also asked the severity of their hot flashes (none/mild/moderate/severe) and the frequency of their hot flashes (never/monthly/weekly/daily). These responses were dependent variables for separate ordinal logistic regression analyses. All variables related to the history of hot flashes were time varying; the variable “had a hot flash” related only to hot flashes previous to the survey date, and did not include future information about the development of hot flashes.
The full data set was used to analyze associations with the history of hot flashes using logistic regression. If the response to the survey question “Have you experienced hot flashes?” is defined as Y, where the Yi are independent Bernoulli random variables where 1 indicates the answer “yes”, E [Yi]=π(Xi), Var(Yi)=π(Xi)(1−π(Xi)), and Xi is the vector of explanatory variables for sample i, then
| (1) |
where β is the vector of the effects of explanatory variables, zi is the indicator of the individual, and γ is normally distributed with a mean of 0 and variance of . A random effects model was used as results from the same individual were assumed to not be independent. Bivariate logistic regression was used to identify potential covariates for a multivariate logistic regression. For this logistic model, Xi initially contained the following variables: smoking history (never smoked, former smoker, current smoker), menopausal status (premenopausal, perimenopausal, or postmenopausal), education level (did not graduate college or graduated college), race (white or non-white), BMI, amount smoked (≤25 packs/year or >25 packs/year), and type of cigarette smoked (filtered or unfiltered). Amount smoked was dichotomized, as the distribution of the continuous variable was highly skewed. Smoking history, menopausal status, and BMI were all time varying. The full model also considered interactions between BMI category and smoking history. Backwards model selection was performed using the likelihood ratio test, with factors maintained at a level of α = 0.1. Confidence intervals (CI) were calculated using the likelihood profile method with a cutoff of 10−5.
A subset of the data, consisting of all women self-reporting as current or former smokers, was used to analyze associations with the history of hot flashes given the years since quitting, where three different configurations of Xi were considered, all including the covariates listed above plus a term for years since quitting. This term was either: a linear term (years since quitting, with a value of 0 for current smokers), a large categorical variable {0, (0–5], (5–15], (15–25], >25}, and a reduced categorical variable {0, (0–5], >5}. Model selection proceeded as with the full data set logistic regression analysis above.
The severity and frequency of hot flashes were analyzed using ordinal logistic regression with a proportional odds model. In the case of severity, Y is defined as the response to the survey question “How severe are your hot flashes?”, where 0 indicates “no hot flashes”, 1 indicates “mild”, 2 indicates “moderate”, and 3 indicates “severe”. In the case of frequency, Y is defined as the response to the survey question “How often do you experience hot flashes?”, where 0 indicates “never”, 1 indicates “monthly”, 2 indicates “weekly”, and 3 indicates “daily”. In this model, E [Yik]=πk(Xi), Var(Yik)=πk(Xi)(1−π(Xi)), Xi is the vector of explanatory variables for sample i, and
| (2) |
where β, zi, and γ are as above, and αk is the intercept for the kth level of Y. Model selection proceeded as with the full data set logistic regression analysis above. This model was fit to all configurations of Xi, with the full data set and with the subset as appropriate.
As baseline reporting of hot flashes differed from following years, sensitivity analyses were performed by omitting the baseline visit from each of the analyses. Model fitting proceeded as detailed above, and results were compared.
Logistic regression was performed using the glmer function of the lme4 package [19] and the proportional hazards model was fit using the ordLORgee function of the multgee package [20]. Models were fit with individual as a random effect to account for within-woman correlation. Proportional odds assumptions were tested by visualization of the empirical cumulative logit function. All analyses were performed in R, using the Revolution R Enterprise system [21].
3. Results
3.1 Description of Data
There were 2,275 observations of 761 women over a 7 year period, with the number of observations per woman varying from 1 to 7. Table 1 shows the baseline characteristics of the women in the study and their association with hot flashes. Compared to women not experiencing hot flashes, women experiencing hot flashes were more likely to have not graduated from college, to be non-white, and to have a BMI of ≥30. Women experiencing hot flashes were also more likely to be a current or former smoker than women not experiencing hot flashes.
Table 1.
