Abstract
Introduction
Little research to date has explored typologies of physical activity among older adults. An understanding of physical activity patterns may help to both determine the health benefits of different types of activity and target interventions to increase activity levels in older adults. This analysis, conducted in 2014, used a latent class analysis approach to characterize patterns of physical activity in a cohort of older adults.
Methods
A total of 3,497 men and women aged 65–75 years living in New York City completed the Physical Activity Scale for the Elderly (PASE) in 2011. PASE scale items were used to classify subjects into latent classes. Multinomial regression was then used to relate individual and neighborhood characteristics to class membership.
Results
Five latent classes were identified: “least active,” “walkers,” “domestic/gardening,” “athletic,” and “domestic/gardening athletic.” Individual-level predictors, including more education, higher income, and better self-reported health, were associated with membership in the more-active classes, particularly the athletic classes. Residential characteristics, including living in single-family housing and living in the lower-density boroughs of New York City, were predictive of membership in one of the domestic/gardening classes. Class membership was associated with BMI even after controlling for total PASE score.
Conclusions
This study suggests that individual and neighborhood characteristics are associated with distinct physical activity patterns in a group of older urban adults. These patterns are associated with body habitus independent of overall activity.
Introduction
The mental and physical health benefits of physical activity in older adulthood are well established.1–5 The context in which physical activity occurs may affect the health-producing benefits of that activity.6, 7 For example, several comprehensive reviews have suggested that outdoor physical activity, particularly in green space, may improve mental health more than indoor physical activity does.8, 9 However, assessing the benefits associated with specific types of physical activity (e.g., gardening, walking) individually is problematic because some activity types are highly correlated (e.g., people who weed gardens are likely to mow lawns and rake leaves).
Latent class analysis (LCA) can reduce analytic complexity by identifying patterns of activity.10–13 Furthermore, patterns may both inform population-level interventions and allow for more targeted individual-level interventions. For example, population-level interventions might improve physical or social resources necessary to support a common activity pattern, whereas individual-level interventions might classify individuals by activity pattern to tailor interventions more personally.11 However, although previous research has characterized patterns of physical activity among adolescents12, 14 and middle-aged adults,15 as well as patterns in overall daily activity in older adults (wherein physical exercise constituted one activity domain),16 to our knowledge, no research has investigated patterning of types of physical activity among older adults or correlates of these patterns.
This analysis uses LCA to identify cross-sectional patterns of physical activity among a sample of men and women aged 65–75 years living in New York City (NYC). The resulting classes are then analyzed in relation to individual and residential neighborhood characteristics and in relation to BMI, controlling for total activity.
Methods
Study Sample
The NYC Neighborhood and Mental Health in the Elderly Study II (NYCNAMES-II) is a 3-year longitudinal cohort study of 3,497 NYC residents aged 65–75 years at baseline. NYCNAMES-II was conducted in part to study the implications of Department of Transportation interventions designed to increase elderly pedestrian safety. Participants were recruited between June and November 2011 using a two-stage area probability sampling design ensuring participants with proximity to intervention sites and sociodemographic heterogeneity reflective of the city as a whole. First, Census tracts in NYC were divided into 16 strata of racial/ethnic mix, walkability,17 and income. Next, a stratified geocoded telephone list was purchased from InfoUSA to identify potential participants. Finally, using that list, 1,500 subjects were recruited from Census tracts within 0.5 miles of an intervention site and 2,000 were recruited from the remaining census tracts. Interviews were conducted by New York Academy of Medicine (n=219) and Abt-SRBI (n=3,281) using a computer-assisted telephone interviewing program. For households with two or more individuals aged between 65 and 75 years, a participant was selected at random. Each telephone number had an equal probability of being selected. For Wave 1, after multiple contact efforts, 57% of selected telephone numbers did not yield a successful contact. Among those contacted, 30% elected to participate, for an overall response rate of 17% (0.57 × 0.30 = 0.17), somewhat lower than the 30%–40% response rate observed in NYC Department of Health telephone surveys of the general NYC population.18 Interviews were conducted by telephone, and participants were offered $10 in compensation for their participation. All subjects provided verbal informed consent. Three participants were removed from the final sample because they had already been interviewed in Wave 1. The study was approved by the IRBs of Columbia University, New York Academy of Medicine, and Abt-SRBI.
Measures
Indicators of activity types were developed from item responses to the Physical Activity Scale for the Elderly (PASE) recorded at baseline. PASE asks subjects to recall past-week engagement in walking, sports and recreation, muscle strengthening and endurance exercises, housework, home repair, gardening, yard work, and caring for others.19 PASE also includes an item assessing physical activity from employment, but this item was excluded to reduce survey burden in this mostly retired population. PASE scores have been validated against several objective activity measures, including accelerometers20, 21 and doubly labeled water.22, 23
PASE was designed to reliably assess quantity of physical activity in older adults. To help distinguish activity classes, two modifications were made. First, to retain information regarding activity duration in categorical variables used by LCA, PASE items for which duration of activity is indicated (walking, sports and recreation, and muscle strengthening exercises), were recoded into dichotomous variables indicating ever (>0 minutes/day on any day) engagement in the activity and often (>30 minutes/day on average) engagement (Appendix S1). Second, PASE items assessing sport and recreation specify three intensity classes: light, moderate, and strenuous. For example, golf with a cart is coded as light activity, whereas golf without a cart is coded as moderate activity. Because many subjects reported engaging in one primary sport/recreation activity, exploratory LCAs that coded the activity intensity categories separately resulted in latent classes that were strongly affected by intensity of the single sport/recreation activity rather than an overall pattern of activity. To increase homogeneity of the classes that were engaged in sport/recreation activity and optimize interpretability of the patterns resulting from the LCA model, all sport/recreation categories were combined for analysis.
