Abstract
Adolescents with type 1 diabetes typically receive clinical care every 3 months. Between visits, diabetes-related issues may not be frequently reflected, learned, and documented by the patients, limiting their self-awareness and knowledge about their condition. We designed a text-messaging system to help resolve this problem. In a pilot, randomized controlled trial with 30 adolescents, we examined the effect of text messages about symptom awareness and diabetes knowledge on glucose control and quality of life. The intervention group that received more text messages between visits had significant improvements in quality of life.
Keywords: Text messaging, Type 1 diabetes, Adolescents
Childhood Type 1 diabetes mellitus (T1D) is growing worldwide, with the incidence peaking at puberty and affecting 1 out of 400 adolescents (SEARCH for Diabetes in Youth Study Group et al., 2006; Writing Group for the SEARCH for Diabetes in Youth Study Group et al., 2007). Adolescents with type 1 diabetes (T1D) have to be constantly aware of their condition to maintain optimal glucose control. Self-management that determines glucose control is a complex process, encompassing administration of daily insulin, glucose testing, dietary modification and exercise along with symptom awareness. The responsibilities that these adolescents face, coupled with their goals of increasing independence that are negotiated with parents and other family caregivers, often contribute to struggles with adherence to T1D care plans. Biological changes of puberty further complicate and frustrate attempts to manage T1D. These include insulin resistance induced by rising sex steroid hormone levels and psycho-developmental factors that may contribute to a decline in self-management adherence (Amiel, Sherwin, Simonson, Lauritano, & Tamborlane, 1986; Rausch et al., 2012) and affect awareness of dysglycemic symptoms (Nurick & Johnson, 1991; Ryan, Dulay, Suprasongsin, & Becker, 2002).
Therefore, it is important for adolescents to consciously link symptoms with low or high blood glucose readings and associated self-management behaviors related to diet, insulin, activity level and emotional well-being. For example, how many episodes of hypoglycemia such as feelings of shakiness or diaphoresis did the adolescent have in the past week? What time of day did the symptom occur, and what self-management behaviors occurred prior to the event? What actions are needed to remedy the symptom based upon glucose level? Although this type of information is assessed by the health care provider during periodic checkups, adolescents are often unreliable historians. Adolescents and their primary family caregivers may report diabetes-related events that occurred over the past week, rather than provide comprehensive information for the entire past 3 months between visits (American Diabetes Association, 2014). As a result, these valuable symptoms and acute event records are often lost in the hectic lives of adolescents, limiting their ability to link their awareness of symptoms to check their blood glucose or take other therapeutic responses.
Additionally, adolescents must learn a large amount of information about their condition including long-term effects of TID, treatment adjustment for sick days, and co-morbidities if present, such as celiac disease and thyroiditis. This information is commonly presented in both written and verbal instructions with the health care providers and diabetes educators at the time of diagnosis. However, with the limited amount of encounter time in the clinic, it is unclear how much information is transferred and retained. Depending on the age at diagnosis, varying amounts of diabetes education may have been provided directly to the patient. As adolescents begin to assume greater shared responsibilities for diabetes management, review of key principles of diabetes management is warranted. An alternative solution may be to present the information to the adolescent using readily available technology via mobile phones, delivering content bit by bit on a daily basis using the process of microlearning (Hug, 2007). Microlearning emphasizes that learning content in small amounts within short periods of time, in this case, the information about symptom awareness and knowledge of diabetes management via text-messaging.
The value of creative self-management interventions is enhanced when one employs a communication approach focusing on technology familiar to adolescents. According to a recent Pew Survey (Lenhart, 2012) approximately 77% of American teens own mobile phones and at least 63% report texting daily. The study also found that mobile phone usage, specifically texting, is their favorite mode of communication. Texting using mobile devices presents opportunities to enhance diabetes management by extending health interventions beyond traditional care. Mobile technology makes it possible for patients to share relevant data at any time, not just at the time of a clinic visit, strengthening best evidence for optimal treatment.
Background Literature
Text messaging has been used extensively in supporting the communication and education of adults and adolescents with diabetes. Text messaging has been used to send blood glucose levels (Ferrer-Roca, Cárdenas, Diaz-Cardama, & Pulido, 2004) and general questions to providers (Rotheram-Borus et al., 2012), and to transmit educational materials (Arora, Peters, Agy, & Menchine, 2012; Foreman et al., 2012; Franklin, Waller, Pagliari, & Greene, 2006; Wangberg, Arsand, & Andersson, 2006), motivational messages (Arora et al., 2012; Franklin et al., 2006), and reminders to patients (Arora et al., 2012; Fischer et al., 2012; Franklin et al., 2006; Hanauer, Wentzell, Laffel, & Laffel, 2009). Few studies have investigated the effectiveness of using a text messaging system to improve glucose control (HbA1c). For the ones that did (Benhamou et al., 2007; Franklin et al., 2006; Hanauer et al., 2009), no significant improvements for HbA1c were obtained.
There are several systems that send questions to patients with diabetes to collect information, similar to the text messaging system previously designed by members of our research group for adolescent patients with asthma (Yun & Arriaga, 2013; Yun et al., 2012). These systems have been designed to send questions to inquire about hypoglycemic events (Tasker, Gibson, Franklin, Gregor, & Greene, 2007), adherence to healthy lifestyle behaviors (Rotheram-Borus et al., 2012), and blood pressure measurements (Fioravanti, Fico, Arredondo,& Leuteritz, 2011). Furthermore, Harris et al. (2010) took a different approach in providing feedback to patients on their reported blood glucose values by asking the patients why they thought their glucose values were high and asked follow-up questions based on the response (Harris et al., 2010). Unfortunately, none of the systems in these studies measured glycemic control.
One of the earliest text messaging systems specifically designed for youth with T1D was developed in Scotland, named Sweet Talk, with the intent to provide education and motivation for better self-management. These researchers designed a large text-messaging database to motivate adolescents to engage in four major activities: insulin injections, blood-glucose testing, healthy eating and exercise (Franklin et al., 2006). The system was rigorously evaluated with a yearlong randomized controlled trial of 92 participants enrolled in three arms of the study: conventional therapy, conventional therapy with Sweet Talk, and intensive therapy with Sweet Talk. Glycemic control (HbA1c) did not change in patients on conventional therapy without or with Sweet Talk, but improved in patients randomized to intensive therapy and Sweet Talk (P < 0.001). Although Sweet Talk alone when included with conventional therapy did not affect glycemic control, the program was associated with improvement in diabetes self-efficacy (P = 0.003) and self-reported adherence (P = 0.042). Eighty-two percent of youth reported that Sweet Talk had improved their diabetes self-management, and 90% wanted to continue receiving messages (Franklin, Greene, Waller, Greene, & Pagliari, 2008).
In a pilot trial of a mobile text-messaging intervention to improve diabetes adherence in adolescents, Mulvaney, Anders, Smith, Pittel, and Johnson (2012) designed messages according to individually-reported barriers to diabetes self-care (Mulvaney et al., 2012). After 3 months, system users rated the content, usability and experiences with the system as very favorable. Intervention and control groups had similar HbA1c levels at baseline. After 3 months, the mean HbA1c level in the intervention group was unchanged (8.8%), but the mean level in the control group was significantly higher (9.9%), P = 0.006. These results demonstrated the feasibility, user acceptance and a promising effect of a texting intervention on glucose control.