Baseline characteristics of women in the cohort by self-reported history of hot flashes (yes is ever had hot flashes) at time of entrance to the study
| Parameter | Level | Yes (n = 347) | No (n = 411) | p-value1 | ||
|---|---|---|---|---|---|---|
|
| ||||||
| n | % | n | % | |||
| Age, years | 45–49 | 184 | 37.1 | 312 | 62.9 | <0.001 |
| 50–54 | 164 | 61.9 | 101 | 38.1 | ||
|
| ||||||
| Education2 | Did not graduate college | 147 | 53.6 | 127 | 46.4 | 0.002 |
| Graduated college | 201 | 41.5 | 283 | 58.5 | ||
|
| ||||||
| Race | White | 216 | 43.0 | 286 | 57.0 | 0.001 |
| Non-white | 132 | 51.4 | 125 | 48.6 | ||
|
| ||||||
| Body Mass Index (kg/m2) | ≥30 | 218 | 47.5 | 241 | 52.5 | <0.001 |
| <30 | 130 | 43.0 | 172 | 57.0 | ||
|
| ||||||
| Cigarette smoking | Current | 49 | 62.0 | 30 | 38.0 | <0.001 |
| Former | 141 | 51.8 | 131 | 48.2 | ||
| Never | 157 | 38.4 | 252 | 61.6 | ||
From a bivariate logistic model for the probability of hot flashes.
Not all women reported education (n=3), race (n=2), or cigarette smoking (n=1)
Table 2 shows the distribution of hot flash severity and frequency by smoking history. Fifteen women quit smoking during the study, and this change in status was included in the analysis. A higher proportion of current and former smokers experienced moderate and severe hot flashes. Monthly hot flashes were the most common in all groups, but current and former smokers were numerically more likely than non-smokers to have hot flashes at higher frequencies. The assumption of proportional odds was met for the ordinal logistic regression analysis.
Table 2.
Hot flash experience at baseline among women reporting a history of hot flashes (at time of entrance to the study) in the cohort, by smoking history
| Parameter | Level | Current Smoker (n = 149) | Former Smoker (n = 52) | Never Smoked (n = 175) | p-value1 | |||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| n | % | n | % | n | % | |||
| Severity of hot flashes2 | None | 30 | 37.5 | 131 | 47.8 | 252 | 60.4 | <0.001 |
| Mild | 10 | 12.5 | 39 | 14.2 | 63 | 15.1 | ||
| Moderate | 33 | 41.2 | 83 | 30.3 | 77 | 18.5 | ||
| Severe | 5 | 6.2 | 16 | 5.8 | 13 | 3.1 | ||
|
| ||||||||
| Frequency of hot flashes2 | None | 30 | 37.5 | 131 | 47.8 | 252 | 60.4 | <0.001 |
| Monthly | 16 | 20 | 60 | 21.9 | 70 | 16.8 | ||
| Weekly | 15 | 18.8 | 40 | 14.6 | 35 | 8.4 | ||
| Daily | 13 | 16.2 | 27 | 9.9 | 40 | 9.6 | ||
From a chi-square model
Not all women reporting hot flashes reported severity (n=8) or frequency (n=31) of those hot flashes
3.2 Effect of Current, Former, and Never Smoking
The results of the analyses based on all data are shown in Table 3. A history of smoking significantly increased the odds of hot flashes, but direct comparison of women who quit smoking with women who continued to smoke (data not shown) showed that women who quit smoking were less likely to suffer from hot flashes (OR = 0.63), less likely to have severe hot flashes (OR = 0.78), and less likely to have frequent hot flashes (OR = 0.78). Likewise, current and former smokers both suffered significantly more severe and more frequent hot flashes than non-smokers, but both severity and frequency of hot flashes were slightly decreased for those who had quit smoking. Amount of smoking and BMI were not significant factors and were not included in any of the final models. Post-menopausal women and non-white women were more likely to report any, more severe, and more frequent hot flashes than perimenopausal women or white women, respectively. Pre-menopausal women reported significantly less severe and less frequent hot flashes than their perimenopausal counterparts, and were significantly less likely to suffer from hot flashes at all. Women who had graduated college were less likely to experience hot flashes than women who had not graduated college, but the effect was not significant and education was not significantly related to severity or frequency of hot flashes. Sensitivity analyses showed consistent results with and without baseline data (results not shown).