The final LCA used the resulting ever and often indicators for activities where duration was indicated as well as the dichotomous indicators for other activities, for a total of 12 items (Table 1).
Table 1.
Items Used to Classify Physical Activity in 3,497 New York City Residents Aged 65–75, Surveyed Between June 2011 and November 2011
| Item | Examples | Proportion of subjects engaged in activity | Proportion of subjects missing data |
|---|---|---|---|
| Ever-sports | Golf, billiards, shuffleboard, dancing, basketball, hiking, jogging | 52.6% | 1.8% |
| Often-sports | Sports for more than 30 minutes a day | 25.2% | |
| Ever-exercises | Calisthenics, sit-ups, weight lifting | 35.6% | 0.7% |
| Often-exercises | Exercises for more than 30 minutes a day | 5.6% | |
| Ever-walking | 88.8% | 1.4% | |
| Often-walking | Walking for more than 30 minutes a day | 48.6% | |
| Light housework | Washing dishes, ironing, laundry | 91.0% | 0.1% |
| Heavy housework | Vacuuming, sweeping, moving furniture | 53.4% | 0.1% |
| Home repairs | Painting, plumbing, carpentry | 11.0% | 0.1% |
| Lawn work or yard care | Shoveling snow, lawn mowing | 16.4% | 0.3% |
| Outdoor gardening | Planting plants, pruning, weeding | 20.3% | 0.2% |
| Caring for others | Caring for a person who requires assistance with daily living tasks (e.g., showering) | 30.6% | 0.4% |
Subjects reported sex, age, educational attainment, race/ethnicity, health status, income, and street address. To allow for non-linear relations with age and income, age at baseline was categorized as 65–68, 69–71, and 72–75 years and household income was categorized as <$20,000, $20,000–$39,999, $40,000–$79,999, and ≥$80,000. Educational attainment was categorized as reported: less than high school graduate, high school graduate, some college, and college graduate. To maintain a balance of individuals in each racial/ethnic group, race/ethnicity was categorized as non-Hispanic black, non-Hispanic white, Hispanic, and other. Street address was geocoded using Geosupport (n=3,321) and Department of City Planning - Linear Integrated Ordered Network (DCP-LION) (n=24), applications produced by the NYC Department of City Planning. If the reported address could not be geocoded (n=152), the ZIP code centroid was used.
Non-response in demographic data was relatively rare; household income was missing for 16.2% of subjects and no other item was missing for >10% of subjects. Under the assumption that these data were missing at random, five complete data sets were imputed using IVEware, using all available survey responses for the imputation. Analyses using multiply imputed data combined estimates using Rubin’s rules.24
However, the missing-at-random assumption was unlikely to hold for PASE items because failure to respond was likely caused by the subject not engaging in the activity. Values of 0 were therefore imputed for all missing PASE data. Relatively little PASE data were missing, ranging from three responses (0.1%) for light housework to 63 responses (1.8%) for any form of sports/recreation.
Statistical Analysis
LCA is a commonly used empirical approach to identify subpopulations (latent classes) by shared item response patterns. By estimating probabilities of observed responses conditional on class membership, LCA allows estimates of posterior probabilities for each individual belonging to each latent class.25
A series of LCA models specifying latent class counts from two to six were created. Model selection in LCA is an area of active research26, 27; in accordance with recommendations, four factors were considered in model selection28:
Bayesian information criteria (BIC), an indicator of model fit wherein differences of >10 units are considered strong evidence of better fit29;
standardized entropy,30 a measure of classification certainty that ranges from 0 to 1, wherein 0 represents complete uncertainty of latent class assignment and 1 represents complete certainty;
the relative size of classes in each model, preferring models with classes larger than 5% of the cohort; and
(4) substantive interpretability, preferring models whose class separations were simplest to articulate.
A “three-step” approach was used to relate latent classes to covariates, wherein Step 1 is to fit an LCA model, Step 2 is to assign subjects to latent classes, and Step 3 is to relate covariates to assigned latent class using multinomial logistic regression.31 For these data, “one-step” approach models (in which regression parameters are estimated as part as latent class model fit) did not converge in poLCA in R32 or PROC LCA in SAS.33 Proportional rather than modal assignment was used, in accordance with recommendations.31
To investigate the informative value of activity classification, multivariable models predicting BMI and obesity status (BMI >30) from PASE score and activity latent class together were developed. Significantly non-zero coefficients for activity classes, after adjustment for total PASE score, indicate the classes contain informative value beyond that of PASE score alone.
Three sensitivity analyses were conducted. First, in an elderly cohort like NYCNAMES, many subjects report health conditions rendering them incapable of performing physical activities. To examine whether the patterns of activity were affected by capability, LCA models were re-run only among those who reported being able to walk one block (n=2,363, 67.5%). Second, to test the assumption that different classes of sports activity would create less interpretable classes, LCA models were created in which light, moderate, and strenuous sports were separate items. Third, to test the findings’ robustness to the assumption that non-response to PASE items indicated no activity, the LCA was repeated using expectation maximization to account for missing data.
