Abstract
Objective
To evaluate the association between the patient-provider relationship, satisfaction with primary care provider’s (PCP) involvement and weight loss in a practice-based weight loss trial.
Methods
POWER was a practice-based randomized controlled behavioral weight loss trial. Participants completed questionnaires about patient-provider relationship and satisfaction with their PCPs’ involvement in the trial. PCPs completed a demographics and practice survey. The main outcome was the mean weight change from baseline to 24 months. We created mixed-effect models, accounting for the random effects of patients clustering with the PCP and the repeated outcome assessments within patient over time, and adjusted for randomization assignment, age, gender, race and clinical site.
Results
347 (of 415) were included. Mean age was 54.8 years, mean BMI was 36.3 kg/m2. Participants reported high quality patient-provider relationships (mean summary score=29.1 [range 14–32]). Patient-provider relationship quality was not associated weight loss in either the intervention or control groups. Among intervention participants, higher ratings of the helpfulness of the PCPs’ involvement was associated with greater weight loss (p=0.005).
Conclusion
Patient-provider relationship quality was not associated with weight loss in a practice-based weight loss trial but rating PCPs as helpful in the intervention was associated with weight loss.
Practice Implications
Partnering with PCPs to deliver weight loss programs may promote greater participant satisfaction and weight loss.
Keywords: obesity, primary care provider, patient-provider relationship
Introduction
Behavioral weight loss interventions in primary care settings have been shown to help patients lose weight and improve adverse health conditions associated with excess body weight such as hypertension and type 2 diabetes (1–8). The U.S. Preventive Services Task Force recommends that primary care providers (PCPs) “screen for obesity and offer or refer patients with a body mass index (BMI) of 30 kg/m2 to intensive, multicomponent behavioral interventions” (9, 10). However, in practice, only about one-third of obese adults receive an obesity diagnosis, less than half are advised to lose weight, and approximately one-fifth receive counseling for weight reduction (11, 12). Despite barriers to translating behavioral weight loss programs into practice (13, 13–16), many PCPs are interested in developing sustainable, practical strategies to promote and support patients’ weight loss efforts (16).
High quality patient-provider relationship, including trust, respect and effective communication, is associated with greater patient satisfaction and behavior change (17, 18). However, compared to people with normal weight, people with obesity report greater doctor shopping, reduced rapport-building dialog with their PCPs and lower levels of trust in their PCPs (19–21). Importantly, understanding the role of patient-provider relationship in primary care-based weight management is especially timely because of changes in reimbursement for obesity management in primary care settings. The Centers for Medicare and Medicaid Services (CMS) now reimburses PCPs for obesity management in primary care settings (22). The Practice-based Opportunities for Weight Reduction (POWER) Trial at Hopkins (2) was one of three NIH-funded trials to assess behavioral interventions for weight loss in primary care settings (23). The POWER trial documented that 2 behavioral interventions significantly reduced weight in obese patients with CVD risk factors (2). This trial was designed for PCPs and practices to have supportive role, including participant referral, review of weight loss progress reports at regularly scheduled clinic visits and outreach for participants who were not engaged (16). In this context, the POWER trial provided an ideal opportunity to assess the quality of patient-provider relationships, provider characteristics and their association with weight loss.
Our main objectives were to examine whether the quality of the patient-provider relationship or patients’ satisfaction with their PCPs involvement in the intervention were associated with weight loss. Our secondary objective was to examine the associations between PCP characteristics (e.g. age, BMI) and weight loss. We hypothesized that higher quality patient-provider relationships and greater patient satisfaction with their PCPs involvement in the trial would be associated with greater weight loss.
Methods
Overview of the POWER trial at Johns Hopkins
Details of the study design and main results of the trial have been published previously (2, 23). Hopkins POWER was a 3-arm randomized controlled trial evaluating the effectiveness of two 24-month practice-based behavioral weight loss interventions. For this analysis we combined the 2 intervention arms, which included the “Remote” arm with a weight-loss health coaches who provided behavioral via telephone and an “In-person” arm, which provided in-person coaching, off site from the primary care practices. Participants in the control arm met with a weight loss health coach once during the study at the time of randomization and, if desired, after the final data collection visit, and received brochures along with a list of recommended weight loss websites. Participants were obese adults, at least 21 years of age, with one or more cardiovascular risk factors (hypertension, hypercholesterolemia, and/or diabetes). They also had to be a patient in one of 6 participating primary care practices. For this analysis, we included 347 out of 415 POWER participants who completed the end of study patient-provider relationship questionnaire.
Forty-six PCPs enrolled participants from 6 primary care practices (about 60 patients per site, range 14 to 122, depending on practice size) in the Baltimore, MD area. PCPs publicized and recommended the POWER study to patients, reviewed weight progress reports during routine patient encounters for the two active intervention arms, and sent re-engagement letters to encourage study participation if intervention patients had not entered their weight on the study website nor talked with their coach for over two months.
