Abstract
Introduction
Medication adherence is essential in HIV care, yet provider communication about adherence is often suboptimal. We designed this study to improve patient-provider communication about HIV medication adherence.
Methods
We randomized 26 providers at three HIV care sites to receive or not receive a one-hour communication skills training based on motivational interviewing principles applied to medication adherence. Prior to routine office visits, non-adherent patients of providers who received the training were coached to discuss adherence with their providers. Patients of providers who did not receive the training providers were not coached. We audio-recorded and coded patient-provider interactions using the Roter Interaction Analysis System (RIAS).
Results
There was more dialogue about therapeutic regimen in visits with intervention patients and providers (167 vs 128, respectively, p=.004), with the majority of statements coming from providers. These visits also included more brainstorming solutions to nonadherence (41% vs. 22%, p=0.026). Intervention compared with control visit providers engaged in more positive talk (44 vs. 38 statements, p=0.039), emotional talk (26 vs. 18 statements, p<0.001), and probing of patient opinion (3 vs. 2 statements, p=0.009).
Conclusion
A brief provider training combined with patient coaching sessions, improved provider communication behaviors and increased dialogue regarding medication adherence.
Eighteen years into the era of highly active antiretroviral therapy (ART), medication adherence continues to be a serious barrier to effective treatment. Of the approximately 363,000 persons living with HIV in the US who are currently using antiretroviral therapy (ART), approximately 25% have detectable viral loads.1, 2 With strong evidence across multiple conditions outside the HIV context indicating that patient-provider communication is related to patient adherence and health outcomes,3, 4 many have suggested that effective patient-provider relationships and communication are likewise of critical importance in HIV care and predictive of ART adherence.5–13 Yet, little is known about the most effective methods of communicating about adherence, or about how best to train providers to engage with patients on this issue.
Data from the few existing studies on this topic suggest that typical HIV physician dialogue regarding ART adherence may be counterproductive. In one study, patients described lecturing or scolding from physicians about adherence, and some reported concealing their non-adherent behavior, discontinuing clinic attendance or stopping medication taking altogether as a result.14 Other studies have demonstrated that discussion of adherence is often cursory15 and that ART counseling, when it occurs, is characterized by more provider directives, control statements, and dominance than other topics, with few open questions, and patients making only a small proportion of statements of opinion, desire or intention.16
Therefore, the objective of this current study was to use a randomized controlled study design to test the impact of complimentary patient and provider communication interventions designed to optimize medication communication compared with standard care (no patient or provider intervention). We hypothesized that patients and providers would engage more effectively about medication adherence as a result of the combined intervention. Our primary goal was to increase patient-provider communication related to medication adherence in a way that engages and supports patients.
METHODS
Study Design, Subjects, and Setting
The Enhancing Communication and HIV Outcomes (ECHO) Study had two phases: an observational phase and an intervention phase. In the observational phase, we applied a conceptual model to understand racial/ethnic differences in the interpersonal processes of care and clinical outcomes.17–21 In the second phase of the ECHO Study (the focus of this current report), we evaluated the impact of complimentary patient and provider communication intervention vs. no intervention on the amount and quality of dialogue about antiretroviral medication adherence. Study subjects were HIV care providers and their patients at three outpatient clinics in the United States (Detroit, New York, and Portland, OR). The study received IRB approval from each of the sites. Eligible providers were physicians, nurse practitioners, or physician assistants who provided primary care to HIV-infected patients at one of the study sites. Eligible patients were English speaking HIV-infected with a history of medication or appointment nonadherence reported in the medical record who had had at least one prior visit with a participating provider.