Imputations were performed using IVEware.34 All subsequent analyses were performed using R, version 2.15.3 and SAS, version 9.3. LCAs used PoLCA package, version 1.432 and PROC LCA.33 Analysis of the imputed data set, including the use of Rubin’s rules to combine estimates, used “mi,” version 0.09–18 and “mitools,” version 2.2.35 Multinomial regression used “nnet,” version 7.3–5.36 Figure 1 was created using Microsoft Excel and Figure 2 was created using “ggplot,” version 0.9.3.1.37 All analyses were conducted in 2014.
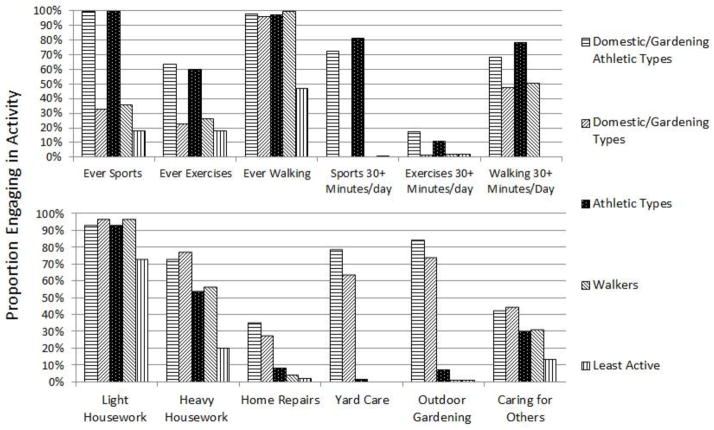
Figure 1.
Proportion of 3,497 adults aged 65–75 residing in New York City reporting participation in types of physical activity, grouped by latent class assignment, June-November 2011
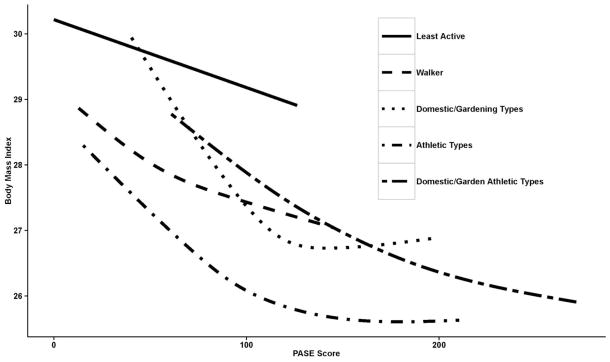
Figure 2.
Relation between PASE scores, latent activity classes, and BMI in NYCNAMES-II participants, aged 65–75, surveyed between June and November 2011.
Results
Table 2 details characteristics of the 3,497 older adults comprising the final sample. A minority (35.1%) lived in single-family housing. The majority (79.5%) reported that their neighborhood was safe for walking after dark.
Table 2.
Selected Characteristics of 3,497 New York City Residents Aged 65–75, Surveyed Between June 2011 and November 2011
| N | Proportion of cohort reporting this value | |
|---|---|---|
| Borough of Residence | ||
| Manhattan | 1,030 | 29.5% |
| Bronx | 522 | 14.9% |
| Brooklyn | 1,053 | 30.1% |
| Queens | 795 | 22.7% |
| Staten Island | 97 | 2.8% |
| Home type | ||
| 1–3 story home | 1,228 | 35.1% |
| Low rise apartment (≤4 stories) | 319 | 9.2% |
| High-rise apartment ≥5 stories) | 1,950 | 55.8% |
| Sex | ||
| Male | 1,403 | 40.1% |
| Female | 2,094 | 59.9% |
| Age group | ||
| 65–68 | 1,045 | 33.2% |
| 69–71 | 664 | 21.1% |
| 72–75 | 1,442 | 45.8% |
| Education | ||
| < High school graduate | 670 | 19.1% |
| High school graduate | 950 | 27.1% |
| Some college | 625 | 17.9% |
| College graduate | 1,252 | 35.8% |
| Race/Ethnicity | ||
| Black (non-Hispanic) | 1,070 | 30.6% |
| White (non-Hispanic) | 1,801 | 51.5% |
| Other | 247 | 7.1% |
| Hispanic | 379 | 10.8% |
| Safe to walk after dark in neighborhood | ||
| Strongly agree | 1,354 | 44.0% |
| Somewhat agree | 1,092 | 35.5% |
| Somewhat disagree | 303 | 9.8% |
| Strongly disagree | 328 | 10.7% |
| Health | ||
| Excellent | 643 | 18.4% |
| Good | 1,524 | 43.6% |
| Fair | 1,050 | 30.0% |
| Poor | 280 | 8.0% |
| Household income | ||
| <$20,000 | 1,264 | 36.2% |
| $20,000–$40,000 | 859 | 24.6% |
| $40,000–$80,000 | 732 | 20.9% |
| $80,000+ | 642 | 18.4% |
| BMI category | ||
| <25 | 1,156 | 33.1% |
| 25–30 | 1,377 | 39.4% |
| ≥30 | 964 | 27.6% |
Differing selection criteria favored different numbers of latent classes. BIC scores were lowest for the six-class model. Entropy increased with more classes, and all models except the six-class model were well balanced regarding count of members; the six-class model contained a small (4.0% of the overall cohort) class whose defining feature was never walking regardless of other activity types. The remaining five classes of the six-class model were less interpretable than their five-class counterparts. Appendix S2 presents fit statistics and activity profiles for models from two to six latent classes.
A five-class model represented the optimal balance of model fit and interpretability (Table 3). The final latent classes were:
Table 3.