Measure of patient-provider relationship quality
At the 24-month end-of-study outcome assessment visit, participants in both the intervention and control arms completed an 11-question instrument to assess patient-provider relationship (Appendix A). Six questions were adapted from the validated The Consumer Assessment of Healthcare Providers and Systems (CAHPS) Adult 12 month survey, 2.0, using the 4-point Likert response scale (1=never to 4=always), which asks patients how often their providers explained things clearly, listened carefully, showed respect, provided easy to understand instructions, knew their medical history and spent enough time (24, 25). A shorter 4-question version of these question showed high internal consistency with a Cronbach’s alpha of 0.86 and the items were strong predictors of other overall ratings of providers (24). We also included the CAHPS global rating of the provider (scale 0 to 10 with 0 being the worst and 10 being the best). Finally, we added a question to address patient-centeredness or the perception of “being known as a person,” which was previously identified as an important domain in the patient-provider relationship and related to patient health (26). We modified the framing of these questions by asking respondents to reflect about their care over the past 2 years, instead of 12 months, as the trial was 2 years long, and also asked whether they had changed providers in the past 2 years. We created a summary patient-provider relationship score by adding up the total responses from the 8 questions (and reversing the 2 opposite scales). This summary score had a minimum of 14 and a maximum of 32.
Measure of satisfaction with the PCP role in the study
Intervention group participants completed an additional questionnaire that we developed to assess the helpfulness of each of the intervention components (e.g., website, coach), including 2 questions about the helpfulness of their PCP’s involvement (“How helpful was your PCP’s involvement in the POWER study” and “How helpful was reviewing your self-monitoring weight graph with your PCP?”). Responses used a 5-point Likert scale (0=did not use or not at all helpful, 4=extremely helpful).
PCP Baseline Survey
At the beginning of the trial, we conducted a survey of participating PCPs to assess their demographic information. Two PCPs were unavailable to complete the survey. We assessed PCPs’ demographic (age, race/ethnicity, training, specialty, years in practice, weight/height), knowledge about weight management and frequency of weight management practices (e.g. BMI calculation, weight loss counseling and referral) (Appendix B). Because we did not identify a standard instrument for these questions, we adapted them from a previously developed needs assessment tool to create an obesity curriculum. PCPs selected ranges (0–9, 10–24, 25–49, 50–74, 75–100%) that best represented the percentage of obese adult patients in which they perform each of several weight management practices. Depending on the response distribution, aiming to have balanced numbers of PCPs in the final combined categories, we dichotomized the categories into the percentage of PCPs who perform each activity among either ≥ 50% or ≥ 75% of their obese patients (e.g. the percentage of PCPs who discuss weight management in ≥ 75% of obese patients).
Main outcome: Mean weight change at the end of the trial
The primary outcome for this analysis was mean difference in weight in lbs. from baseline to the end of the study, 24 months after randomization. Weights were measured on a high-quality, calibrated digital scale with the participant wearing light, indoor clothes without shoes. Trained, certified staff, masked to treatment assignment, obtained measurements.
Other covariates
Other covariates included participants’ demographic characteristics and medical history, which were collected by in-person or online surveys at baseline.
Statistical analysis
To assess the association between the patient-provider relationship, patient satisfaction with their PCPs’ involvement in the trial, provider characteristics and the outcome of mean weight change, we used likelihood-based, repeated-measure, mixed-effects models. We tested the summary patient-provider relationship score first and then developed models for each individual relationship quality term. These models accounted for the random effects of patients clustering within the PCP (since PCPs varied in the number of their patients who participated in the trial) and the repeated outcome assessments within patient over time, and adjusted for intervention vs. control randomization assignment, participant age, gender, race and clinical site. We presented results by combined intervention vs. control group because we believed that the association between PCP relationship quality and weight loss might differ by study arm (i.e. the intervention group received intense weight loss coaching, had weight reports reviewed by PCPs and lost more weight).
We also created models for adjusted mean weight change associated with each of the ratings of helpfulness of the PCP, and calculated an overall p-value using a likelihood ratio test.
We conducted 3 additional sensitivity analyses to assess the association between the primary outcome of weight loss at 24 months and the summary patient-provider relationship score. In the first sensitivity analysis we used multiple imputation to impute the summary score for the entire trial sample of N=415 and then re-evaluated the model results. In the second sensitivity analysis we used multiple imputation to impute the missing items for the satisfaction questionnaire for the entire sample in the combined intervention arms (N=277) and re-evaluated the model results. In the third sensitivity analysis, we excluded the 38 patients who reported changing PCPs in the past 2 years of the trial and evaluated the model results.
All analyses were conducted using the Statistical Analysis System (SAS) version 9.2 (SAS Institute, Carey, NC) or R 2.10.0.
Ethical review
The Institutional Review Board of The Johns Hopkins University School of Medicine approved this study.
Results
Participant characteristics
Table 1 shows the characteristics of the 347 out of the 415 participants in the POWER trial, who completed the end-of-study patient-provider questionnaires and were included in the sample. Participants attended an in-person end-of-study outcome assessment visit in order to complete this questionnaire, reducing the response rate. 239 (68.9%) were in one of the 2 intervention arms of the study.
Table 1.