Provider Intervention and Data Collection
All HIV providers gave informed consent, completed a baseline questionnaire, and then were randomized to either receive or not receive training. Provider randomization was done by random number generator within sites, such that the number of providers in the intervention and control arms was balanced at each study location. The provider intervention consisted of a one-hour didactic presentation delivered by one of the co-investigators (IW) to introduce how principles of motivational interviewing (MI) and adult learning theory might apply to dialogue with patients regarding medication adherence.22 The intervention began with providers listening to an audio-recording of typical yet ineffective adherence dialogue, and then focused on four specific behaviors (1) resist the ‘righting reflex’ (e.g. avoid correcting and lecturing to patients), (2) understand patient motivations (e.g. differences between intentional and unintentional adherence), (3) listen to the patient (e.g. avoid missing opportunities for empathic reflection), and (4) empower the patient (e.g. ask the patients’ opinion of what they should do, compliment positive health behaviors in which the patient has engaged, etc.). Providers were told that this lecture was not intended to make them proficient in MI, but rather to introduce them to the concepts and provide them with resources to learn more. Six weeks after the intervention, we mailed providers a summary of key points and the book, “Motivational Interviewing in Healthcare.”22
On baseline questionnaires, providers reported basic demographic information (age, sex, and race/ethnicity). At the completion of the study, we asked providers to rate how helpful they found the brief intervention (not at all – very helpful), and whether the patient coaching intervention (described below) was disruptive to their patient flow (yes/no) and whether they noticed that it raised new issues that were worth talking about (yes/no).
Patient Intervention and Data Collection
After the provider training, we approached eligible patients of intervention and control providers in waiting rooms. All patients gave informed consent. Patients of intervention providers also received an intervention, and patients of control providers did not. The patient intervention consisted of a one-time activating patient coaching session just prior to a routine scheduled appointment. We based our patient activation intervention on prior research using patient coaching interventions.23–25 Trained research assistants applied a structured algorithm to explore any barriers to medication adherence (e.g. concerns about efficacy, side effects, dose scheduling difficulties, etc.) and questions that patients may have regarding their medications. Then, the research assistant wrote the patient’s main concerns/questions on a brightly colored card, and offered the card to the patient as a reminder. Patients were free to use or not use the card in their provider encounter. Research assistants reported that most (72%) of coaching sessions were 10 minutes or less, while the remainder (28%) were between 10 and 20 minutes.
In post-visit interviews, patients were asked to rate their overall satisfaction with care and also self-reported additional socio-demographic information such as age, sex, education, overall adherence to medications (using a previously-validated single item question, “How would you rate your adherence to your anti-HIV medications?”; very poor to excellent),26 and drug use (using the addiction-severity index (ASI)-lite).27 Additionally, patients in the intervention arm answered one question about how helpful they found the intervention. Finally, we abstracted data from medical records to obtain HIV-1 viral load counts.
Outcome Measures
All patient-provider encounters were audio recorded. Audio recordings were analyzed using the Roter Interaction Analysis System (RIAS), a widely used coding system to assess patient and provider communication behaviors during medical encounters, with well-documented reliability and predictive validity. 28–32 RIAS analysts assign one of 37 mutually exclusive and exhaustive categories to each complete thought expressed by either the patient or provider (referred to as a statement). For this study, based on a priori decisions, we focused on the particular patient, provider, and combined patient/provider behaviors as measured by RIAS that we expected to change based on the patient and provider interventions. For patient behaviors, we focused on the total number of patient statements about therapeutic regimens, as well as several specific behaviors that signal greater patient engagement (total number of patient questions, and total number of times the patient requested a service, checked to ensure the provider understands them, or checked their own understanding). For provider behaviors, we focused on the total number of provider statements about therapeutic regimens, total number of positive (such as compliments and approval) and emotional statements (such as empathy or legitimation), and total number of times the provider asked for the patient’s opinion. For overall measures of patient and provider behavior, we measured visit length in minutes, total number (patient and provider) of therapeutic statements, the ratio of provider/patient statements (i.e. ‘provider verbal dominance’), and whether or not there was any of the dialogue contained problem-solving about barriers to adherence in the encounter. All RIAS coding was done by two coders, and the overall intercoder reliability, calculated on a random sample of 41 audiotapes, across categories for patient and provider behaviors was 0.71–0.95.
Analysis
We used descriptive statistics to explore and compare the characteristics of our study providers and patients as a whole, and then stratified by intervention status, and also used descriptive statistics to explore the provider response to the communication training and patient coaching interventions. We performed t-tests for continuous variables and chi-squared tests for categorical variables to assess patient and provider characteristics which may be associated with intervention status. Because there were no significant differences in patient or provider characteristics across intervention groups, all subsequent analyses were unadjusted.