In summary, current evidence suggests that text messaging interventions are feasible and developmentally well-suited for adolescents, but their clinical significance for long-term diabetes management and glycemic control is uncertain. Most previous text-messaging studies were designed without the key input of diabetes team members (physicians, nurses, and certified diabetes educators) and were not based on behavioral theory (Herbert, Owen, Pascarella, & Streisand, 2013). Additional clinical trials that address approaches for incorporating these interventions with routine care and provider engagement are needed to determine the potential effect and sustainability on clinical outcomes (Herbert et al., 2013).
We therefore explored the feasibility of collecting valuable health information from adolescents related to symptom awareness as well as educating them through this modality (Lenhart, Ling, Campbell, & Purcell, 2010). We designed a system that sends questions to the adolescents’ mobile phones via text messages asking them about their recent symptoms and challenging them on their knowledge about diabetes. Previous studies based upon the health belief model (HBM) and conducted by this study team’s members used text messaging that required recipients to send a response to specific symptom and knowledge questions and showed promising results in improving the clinical outcomes of adolescents with asthma (Yun & Arriaga, 2013; Yun et al., 2012). Leveraging the success in these studies by members of our research group, we were interested in understanding whether similar technology could effectively support adolescents with T1D. Using a pilot, randomized controlled study, we hypothesized that adolescents receiving text messages (SMS, short message service) about symptom awareness and knowledge of diabetes would experience less diabetes distress, better quality of life and improved glucose control compared to either those receiving only text messages about symptom awareness or those receiving usual care. We also hypothesized that those receiving text messages about symptoms would experience better outcomes than those receiving usual care. To further evaluate the practical aspect of using a text messaging intervention with this population, we conducted exit interviews with participants, as well as health care providers (diabetes educators, physicians, and nurse practitioners) to ascertain their satisfaction and recommendations for improvements in the text messaging system.
System Design
The study design and theoretical rational are based upon a previously tested text-messaging system developed by members of this research team for adolescents with asthma (Yun & Arriaga, 2013; Yun et al., 2012). The current study design focused on examining the effect of text messaging between regular clinic appointments (3–4 months) to engage adolescents in their personal awareness of symptoms and knowledge of diabetes management. It included an alert interface for health care providers between regular clinic visits, as well as a summary of symptoms at the follow up visit to providers.
The system designed by our group differed from the aforementioned text messaging-based systems in several ways, including engagement of the team of pediatric diabetes health care providers and educators in the development and implementation of the intervention. Additionally, many of the questions from other studies required a fairly lengthy response. Our text messaging system only required a one character response (“Y”, “N”, “T”, “F”). Similar to the text messaging systems designed by Rotheram-Borus et al. (Rotheram-Borus et al., 2012) and Tasker et al. (Tasker et al., 2007), our system also delivered a maximum of one question a day to the study participants, thereby minimizing the burden of needing to respond to multiple text messages per day.
Our initial step in designing our text messaging system was to assess work flow and documentation in the diabetes clinic setting where recruitment would occur. A major observation at the time we conducted the study was that the clinic still relied on paper charts. There were no desktop computers in the exam rooms. When patients arrived for their appointments, their glucose levels in their meters were downloaded and printed so that the data could be placed in the chart. Between visits, one of the primary responsibilities of the diabetes educators was to communicate with the patient’s family. The diabetes educators returned phone calls, replied to emails, and made insulin adjustments for patients. These observations were essential to our system design that is described in the next section. The text messaging system contained three main components: (1) text messaging management for sending and receiving text messages; (2) Web-based dashboard for reviewing the text message responses by diabetes educators and providers; and (3) visualization printout from the dashboard.
Text Messaging Management
This component sends questions as text messages to the mobile phones of the adolescents with T1D. The adolescent then responds to the question by replying to the incoming text message. Depending on the study group, the adolescents receive at most one question a day on their mobile phones at a time of day they specified at recruitment.
Guided by the premises of HBM whereby perceived severity of disease, knowledge, and cue to action can influence health behavior (Rosenstock, 1974) two types of questions for text messages: symptom awareness (perceived severity) and knowledge (knowledge) were developed. The application of HBM for the question designs are described in detail in the prior asthma study paper (Yun & Arriaga, 2013). We designed both types of questions with input from multiple clinical collaborators (2 physicians and 1 nurse practitioner) to ensure clarity and appropriateness for the target population, thus providing face and content validity. There were 15 items for each type of questions.
To encourage the participants to respond, we made the process extremely simple. First, the questions were short (<110 characters). This length limitation was designed to fit each text messaging question (and knowledge answers) into one single text message as well as make it easier for the participants to read and understand the questions quickly. Second, the knowledge and symptom questions only required a binary, one-character response (Y/N or T/F). This design minimized the amount of typing effort in sending the response. If the participant did not know the answer to a symptom question, they were asked to respond “Yes” as shown in Table 1. The rationale to group the responses in this manner was so that those who were not cognizant of recognizing important symptoms, along with those who had actual symptoms, represented individuals with potential problems in diabetes management.
Table 1.
Diabetes symptom awareness questions.
| No. | Question | Weight |
|---|---|---|
| 1 | In the past 4 weeks, did you ever have times when you passed out even for a short time? N = No Y = Yes/Don’t know | 3 |
| 2 | In the past 4 weeks, did you ever have increased thirst? N = No Y = Yes/Don’t know | 1 |
| 3 | In the past 4 weeks, did your blood sugar drop under 70 before breakfast? N = No Y = Yes/Don’t know | 3 |
| 4 | In the past 4 weeks, did you ever urinate 2 or more times at night? N = No Y = Yes/Don’t know | 2 |
| 5 | In the past 4 weeks, have you had symptoms of a low blood sugar 3 or more times? Y = Yes/Don’t know | 1 |
| 6 | In the past 4 weeks, did you ever have nausea or vomiting? N = No Y = Yes/Don’t know | 0 |
| 7 | In the past 4 weeks, did you miss days of school because of your diabetes? N = No Y = Yes/Don’t know | 3 |
| 8 | In the past week, did you have more than 2 episodes of ketones? N = No Y = Yes/Don’t know | 2 |
| 9 | In the past 4 weeks, any trouble following your diabetes treatment when you are with friends? N = No Y = Yes/Don’t know | 0 |
| 10 | In the past 4 weeks, did something with your diabetes make you very unhappy? N = No Y = Yes/Don’t know | 0 |
| 11 | In the past 4 weeks, do you believe that your diabetes was out of control? N = No Y = Yes/Don’t know | 1 |
| 12 | In the past 4 weeks, did you have trouble taking your insulin as directed? N = No Y = Yes/Don’t know | 1 |
| 13 | In the past 4 weeks, is your family NOT giving you enough help with diabetes? N = No Y = Yes/Don’t know | 0 |
| 14 | In the past week, did you go to the emergency room or urgent care because of diabetes? N = No Y = Yes/Don’t know | 3 |
| 15 | In the past 4 weeks, did you ever stay overnight in the hospital because of diabetes? N = No Y = Yes/Don’t know | 3 |
The symptom questions were weighed from 0 to 3 with “0” representing no need to obtain a response from a health care provider at the time to “3,” indicating that the particular symptom may require follow up from the health care provider. The weights were determined by our clinical collaborators and were used to categorize the participants into “zones” that help the health care providers see which participant is struggling just by glancing at the Web-based dashboard and visualization printouts, which are described in the next two sections. The participants were not informed about the weight each question was given. An email alert was sent to the health care provider if a participant provided a response to a question with a weight of 2 or 3. Each email alert was initiated by a new response from a participant which was not influenced by prior responses. Because participants were predominantly asked to identify symptoms over a 4 week period of time, the alert system was not designed to address emergency or acute responses. For privacy concerns, the email only specified the problematic response but it did not specify which participant was having problems. To find out who the participant was, the health care provider had to log on to the Web-based dashboard.