Table 3.
Results of a logistic regression for the probability of hot flashes and ordinal regressions for the severity and frequency of hot flashes, based on a longitudinal data analysis with perimenopausal women over 7 years.
| Parameter | Level | Probability of Hot Flashesa | Severity of Hot Flashesb | Frequency of Hot Flashesc |
|---|---|---|---|---|
|
| ||||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | ||
| Smoking (never smoked is referent) | former smoker | 2.55 (1.51, 4.42) | 1.66 (1.29, 2.13) | 1.41 (1.08, 1.83) |
| current smoker | 4.01 (1.80, 9.25) | 2.13 (1.44, 3.15) | 1.80 (1.22, 2.65) | |
|
| ||||
| Menopausal status (perimenopausal is referent) | post-menopausal | 1.61 (0.97, 2.69) | 1.18 (0.96, 1.45) | 1.27 (1.02, 1.58) |
| pre-menopausal | 0.05 (0.03, 0.08) | 0.28 (0.23, 0.34) | 0.20 (0.17, 0.25) | |
|
| ||||
| College graduate (less than college is referent) | 0.82 (0.47, 1.4) | NS | NS | |
|
| ||||
| Race (non-white is referent) | 0.48 (0.28, 0.83) | 0.65 (0.51, 0.84) | 0.68 (0.52, 0.88) | |
Includes 761 women and 2,275 observations over 7 years.
Includes 760 women and 2,269 observations over 7 years.
Includes 750 women and 2,207 observations over 7 years.
NS: Not significant (p > 0.1, removed from final model)
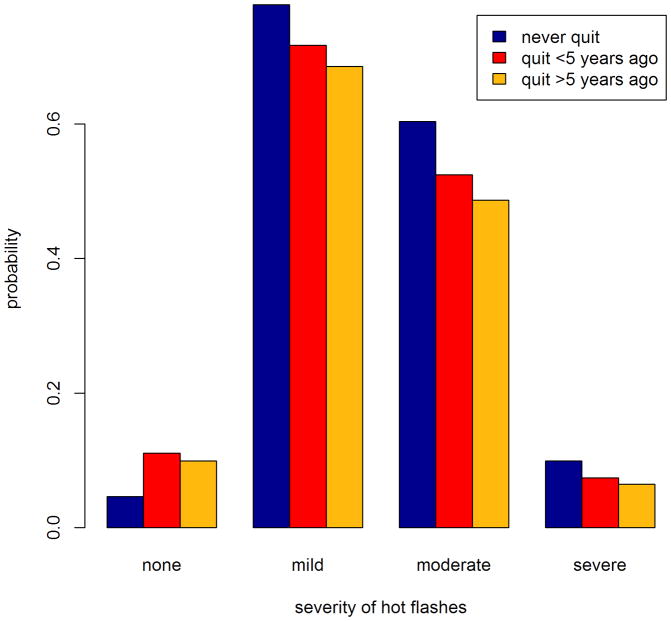
3.3 Effect of Time Since Quitting
The results of the analyses based on the subset of women who ever smoked are shown in Table 4 and Figure 1. The linear variable for years quit was not significantly associated with any outcome (data not shown). The categorical variable with 5 categories for years since quitting was significantly associated with all outcomes, but estimates were similar for categories representing quitting for more than 5 years (data not shown). Therefore, the categorical variable with 3 categories for years since quitting is reported here. Quitting smoking for longer than 5 years decreased the odds, severity, and frequency of hot flashes compared to never quitting. Quitting smoking for longer than 5 years also decreased the severity (OR = 0.86) and frequency of hot flashes (OR = 0.81) compared to quitting for less than 5 years, which had an association with a decrease in risk, severity, and frequency of hot flashes compared to never quitting. Type of cigarette smoked, amount of smoking, BMI, race, and education were not significant factors and were not included in any of the final models. Among the ever smokers, post-menopausal women were at slightly higher risk for ever experiencing hot flashes as well as experiencing more severe and more frequent hot flashes, and pre-menopausal women were at significantly lower risk, compared to peri-menopausal women. Sensitivity analyses showed consistent results with and without baseline data (results not shown).