Proportion of 3,497 New York City Residents Aged 65–75 Within Each Latent Class Assignment Who Reported Conducting Each Form of Physical Activity
| Activity | Domestic/ Gardening Athletic type | Walker | Athletic type | Domestic/ Gardening type | Least Active |
|---|---|---|---|---|---|
| Ever sports | 100% | 36% | 100% | 33% | 18% |
| Ever exercises | 64% | 27% | 60% | 23% | 18% |
| Ever walking | 98% | 100% | 98% | 96% | 47% |
| Sports 30+ Minutes/day | 73% | 0% | 81% | 0% | 1% |
| Exercises 30+ Minutes/day | 18% | 2% | 11% | 2% | 2% |
| Walking 30+ Minutes/day | 68% | 51% | 78% | 48% | 0% |
| Light housework | 93% | 97% | 93% | 97% | 73% |
| Heavy housework | 73% | 56% | 54% | 77% | 20% |
| Home repairs | 36% | 5% | 8% | 28% | 2% |
| Yard care | 79% | 0% | 2% | 64% | 0% |
| Outdoor gardening | 84% | 1% | 8% | 74% | 1% |
| Caring for others | 43% | 31% | 30% | 45% | 14% |
|
| |||||
| Mean PASE Score | 150.8 | 64.1 | 90.2 | 117.6 | 33.0 |
| PASE Score 95% CI | 69.2, 232.3 | 13.8, 114.5 | 26.4, 154.0 | 54.3, 180.8 | 0, 78.8 |
| Percent of cohort | 9.9% | 36.7% | 21.8% | 12.8% | 18.8% |
Note: All interviews conducted in June-November 2011
subjects who reported little activity overall (18.8% of subjects, “least active”);
subjects who reported walking and some housework, but little other activity (36.7% of subjects, “walkers”);
subjects whose activities included home-related activities such as lawn/yard work, gardening, and home repairs but only low amounts of sport or strengthening activities (12.8% of subjects, “domestic/gardening types”);
subjects who did not generally report home and garden activities but were physically active, particularly engaging in sports or recreational activities (21.8% of subjects, “athletic types”); and
subjects who reported both home-related activities and sports and recreational activities (9.9% of subjects, “domestic/gardening athletic types”).
Figure 1 displays the proportion of subjects reporting participating in an activity conditional on assigned class membership.
In multivariate analysis, housing type, education level, self-reported health status, sex, and income were most strongly predictive of latent class membership. Living in high-rise apartments was strongly negatively associated with the probability of being in one of the domestic/gardening classes relative to being in the least active class (relative risk [RR]=0.19, 95% CI=0.13, 0.28 for domestic/gardening types; RR=0.18, 95% CI=0.12, 0.28 for domestic/gardening athletic types) and positively associated with the probability of being in the walker classes relative to being in the least active class (RR=1.58, 95% CI=1.18, 2.13) or athletic types (RR=1.67, 95% CI=1.18, 2.37). Worse self-reported health was negatively associated with the probability of being in any active class as compared with the probability of being in the least active class (e.g., RR=0.03, 95% CI=0.01, 0.09 comparing risk of being in domestic/gardening athletic class versus least active, conditional on poor self-reported health versus excellent self-reported health). Higher levels of income were associated with increased probability of being in one of the domestic/gardening type classes as compared with the least active class (RR=2.08, 95% CI=1.20, 3.60 comparing household income ≥$80,000 to <$20,000). Table 4 shows RRs of class membership as compared with the least active class in the final multivariable model.
Table 4.
Relative Risk of Membership of 3,497 New York City Residents Aged 65–75 in Specified Class Compared to “Least Active” Class in Multivariable Model
| Walker | Domestic/ Gardening type | Athletic type | Domestic/Gardening Athletic type | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Relative risk | 95% CI | Relative risk | 95% CI | Relative risk | 95% CI | Relative risk | 95% CI | |||||
| Borough | ||||||||||||
| Manhattan | 0.81 | 0.57 | 1.15 | 0.66 | 0.39 | 1.10 | 1.13 | 0.76 | 1.67 | 1.65 | 0.96 | 2.81 |
| Bronx | 0.61 | 0.41 | 0.88 | 0.51 | 0.30 | 0.85 | 0.68 | 0.43 | 1.07 | 0.77 | 0.43 | 1.38 |
| Brooklyn | 0.93 | 0.67 | 1.30 | 0.79 | 0.53 | 1.16 | 0.89 | 0.61 | 1.31 | 0.89 | 0.57 | 1.39 |
| Queens | -- | -- | -- | -- | ||||||||