The knowledge questions were based on common diabetes myths listed on several Websites (“12 Common Diabetes Myths Debunked,” n.d.; “Diabetes Facts,” n.d.; “Diabetes Myths,” n.d.) (Table 2). These questions were not weighted. When the participant responded to a question, the system sent a follow-up text message indicating whether the answer was correct and a short explanation of the reasoning behind the answer.
Table 2.
Diabetes knowledge questions and answers.
| No. | Question | Answer & explanation (incorrect version) |
|---|---|---|
| 1 | There is only one dangerous kind of diabetes. F = False T = True | Incorrect. There are many kinds of Diabetes: type 1, type 2 and gestational. All dangerous if untreated. |
| 2 | Nothing can be done to prevent diabetes complications. F = False T = True | Incorrect. Diabetes complications can be prevented or delayed by a treatment plan and regular checkups. |
| 3 | If you have diabetes, you should not exercise. F = False T = True | Incorrect. Exercise is important for diabetes management. It helps you use insulin better and control weight. |
| 4 | People who follow their diabetes treatment plan never have high blood sugar readings. F = False T = True | Incorrect. Your body is constantly changing so it is possible to get high readings when following treatment plans. |
| 5 | People diagnosed with diabetes are doomed. F = False T = True | Incorrect. Most people with diabetes are fully active. You can still live a fulfilling life with diabetes. |
| 6 | Diabetes is not that serious of an illness. F = False T = True | Incorrect. Diabetes causes more preventable deaths a year than breast cancer and AIDS combined. |
| 7 | Eating too much sugar causes diabetes. F = False T = True | Incorrect. Diabetes is caused by lifestyle factors (type 2) and unknown factors (type 1) and genetics (both). |
| 8 | If you have diabetes, you need to eat special diabetic food. F = False T = True | Incorrect. Your meal plan is the same as a healthy diet for anyone without diabetes. |
| 9 | You can catch diabetes from someone. F = False T = True | Incorrect. Diabetes is not contagious. |
| 10 | You are more likely to get colds and other illnesses. F = False T = True | Incorrect. However, you are advised to get flu shots because any illness can make diabetes harder to control. |
| 11 | If you have diabetes, fruit is not good for you. F = False T = True | Incorrect. Fruits are healthy so you should not avoid them. |
| 12 | If you have diabetes, you have to give up all sweets. F = False T = True | Incorrect. If you know how to read food labels, you can learn what you can eat when it comes to sweets. |
| 13 | If you have diabetes, sugar-free food is ok to eat. F = False T = True | Incorrect. Sugar-free food may still have high calories, fat and carbohydrates that are not good for you. |
| 14 | It is ok to eat sweets if your blood sugar is too low. F = False T = True | Incorrect. Sweets may have more calories than needed. Use pure glucose in tablets, gel or liquid to treat a low. |
| 15 | If you have diabetes, fat does not matter. F = False T = True | Incorrect. Dietary fat is problematic. It provides many calories and causes weight control problems. |
Web-Based Dashboard
The Web-based dashboard is an Adobe Flash® application that shows the participants’ responses over time. It is a modified version of the dashboard used in the asthma studies (Yun & Arriaga, 2013; Yun et al., 2012). The users of this dashboard are the diabetes educators that typically interact with patients between clinic visits. There are two views in the dashboard: patient status view and patient list view.
Patient Status View shows the status of the participants currently being followed based on their responses to the symptom awareness questions using a bar chart. This view is presented first when the diabetes educators log in to give an overview of the status of the participants based on their text message responses to the weighted symptom questions.
The participants are classified into three “zones.” The zones are color-coded in traffic-light colors: green, yellow, and red. All participants start in the green zone, indicating they are OK. The system updates the participant’s assigned zone when they respond. If they responded with an issue, they may be moved to different zone based on the accumulated weight of recent symptom question responses. For example, responding a blood sugar drop below 70 before breakfast in the past 4 weeks (question weight = 3) will immediately send the participant into the red zone and generate an email alert to the diabetes educators. The participant may only be moved to the yellow zone if responding to questions with a lighter weight (1 or 2). As the weights can be accumulated to determine zone assignments, participants may also be sent to the red zone if they responded with several minor issues within a limited amount of time. Note that the diabetes educators could manually move participants in the red zone to the green zone in a different view if they consider that the responded issues do not need further attention anymore.
The Patient List View shows the list of participants and their basic information including name, age, gender, zone, recent ER visit, recent hospitalizations because of diabetes, and mobile phone number. Clicking on the row of the participant in this view brings up detailed participant responses over time that allows visualization of the trends in each participant’s responses for either symptom awareness questions or diabetes knowledge questions. Every time the participant had a problematic response to a symptom question or answered incorrectly to a knowledge question, the corresponding score is increased and charted.
Visualization Printout From the Dashboard
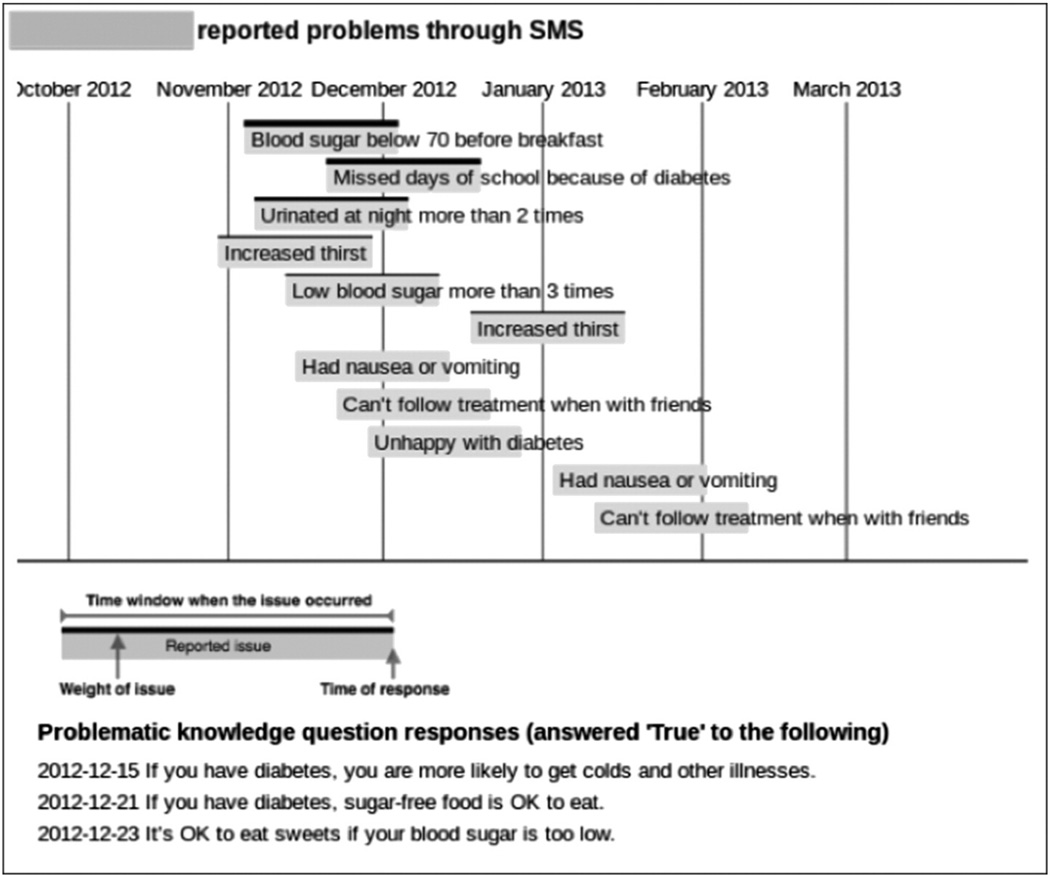
Because the diabetes clinic where we conducted the study relied primarily on paper charts, information from a Web-based dashboard would have been hard to use during the busy clinic visitation hours. As a result, we designed a visualization of the recent symptom and knowledge responses from the participant that can be printed out from the Web-based dashboard as shown in Figure 1. In the visualization, each horizontal bar represents an issue (from symptom questions) reported by the participant. For example, in Figure 1, the first bar shows that the participant responded Yes/Don’t know to symptom question 3 (Table 1): “In the past 4 weeks, did your blood sugar drop under 70 before breakfast?” in early December 2012. Therefore, the problem could have occurred between early November 2012 and early December 2012, which is the time window covered by the bar. The thickness of the upper border of the bar reflects the weight of the question. Problematic knowledge question responses are listed in the bottom if available. During the participant follow up visit, the visualization was available for health care providers to at-a-glance see how the participant had been responding to the text messaging system, and it was placed together with the rest of the participant’s chart to bring into the exam room as a reference.