Characteristics1 of 347 study participants who completed the patient-provider relationship questionnaire in the Hopkins POWER study, by Intervention and Control groups
| Total N=347 |
Intervention2 N=239 |
Control N=108 |
p-value | |
|---|---|---|---|---|
| Age, years | 54.8 (10.0) | 55.1 (10.1) | 54.3 (9.8) | 0.52 |
| Gender | ||||
| Female | 62.5% | 62.3% | 63.0% | 0.91 |
| Race | 0.42 | |||
| African-American | 39.5% | 39.8% | 38.9% | |
| White | 57.6% | 58.2% | 56.5% | |
| Other races | 2.9% | 2.1% | 4.6% | |
| Education | 0.47 | |||
| High school graduate or less | 8.9% | 8.8% | 9.3% | |
| Some college | 30.0% | 28.0% | 34.3% | |
| College graduate | 61.1% | 63.2% | 56.5% | |
| Health insurance3 | 0.06 | |||
| Commercial only | 87.0% | 87.0% | 87.0% | |
| Medicare or Medicaid | 12.1% | 13.0% | 10.2% | |
| Employment | 0.37 | |||
| Employed | 74.4% | 74.5% | 74.1% | |
| Retired | 16.4% | 17.6% | 13.9% | |
| Other | 9.2% | 8.0% | 12.0% | |
| Household income | 0.98 | |||
| Less than $50,000 | 21.9% | 21.8% | 22.2% | |
| $50–99,000 | 37.5% | 37.2% | 38.0% | |
| 100,000 or more | 40.6% | 41.0% | 39.8% | |
| Medical conditions | ||||
| Diabetes | 22.8% | 22.6% | 23.2% | 0.91 |
| Hypertension | 75.2% | 74.9% | 75.9% | 0.84 |
| Hyperlipidemia | 70.6% | 69.9% | 72.2% | 0.66 |
| Baseline measures | ||||
| Weight, lbs | 227.5 (39.7) | 227.0 (40.0) | 228.4 (39.1) | 0.76 |
| BMI, kg/m | 36.3 (5.1) | 36.2 (5.1) | 36.5 (5.2) | 0.63 |
| End of study measures | ||||
| Weight loss at 24 months (lbs)4 | 9.0 (18.4) | 11.8 (19.2) | 2.8 (14.9) | <0.001 |
| % weight loss at 24 months4 | 3.9 (7.6) | 5.1 (7.9) | 1.1 (6.2) | <0.001 |
| # Weight reports reviewed with PCP | 2.98 (1.90 | 2.2 (1.6) | n/a | n/a |
| # Coaching contacts | 24.4 (7.3) | 24.7 (7.5) | n/a | n/a |
| Patient-PCP relationship summary score5 | 29.1 (3.6) | 29.2 (3.7) | 29.1 (3.4) | 0.92 |
Mean (Standard Deviation) or %
2 intervention groups (remote and in-person) were combined
3 participants were uninsured. P value was across comparison between Commercial, Medicaid, Medicare and no insurance categories.
N=346 (instead of 347) because 1 participant was censored at 24 months because of having bariatric surgery.
Summary score calculated as sum of 8 questions. Possible range was 14–32 but calculated range was 28–32. In Table 2 the summary score was assessed as a continuous variable (n=336 for this analysis because we required all 8 questions to be completed)
Abbreviations: BMI=body mass index; PCP=primary care provider
In the study sample, 62.5% were female, 39.5% were African American and 61.1% were college graduates. The most common co-morbid medical condition was hypertension (75.2%) followed by hyperlipidemia (70.2%) and diabetes (23.1%). BMI at study entry was 36.3 (SD 5.1). The majority of participants had commercial health insurance (87%). (Table 1).
At the end of the study, the intervention group participants had a mean weight loss of 11.8 lbs. (SD 19.2) and control group participants had mean weight loss of 2.8 lbs. (SD 14.9). During the 24-month study, intervention group participants had a mean of 24.7 (SD 7.5) coaching contacts and a mean of 2.2 (SD 1.6) clinic visits when the PCP reviewed the weight progress reports. 11% reported changing PCPs during the study. Compared to the 68 participants who did not respond to the end-of-study patient-provider questionnaire, respondents tended to be older, had higher education and achieved greater weight loss at 24 months (data not shown).
Provider and practice characteristics
Table 2 shows the characteristics of the 44 PCPs from 6 primary care practices with participants in trial. Mean age was 46.3, 56.8% were female, 15.9% were African American, 59.1% were Caucasian and 25% were from other racial groups. Four PCPs were nurse practitioners and 42 were physicians. Each PCP had a mean of 8 patients in the trial. The majority of PCPs reported at least intermediate knowledge of weight management and 47% reported calculating BMI or assessing motivation to lose weight in most (>75%) obese patients. 83% reported never or rarely prescribing weight loss medications.
Table 2.