| Staten Island | 0.42 | 0.19 | 0.93 | 0.70 | 0.33 | 1.51 | 0.64 | 0.26 | 1.57 | 0.84 | 0.36 | 1.97 |
|
| ||||||||||||
| Home type | ||||||||||||
| Single family | 0.62 | 0.46 | 0.84 | 5.30 | 3.56 | 7.89 | 0.60 | 0.42 | 0.84 | 5.68 | 3.62 | 8.90 |
| Low rise apartment | 0.83 | 0.57 | 1.19 | 1.05 | 0.56 | 1.95 | 0.77 | 0.51 | 1.17 | 1.33 | 0.73 | 2.43 |
| High-rise apartment | -- | -- | -- | -- | ||||||||
|
| ||||||||||||
| Sex | ||||||||||||
| Male | -- | -- | -- | -- | ||||||||
| Female | 1.00 | 0.79 | 1.26 | 0.85 | 0.63 | 1.14 | 0.73 | 0.57 | 0.95 | 0.68 | 0.49 | 0.94 |
|
| ||||||||||||
| Age group | ||||||||||||
| 65–68 | -- | -- | -- | -- | ||||||||
| 69–71 | 0.91 | 0.67 | 1.24 | 1.09 | 0.73 | 1.64 | 1.03 | 0.73 | 1.46 | 0.77 | 0.49 | 1.20 |
| 72–75 | 0.90 | 0.70 | 1.16 | 1.05 | 0.74 | 1.47 | 0.86 | 0.64 | 1.15 | 0.93 | 0.65 | 1.33 |
|
| ||||||||||||
| Education | ||||||||||||
| < High school graduate | 0.64 | 0.47 | 0.89 | 0.81 | 0.51 | 1.27 | 0.68 | 0.45 | 1.01 | 0.61 | 0.34 | 1.08 |
| High school graduate | -- | -- | -- | -- | ||||||||
| Some college | 1.03 | 0.73 | 1.45 | 1.08 | 0.69 | 1.69 | 1.21 | 0.82 | 1.80 | 1.13 | 0.69 | 1.87 |
| College graduate | 0.89 | 0.64 | 1.26 | 1.12 | 0.73 | 1.71 | 1.31 | 0.89 | 1.93 | 1.41 | 0.89 | 2.22 |
|
| ||||||||||||
| Race/Ethnicity | ||||||||||||
| Black (non-Hispanic) | 1.28 | 0.97 | 1.69 | 0.93 | 0.65 | 1.34 | 1.19 | 0.86 | 1.65 | 1.03 | 0.68 | 1.54 |
| White (non-Hispanic) | -- | -- | -- | -- | ||||||||
| Other | 1.59 | 0.96 | 2.64 | 1.47 | 0.79 | 2.76 | 1.65 | 0.91 | 3.00 | 1.93 | 0.98 | 3.76 |
| Hispanic | 0.87 | 0.59 | 1.29 | 0.72 | 0.38 | 1.35 | 1.12 | 0.70 | 1.79 | 0.75 | 0.35 | 1.60 |
|
| ||||||||||||
| Safe to walk after dark in neighborhood | ||||||||||||
| Strongly agree | -- | -- | -- | -- | ||||||||
| Somewhat agree | 1.05 | 0.81 | 1.36 | 0.95 | 0.67 | 1.33 | 1.02 | 0.76 | 1.37 | 0.83 | 0.57 | 1.19 |
| Somewhat disagree | 0.78 | 0.53 | 1.13 | 0.83 | 0.50 | 1.37 | 0.72 | 0.46 | 1.13 | 0.70 | 0.40 | 1.26 |
| Strongly disagree | 0.95 | 0.67 | 1.35 | 0.95 | 0.57 | 1.57 | 0.69 | 0.44 | 1.09 | 0.78 | 0.42 | 1.46 |
|
| ||||||||||||
| Health | ||||||||||||
| Excellent | 1.46 | 0.96 | 2.20 | 1.60 | 0.99 | 2.61 | 2.14 | 1.41 | 3.24 | 2.72 | 1.70 | 4.35 |
| Good | -- | -- | -- | -- | ||||||||
| Fair | 0.72 | 0.56 | 0.94 | 0.61 | 0.43 | 0.86 | 0.41 | 0.30 | 0.56 | 0.34 | 0.22 | 0.52 |
| Poor | 0.31 | 0.21 | 0.44 | 0.18 | 0.09 | 0.33 | 0.13 | 0.07 | 0.22 | 0.09 | 0.03 | 0.23 |
|
| ||||||||||||
| Household income | ||||||||||||
|
| ||||||||||||
| <$20,000 | -- | -- | -- | -- | ||||||||
| $20,000–$39,999 | 1.05 | 0.76 | 1.45 | 1.73 | 1.10 | 2.74 | 1.32 | 0.91 | 1.91 | 1.87 | 1.10 | 3.20 |
| $40,000–$79,999 | 1.25 | 0.85 | 1.84 | 1.82 | 1.06 | 3.13 | 1.66 | 1.07 | 2.58 | 2.15 | 1.12 | 4.13 |
| $80,000+ | 1.11 | 0.72 | 1.71 | 2.07 | 1.20 | 3.55 | 1.52 | 0.95 | 2.42 | 2.14 | 1.19 | 3.88 |
Note: All interviews conducted in June-November 2011.
Boldface indicates statistical significance (p < 0.05)
Physical activity classes were predictive of obesity status: 42.5% of the least active class was obese, compared with 30.3%, 24.8%, 20.2%, and 20.3% of the walkers, domestic/gardening types, athletic types, and domestic/gardening athletic types, respectively (χ2 test, p<0.001). In multivariable models, latent class and PASE score acted as independent predictors of BMI, suggesting that pattern of activity provided information above and beyond PASE score alone (PASE, r2 =0.025; latent class, r2 =0.035; both, r2 =0.040). Figure 2 shows restricted cubic spline functions with five knots relating PASE score to BMI within strata of latent class membership, illustrating the generally negative association between PASE and BMI and the different mean BMIs and ranges of PASE scores within latent classes.
LCAs in subjects able to walk one block without difficulty were similar with the elimination of the least active group (Appendix Table S3). LCAs performed without recoding sports activities resulted in latent classes that were more difficult to interpret (Appendix Table S4). LCAs using expectation maximization to account for missing data were comparable to those imputing zeroes (Appendix Table S5).