Figure 1.
Web-based dashboard: Visualization printout presented to health care providers at follow-up visit.
Method
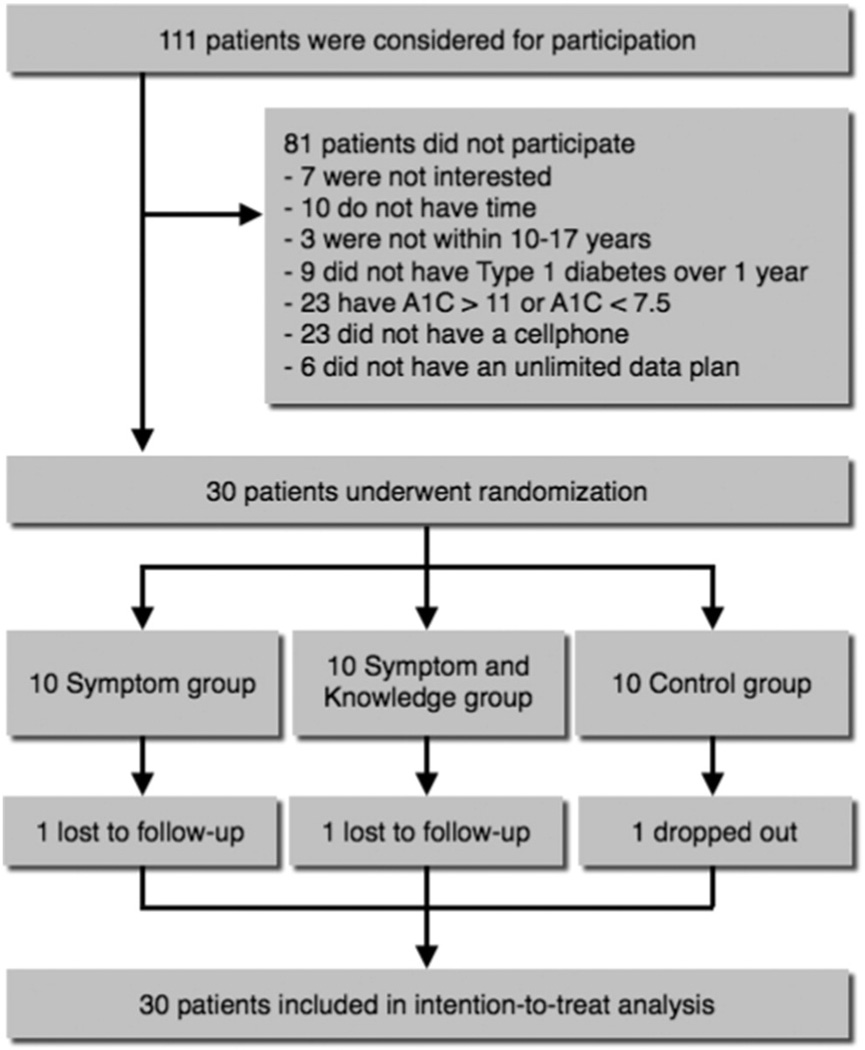
We recruited 30 preadolescents or adolescents with T1D at a diabetes clinic in the Southeast United States during their regularly scheduled checkup from October to December 2012. Inclusion criteria were as follows: (1) be 10–17 years of age, (2) have been diagnosed with TID for over 1 year, (3) have the most recent HbA1c test result between 7.5% and 11%, (4) have his or her own cell phone, (5) have an unlimited SMS text plan, and (6) be able to read English at a 5th grade level. Participants were randomly assigned into one of the following three equal-sized groups (Figure 2):
Control group: Participants in this group did not receive any text messages from us.
Symptom awareness group (S group): Participants in this group received only the symptom questions. The questions were delivered every other day.
Symptom awareness and knowledge group (SK group): Participants in this group received both the symptom and knowledge questions. A question was delivered every day but with alternating types.
Figure 2.
Recruitment flow diagram.
Outcome Measures
We measured both physiological and psychological outcomes in the beginning and end of the study. The technology usage by the participants was measured by the response rate to the text messaging system. The response rate provided information to support fidelity of the text messaging intervention.
Metabolic Control
Glycosylated hemoglobin (HbA1c) provides objective criteria of metabolic control over the most recent 8–12 weeks. Analyses was performed using the Bayer-Siemens Diagnostics DCA2000® (Siemens Medical Solutions Diagnostics, Tarrytown, NY) which provides results in 6 minutes using a fingerstick blood sample (normal range =4.2–6.3%). The correlation coefficients between DCA 2000 and high-performance liquid chromatography (HPLC) are reported between 0.94 and 0.98 from a large, multi-site clinical study (Guerci et al., 1997). The accuracy and reliability of this method are previously reported (Arsie et al., 2000).
Quality of Life Scales
We used an updated version of the Problem Areas in Diabetes (PAID) questionnaire (Welch, Weinger, Anderson, & Polonsky, 2003) and the Diabetes Quality of Life for Youth (DQOLY) questionnaire (Ingersoll & Marrero, 1991) to assess the influence of having diabetes on the quality of life of the participants. The PAID we used is a 20-item questionnaire, 5-point Likert scale, that measures overall diabetes-related emotional distress. Participants rate the degree to which each item is currently problematic for them, from 0 (“not a problem”) to 4 (“serious problem”). A total scale score was computed by summing total item responses and multiplying them by 1.25. Cronbach’s alpha was reported as .96 (Paddison, Alpass, & Stephens, 2010). The PAID has convergent validity as noted with positive associations to measures of general emotional distress, fear of hypoglycemia, and negative associations to adherence with blood glucose testing, insulin usage, and meal planning.
The DQOLY (is a well-established questionnaire, composed of a 17-item Diabetes Life Satisfaction scale, a 23-item Disease Impact scale, and an 11-item Disease-Related Worries scale. Original Cronbach’s alpha reliabilities for the subscales range from .82 to .85. Each item is scored on a scale of 1 to 5 (1 = never or very unsatisfied to 5 = all of the time or very satisfied).
Study Procedure
Institutional review board approval was obtained before the start of the study. We approached potential participants at the diabetes clinic about the research study. If they expressed interest, we then assessed if they were eligible to participate. Child assent and parental permission (consent) were obtained. After obtaining consent, we gave the participants several questionnaires to collect data on their demographic information, mobile and Internet technology usage, and baseline outcome measures (i.e., HbA1c, PAID, and DQOLY instruments). All the questionnaires took about 30–60 minutes to finish.