Characteristics and weight management clinical practices of the 44 PCPs with patients in the Hopkins POWER trial
| PCPs N=44 |
|
|---|---|
| PCP characteristics, Mean (SD) or % | |
| Mean Age (SD) | 46.3 (9.4) |
| Gender | |
| Female | 56.8% |
| Race | |
| African American | 15.9% |
| Caucasian | 59.1% |
| Other races | 25.0% |
| Mean BMI (SD) | 24.4 (3.1) |
| General internal medicine (vs. Family Practice) training | 75.0% |
| Physician (vs Nurse Practitioner) | 90.9% |
| Mean years in practice (SD) | 16.9 (9.5) |
| Past participation in research studies | 60.0% |
| Mean number of patients in Hopkins POWER trial (SD) | 7.9 (6.6) |
| Weight management clinical practices 1,2, % | |
| Has intermediate/advanced knowledge of weight management | 91.7% |
| Calculate BMI in 75% or more of patients | 47.2% |
| Discuss weight management in 75% or more of your obese patients | 41.7% |
| Assess motivation to lose weight in 75% or more of obese patients | 25.0% |
| Discuss dietary recommendations for weight loss in 50% or more of obese patients | 80.6% |
| Discuss specific physical activity recommendations related to losing or maintaining weight in 50% or more of obese patients | 66.7% |
| Provide behavioral counseling and help setting goals in >50% or more obese patients | 40.0% |
| Refer 50% or more obese patients to a commercial weight loss program | 28.6% |
| Prescribe weight loss medication never or rarely | 83.3% |
8 PCPs did not respond the questions about weight management practices (n=36)
Categories were dichotomized into the percentage of PCPs who perform each activity among either ≥ 50% or ≥ 75% of their obese patients (e.g. the percentage of PCPs who discuss weight management in ≥ 75% of obese patients) to have balanced numbers of PCPs in the final combined categories.
Abbreviations: BMI=body mass index; PCP=primary care provider; SD=standard deviation
Over the two-year trial, two PCPs switched to another practice in the trial and five PCPs left all the participating practices. Two new PCPs joined the trial. 11% of study participants reported changing PCPs during the trial, and among these 47% changed within their same practice. Compared to the 309 participants who did not change PCPs during the trial, the 38 participants who reported changing PCPs were more likely to be White (vs. African American) but there were no other differences by age, income, baseline weight or weight loss during the trial (data not shown). Those who changed PCPs reported lower patient-provider relationship quality scores (27.2 vs. 29.3 summary score, p<0.001).
Association between patient-provider relationship and weight change
Overall, participants rated the quality of their relationships with PCPs very highly with mean summary scores of 29.1 and 29.2 in the Intervention and Control groups, respectively, out of a total possible score of 32 (Table 1). Table 3 shows the mean weight change for participants who reported high patient-provider quality, i.e. rating “always” for each quality item, compared those who rated less than “always,” within the Intervention and Control groups. Overall, participants in the intervention group lost more weight than in the control group, regardless of ratings on the patient-provider items. We did not detect any statistically significant differences in weight change by high vs. lower patient-provider relationship ratings, within each treatment group. The treatment group interaction term for the quality item “explained things in a way that was easy to understand” was statistically significant (p<0.05). Participants in the control arm who rated the PCP as “always” explaining “things in a way that was easy to understand” had greater weight loss (7.2 lbs.) than those who rated the PCP as “always” explaining things clearly and had received the intervention (Table 3).
Table 3.
Weight change (lbs) at 24 months in Intervention and Control groups, by quality of the patient-provider relationship and PCP characteristics
| Intervention | Control | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Patient-PCP relationship (always vs. other)1 | Weight change (lbs) | 95% CI | p-value | Weight change (lbs) | 95% CI | p-value |
| Summary Score2 | −0.1 | −0.8,0.5 | 0.71 | −0.4 | −1.4,0.7 | 0.50 |
| Explained things so easy to understand3 | 3.7 | −2.1,9.4 | 0.21 | −7.2 | −16.3,1.8 | 0.11 |
| Knows my medical history | −3.0 | −8.1,2.1 | 0.24 | 2.1 | −5.3,9.5 | 0.58 |
| Knows me as a person | −0.9 | −5.5,3.7 | 0.71 | 1.4 | −5.4,8.2 | 0.69 |
| Shows me respect | 0.7 | −6.1,7.5 | 0.84 | −2.9 | −11.3,5.5 | 0.50 |
| Spends enough time with me | −1.0 | −6.1,4.1 | 0.69 | 2.5 | −4.7,9.7 | 0.50 |
| Involves me in decision making | −1.1 | −6.3,4.1 | 0.68 | 1.7 | −6.8,10.3 | 0.69 |
| Cares about me as a person | −2.3 | −7.7,3.1 | 0.40 | −0.4 | −7.7,7.0 | 0.92 |
| I would recommend my PCP | −3.1 | −9.8,3.6 | 0.37 | −3.5 | −12.2,5.3 | 0.43 |
| PCP characteristics (present vs. not) | ||||||
| PCP age ≥ 50 (vs. < age 50) | −1.6 | −6.2,3.0 | 0.49 | 0.5 | −6.3,7.4 | 0.88 |
| Physician (vs. Nurse Practitioner) as PCP4 | −10.8 | −20.4,−1.1 | 0.03 | −8.6 | −23.3,6.1 | 0.25 |
| BMI (per unit increase) | −0.2 | −1.0,1.5 | 0.68 | 0.3 | −1.1,0.7 | 0.65 |
| PCP had prior experience with research | −2.4 | −7.6,2.8 | 0.37 | −7.4 | −14.7,−0.18 | 0.04 |
Patient-PCP relationship scale was dichotomized as always vs. all other responses (never, sometimes and usually)
The summary score was calculated as the sum of all 8 questions (and reversing the 2 opposite scales). The summary score had a minimum of 14 and a maximum of 32
The interaction term for weight loss (in lbs) between the Intervention and Control groups had a p value < 0.05
Reference group gender non-concordance between the PCP and patient – i.e. male PCP with female patient or female PCP with male patient.