Discussion
This analysis identified five latent classes of physical activity in older adults in NYC: least active, walkers, domestic/gardening types, athletic types, and domestic/gardening athletic types. Housing type was strongly correlated with being classified as a domestic/gardening or domestic/gardening athletic type. After adjustment for self-reported health, the least active class was associated with lower education, lower income, and worse self-reported health, but not with increased age. Latent classes significantly predicted BMI even after accounting PASE score, suggesting patterns of activity may be as important a driver of health status as overall activity, though this analysis was descriptive and should not be interpreted causally.
Several details about the identified latent classes warrant further discussion. First, engagement in domestic/gardening activities (gardening, yard work, and home repair) was independent of engagement in athletic activities (sports and strengthening exercises). It has recently been suggested that domestic work, including gardening, may not contribute sufficient physical activity to produce fitness benefits.38, 39 In this analysis, the domestic/gardening class had a higher mean PASE score than the athletes. Second, the engagement of nearly every subject in some amount of walking was intriguing. In this urban cohort, walking may represent purposeful rather than recreational physical activity; the larger size of the walker class in NYC’s more–fdensely populated boroughs, where destinations of daily living are more often reachable on foot, supports this hypothesis.
Although there is no previous body of research on LCAs of activity patterns in older adults to compare to, our results do display similarities with patterns identified in adults aged 36 and 43 years in the United Kingdom, including separation of sports and gardening as separate classes of activity.15, 40 More generally, the finding that walking and gardening define distinct domains of activity is consistent with several previous studies of physical activity in older adults.41–44
The higher PASE scores of the domestic/gardening classes and association of those classes with single-family housing and lower-density boroughs suggests that lack of access to outdoor maintenance opportunities may be an impediment to physical activity in the more densely populated areas of NYC. An increase in “citizen pruner” and community garden programs may be an appropriate complement to increasing walkability in less pedestrian-oriented parts of the city, though further analysis incorporating motivation for selected activity modalities should be a part of developing any interventions.45, 46
Limitations
Strengths of this study include the relatively large sample size, use of multiple imputation to account for missing data, and diverse residential environments present in NYC. However, study findings should also be considered in light of several limitations. First, our information regarding activity is limited to our modified PASE, which did not assess some forms of physical activity that may be important, such as volunteer work. Furthermore, particularly among older adults for whom cognitive functioning was not assessed, self-report of physical activity may over-report actual activity47 or create spurious latent classes of activity. No objective measures of physical activity or information regarding motivation for physical activity are available. Future studies should address both these limitations. Second, although the five boroughs of NYC contain a broad range of urban- and suburban-style neighborhoods, these typologies of activity may not be replicable in other spatial contexts. However, LCA methods applied to populations in other contexts may identify patterns of activity that might suggest novel interventions to promote active lifestyles in those contexts. Third, the 17% response rate raises the possibility that those who participated do not represent the broader older adult population of NYC. Finally, “three-step” estimation approach can result in biased estimates when class membership is used as a predictor.48 However, since three-step estimates underestimate true associations,49 this limitation is unlikely to have led to overstated findings.
Conclusions
This LCA suggests there are five distinct typologies of physical activity among elderly adults in NYC. More income and better self-reported health are associated with being in a more active class, whereas living in a single-family home is associated with being in a domestic/gardening class. These typologies are predictive of BMI even after controlling for overall physical activity. More research is needed to establish whether these activity typologies describe activity patterns in other older adult populations, and if so, how the activity patterns relate to mental and physical health outcomes.
Supplementary Material
Acknowledgments
This research presented here was supported by National Institute for Mental Health grant 5R01MH085132-05 and National Cancer Institute grant T32 CA09529.
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute for Mental Health or the National Cancer Institute.
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. CMAJ. 2006;174(6):801–809. doi: 10.1503/cmaj.051351. http://dx.doi.org/10.1503/cmaj.051351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strawbridge WJ, Deleger S, Roberts RE, Kaplan GA. Physical activity reduces the risk of subsequent depression for older adults. Am J Epidemiol. 2002;156(4):328–334. doi: 10.1093/aje/kwf047. http://dx.doi.org/10.1093/aje/kwf047. [DOI] [PubMed] [Google Scholar]