After filling out the questionnaires, the participants were given an envelope with a letter that randomized them into one of the three study groups. The letter specified which study group the participants were randomized into and outlined the intervention they would receive. The participants were compensated $15 in cash at the end of the recruitment. Within days, text messages began to be sent to the participants’ mobile phones.
We gathered data (text responses) over the period between two regularly scheduled visits. This period is typically 3–4 months. This duration is also comparable to a prior asthma studies with a similar technology intervention (Yun & Arriaga, 2013; Yun et al., 2012). This short-term evaluation was done to examine the need for intervention refinement prior to use in routine clinical practice for pediatric diabetes management over longer time periods. Consent for study participation was also obtained for the diabetes educators who were trained and given access to the Web-based dashboard at the beginning of the study to monitor the responses. These educators were able to receive email alerts sent to their clinic’s general diabetes email address.
We again met the participants at their follow up clinic visit. We obtained consent from the health care providers that saw the participants that day and provided the visualization printout from the dashboard (only for those in the intervention groups) so that they could use it in the visit. During this visit the outcome measures (described earlier) and semi-structured interviews that focused on understanding the adolescents’ experiences using our technology were completed. After the data collection process, the adolescents were given another $15 and were thanked for their participation.
Once the study was completed (all returning participants completed post evaluation) we sought to get feedback from the health care providers that interacted with the study groups. Following informed consent, health care providers were interviewed on their perspectives for using the text-messaging program. Interviews of adolescents and health care providers included similar questions regarding what they liked most about the text-messaging system, what they liked least and suggestions they had for improvement. All interviews were audio taped at the end of the trial and transcribed verbatim.
Data Analysis
The statistical analyses were performed in R (ver. 3.0.1), a free statistical analysis tool (R Core Team, 2012). The baseline data were compared between the study groups with chi square analysis for categorical variables and one-way analysis of variance (ANOVA) for continuous variables. Intention-to-treat analyses were conducted. Paired-t tests were used to examine changes within groups over time. Analysis of covariance (ANCOVA) was used to study changes between groups, controlling for the baseline data. The effect sizes were calculated with Cohen’s d for paired-t tests within groups and partial eta squared for ANCOVA between groups. Pairwise comparisons between groups with the Tukey method were conducted. Statistical significance was defined as P < .05 with one-sided tests because we hypothesized that our technology would improve the physiological and psychological outcomes. Qualitative analyses based on semi-structured interview questions were completed using matrices to organize themes in the data based upon responses from adolescents and health care providers.
Results
Of the 30 adolescents enrolled into the study, 27 completed the study. Initially, 10 participants were recruited in each group. Figure 2 provides details about attrition. The demographic characteristics of the participants are shown in Table 3. The mean age of the participants was 13.7 years. Among these participants, 57% were female and 77% were Caucasian. At baseline, there were no statistically significant differences between groups in age, gender, duration of diabetes, HbA1c, PAID scale, DQOLY-Worries about diabetes subscale, and DQOLY-Satisfaction with diabetes subscale. However, there were significant differences in race (P = .031) and DQOLY-Impact on diabetes subscale (P = .005). We had significantly more African American participants randomized into group 3 (5/10) and a higher DQOLY-Impact on diabetes baseline for group SK (Tables 3 and 4).
Table 3.
Demographic characteristics of the adolescents.
| Control (n = 10) |
Symptom (n = 10) |
Symptom + Knowledge (n = 10) |
|
|---|---|---|---|
| Age (years) | 12.9 (2.183) | 13.8 (1.874) | 14.5 (1.650) |
| Sex (female) | 5 (50%) | 6 (60%) | 6 (60%) |
| Duration of diabetes (years) | 7.3 (3.164) | 6 (4.662) | 7.6 (4.033) |
| Race | |||
| Caucasian | 10 (100%) | 8 (80%) | 5 (50%) |
| African American | 0 (0%) | 1 (10%) | 5 (50%) |
| Asian | 0 (0%) | 1 (10%) | 0 (0%) |
Data are means (±SD) or numbers (%).
Table 4.
Outcome measures for the control (C), symptom (S) and symptom + knowledge (SK) groups.
| Variable | Baseline | Follow-up | Diff | Effect | P |
|---|---|---|---|---|---|
| HbA1c (%) | |||||
| C | 8.78 (0.728) | 8.57 (0.786) | −0.21 | 0.466 | .087 |
| S | 8.60 (0.867) | 8.23 (1.370) | −0.37 | 0.394 | .122 |
| SK | 9.23 (1.093) | 9.20 (1.346) | −0.03 | 0.037 | .455 |
| PAID | |||||
| C | 7.13 (6.873) | 10.48(13.844) | 3.35 | −0.312 | .825 |
| S | 14.88 (13.339) | 14.86 (14.737) | −0.02 | 0.001 | .498 |
| SK | 18.63 (18.796) | 13.89 (17.848) | −4.74 | 0.442 | .098 |
| DQOL-Impact on diabetes | |||||
| C | 44.50 (8.303) | 48.78 (10.654) | 4.28 | −0.625 | .960 |
| S | 49.10 (12.032) | 49.00 (14.337) | −0.1 | 0.015 | .482 |
| SK | 61.20 (11.322) | 50.78 (8.917) | −10.42 | 1.457 | <.001 ** |
| DQOL-Worries about diabetes | |||||
| C | 17.80 (5.827) | 19.00 (6.566) | 1.2 | −0.214 | .743 |
| S | 21.00 (7.211) | 19.60 (8.514) | −1.4 | 0.233 | .240 |
| SK | 25.90 (10.236) | 18.11 (6.045) | −7.79 | 0.856 | .012 * |
| DQOL-Satisfaction with diabetes | |||||
| C | 71.70 (9.730) | 65.22 (19.798) | −6.48 | 0.449 | .905 |
| S | 60.20 (20.335) | 66.89 (10.888) | 6.69 | −0.269 | .209 |
| SK | 62.50 (13.410) | 66.22 (11.679) | 3.72 | −0.318 | .170 |
Data are means (SD) or frequencies (%).
P < 0.05.
P < 0.001.
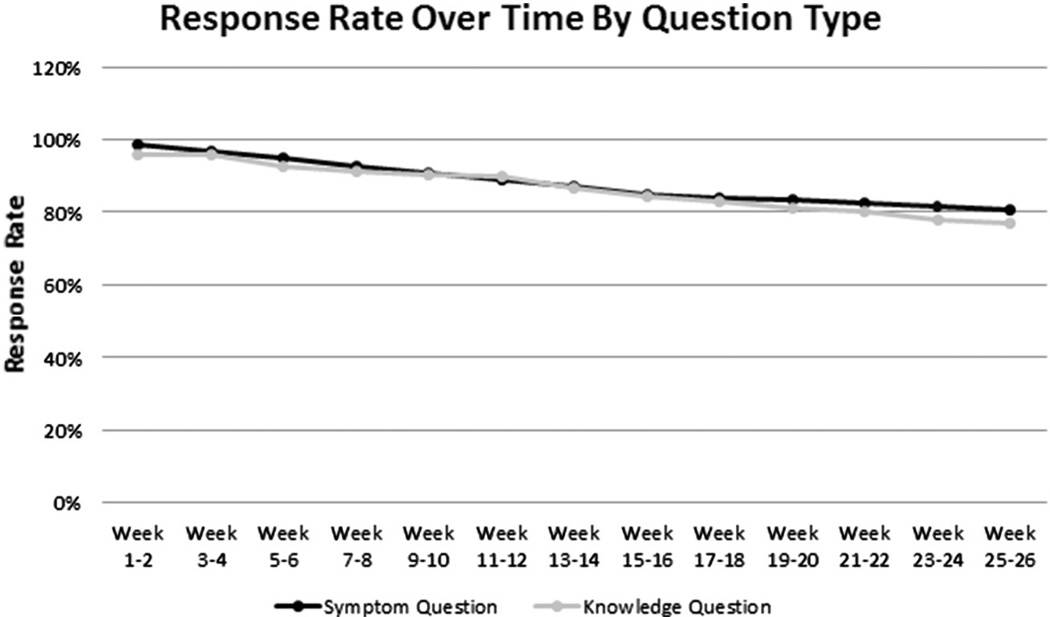
The response rate to text messages was calculated by dividing the total number of responses by the total number of questions sent. Figure 3 shows the response rates calculated at the end of every 2 week period in the study by question type. Therefore, the last data point is the response rate for the entire study. The response rate for the symptom questions was 80.88%, whereas the response rate for the knowledge questions was 76.96%. By intervention group, the response rate for S group was 87.97% and for SK group was 75.35%. The overall response rate by the end of the study was 79.58% for all the participants in the intervention groups.