Table 4.
Results of a logistic regression for the probability of hot flashes and ordinal regressions for the severity and frequency of hot flashes, based on a longitudinal data analysis of a subset of perimenopausal women, those who reported having ever smoked, over 7 years.
| Parameter | Level | Probability of Hot Flashesa | Severity of Hot Flashesb | Frequency of Hot Flashesc |
|---|---|---|---|---|
|
| ||||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | ||
| Years since quitting smoking (current smoker is referent) | ≤5 | 0.39 (0.11, 1.38) | 0.72 (0.41, 1.27) | 0.83 (0.46, 1.49) |
| >5 | 0.44 (0.18, 1.02) | 0.62 (0.42, 0.92) | 0.67 (0.44, 1.03) | |
|
| ||||
| Menopausal status (perimenopausal is referent) | post-menopausal | 1.36 (0.65, 2.9) | 1.04 (0.8, 1.35) | 1.31 (0.96, 1.8) |
| pre-menopausal | 0.04 (0.02, 0.08) | 0.32 (0.24, 0.42) | 0.22 (0.17, 0.3) | |
Includes 353 women and 992 observations over 7 years.
Includes 352 women and 987 observations over 7 years.
Includes 347 women and 951 observations over 7 years.
NS: Not significant (p > 0.1, removed from final model)
Figure 1.
Probability of hot flashes, by level of severity and smoking history, predicted by analysis of a cohort study of perimenopausal women. Probability of no hot flashes was predicted by a logistic regression model. Probability of different levels of severity was predicted by a proportional hazards model. All other covariates were assumed to be at baseline level.
4. Discussion
Results of this prospective cohort study show that smoking increases the risk, severity and frequency of hot flashes, but that quitting smoking lessens this effect. To our knowledge, this is the first study to consider time as a factor in the effect of quitting smoking on hot flashes.
This study is also unique, as it examined the issue of quitting smoking and midlife hot flashes using longitudinal data, which allowed for the capture of symptom development over time; women in the perimenopausal period may begin to experience hot flashes or experience a change in frequency and severity as they progress towards menopause. Cross-sectional studies during the perimenopausal period may underestimate the risk, as they are able only to account for symptoms that have already occurred. In fact, our estimates for the effect of smoking history on the probability of hot flashes indicate a higher risk associated with smoking than previously reported. Previous analysis of these and similar data [10,11] found that the increased risk of hot flashes was borderline to non-significant for former smokers, and that the risk for current smokers was 1.5–3 fold, as opposed to the OR of 4 reported here. Those analyses, however, were based on cross-sectional analysis of baseline information. The addition of the longitudinal element to the analysis, allowing capture of recent changes in smoking history and hot flash symptoms, increases the sensitivity of the study. Our estimates for the effect of smoking history on the severity and frequency of hot flashes are similar to that reported previously. The use of ordinal logistic regression enabled us to determine a more precise estimate, however, as previous studies used simple logistic regression with grouped categories (moderate or severe vs. never and weekly or daily vs. never).
The analysis of time since quitting was able to show that the advantages of quitting smoking were more apparent after 5 years (Figure 1). This indicates that there may be lingering biological effects on circulating estrogen levels after quitting smoking. These results may strengthen arguments for early smoking cessation, as this is one area in which the health impacts are not immediate. We were unable to detect a linear trend between years since quitting and hot flashes, however. Analysis of the 5-category variable for time since quitting showed no additional effect after 5 years, so it is possible that the effects of quitting do not increase indefinitely. The results reported here are based on ongoing data collection. It may be of interest to return to the study at a later time, when all subjects have been followed for as long as possible, to see if the improved power allows for a more exact relationship between time since quitting and hot flashes to be resolved.