- 3.Blondell SJ, Hammersley-Mather R, Veerman JL. Does physical activity prevent cognitive decline and dementia?: A systematic review and meta-analysis of longitudinal studies. BMC Public Health. 2014;14(1):510. doi: 10.1186/1471-2458-14-510. http://dx.doi.org/10.1186/1471-2458-14-510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wassink-Vossen S, Collard RM, Oude Voshaar RC, Comijs HC, de Vocht HM, Naarding P. Physical (in) activity and depression in older people. J Affect Disord. 2014;161:65–72. doi: 10.1016/j.jad.2014.03.001. http://dx.doi.org/10.1016/j.jad.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 5.Rimer J, Dwan K, Lawlor DA, et al. Exercise for depression. Cochrane Database Syst Rev. 2012:7. doi: 10.1002/14651858.CD004366.pub5. [DOI] [PubMed] [Google Scholar]
- 6.Peeters G, van Gellecum YR, van Uffelen JG, Burton NW, Brown WJ. Contribution of house and garden work to the association between physical activity and well-being in young, mid-aged and older women. Br J Sports Med. 2014;48(12):996–1001. doi: 10.1136/bjsports-2012-091103. http://dx.doi.org/10.1136/bjsports-2012-091103. [DOI] [PubMed] [Google Scholar]
- 7.Teychenne M, Ball K, Salmon J. Physical activity and likelihood of depression in adults: a review. Prev Med. 2008;46(5):397–411. doi: 10.1016/j.ypmed.2008.01.009. http://dx.doi.org/10.1016/j.ypmed.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 8.Thompson Coon J, Boddy K, Stein K, Whear R, Barton J, Depledge MH. Does participating in physical activity in outdoor natural environments have a greater effect on physical and mental wellbeing than physical activity indoors? A systematic review. Environ Sci Technol. 2011;45(5):1761–1772. doi: 10.1021/es102947t. http://dx.doi.org/10.1021/es102947t. [DOI] [PubMed] [Google Scholar]
- 9.Barton J, Pretty J. What is the best dose of nature and green exercise for improving mental health? A multi-study analysis. Environ Sci Technol. 2010;44(10):3947–3955. doi: 10.1021/es903183r. http://dx.doi.org/10.1021/es903183r. [DOI] [PubMed] [Google Scholar]
- 10.Lanza ST, Rhoades BL. Latent class analysis: An alternative perspective on subgroup analysis in prevention and treatment. Prev Sci. 2013;14(2):157–168. doi: 10.1007/s11121-011-0201-1. http://dx.doi.org/10.1007/s11121-011-0201-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heitzler C, Lytle L, Erickson D, Sirard J, Barr-Anderson D, Story M. Physical activity and sedentary activity patterns among children and adolescents: a latent class analysis approach. J Phys Act Health. 2011;8(4):457. doi: 10.1123/jpah.8.4.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huh J, Riggs NR, Spruijt-Metz D, Chou CP, Huang Z, Pentz M. Identifying patterns of eating and physical activity in children: a latent class analysis of obesity risk. Obesity. 2011;19(3):652–658. doi: 10.1038/oby.2010.228. http://dx.doi.org/10.1038/oby.2010.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Iannotti RJ, Wang J. Patterns of Physical Activity, Sedentary Behavior, and Diet in U.S. Adolescents. J Adolesc Health. 2013;53(2):280–286. doi: 10.1016/j.jadohealth.2013.03.007. http://dx.doi.org/10.1016/j.jadohealth.2013.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jago R, Fox KR, Page AS, Brockman R, Thompson JL. Physical activity and sedentary behaviour typologies of 10–11 year olds. Int J Behav Nutr Phys Act. 2010;7:59. doi: 10.1186/1479-5868-7-59. http://dx.doi.org/10.1186/1479-5868-7-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Silverwood RJ, Nitsch D, Pierce M, Kuh D, Mishra GD. Characterizing longitudinal patterns of physical activity in mid-adulthood using latent class analysis: results from a prospective cohort study. Am J Epidemiol. 2011;174(12):1406–1415. doi: 10.1093/aje/kwr266. http://dx.doi.org/10.1093/aje/kwr266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morrow-Howell N, Putnam M, Lee YS, Greenfield JC, Inoue M, Chen H. An Investigation of Activity Profiles of Older Adults. J Gerontol B Osychol Sci Soc Sci. 2014;69(5):809–821. doi: 10.1093/geronb/gbu002. http://dx.doi.org/10.1093/geronb/gbu002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neckerman KM, Lovasi GS, Davies S, et al. Disparities in urban neighborhood conditions: evidence from GIS measures and field observation in New York City. J Public Health Policy. 2009:S264–S285. doi: 10.1057/jphp.2008.47. http://dx.doi.org/10.1057/jphp.2008.47. [DOI] [PubMed]
- 18.New York City Department of Health and Mental Hygiene. Survey Data on the Health of New Yorkers. 2013 www.nyc.gov/html/doh/html/data/chs-methods.shtml.
- 19.Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46(2):153–162. doi: 10.1016/0895-4356(93)90053-4. http://dx.doi.org/10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 20.Washburn R, Ficker J. Physical Activity Scale for the Elderly (PASE): the relationship with activity measured by a portable accelerometer. J Sports Med Phys Fitness. 1999;39(4):336–340. [PubMed] [Google Scholar]
- 21.Harada ND, Chiu V, King AC, Stewart AL. An evaluation of three self-report physical activity instruments for older adults. Med Sci Sports Exerc. 2001;33(6):962–970. doi: 10.1097/00005768-200106000-00016. http://dx.doi.org/10.1097/00005768-200106000-00016. [DOI] [PubMed] [Google Scholar]
- 22.Schuit AJ, Schouten EG, Westerterp KR, Saris WH. Validity of the Physical Activity Scale for the Elderly (PASE): according to energy expenditure assessed by the doubly labeled water method. J Clin Epidemiol. 1997;50(5):541–546. doi: 10.1016/s0895-4356(97)00010-3. http://dx.doi.org/10.1016/S0895-4356(97)00010-3. [DOI] [PubMed] [Google Scholar]
- 23.Bonnefoy M, Normand S, Pachiaudi C, Lacour JR, Laville M, Kostka T. Simultaneous validation of ten physical activity questionnaires in older men: a doubly labeled water study. J Am Geriatr Soc. 2001;49(1):28–35. doi: 10.1046/j.1532-5415.2001.49006.x. http://dx.doi.org/10.1046/j.1532-5415.2001.49006.x. [DOI] [PubMed] [Google Scholar]