Figure 3.
Response rate over time by question type.
The system sent out a total of 60 email alerts to the health care team. Of the 60 alerts, 28 were from a question with a weight of “3” which included 17 instances of participants reporting that their sugar dropped below 70 before breakfast, 9 instances of missing school for diabetes related reasons, and 2 reports of emergency room visits for diabetes related problems. The adolescent’s responses were based upon symptoms occurring over the past 1 or 4 weeks, depending on the question, at the time of the response. Four diabetes educators were trained and given access to the Web-based dashboard. The decision to respond to any of the alerts was based upon their personal interpretation of the need to respond for a particular patient. Only 2 of the 4 educators accessed it after their training sessions during the study period. There were a total of 11 logins in the first 15 weeks since the first participant was recruited. One educator logged in 2 times and the other logged in 9 times. The fact that the alerts were not “real time” but rather a reflection of symptoms over several weeks likely diminished any urgency for the educators to intervene. Knowing that parents or other family members are often available to respond and seek follow up care for their child may have also influenced a lower response from the educators.
There were no significant differences in HbA1c changes between the three groups when controlling for the baseline values. However, over time, all three groups had non-significant mean reductions in HbA1c levels. There was no significant difference in HbA1c change between any two of the study groups. Of particular note, is the higher baseline HbA1c in the SK group when compared to the other groups. Fifty percent of the adolescents in the SK group were African American. Prior evidence has indicated that minority youth have greater risks for poorer metabolic control (Hilliard, Wu, Rausch, Dolan, & Hood, 2013), although, the cause for this difference is currently unknown.
In contrast to metabolic control, the use of our technology significantly improved some aspects of quality of life for the adolescents in the SK group. No significant changes in quality of life measures between baseline and follow-up were found in the control or S group; however, the DQOLY-Worries subscale scores decreased in the S group and increased in the control group (Table 4). The SK group significantly reduced their worries and perceived impact about diabetes on their lives compared to baseline. In comparison to the control group and S group, adolescents in the SK group significantly improved their perception of the impact of diabetes on their lives (Table 5). Adolescents in the SK group reported a decrease in diabetes distress measured with the PAID scale at the end of the trial when compared to their baseline and to the control group. Although these changes were not statistically significant at the 0.05 level, they did support a trend toward improvement in perceptions of diabetes distress. In contrast, there were no significant differences in perceived satisfaction with diabetes either over time or between groups. However, the DQOLY-Satisfaction subscale scores increased at follow up for both the S and SK groups, and decreased for controls.
Table 5.
Outcome measures—between groups.
| Control–Group S |
Control–Group SK |
Group S–Group SK |
All groups |
|||||
|---|---|---|---|---|---|---|---|---|
| Difference | P | Difference | P | Difference | P | Effect size | P | |
| HbA1c (%) | −0.1570 | .627 | 0.1724 | .960 | 0.3293 | .993 | 0.031 | .666 |
| PAID | −2.351 | .589 | −6.587 | .208 | −4.236 | .381 | 0.071 | .383 |
| DQOL-Impact on diabetes | −3.7951 | .263 | −12.5765 | .003 ** | −8.7814 | .022 * | 0.311 | .008 ** |
| DQOL-Worries about diabetes | −1.0174 | .653 | −4.9842 | .122 | −3.9667 | .192 | 0.112 | .214 |
| DQOL-Satisfaction with diabetes | 4.7631 | .497 | 3.4745 | .589 | −1.2886 | .900 | 0.020 | .771 |
P < 0.05.
P < 0.01.
Semi-structured interviews were conducted with 27 adolescents who completed the study. Eight health care providers (2 nurse practitioners, 3 diabetes educators, and 3 physicians) were interviewed for feedback regarding the use of the email notification system, dashboard and clinic printout. Key themes from adolescents included improving awareness of symptoms, receiving reminders for checking glucose, gaining a better understanding of diabetes management for glucose testing and checking urine ketones. These were all themes that were reflected in the text messages. Adolescents reported that the system was easy, simple, and enjoyable to use, but did not like the repetition of the questions. Recommendations to improve the system included a greater variety of questions to decrease the repetition as well as more personal questions regarding day-to-day management.
When queried about the utility of the visualization data for their participants, the health care providers emphasized the value of learning about home-based diabetes problems, misconceptions about diabetes by adolescents and knowledge of adolescents’ feelings about diabetes. The system allowed the health care providers to target conversations, during the clinic visit, to issues pertinent to the adolescents. It enabled providers to use text messaging data to ask more specific questions that otherwise might have been overlooked. Several providers remarked that the information gained from the symptom and knowledge questions regarding psychosocial issues were extremely helpful in facilitating dialogue. The health care providers did not report any change in the amount of workload. Recommendations included adding more questions related to mental health and coping and questions related to needed intervention on insulin management, or low or high blood glucose.
Discussion
This pilot investigation focused on using text-messaging about diabetes symptom awareness and knowledge to improve quality of life and glucose control in adolescents with T1D. It also included a Web-based dashboard that allowed the health care providers to access this information as it was being sent by the participants and to visualize the responses for a given participant. We were able to determine that receiving a daily text message lessened some of the negative impact of having diabetes in the study participants. The text message response rate in our system was around 80% for both symptom and knowledge questions, indicating that adolescents were quite receptive to this type of technology for intervention delivery. This preference for text messaging was also noted by Tasker et al. (2007) who found that young participants responded more to questions when they were delivered using mobile phone as opposed to computer or paper diary.
Results indicated trends toward improvement in life satisfaction and metabolic control, as well as a decrease in worries related to diabetes in the group receiving text messages on symptom awareness every other day. These findings support the value in further examination of developing additional text messages that can be incorporated on a daily basis to continue to improve symptom awareness and overall diabetes management in adolescents. Prior research has shown that diabetes quality of life of adolescents, measured by the DQOLY, is strongly correlated with metabolic control as measured by HbA1c (Guttmann-Bauman, Flaherty, Strugger, & McEvoy, 1998). Therefore, future studies should extend the study duration to further investigate the effectiveness of our technology in improving not only quality of life outcomes but also glycemic control.
For the measure of quality of life using the PAID and DQOLY questionnaires (impact, worries), the groups receiving more text messages improved more (SK group > S group > Control). This finding is in line with the findings from the asthma studies (Yun & Arriaga, 2013; Yun et al., 2012). We think the reason for this result is that more text messages help adolescents increase awareness of their symptoms, possibly leading to better adherence to treatment plans and insulin management. As our participants only received at most one question a day, there could be an opportunity to increase the number of text messages to see if there can be further improvement in diabetes outcomes.