Based on the positive skew of the patient satisfaction variable, we dichotomized overall satisfaction (‘excellent’ vs. all other responses), and used chi-squared tests to assess the association of intervention status with patient satisfaction. Because most of the outcome variables of interest were skewed, we used nonparametric Kruskall-Wallis tests to compare the number outcomes (statements in each particular communication behavioral category, as well as visit length and ratios of provider to patient dialogue) in the control vs. intervention encounters. Based on these results, we conducted a post-hoc analysis exploring the association of verbal dominance with patient satisfaction, stratified by intervention arm. All analyses were conducted using Stata Version 11.0.
RESULTS
Study Sample
Characteristics of the study sample are shown in Table 1. Twenty-six providers enrolled in the study. Providers had a mean age of 46 years and most were white (71%) and male (52%). There were no differences by study arm in provider demographic characteristics. One hundred-sixty patients enrolled in the study. Most were male (77%), African-American (50%), with at least a high school degree (72%), and on ARV (78%). Only 25% of those on ARV had a suppressed viral load. There were no differences by study arm in the demographic characteristics of patients.
Table 1.
Baseline Patient and Provider Characteristics
| Total Sample | Intervention | Control | Control vs. Intervention p-value | |
|---|---|---|---|---|
| Provider Characteristics | N=26 | n=13 | n=13 | |
|
| ||||
| Age, Mean (SD) | 46 (9) | 46 (10) | 46 (9) | 0.902 |
| Female, n(%) | 12 (48) | 5 (38) | 8 (66) | 0.158 |
| White, n(%) | 17 (71) | 9 (75) | 8 (66) | 0.653 |
|
| ||||
| Patient Characteristics | N=160 | n=81 | n=79 | |
|
| ||||
| Age, Mean (SD) | 45.1 (8.4) | 45.4 (8.2) | 44.9 (8.6) | 0.711 |
| Female, n(%) | 51 (33) | 28 (36) | 23 (29) | 0.393 |
| High school degree, n (%) | 112 (72) | 53 (67) | 59 (77) | 0.228 |
| Race/Ethnicity | ||||
| Non-Hispanic Black, n(%) | 78 (50) | 37 (47) | 41 (53) | |
| Non-Hispanic White, n(%) | 53 (34) | 25 (32) | 28 (36) | |
| Hispanic, n(%) | 17 (11) | 11 (14) | 6 (8) | 0.504 |
| Active drug use, n(%) | 60 (38) | 38 (35) | 32 (41) | 0.438 |
| On ARV, n(%) | 125 (78) | 62 (77) | 63 (80) | 0.624 |
| Adherence, n(%) reported “excellent” | 55 (37) | 28 (38) | 27 (36) | 0.905 |
| HIV RNA suppression (if on ARV), n (%) | 39 (25) | 16 (21) | 23 (31) | 0.150 |
Intervention vs. Control Communication Behaviors
Differences in patient, provider and overall communication measures are displayed in Table 2. Although visit length did not differ, there was significantly more dialogue about therapeutic regimen in visits with intervention patients and providers than visits of control patients and providers (167 vs 128, respectively, p=.004), with the majority of these statements coming from providers rather than patients. Consequently, therapeutic regimen talk was verbally dominated by providers to a greater extent in intervention than control visits. These visits also included more brainstorming solutions to nonadherence, with 41% of intervention visits compared vs. 22% of control visits including some adherence brainstorming (p=0.026).
Table 2.