Four nurse practitioners were included, compared to 40 physicians, in the study
Abbreviations: BMI=body mass index; PCP=primary care provider; SD=standard deviation
In the intervention having a PCP who was a physician (vs. nurse practitioner) and in the control group, having a PCP who had previously been involved with research, were both associated with greater weight loss (−10.8 lbs, 95% CI: −20.4 to −1.1; −7.4 lbs, 95% CI: −14.7 to −0.18, respectively) (Table 3).
In sensitivity analyses using multiple imputation of the summary scores for the entire study sample (n=415) and in an analysis excluding the 38 participants who changed PCPs during the 2 year trial, the non-statistically significant relationship remained between mean weight change and patient-provider relationship summary score within the Intervention and Control groups.
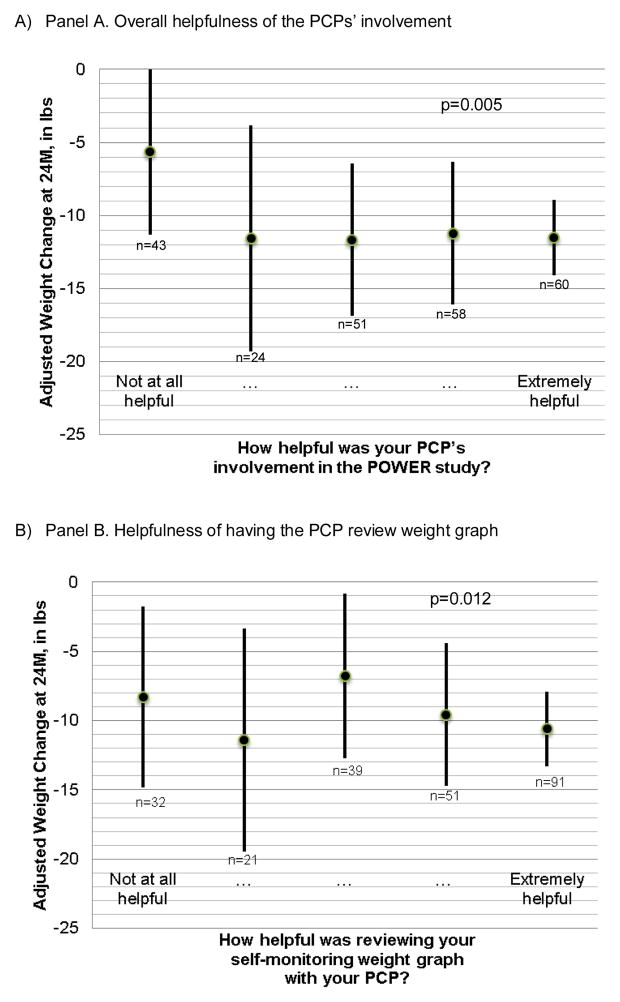
Association between satisfaction with PCP’s involvement and weight change
Among the 277 participants in the 2 combined intervention arms, 239 (86%) completed an end of study satisfaction survey. We identified a statistically significant trend (p=0.005) between a greater weight loss and higher ratings (not helpful to extremely helpful) of the overall “helpfulness of the PCP involvement in the POWER study” in adjusted analyses. Higher ratings of “PCP helpfulness in reviewing the weight graph” were also associated with greater weight loss (p-vale for the trend was p=0.012) (Figure 1). In the sensitivity analysis using multiple imputation of the missing items that addressed provider satisfaction the statistically significant relationship trend remained, but was weakened (p=0.017) (data not shown).
Figure 1.
Adjusted1 association between satisfaction with PCP involvement and weight change (lbs) among the 239 patients in intervention group of the Hopkins POWER trial
Footnote:
1. Analyses adjusted for the random effects of the PCP (since PCPs varied in the number of their patients who participated in the trial) and study visits, and participant age, gender, race and clinical site.
2. Overall p-vales were calculated using Likelihood ratio testing from mixed effects effect models.
Discussion and Conclusion
In this study of 347 patients who participated in the POWER practice-based weight loss trial, high quality patient-provider relationship was not associated with greater weight loss. However, overall, study participants had very positive perceptions of the quality of their relationships with PCPs. The lack of variation in quality ratings likely limited our ability to discern an association with weight change outcomes. We noted that control group participants who rated the PCP highly for communication, as “always” explaining “things in a way that was easy to understand,” had greater weight loss than intervention group participants with high ratings on this item. This finding may indicate a PCP-related weight loss effect unique to those who did not receive any intervention. Finally, among intervention group participants, we identified a consistent and significant relationship between high ratings of the helpfulness of PCPs’ involvement in the trial and greater weight loss.