Our study design included the additional questions about diabetes knowledge for group SK when compared to group S. As a result, further investigations should address whether the inclusion of only knowledge questions are valuable to improving the study outcomes. This type of comparison could be relevant since some adolescents may not have received comprehensive self-management diabetes education if they were very young at the time of diagnosis. Parents may have been the recipients of the education, making developmental appropriate diabetes education a priority for adolescents who have not previously received it.
Our study has a number of limitations: (1) the sample size is small, (2) the study was conducted in one diabetes clinic, (3) the duration of the study was short (minimal 3–4 months for each participant), and (4) only adolescents who owned mobile phones and unlimited text messaging plans could participate. Although we found preliminary evidence that the system was able to improve quality of life and have sustained engagement as measured by the response rate, further studies are required to see if our results can be generalized to a broader range of adolescents with T1D. By replicating the technology for delivering this type of intervention not only for adolescents with asthma (Yun et al., 2012), but also with those with T1D, we showed that such a text messaging system is potentially clinically applicable to other youth populations that are managing chronic illnesses. It also showed that enhancing continuous assessment of patient symptoms and knowledge has value for the patient outcomes as well as potential to improve point of care interactions between the health care providers and the patient.
We found early clinical evidence that adolescents with T1D may benefit from a text messaging system. For adolescents in the SK group, the significant improvement of quality of life showed that our technology was effective in the short term between regular clinic visits. Such findings in this pilot study lend support for innovative approaches from the multidisciplinary diabetes team (nurses, physicians, diabetes educators) to enhance support for diabetes management between routine follow up visits. Future investigation on the use of text-messaging technology to reach adolescents who may be the most vulnerable for optimal diabetes control is certainly warranted. Larger samples sizes will also allow researchers to further analyze differences in outcomes for subgroups, such as gender and minority status.
Although we found evidence to support the use of mobile technologies for enhancing quality of life in adolescents with T1D, health care providers did not engage with the Web-based dashboard regularly during the study. This was the case even when they received emails alerting them to the fact that participants had answered yes to a question that landed them in the “red zone.” This was likely due to the fact that this was a short-term study with only 20 participants. Thus, it did not warrant change to their workflow. However, interview data indicated that health care providers found that having information about their patients’ symptoms and knowledge between visits lead to improved communication during the follow up visit. This is important because there is evidence that improved communication between the health care provider and the patients leads to greater adherence in patients and satisfaction with their care regiment (Martin, Williams, Haskard, & DiMatteo, 2005). In summary, key nursing implications should focus on assessing personal choices of adolescents for using mobile technologies to achieve greater awareness of diabetes-related symptoms and knowledge regarding appropriate self-management. Because text-messaging is so widely used by adolescents, more research is clearly needed to evaluate the most effective design that resides in their hands to enhance daily management and also facilitate provider communication when needed, between regular clinic visits and during patient-provider encounters.
Acknowledgments
We would like to thank the clinical staff that supported this study and our study participants.
References
- [Retrieved January 30, 2014];12 Common Diabetes Myths Debunked (n.d.) http://www.caring.com/articles/diabetes-myths.
- American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2014;37:S14–S80. doi: 10.2337/dc14-S014. http://dx.doi.org/10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- Amiel SA, Sherwin RS, Simonson DC, Lauritano AA, Tamborlane WV. Impaired insulin action in puberty. A contributing factor to poor glycemic control in adolescents with diabetes. The New England Journal of Medicine. 1986;315:215–219. doi: 10.1056/NEJM198607243150402. http://dx.doi.org/10.1056/NEJM198607243150402. [DOI] [PubMed] [Google Scholar]
- Arora S, Peters AL, Agy C, Menchine M. A mobile health intervention for inner city patients with poorly controlled diabetes: Proof-of-concept of the TExT-MED program. Diabetes Technology & Therapeutics. 2012;14:492–496. doi: 10.1089/dia.2011.0252. http://dx.doi.org/10.1089/dia.2011.0252. [DOI] [PubMed] [Google Scholar]
- Arsie MP, Marchioro L, Lapolla A, Giacchetto GF, Bordin MR, Rizzotti P, et al. Evaluation of diagnostic reliability of DCA 2000 for rapid and simple monitoring of HbA1c. Acta Diabetologica. 2000;37:1–7. doi: 10.1007/s005920070028. [DOI] [PubMed] [Google Scholar]
- Benhamou P-Y, Melki V, Boizel R, Perreal F, Quesada J-L, Bessieres-Lacombe S, et al. One-year efficacy and safety of Web-based follow-up using cellular phone in type 1 diabetic patients under insulin pump therapy: The PumpNet study. Diabetes & Metabolism. 2007;33:220–226. doi: 10.1016/j.diabet.2007.01.002. http://dx.doi.org/10.1016/j.diabet.2007.01.002. [DOI] [PubMed] [Google Scholar]
- [Retrieved January 30, 2014];Diabetes Facts ()). 10 Common myths busted. http://www.lifescript.com/health/centers/diabetes/articles/10_diabetes_myths_busted.aspx.
- [Retrieved January 30, 2014];Diabetes myths ()) http://www.diabetes.org/diabetes-basics/myths/
- Ferrer-Roca O, Cárdenas A, Diaz-Cardama A, Pulido P. Mobile phone text messaging in the management of diabetes. Journal of Telemedicine and Telecare. 2004;10:282–285. doi: 10.1258/1357633042026341. [DOI] [PubMed] [Google Scholar]
- Fioravanti A, Fico G, Arredondo MT, Leuteritz J-P. A mobile feedback system for integrated E-health platforms to improve self-care and compliance of diabetes mellitus patients; Conference Proceedings: Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Conference; 2011. pp. 3550–3553. http://dx.doi.org/10.1109/IEMBS.2011.6090591. [DOI] [PubMed] [Google Scholar]
- Fischer HH, Moore SL, Ginosar D, Davidson AJ, Rice-Peterson CM, Durfee MJ, et al. Care by cell phone: Text messaging for chronic disease management. The American Journal of Managed Care. 2012;18:e42–e47. [PubMed] [Google Scholar]
- Foreman KF, Stockl KM, Le LB, Fisk E, Shah SM, Lew HC, et al. Impact of a text messaging pilot program on patient medication adherence. Clinical Therapeutics. 2012;34:1084–1091. doi: 10.1016/j.clinthera.2012.04.007. http://dx.doi.org/10.1016/j.clinthera.2012.04.007. [DOI] [PubMed] [Google Scholar]