Differences in Observed Measures of Patient-Provider Communication, Intervention Compared to Control
| Intervention | Control | Intervention vs. Control p-value^ | |
|---|---|---|---|
| PROVIDER BEHAVIORS (# of statements) | |||
| Provider therapeutic talk* | 110.6 | 78.0 | <0.001 |
| Provider positive talk | 43.6 | 37.6 | 0.039 |
| Provider emotional talk | 26.1 | 17.6 | <0.001 |
| Provider asks for patient opinion | 2.9 | 2.0 | 0.009 |
| PATIENT BEHAVIORS (# of statements) | |||
| Patient therapeutic talk* | 56.4 | 49.9 | 0.211 |
| Patient question-asking* | 10.9 | 10.9 | 0.965 |
| Confirms provider’s understanding | 0.9 | 0.5 | 0.012 |
| Paraphrases/checks own understanding | 5.0 | 5.0 | 0.695 |
| OVERALL MEASURES | |||
| Visit length (minutes) | 21.1 | 19.3 | 0.292 |
| Total (patient and provider) therapeutic talk* | 167.0 | 127.9 | 0.004 |
| Ratio of all provider/patient talk (verbal dominance) | 1.48 | 1.22 | 0.002 |
| Ratio of provider/patient therapeutic talk* (therapeutic verbal dominance) | 2.4 | 1.9 | 0.003 |
| Any problem-solving talk about barriers to adherence, % | 41% | 22% | 0.026 |
obtained for all measures of communication using Krustkall Wallis tests to account for nonparametric data; obtained using chi-squared tests for % visits with problem-solving talk
including question-asking and information-giving/counseling all values are means except where otherwise noted
Compared with control providers, intervention providers also demonstrated more positive talk such as agreements, approvals and compliments (44 vs. 38 statements, p=0.039), more emotional talk such as empathy and reassurance (26 vs. 18 statements, p<0.001) and more probing patient opinion (3 vs. 2 statements, p=0.009). There were no differences in the communication of patients in intervention and control visits with the exception of patient statements made to clarify the provider’s understanding.
In post-hoc analysis, we found that greater physician verbal dominance was associated with lower patient satisfaction in the control arm, but not in the intervention arm (see Table 3).
Table 3.
Relative Risk of Patient Being Very Satisfied based on Provider Verbal Dominance, by Intervention Status
| Very Satisfied | ||||
|---|---|---|---|---|
|
Control n=73 |
Intervention n=71 |
|||
| RR | 95% CI | RR | 95% CI | |
| Verbal Dominance | 0.63 | (0.49–0.81) | 0.9 | (0.59–1.38) |
Provider and Patient Response to Intervention
Of the 13 providers who received the communication skills training intervention, 62% felt it was very or extremely helpful, 23% felt it was somewhat helpful, and 13% felt it was a little or not at all helpful. Nearly all the providers (85%) whose patients received the intervention reported that the coaching raised issues that were important to discuss in the visit and that it did not disrupt patient flow. Most patients (62%) who received the coaching intervention reported that it was very or extremely helpful, 24% somewhat helpful, and 14% a little or not helpful. Patients in the intervention vs. control arm had a trend towards higher satisfaction that did not meet the threshold for statistical significance (see Figure 1).
Figure 1.
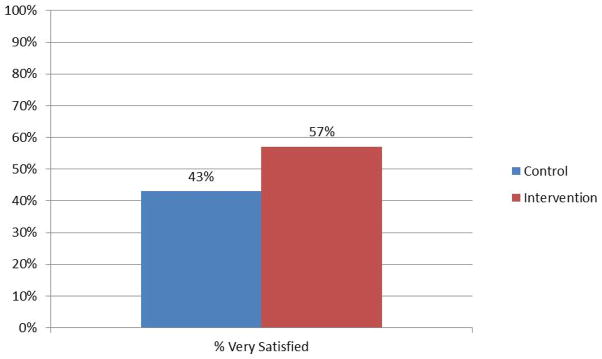
Patient Satisfaction by Intervention Status
DISCUSSION
We found that a brief training intervention enhanced the quality of visit communication by increasing dialogue regarding medication adherence and improving the overall character of the visit in terms of emotional, positive and facilitative provider talk. We also found that trained providers were more verbally dominant, both overall and specifically while discussing medication adherence with patients, and that coached patient dialogue didn’t substantively change their level of verbal engagement. These apparently conflicting results deserve separate consideration.
Although patients who were coached did make more attempts to clarify their provider’s understanding, they did not increase the number of questions they asked, nor did they significantly increase the amount of talk about their therapeutic regimen. Since physicians in the intervention arm provided more information and counseling about medications and adherence-related issues, it is possible that they pre-empted questions by obviating the need to for patients to ask. Moreover, the patient training may have framed the visit for patients making them more receptive to provider messages and counsel. A number of types of coaching intervention have previously been shown to be effective,23–25 though none of these were done in HIV care and none included complimentary provider training.