As the mechanism behind the association between smoking and hot flashes is unknown, we can only speculate on the mechanism by which quitting smoking decreases hot flash risk, severity, and frequency. It has been proposed that the risk from cigarette smoking is due to alterations in hormone levels [13–16], via changes to the metabolism of those hormones [17]. If this is the case, the effect of quitting could be related to changes in metabolic pathways; evidence suggests that smoking cessation of just 6 weeks can improve hepatic metabolism [22]. Others have suggested that smoking interferes with thermoregulatory pathways associated with hot flashes, [23,24] potentially through norepinephrine changes [24]. Smoking has been found to increase norepinephrine levels via the monoamine oxidase pathway [25] and the effect appears to be long-lasting [26], which would explain the lack of significant effect for women who quit smoking for less than 5 years. Further elucidation of the mechanism of hot flashes would allow a causal pathway to be better understood.
5. Conclusions
This study has demonstrated the benefit to be gained from quitting smoking with regards to menopausal symptoms. These results may be of use to health providers in encouraging women to quit smoking.
Highlights.
We analyzed risk, severity, and frequency of hot flashes in peri-menopausal women.
A history of ever smoking increased risk, severity, and frequency of hot flashes.
Quitting smoking decreased risk, severity, and frequency of hot flashes.
Quitting smoking was only effective in decreasing hot flashes after 5 years.
Acknowledgments
We would like to thank the participants and staff who made the Women’s Mid-Life Health Study possible. This work was supported by NIH (R01 AG18400).
Funding
This study was funded by a grant from the National Institute on Aging (R01 AG18400).
Footnotes
Competing interests
The authors declare no conflict of interest
Contributors and their role
Rebecca L. Smith, DVM MS PhD: conception, design, and analysis of statistical study and preparation of the manuscript.
Jodi A. Flaws, PhD: conception, design, and implementation of the Women’s Mid-Life Health Study and preparation of the manuscript.
Lisa Gallicchio, PhD: conception, design, and implementation of the Women’s Mid-Life Health Study and preparation of the manuscript.
Ethical Approval
Written informed consent was obtained for all participants and the institutional review boards of the University of Illinois and Johns Hopkins University approved all protocols.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.United States Census. 2000 [Google Scholar]
- 2.Rodgers J, Martin CR, Morse RC, Kendell K, Verrill M. An investigation into the psychometric properties of the Hospital Anxiety and Depression Scale in patients with breast cancer. 2005;12:1–12. doi: 10.1186/1477-7525-3-Received. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mishra G, Kuh D. Perceived change in quality of life during the menopause. Soc Sci Med. 2006;62:93–102. doi: 10.1016/j.socscimed.2005.05.015. [DOI] [PubMed] [Google Scholar]
- 4.Elavsky S, McAuley E. Physical activity, symptoms, esteem, and life satisfaction during menopause. Maturitas. 2005;52:374–85. doi: 10.1016/j.maturitas.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 5.Gold EB, Colvin A, Avis N, Bromberger J, Greendale GA, Powell L, et al. Longitudinal analysis of the association between vasomotor symptoms and race/ethnicity across the menopausal transition: Study of women’s health across the nation. Am J Public Health. 2006;96:1226–35. doi: 10.2105/AJPH.2005.066936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gallicchio L, Miller SR, Kiefer J, Greene T, Zacur HA, Flaws JA. Change in body mass index, weight, and hot flashes: a longitudinal analysis from the midlife women’s health study. J Womens Health (Larchmt) 2014;23:231–7. doi: 10.1089/jwh.2013.4526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li C, Samsioe G, Borgfeldt C, Lidfeldt J, Agardh CD, Nerbrand C. Menopause-related symptoms: What are the background factors? A prospective population-based cohort study of Swedish women (the Women’s Health in Lund Area study) Am J Obstet Gynecol. 2003;189:1646–53. doi: 10.1016/S0002-9378(03)00872-X. [DOI] [PubMed] [Google Scholar]