High quality patient-provider relationships, consisting of empathy, effective communication, collaborative decision making, trust and feeling cared for, have been associated with appointment and medication adherence (27, 28) and patient satisfaction (29). Obese patients are at particularly high risk of suffering from poor quality patient-provider relationships, with evidence of decreased respect (30) and weight bias from providers (30, 31). Prior studies have focused on PCPs’ barriers to weight loss counseling (13–15, 32); however, PCPs may also be in a unique position to positively influence patients’ weight loss. In our prior work, we utilized the opportunity of the POWER trial to convene focus groups with these participating PCPs to explore their communication with patients and their perspective on their role in the trial (16, 33). PCPs described their longstanding continuity relationships with patients as important to their role in the study and also to patients’ successes (16). Given the importance of high quality patient-provider relationships in chronic disease management (34) and new primary care practice-based models for weight management (22), our current study complements our prior qualitative work by providing the patients’ perspective and assessment of the PCPs’ involvement in their weight loss. Our results showing the association between patient perception of PCP involvement and weight loss success are consistent with the PCPs’ perspective from focus groups, which described key aspects of their roles, such as providing accountability and cheerleading for patients, but remaining peripheral to the mostly coach-delivered behavioral weight management program (2, 16). Collectively, our findings indicate the importance of the PCP being involved at some level with weight management programs to improve patients’ satisfaction and successful weight loss, but it is unclear whether the quality of relationships with providers influences patient outcomes.
We identified several limitations of our study. First, the study was cross-sectional because we collected information about patient-provider relationship at a single time point, at the end of the study. Pre-post data would have enabled us to assess the change in the patient-provider relationship as a result of the patient’s participation in the study, as well as the stability of the relationship quality over time. Because of the cross-sectional design, we cannot determine directionality. For example, patients who successfully lost more weight may have been more satisfied with their PCPs’ involvement (e.g. because of referral into the program) or PCPs may have influenced their patients weight loss during the study, leading to both greater weight loss and participant satisfaction with their role. Either interpretation indicates the importance of the PCP being involved at some level with weight management programs to improve patients’ satisfaction and successful weight loss. However, because we stratified our analyses by intervention vs. control groups, we were able to assess the association between weight loss and end-of-study patient-provider relationship absent the effect of the intervention (i.e. the control), and did not detect any association in either group. Second, as mentioned above, ratings of the patient-provider relationship were right skew, indicating a possible ceiling effect with very high quality relationships, but limiting our ability to discern a difference between degree of relationship quality and weight loss. Notably, our results showing high relationship quality are comparable to data from the CAHPS Database, a repository of results from CAHPS surveys, with more than 90% of those participants endorsing the highest category (“Yes, definitely”) to the 6 patient-provider communication questions (35). Third, because coaching occurred off site from the individual practices, we were limited in the type of clinic utilization data we obtained, and only have records of when the patient was seen and a weight report was reviewed. Patient-provider relationship during the study may have been impacted by frequency of PCP contact, which we were unable to sufficiently adjust for in this analysis. Fourth, the study was based within a single trial in one geographic location, and may not be generalizable to other practices and weight management programs. Fifth, we did not account for the accumulation of type 1 error through multiple comparisons across patient-provider relationship quality items. Notably, we only identified one statistically significant relationship in the communication item and weight loss in the control group, which is a finding that could be by chance. However, the large difference in weight (weight loss of 7.2 lbs in the Control group for those with higher vs. lower ratings) may have clinical significance. Sixth, the response rate for the end of study surveys was 83.6% and we detected differences between survey respondents and non-respondents, indicating the possibility of selection bias. To explore this concern, we conducted sensitivity analyses using multiple imputation methods to impute the missing items and confirmed a statistically significant, but slightly weakened, association between satisfaction with the provider role and weight loss.
This study also had several strengths, including high rates of participant follow-up for the outcome of weight (2) and survey completion at the end of the study, the diversity of the population, and the commitment of the practices and PCPs to the study.
Conclusion
In conclusion, our study of 347 patients enrolled in the POWER weight loss trial showed an association between high levels of participant satisfaction with the PCP role and greater weight loss. We did not detect an association between the quality of the patient-provider relationship and weight loss. In designing future practice-based models for weight loss programs, successful engagement of PCPs has potential to improve patients’ satisfaction and weight loss success.
Our results show the high value of partnering with PCPs and their practices to develop innovative models to deliver weight loss programs, which may promote greater participant satisfaction, weight loss, and possibly retention, given the high level in this trial (2).
Supplementary Material
Highlights.
We surveyed participants in trial about their patient-provider relationship.
Weight loss was not associated with patient-provider relationship quality.
Satisfaction with the providers’ involvement in trial was associated with greater weight loss.
Partnering with PCPs may promote greater participant satisfaction and weight loss.
Practice Implications.
Our results have important implications for developing weight management programs integrated primary care settings and for the CMS policy to reimburse PCPs for weight loss counseling (22). Our results highlight that patients in this trial highly value their providers, through their report of very high quality relationships, and that they value their PCPs involvement in their weight loss efforts. We showed that patients who most highly rated the involvement of the PCP as helpful in the weight loss intervention were also likely to have lost the most weight, indicating a possible direct role of the PCP, such as through referring the patient to the program, supervising the titration of medications or providing encouragement over the 2-year trial. These results may indicate patients’ desire to have PCPs involved in their weight loss efforts, both directly and indirectly, through their supervision in multidisciplinary programs with health coaches, nutritionists or even in commercial weight loss programs. PCPs are ideally positioned to manage obesity as a long-term chronic illness, which requires sustained behavioral changes, and a combination of periodic intensive programs superimposed on longer term strategies aimed at small, incremental changes and weight maintenance. Several primary care team-based models might provide a framework for weight management programs that are based within or linked to primary care practices. The creation of a patient centered medical home (36) for obesity could include a multidisciplinary practice environment with health coaches, behavioral psychologists and nutritionists who work alongside PCPs. The POWER trial provided a unique example of health coaches who remotely delivered the intervention to patients who felt connected to PCPs and practices associated with the intervention (2). However, identifying methods to replicate this effective weight loss model in primary care requires creative reimbursement strategies, such as offering wellness benefits through employers, or within accountable care organizations that focus on chronic disease prevention (37).