The increased verbal dominance of intervention providers is interesting, yet should be interpreted cautiously. It is worth noting that more physician dialogue did not come at the expense of patient dialogue, because the total amount of patient talk about the therapeutic regimen went up slightly for the intervention patients, but to a lesser extent than the increase in provider talk. Also, although increased verbal dominance is generally found to be associated with lower patient satisfaction, in our study, despite this increase in provider verbal dominance, we found a trend towards higher satisfaction among intervention patients. A paper by Laws et al. that used data from the first, descriptive, phase of the ECHO study, may explain this apparently conflicting finding.33 Laws et al. used a new method of dialogue analysis, the Comprehensive Analysis of the Structure of Encounters System (CASES) that first divides visits into threads, defined as a problem or a topic that is discussed. Next it divides each thread into four component parts or basic tasks: presentation, information, resolution, and engagement. Some provider behaviors, like verbal dominance, may be inappropriate during presentation, when the patient is presenting a problem, but appropriate or even necessary during the information component of the thread, when the patient is asking the physician for information. They show that aggregating across these different parts of the interview, which have different purposes, can be misleading. Indeed, when we examined the association between patient satisfaction and provider verbal dominance in this current study, we found that there was no association for those in the intervention group, but patients in the control group were less satisfied with higher provider dominance. If physicians were more verbally dominant in the intervention arm because they were doing a better job answering patient’s questions, which we cannot specifically test using these data, then these findings would be consistent.
Several limitations are worth noting. First, though our study was the largest of HIV patient-provider communication to date, conducted at three different cities across the US, it still was a relatively small study with a small number of providers. Second, we provided only a very brief provider intervention. Despite this, we were able to demonstrate changes in provider behavior, which may indicate that less intensive, brief, and easily replicable training may be sufficient to impacting provider communication behavior. Third, although we randomized providers and did not find any differences in basic demographic characteristics, we did not measure communication at baseline and cannot be certain that some differences did not exist which would confound our results. Fourth, although we trained, and provided an extensive coaching procedure manual, to our research assistants, the negative results related to patient coaching may reflect some lack of skill or training. We did not have resources to audio record and measure their fidelity to the coaching protocol. Finally, we only measured the effect of the intervention on communication behaviors, and did not test the effect of communication interventions on patient medication adherence or clinical outcomes. Although MI has an extensive body of evidence supporting its effectiveness in promoting patient behavior change,22 whether or not teaching HIV providers to apply the principles in a busy practice setting will improve patient outcomes is unclear. Our data support the need for clinical trials to assess the effect of a brief communication intervention on patient adherence and clinical outcomes.
In conclusion, a brief provider training based on the principles of motivational interviewing, combined with patient coaching sessions, enhanced visit communication in important ways by increasing the amount of dialogue and problem solving regarding medication adherence in a supportive and facilitative way. However, most of the increase in adherence dialogue was provider rather than patient talk, which either indicates that further training is required to help providers engage patients more effectively in the conversation or that providers became engaged more effectively and in a patient-centered manner. Future studies with larger sample sizes that examine patient-reported and clinical outcomes, in addition to communication measures, may be able to disentangle these hypotheses and understand the degree to which changing communication can change patient adherence and clinical outcomes.
Acknowledgments
Support. This research was supported by a contract from the Health Resources Service Administration and the Agency for Healthcare Research and Quality (AHRQ 290-01-0012). In addition, Dr. Korthuis was supported by the National Institute of Drug Abuse (K23 DA019809), Dr. Saha was supported by the Department of Veterans Affairs, Dr. Beach was supported by the Agency for Healthcare Research and Quality (K08 HS013903-05) and both Drs. Beach and Saha were supported by Robert Wood Johnson Generalist Physician Faculty Scholars Awards.
Footnotes
None of the funders had a role in the design and conduct of this analysis, nor was it subject to their final approval.