- 24.Little R, Rubin D. Statistical Analysis with Missing Data. Hoboken, NJ: John Wiley & Sons, Inc; 2002. http://dx.doi.org/10.1002/9781119013563. [Google Scholar]
- 25.Muthén B, Muthén LK. Integrating person-centered and variable-centered analyses: Growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res. 2000;24(6):882–891. http://dx.doi.org/10.1111/j.1530-0277.2000.tb02070.x. [PubMed] [Google Scholar]
- 26.Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Struct Equ Modeling. 2007;14(4):535–569. http://dx.doi.org/10.1080/10705510701575396. [Google Scholar]
- 27.Dias JG. From Data and Information Analysis to Knowledge Engineering. Springer; 2006. Latent class analysis and model selection; pp. 95–102. http://dx.doi.org/10.1007/3-540-31314-1_10. [Google Scholar]
- 28.Muthén B. Statistical and substantive checking in growth mixture modeling: comment on Bauer and Curran (2003) Psychol Methods. 2003;8(3):369–77. doi: 10.1037/1082-989X.8.3.369. discussion 384–93. http://dx.doi.org/10.1037/1082-989X.8.3.369. [DOI] [PubMed] [Google Scholar]
- 29.Muthen B. New developments and techniques in structural equation modeling. Psychology Press; 2001. Latent variable mixture modeling; pp. 1–33. [Google Scholar]
- 30.Celeux G, Soromenho G. An entropy criterion for assessing the number of clusters in a mixture model. Journal of classification. 1996;13(2):195–212. http://dx.doi.org/10.1007/BF01246098. [Google Scholar]
- 31.Vermunt JK. Latent class modeling with covariates: Two improved three-step approaches. Polit Anal. 2010;18(4):450–469. http://dx.doi.org/10.1093/pan/mpq025. [Google Scholar]
- 32.Linzer DA, Lewis JB. poLCA: An R package for polytomous variable latent class analysis. J Stat Softw. 2011;42(10):1–29. [Google Scholar]
- 33.Lanza ST, Collins LM, Lemmon DR, Schafer JL. PROC LCA: A SAS procedure for latent class analysis. Struct Equ Modeling. 2007;14(4):671–694. doi: 10.1080/10705510701575602. http://dx.doi.org/10.1080/10705510701575602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Raghunathan TE, Lepkowski JM, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Surv Methodol. 2001;27(1):85–96. [Google Scholar]
- 35.Su Y-S, Yajima M, Gelman AE, Hill J. Multiple imputation with diagnostics (mi) in R: opening windows into the black box. J Stat Softw. 2011;45(2):1–31. [Google Scholar]
- 36.Venables WN, Ripley BD. Modern applied statistics with S. Springer; 2002. http://dx.doi.org/10.1007/978-0-387-21706-2. [Google Scholar]
- 37.Wickham H. ggplot2: elegant graphics for data analysis. Springer; 2009. [Google Scholar]
- 38.Lawlor D, Taylor M, Bedford C, Ebrahim S. Is housework good for health? Levels of physical activity and factors associated with activity in elderly women. Results from the British Women’s Heart and Health Study. J Epidemiol Community Health. 2002;56(6):473–478. doi: 10.1136/jech.56.6.473. http://dx.doi.org/10.1136/jech.56.6.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Murphy MH, Donnelly P, Breslin G, Shibli S, Nevill AM. Does doing housework keep you healthy? The contribution of domestic physical activity to meeting current recommendations for health. BMC public health. 2013;13(1):966. doi: 10.1186/1471-2458-13-966. http://dx.doi.org/10.1186/1471-2458-13-966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kuh D, Cooper C. Physical activity at 36 years: patterns and childhood predictors in a longitudinal study. J Epidemiol Community Health. 1992;46(2):114–119. doi: 10.1136/jech.46.2.114. http://dx.doi.org/10.1136/jech.46.2.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yusuf HR, Croft JB, Giles WH, et al. Leisure-time physical activity among older adults: United States, 1990. Arch Intern Med. 1996;156(12):1321. http://dx.doi.org/10.1001/archinte.1996.00440110093012. [PubMed] [Google Scholar]
- 42.Moschny A, Platen P, Klaaßen-Mielke R, Trampisch U, Hinrichs T. Physical activity patterns in older men and women in Germany: a cross-sectional study. BMC public health. 2011;11(1):559. doi: 10.1186/1471-2458-11-559. http://dx.doi.org/10.1186/1471-2458-11-559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Armstrong ME, Cairns BJ, Green J, Reeves GK, Beral V. Reported frequency of physical activity in a large epidemiological study: relationship to specific activities and repeatability over time. BMC Med Res Methodol. 2011;11(1):97. doi: 10.1186/1471-2288-11-97. http://dx.doi.org/10.1186/1471-2288-11-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fan JX, Kowaleski-Jones L, Wen M. Walking or Dancing Patterns of Physical Activity by Cross-Sectional Age Among U.S. Women. J Aging Health. 2013;25(7):1182–1203. doi: 10.1177/0898264313495561. http://dx.doi.org/10.1177/0898264313495561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Trees New York. Licensed to Prune. www.treesny.org/citizenpruner.
- 46.New York City Department of Parks and Recreation. GreenThumb. www.greenthumbnyc.org/
- 47.Tucker JM, Welk GJ, Beyler NK. Physical activity in U.S. adults: compliance with the physical activity guidelines for Americans. Am J Prev Med. 2011;40(4):454–461. doi: 10.1016/j.amepre.2010.12.016. http://dx.doi.org/10.1016/j.amepre.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 48.Bakk Z, Tekle FB, Vermunt JK. Estimating the Association between Latent Class Membership and External Variables Using Bias-adjusted Three-step Approaches. Sociol Methodol. 2013;43(1):272–311. http://dx.doi.org/10.1177/0081175012470644. [Google Scholar]
- 49.Bolck A, Croon M, Hagenaars J. Estimating latent structure models with categorical variables: One-step versus three-step estimators. Polit Anal. 2004;12(1):3–27. http://dx.doi.org/10.1093/pan/mph001. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.