- 8.Avis NE, Crawford SL, McKinlay SM. Psychosocial, behavioral, and health factors related to menopause symptomatology. Womens Health. 1997;3:103–20. [PubMed] [Google Scholar]
- 9.Dennerstein L, Smith AM, Morse C, Burger H, Green A, Hopper J, et al. Menopausal symptoms in Australian women. Med J Aust. 1993;159:232–6. doi: 10.5694/j.1326-5377.1993.tb137821.x. [DOI] [PubMed] [Google Scholar]
- 10.Whiteman MK, Staropoli CA, Langenberg PW, McCarter RJ, Kjerulff KH, Flaws JA. Smoking, body mass, and hot flashes in midlife women. Obstet Gynecol. 2003;101:264–72. doi: 10.1016/S0029-7844(02)02593-0. [DOI] [PubMed] [Google Scholar]
- 11.Gallicchio L, Miller SR, Visvanathan K, Lewis LM, Babus J, Zacur H, et al. Cigarette smoking, estrogen levels, and hot flashes in midlife women. Maturitas. 2006;53:133–43. doi: 10.1016/j.maturitas.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 12.Staropoli C, Flaws J, Bush T, Moulton A. Predictors of menopausal hot flashes. J Women’s Heal. 1998;7:1149–59. doi: 10.1089/jwh.1998.7.1149. [DOI] [PubMed] [Google Scholar]
- 13.Baron JA. Smoking and estrogen-related disease. Am J Epidemiol. 1984;119:9–22. doi: 10.1093/oxfordjournals.aje.a113730. [DOI] [PubMed] [Google Scholar]
- 14.Khaw K-T, Tazuke S, Barrett-Connor E. Cigarette smoking and levels of adrenal androgens in postmenopausal women. N Engl J Med. 1988;318:1705–9. doi: 10.1056/NEJM198806303182601. [DOI] [PubMed] [Google Scholar]
- 15.Kapoor D, Jones TH. Smoking and hormones in health and endocrine disorders. Eur J Endocrinol. 2005;152:491–9. doi: 10.1530/eje.1.01867. [DOI] [PubMed] [Google Scholar]
- 16.Tankó LB, Christiansen C. An update on the antiestrogenic effect of smoking: a literature review with implications for researchers and practitioners. Menopause. 2004;11:104–9. doi: 10.1097/01.GME.0000079740.18541.DB. [DOI] [PubMed] [Google Scholar]
- 17.Michnovicz J, Hershcoff R, Naganuma H, Bradlow H, Fishman J. Increased 2-hydroxylation of estradiol as a possible mechanism for the anti-estrogenic effect of cigarette smoking. N Engl J Med. 1986;315:1305–9. doi: 10.1056/NEJM198611203152101. [DOI] [PubMed] [Google Scholar]
- 18.Fisher TE, Chervenak JL. Lifestyle alterations for the amelioration of hot flashes. Maturitas. 2012;71:217–20. doi: 10.1016/j.maturitas.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 19.Bates D, Maechler M, Bolker B, Walker S, Christensen RHB, Singmann H, et al. Linear mixed-effects models using Eigen and S4. 2014 [Google Scholar]
- 20.Touloumis A. GEE Solver for Correlated Nominal or Ordinal Multinomial Responses. 2014 [Google Scholar]
- 21.Revolution R Enterprise. 2011 [Google Scholar]
- 22.O’Malley S, Wu R, Mayne S, Jatlow P. Smoking Cessation Is Followed by Increases in Serum Bilirubin, an Endogenous Antioxidant Associated With Lower Risk of Lung Cancer and Cardiovascular Disease. Nicotine Tob Res. 2014;16:1145–9. doi: 10.1093/ntr/ntu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kronenberg F, Downey Ja. Thermoregulatory physiology of menopausal hot flashes: a review. Can J Physiol Pharmacol. 1987;65:1312–24. doi: 10.1139/y87-208. [DOI] [PubMed] [Google Scholar]
- 24.Freedman RR. Physiology of hot flashes. Am J Hum Biol. 2001;13:453–64. doi: 10.1002/ajhb.1077. [DOI] [PubMed] [Google Scholar]
- 25.Rendu F, Peoc’h K, Berlin I, Thomas D, Launay JM. Smoking related diseases: The central role of monoamine oxidase. Int J Environ Res Public Health. 2011;8:136–47. doi: 10.3390/ijerph8010136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Launay JM, Del Pino M, Chironi G, Callebert J, Paoc’h K, Mégnien JL, et al. Smoking induces long-lasting effects through a monoamine-oxidase epigenetic regulation. PLoS One. 2009;4 doi: 10.1371/journal.pone.0007959. [DOI] [PMC free article] [PubMed] [Google Scholar]