None of the authors have any relevant financial conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.Gardner EM, McLees MP, Steiner JF, Del RC, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CDC F. Today’s HIV/AIDS Epidemic. 10-1-2014. Centers for Disease Control and Prevention; May 15, 2013. [Google Scholar]
- 3.Arbuthnott A, Sharpe D. The effect of physician-patient collaboration on patient adherence in non-psychiatric medicine. Patient Educ Couns. 2009;77(1):60–67. doi: 10.1016/j.pec.2009.03.022. [DOI] [PubMed] [Google Scholar]
- 4.Zolnierek KB, DiMatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47(8):826–834. doi: 10.1097/MLR.0b013e31819a5acc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schneider J, Kaplan SH, Greenfield S, Li W, Wilson IB. Better physician-patient relationships are associated with higher reported adherence to antiretroviral therapy in patients with HIV infection. J Gen Intern Med. 2004;19(11):1096–1103. doi: 10.1111/j.1525-1497.2004.30418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schilder AJ, Kennedy C, Goldstone IL, Ogden RD, Hogg RS, O’Shaughnessy MV. “Being dealt with as a whole person” Care seeking and adherence: the benefits of culturally competent care. Soc Sci Med. 2001;52(11):1643–1659. doi: 10.1016/s0277-9536(00)00274-4. [DOI] [PubMed] [Google Scholar]
- 7.Murri R, Antinori A, Ammassari A, et al. Physician estimates of adherence and the patient-physician relationship as a setting to improve adherence to antiretroviral therapy. J Acquir Immune Defic Syndr. 2002;31 (Suppl 3):S158–S162. doi: 10.1097/00126334-200212153-00015. [DOI] [PubMed] [Google Scholar]
- 8.Wu AW, Ammassari A, Antinori A. Adherence to antiretroviral therapy: where are we, and where do we go from here? J Acquir Immune Defic Syndr. 2002;31 (Suppl 3):S95–S97. doi: 10.1097/00126334-200212153-00001. [DOI] [PubMed] [Google Scholar]
- 9.Roberts KJ. Physician-patient relationships, patient satisfaction, and antiretroviral medication Adherence among HIV-infected adults attending a public health clinic. AIDS Patient Care STDS. 2002;16(1):43–50. doi: 10.1089/108729102753429398. [DOI] [PubMed] [Google Scholar]
- 10.Davis-Michaud M, Yurk R, Lansky D, Asch S, Wu AW. Quality Care for People with HIV/AIDS: Patients’ Perspectives. HIV Clin Trials. 2004;5(6):406–415. doi: 10.1310/GQ98-PGK7-0T97-47XH. [DOI] [PubMed] [Google Scholar]
- 11.U.S.Department of Health and Human Services (DHHS) [Accessed April 13, 2005];Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents. 2005 Apr 7; http://aidsinfo.nih.gov. Available at: http://aidsinfo.nih.gov.
- 12.Bakken S, Holzemer WL, Brown MA, et al. Relationships between perception of engagement with health care provider and demographic characteristics, health status, and adherence to therapeutic regimen in persons with HIV/AIDS. AIDS Patient Care STDS. 2000;14(4):189–197. doi: 10.1089/108729100317795. [DOI] [PubMed] [Google Scholar]
- 13.Beach MC, Keruly J, Moore RD. Is the quality of the patient-provider relationship associated with better adherence and health outcomes for patients with HIV? J Gen Intern Med. 2006;21(6):661–665. doi: 10.1111/j.1525-1497.2006.00399.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tugenberg T, Ware NC, Wyatt MA. Paradoxical effects of clinician emphasis on adherence to combination antiretroviral therapy for HIV/AIDS. AIDS Patient Care STDS. 2006;20(4):269–274. doi: 10.1089/apc.2006.20.269. [DOI] [PubMed] [Google Scholar]
- 15.Barfod TS, Hecht FM, Rubow C, Gerstoft J. Physicians’ communication with patients about adherence to HIV medication in San Francisco and Copenhagen: a qualitative study using Grounded Theory. BMC Health Serv Res. 2006;6:154. doi: 10.1186/1472-6963-6-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wilson IB, Laws MB, Safren SA, et al. Provider-focused intervention increases adherence-related dialogue but does not improve antiretroviral therapy adherence in persons with HIV. J Acquir Immune Defic Syndr. 2010;53(3):338–347. doi: 10.1097/QAI.0b013e3181c7a245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saha S, Sanders DS, Korthuis PT, et al. The role of cultural distance between patient and provider in explaining racial/ethnic disparities in HIV care. Patient Educ Couns. 2011;85(3):e278–e284. doi: 10.1016/j.pec.2011.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saha S, Korthuis PT, Cohn JA, Sharp VL, Moore RD, Beach MC. Primary care provider cultural competence and racial disparities in HIV care and outcomes. J Gen Intern Med. 2013;28(5):622–629. doi: 10.1007/s11606-012-2298-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beach M, Roter D, Korthuis P, et al. Association of provider mindfulness patient-provider communication in HIV care. Annals of Family Medicine. 2013 [Google Scholar]