- Franklin VL, Greene A, Waller A, Greene SA, Pagliari C. Patients’ engagement with “Sweet Talk” - A text messaging support system for young people with diabetes. Journal of Medical Internet Research. 2008;10:e20. doi: 10.2196/jmir.962. http://dx.doi.org/10.2196/jmir.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin VL, Waller A, Pagliari C, Greene SA. A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabetic Medicine: A Journal of the British Diabetic Association. 2006;23:1332–1338. doi: 10.1111/j.1464-5491.2006.01989.x. http://dx.doi.org/10.1111/j.1464-5491.2006.01989.x. [DOI] [PubMed] [Google Scholar]
- Guerci B, Durain D, Leblanc H, Rouland JC, Passa P, Godeau T, et al. Multicentre evaluation of the DCA 2000 system for measuring glycated haemoglobin. DCA 2000 Study Group. Diabetes & Metabolism. 1997;23:195–201. [PubMed] [Google Scholar]
- Guttmann-Bauman I, Flaherty BP, Strugger M, McEvoy RC. Metabolic control and quality-of-life self-assessment in adolescents with IDDM. Diabetes Care. 1998;21:915–918. doi: 10.2337/diacare.21.6.915. [DOI] [PubMed] [Google Scholar]
- Hanauer DA, Wentzell K, Laffel N, Laffel LM. Computerized Automated Reminder Diabetes System (CARDS): E-mail and SMS cell phone text messaging reminders to support diabetes management. Diabetes Technology & Therapeutics. 2009;11:99–106. doi: 10.1089/dia.2008.0022. http://dx.doi.org/10.1089/dia.2008.0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris LT, Tufano J, Le T, Rees C, Lewis GA, Evert AB, et al. Designing mobile support for glycemic control in patients with diabetes. Journal of Biomedical Informatics. 2010;43:S37–S40. doi: 10.1016/j.jbi.2010.05.004. http://dx.doi.org/10.1016/j.jbi.2010.05.004. [DOI] [PubMed] [Google Scholar]
- Herbert L, Owen V, Pascarella L, Streisand R. Text message interventions for children and adolescents with type 1 diabetes: A systematic review. Diabetes Technology & Therapeutics. 2013;15:362–370. doi: 10.1089/dia.2012.0291. http://dx.doi.org/10.1089/dia.2012.0291. [DOI] [PubMed] [Google Scholar]
- Hilliard ME, Wu YP, Rausch J, Dolan LM, Hood KK. Predictors of deteriorations in diabetes management and control in adolescents with type 1 diabetes. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine. 2013;52:28–34. doi: 10.1016/j.jadohealth.2012.05.009. http://dx.doi.org/10.1016/j.jadohealth.2012.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hug T. Didactics of microlearning: Concepts, discourses and examples. Waxmann Verlag; 2007. [Google Scholar]
- Ingersoll GM, Marrero DG. A modified quality-of-life measure for youths: Psychometric properties. The Diabetes Educator. 1991;17:114–118. doi: 10.1177/014572179101700219. [DOI] [PubMed] [Google Scholar]
- Lenhart A. Pew Internet teens, smartphones & texting. Survey Results and Analysis. 2012 1615 L St., NW - Suite 700: The Pew Research Center, 34 Retrieved from http://pewinternet.org/Reports/2012/Teens-and-smartphones.aspx.
- Lenhart Amanda, Ling R, Campbell S, Purcell K. Teens and mobile phones. 2010 Pew Internet & American Life Project (Retrieved from http://www.pewinternet.org/Reports/2010/Teens-and-Mobile-Phones.aspx)
- Martin LR, Williams SL, Haskard KB, DiMatteo MR. The challenge of patient adherence. Therapeutics and Clinical Risk Management. 2005;1:189–199. [PMC free article] [PubMed] [Google Scholar]
- Mulvaney SA, Anders S, Smith AK, Pittel EJ, Johnson KB. A pilot test of a tailored mobile and web-based diabetes messaging system for adolescents. Journal of Telemedicine and Telecare. 2012 doi: 10.1258/jtt.2011.111006. http://dx.doi.org/10.1258/jtt.2011.110006. [DOI] [PMC free article] [PubMed]
- Nurick MA, Johnson SB. Enhancing blood glucose awareness in adolescents and young adults with IDDM. Diabetes Care. 1991;14:1–7. doi: 10.2337/diacare.14.1.1. [DOI] [PubMed] [Google Scholar]
- Paddison C, Alpass FM, Stephens CV. Using the common sense model of illness self-regulation to understand diabetes-related distress: The importance of being able to “make sense” of diabetes. New Zealand Journal of Psychology. 2010;39:44–49. [Google Scholar]
- R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2012. (Retrieved from http://www.R-project.org/) [Google Scholar]
- Rausch JR, Hood KK, Delamater A, Shroff Pendley J, Rohan JM, Reeves G, et al. Changes in treatment adherence and glycemic control during the transition to adolescence in type 1 diabetes. Diabetes Care. 2012;35:1219–1224. doi: 10.2337/dc11-2163. http://dx.doi.org/10.2337/dc11-2163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenstock IM. Historical origins of the health belief model. Health Education Monographs. 1974;2:328–335. doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Tomlinson M, Gwegwe M, Comulada WS, Kaufman N, Keim M. Diabetes buddies: Peer support through a mobile phone buddy system. The Diabetes Educator. 2012;38:357–365. doi: 10.1177/0145721712444617. http://dx.doi.org/10.1177/0145721712444617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan CM, Dulay D, Suprasongsin C, Becker DJ. Detection of symptoms by adolescents and young adults with type 1 diabetes during experimental induction of mild hypoglycemia: Role of hormonal and psychological variables. Diabetes Care. 2002;25:852–858. doi: 10.2337/diacare.25.5.852. [DOI] [PubMed] [Google Scholar]
- SEARCH for Diabetes in Youth Study. GroupLiese AD, D’Agostino RB, Jr, Hamman RF, Kilgo PD, Lawrence JM, et al. The burden of diabetes mellitus among US youth: Prevalence estimates from the SEARCH for Diabetes in Youth Study. Pediatrics. 2006;118:1510–1518. doi: 10.1542/peds.2006-0690. http://dx.doi.org/10.1542/peds.2006-0690. [DOI] [PubMed] [Google Scholar]
- Tasker APB, Gibson L, Franklin V, Gregor P, Greene S. What is the frequency of symptomatic mild hypoglycemia in type 1 diabetes in the young?: Assessment by novel mobile phone technology and computer-based interviewing. Pediatric Diabetes. 2007;8:15–20. doi: 10.1111/j.1399-5448.2006.00220.x. http://dx.doi.org/10.1111/j.1399-5448.2006.00220.x. [DOI] [PubMed] [Google Scholar]
- Wangberg SC, Arsand E, Andersson N. Diabetes education via mobile text messaging. Journal of Telemedicine and Telecare. 2006;12:55–56. doi: 10.1258/135763306777978515. http://dx.doi.org/10.1258/135763306777978515. [DOI] [PubMed] [Google Scholar]
- Welch G, Weinger K, Anderson B, Polonsky WH. Responsiveness of the Problem Areas In Diabetes (PAID) questionnaire. Diabetic Medicine: A Journal of the British Diabetic Association. 2003;20:69–72. doi: 10.1046/j.1464-5491.2003.00832.x. [DOI] [PubMed] [Google Scholar]
- Writing Group for the SEARCH for Diabetes in Youth Study. GroupDabelea D, Bell RA, D’Agostino RB, Jr, Imperatore G, Johansen JM, et al. Incidence of diabetes in youth in the United States. JAMA, the Journal of the American Medical Association. 2007;297:2716–2724. doi: 10.1001/jama.297.24.2716. http://dx.doi.org/10.1001/jama.297.24.2716. [DOI] [PubMed] [Google Scholar]
- Yun T-J, Arriaga RI. A text message a day keeps the pulmonologist away. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems; New York, NY, USA: ACM; 2013. pp. 1769–1778. http://dx.doi.org/10.1145/2470654.2466233. [Google Scholar]
- Yun TJ, Jeong HY, Hill TD, Lesnick B, Brown R, Abowd GD, et al. Using SMS to provide continuous assessment and improve health outcomes for children with asthma; Proceedings of the 2n d ACM SIGHIT International Health Informatics Symposium; New York, NY, USA: ACM; 2012. pp. 621–630. http://dx.doi.org/10.1145/2110363.2110432. [Google Scholar]