Footnotes
Disclosure
This work was supported with a grant from the Johns Hopkins University Osler Center for Clinical Excellence at Johns Hopkins. POWER Hopkins was supported by a grant from the National Heart, Lung and Blood Institute (5U01HL087085-05). The original trial’s clinical trials.gov registration number was NCT00783315. Dr. Wendy Bennett is supported by a career development award from the National Heart, Lung, and Blood Institute, 5K23HL098476– 02. Dr. Nae-Yuh Wang is also supported by grants from the National Center for Advancing Translational Sciences, UL1 TR000424, and National Institute of Diabetes and Digestive and Kidney Diseases, P30DK079637. The original trial involved a collaboration with Healthways, Inc., a disease management company. Healthways provided coaching effort for the transtelephonic intervention and developed the website used in the intervention. Healthways provided some research funding to supplement NIH support. Under an institutional consulting agreement with Healthways, the Johns Hopkins University received fees for advisory services to Healthways during the POWER trial. Faculty members who participated in the consulting services received a portion of the University fees.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Leblanc ES, O’Connor E, Whitlock EP, Patnode CD, Kapka T. Effectiveness of primary care-relevant treatments for obesity in adults: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2011;155(7):434–47. doi: 10.7326/0003-4819-155-7-201110040-00006. [DOI] [PubMed] [Google Scholar]
- 2.Appel LJ, Clark JM, Yeh HC, Wang NY, Coughlin JW, Daumit G, et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med. 2011;365(21):1959–68. doi: 10.1056/NEJMoa1108660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA. 2003;289(16):2083–93. doi: 10.1001/jama.289.16.2083. [DOI] [PubMed] [Google Scholar]
- 4.Wadden TA, Volger S, Sarwer DB, Vetter ML, Tsai AG, Berkowitz RI, et al. A two-year randomized trial of obesity treatment in primary care practice. N Engl J Med. 2011;365(21):1969–79. doi: 10.1056/NEJMoa1109220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bennett GG, Warner ET, Glasgow RE, Askew S, Goldman J, Ritzwoller DP, et al. Obesity treatment for socioeconomically disadvantaged patients in primary care practice. Arch Intern Med. 2012;172(7):565–74. doi: 10.1001/archinternmed.2012.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tsai AG, Wadden TA. Treatment of obesity in primary care practice in the United States: a systematic review. J Gen Intern Med. 2009;24(9):1073–9. doi: 10.1007/s11606-009-1042-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wadden TA, Butryn ML, Hong PS, Tsai AG. Behavioral treatment of obesity in patients encountered in primary care settings: a systematic review. JAMA. 2014;312(17):1779–91. doi: 10.1001/jama.2014.14173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levine DM, Savarimuthu S, Squires A, Nicholson J, Jay M. Technology-assisted weight loss interventions in primary care: a systematic review. J Gen Intern Med. 2015;30(1):107–17. doi: 10.1007/s11606-014-2987-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McTigue KM, Harris R, Hemphill B, Lux L, Sutton S, Bunton AJ, et al. Screening and interventions for obesity in adults: summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2003;139(11):933–49. doi: 10.7326/0003-4819-139-11-200312020-00013. [DOI] [PubMed] [Google Scholar]
- 10.Moyer VA on behalf of the U.S. Preventive Services Task Force. Screening for and Management of Obesity in Adults: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2012 doi: 10.7326/0003-4819-157-5-201209040-00475. [DOI] [PubMed] [Google Scholar]
- 11.Ko JY, Brown DR, Galuska DA, Zhang J, Blanck HM, Ainsworth BE. Weight loss advice U.S. obese adults receive from health care professionals. Prev Med. 2008;47(6):587–92. doi: 10.1016/j.ypmed.2008.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bleich SN, Pickett-Blakely O, Cooper LA. Physician practice patterns of obesity diagnosis and weight-related counseling. Patient Educ Couns. 2011;82(1):123–9. doi: 10.1016/j.pec.2010.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang J, Yu H, Marin E, Brock S, Carden D, Davis T. Physicians’ weight loss counseling in two public hospital primary care clinics. Acad Med. 2004;79(2):156–61. doi: 10.1097/00001888-200402000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Kushner RF. Barriers to providing nutrition counseling by physicians: a survey of primary care practitioners. Prev Med. 1995;24(6):546–52. doi: 10.1006/pmed.1995.1087. [DOI] [PubMed] [Google Scholar]
- 15.Alexander SC, Ostbye T, Pollak KI, Gradison M, Bastian LA, Brouwer RJ. Physicians’ beliefs about discussing obesity: results from focus groups. Am J Health Promot. 2007;21(6):498–500. doi: 10.4278/0890-1171-21.6.498. [DOI] [PubMed] [Google Scholar]