- 20.Beach MC, Saha S, Korthuis PT, et al. Differences in Patient-Provider Communication for Hispanic Compared to Non-Hispanic White Patients in HIV Care. J Gen Intern Med. 2010;25(7):682–687. doi: 10.1007/s11606-010-1310-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beach MC, Saha S, Korthuis PT, et al. Patient-Provider Communication Differs for Black Compared to White HIV-Infected Patients. AIDS Behav. 2011;15(4):805–811. doi: 10.1007/s10461-009-9664-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rollnick S, Miller WR, Butler C. Motivational Interviewing in Health Care. New York, NY: The Guilford Press; 2008. [Google Scholar]
- 23.Griffin SJ, Kinmonth AL, Veltman MW, Gillard S, Grant J, Stewart M. Effect on health-related outcomes of interventions to alter the interaction between patients and practitioners: a systematic review of trials. Ann Fam Med. 2004;2(6):595–608. doi: 10.1370/afm.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rao JK, Anderson LA, Inui TS, Frankel RM. Communication interventions make a difference in conversations between physicians and patients: a systematic review of the evidence. Med Care. 2007;45(4):340–349. doi: 10.1097/01.mlr.0000254516.04961.d5. [DOI] [PubMed] [Google Scholar]
- 25.Harrington J, Noble LM, Newman SP. Improving patients’ communication with doctors: a systematic review of intervention studies. Patient Educ Couns. 2004;52(1):7–16. doi: 10.1016/s0738-3991(03)00017-x. [DOI] [PubMed] [Google Scholar]
- 26.Lu M, Safren SA, Skolnik PR, et al. Optimal recall period and response task for self-reported HIV medication adherence. AIDS Behav. 2008;12(1):86–94. doi: 10.1007/s10461-007-9261-4. [DOI] [PubMed] [Google Scholar]
- 27.McLellan AT, Cacciola JS, Zanis D. [Accessed February 14, 2007];Addiction Severity Index, Lite Version (ASI-Lite) 1997 http://www.who int/substance_abuse/research_tools/addictionseverity/en/index.html. Available at: http://www.who.int/substance_abuse/research_tools/addictionseverity/en/index.html.
- 28.Bertakis KD, Roter D, Putnam SM. The relationship of physician medical interview style to patient satisfaction. J Fam Pract. 1991;32(2):175–181. [PubMed] [Google Scholar]
- 29.Levinson W, Roter DL, Mullooly JP, Dull VT, Frankel RM. Physician-patient communication. The relationship with malpractice claims among primary care physicians and surgeons. JAMA. 1997;277(7):553–559. doi: 10.1001/jama.277.7.553. [DOI] [PubMed] [Google Scholar]
- 30.Roter DL. Patient participation in the patient-provider interaction: the effects of patient question asking on the quality of interaction, satisfaction and compliance. Health Educ Monogr. 1977;5(4):281–315. doi: 10.1177/109019817700500402. [DOI] [PubMed] [Google Scholar]
- 31.Wissow LS, Roter D, Bauman LJ, et al. Patient-provider communication during the emergency department care of children with asthma. The National Cooperative Inner-City Asthma Study, National Institute of Allergy and Infectious Diseases, NIH, Bethesda, MD. Med Care. 1998;36(10):1439–1450. doi: 10.1097/00005650-199810000-00002. [DOI] [PubMed] [Google Scholar]
- 32.Roter DL, Hall JA, Katz NR. Relations between physicians’ behaviors and analogue patients’ satisfaction, recall, and impressions. Med Care. 1987;25(5):437–451. doi: 10.1097/00005650-198705000-00007. [DOI] [PubMed] [Google Scholar]
- 33.Laws MB, Taubin T, Bezreh T, Lee Y, Beach MC, Wilson IB. Problems and processes in medical encounters: the cases method of dialogue analysis. Patient Educ Couns. 2013;91(2):192–199. doi: 10.1016/j.pec.2012.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]