- 16.Bennett WL, Gudzune KA, Appel LJ, Clark JM. Insights from the POWER Practice-Based Weight Loss Trial: A Focus Group Study on the PCP’s Role in Weight Management. J Gen Intern Med. 2013 doi: 10.1007/s11606-013-2562-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berry LL, Parish JT, Janakiraman R, Ogburn-Russell L, Couchman GR, Rayburn WL, et al. Patients’ commitment to their primary physician and why it matters. Ann Fam Med. 2008;6(1):6–13. doi: 10.1370/afm.757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones DE, Carson KA, Bleich SN, Cooper LA. Patient trust in physicians and adoption of lifestyle behaviors to control high blood pressure. Patient Educ Couns. 2012;89(1):57–62. doi: 10.1016/j.pec.2012.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gudzune KA, Bennett WL, Cooper LA, Bleich SN. Patients who feel judged about their weight have lower trust in their primary care providers. Patient Educ Couns. 2014;97(1):128–31. doi: 10.1016/j.pec.2014.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gudzune KA, Huizinga MM, Beach MC, Cooper LA. Obese patients overestimate physicians’ attitudes of respect. Patient Educ Couns. 2012;88(1):23–8. doi: 10.1016/j.pec.2011.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gudzune KA, Beach MC, Roter DL, Cooper LA. Physicians build less rapport with obese patients. Obesity (Silver Spring) 2013 doi: 10.1002/oby.20384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.The Centers for Medicare and Medicaid Services (CMS). Centers for Medicare and Medicaid (CMS) [Accessed March 16, 2015];Intensive Behavioral Therapy for Obesity. (CAG-00423N). http://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?&NcaName=Intensive%20Behavioral%20Therapy%20for%20Obesity&bc=ACAAAAAAIAAA&NCAId=253&.
- 23.Yeh HC, Clark JM, Emmons KE, Moore RH, Bennett GG, Warner ET, et al. Independent but coordinated trials: insights from the practice-based Opportunities for Weight Reduction Trials Collaborative Research Group. Clin Trials. 2010;7(4):322–32. doi: 10.1177/1740774510374213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hargraves JL, Hays RD, Cleary PD. Psychometric properties of the Consumer Assessment of Health Plans Study (CAHPS) 2.0 adult core survey. Health Serv Res. 2003;38(6 Pt 1):1509–27. doi: 10.1111/j.1475-6773.2003.00190.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Agency for Healthcare Research and Quality. [Accessed March 16, 2015];CAHPS Clinician & Group Survey- Adult Primary Care Questionnaire 1.0. http://www.cahps.ahrq.gov/content/products/CG/PROD_CG_CG40Products.asp.
- 26.Beach MC, Keruly J, Moore RD. Is the quality of the patient-provider relationship associated with better adherence and health outcomes for patients with HIV? J Gen Intern Med. 2006;21(6):661–5. doi: 10.1111/j.1525-1497.2006.00399.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cruz M, Roter DL, Cruz RF, Wieland M, Larson S, Cooper LA, et al. Appointment length, psychiatrists’ communication behaviors, and medication management appointment adherence. Psychiatr Serv. 2013;64(9):886–92. doi: 10.1176/appi.ps.201200416. [DOI] [PubMed] [Google Scholar]
- 28.Ratanawongsa N, Karter AJ, Parker MM, Lyles CR, Heisler M, Moffet HH, et al. Communication and medication refill adherence: the Diabetes Study of Northern California. JAMA Intern Med. 2013;173(3):210–8. doi: 10.1001/jamainternmed.2013.1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pollak KI, Alexander SC, Tulsky JA, Lyna P, Coffman CJ, Dolor RJ, et al. Physician empathy and listening: associations with patient satisfaction and autonomy. J Am Board Fam Med. 2011;24(6):665–72. doi: 10.3122/jabfm.2011.06.110025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huizinga MM, Cooper LA, Bleich SN, Clark JM, Beach MC. Physician respect for patients with obesity. J Gen Intern Med. 2009;24(11):1236–9. doi: 10.1007/s11606-009-1104-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring) 2009;17(5):941–64. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 32.Alexander SC, Cox ME, Boling Turer CL, Lyna P, Ostbye T, Tulsky JA, et al. Do the five A’s work when physicians counsel about weight loss? Fam Med. 2011;43(3):179–84. [PMC free article] [PubMed] [Google Scholar]
- 33.Gudzune KA, Clark JM, Appel LJ, Bennett WL. Primary care providers’ communication with patients during weight counseling: a focus group study. Patient Educ Couns. 2012;89(1):152–7. doi: 10.1016/j.pec.2012.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Beck RS, Daughtridge R, Sloane PD. Physician-patient communication in the primary care office: a systematic review. J Am Board Fam Pract. 2002;15(1):25–38. [PubMed] [Google Scholar]
- 35.CAHPS Database. 2015 Mar 16; https://cahps.ahrq.gov/cahps-database/index.html.
- 36.Stange KC, Nutting PA, Miller WL, Jaen CR, Crabtree BF, Flocke SA, et al. Defining and measuring the patient-centered medical home. J Gen Intern Med. 2010;25(6):601–12. doi: 10.1007/s11606-010-1291-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fisher ES, Shortell SM. Accountable care organizations: accountable for what, to whom, and how. JAMA. 2010;304(15):1715–6. doi: 10.1001/jama.2010.1513. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.