Abstract
Setting:
Zomba Central Hospital, Malawi.
Objective:
To determine diagnostic management and outcomes of pulmonary tuberculosis (PTB) suspects admitted to adult wards.
Design:
A retrospective, cross-sectional review of medical records of patients admitted to hospital between July and September 2010.
Results:
There were 141 PTB suspects. Sputum examination was requested and performed in 67 (48%) suspects, but none were smear-positive. Chest X-ray (CXR) was requested and performed in 26 (39%) suspects whose sputum smears were negative. Eleven suspects had a CXR suggestive of PTB: two were started on TB treatment and eight died before treatment started. Human immunodeficiency virus (HIV) status was known for 50 patients (35% of all suspects) on admission, all of whom were HIV-positive. HIV testing was requested for 37 patients, but was only performed in 12, five of whom were HIV-positive. Only one patient was referred for antiretroviral treatment. There were 41 (29%) deaths, eight of whom had probable TB and were not treated. In the remaining 33 patients who died, only nine (27%) had sputum smears examined and four (12%) had a CXR.
Conclusion:
The study shows inadequacies in the diagnostic management of PTB suspects in the Zomba Central Hospital, but suggests opportunities for improvement.
Keywords: PTB suspects, diagnosis, management, outcomes, Malawi
Abstract
Contexte:
Hôpital Central de Zomba au Malawi.
Objectif:
Déterminer la prise en charge diagnostique et les résultats obtenus chez les suspects de tuberculose pulmonaire (TBP) hospitalisés dans des salles pour adultes.
Schéma:
Revue rétrospective transversale des dossiers médicaux des patients admis à l’hôpital entre juillet et septembre 2010.
Résultats:
Il y a eu 141 sujets suspects de TBP. L’examen des crachats a été demandé et exécuté chez 67 suspects (48%), mais on n’a observé de bacilloscopie positive des frottis chez aucun. Le cliché thoracique (CXR) a été demandé et exécuté chez 26 suspects (39%) dont la bacilloscopie des frottis de crachats était négative. Chez 11 suspects, le CXR était suggestif d’une TBP : deux ont été mis sous traitement antituberculeux et huit sont décédés avant la mise en route du traitement. Le statut du virus de l’immunodéficience humaine (VIH) était connu chez 50 patients à l’admission (35% de l’ensemble des suspects), qui étaient tous séropositifs pour le VIH. Le test VIH a été demandé chez 37 patients, mais n’a été pratiqué que chez 12 dont cinq ont été séropositifs pour le VIH. Un patient seulement a été référé en vue d’un traitement antirétroviral. Il y a eu 41 décès (29%) dont huit étaient atteints d’une TB probable et n’avaient pas été traités. Chez les 33 décédés restants, neuf seulement avaient eu un examen des frottis de crachats (27%) et quatre (12%) un CXR.
Conclusion:
Cette étude révèle des erreurs dans la prise en charge diagnostique des suspects de TBP dans les salles de l’Hôpital Central de Zomba, mais suggère aussi des occasions d’amélioration.
Abstract
Marco de referencia:
El hospital central de Zomba, en Malawi.
Objetivo:
Determinar la calidad del diagnóstico, el tratamiento y el desenlace clínico de los pacientes que se hospitalizan con presunción clínica de tuberculosis pulmonar (TBP) en los servicios de adultos.
Método:
Se llevó a cabo un estudio transversal retrospectivo de las historias clínicas de los pacientes hospitalizados entre julio y septiembre del 2010.
Resultados:
Se observaron 141 casos con presunción de TBP. La baciloscopia del esputo se solicitó y se obtuvo en 67 casos (48%), pero en ningún caso el resultado fue positivo. La radiografía de tórax (CXR) se solicitó y se obtuvo en 26 de los casos presuntos de TB (39%) que presentaron resultados negativos en la baciloscopia. En 11 de los pacientes se observaron CXR indicativas de TBP: se inició el tratamiento antituberculoso en dos pacientes y ocho fallecieron antes de haberlo comenzado. En el momento de la hospitalización, se conocía la situación con respecto al virus de la inmunodeficiencia humana (VIH) en 50 pacientes (35% de todos los casos con presunción de TB) y todos tenían una serología positiva. Se solicitó la prueba diagnóstica del VIH a 37 pacientes, pero solo se obtuvo en 12 casos y cinco de ellos tuvieron un resultado positivo. Solo se remitió un paciente para tratamiento antirretrovírico. Hubo en el grupo estudiado 41 defunciones (29%) y en ocho casos fue probable el diagnóstico de TB, pero no recibieron tratamiento. De los 33 pacientes restantes que fallecieron, solo nueve (27%) tuvieron un examen microscópico del esputo y cuatro (12%) una CXR.
Conclusión:
El presente estudio revela las deficiencias en el diagnóstico y el tratamiento de las personas con presunción diagnóstica de TB en los servicios del hospital central de Zomba y al mismo tiempo señala las oportunidades que existen de mejorar la atención de salud.
Tuberculosis (TB) remains a major global public health problem, with more cases estimated today than at any other time in history.1 Malawi is one of the countries in Central Southern Africa most severely affected by the human immunodeficiency virus (HIV) epidemic, and has consequently experienced a huge increase in TB cases in the last 10–20 years.1 It is estimated that 70% or more of TB patients in the country are co-infected with HIV, which is responsible not only for increasing TB case notifications but also for adversely affecting TB treatment outcomes.2
In Malawi, TB cases are detected through passive case finding. Patients with a cough of ≥2 weeks are identified as pulmonary tuberculosis (PTB) suspects, and are supposed to submit sputum specimens to health facility laboratories for smear examination of acid-fast bacilli (AFB).3 Patients with AFB-negative sputum smears should be managed by an algorithm that includes antibiotic treatment and chest radiography (CXR) to determine whether or not the patients have smear-negative PTB. The algorithm also includes HIV testing, as many PTB suspects are also likely to have HIV infection and would benefit from antiretroviral therapy (ART).
Information about the management and outcomes of PTB suspects is limited. A recent study in Guinea Bissau found that only 25% of PTB suspects were diagnosed with PTB. Of the remaining suspects with no TB diagnosis, 4% died within a month of investigation, over 40% remained symptomatic, some of whom were subsequently found to have PTB on further investigation, and 39% were found to be HIV-positive.4 Similar findings were reported from Zimbabwe, where 18% of patients diagnosed as smear-negative after sputum smear examination were subsequently diagnosed with pulmonary TB through CXR and 63% were HIV-infected.5
In Malawi, there is a similar lack of information. Many PTB suspects are admitted to hospital wards where the process of confirming or ruling out the TB diagnosis is carried out. Two studies in the late 1990s in Malawi looked at this issue in the hospital setting. One study in five district and mission hospitals found that 37% of TB suspects were diagnosed with TB, 38% were given another diagnosis, and of the remainder nearly 20% died before a diagnosis was made.6 Another study in Lilongwe Central Hospital (LCH), a district and tertiary health care facility, found that 25% of TB suspects had a diagnosis of TB, 30% had another diagnosis, the most common being pneumonia, and 45% had no documented diagnosis in the case note files. Among those not diagnosed with TB, 64% died, 24% with an alternative diagnosis and 76% with no diagnosis made.7
Zomba Central Hospital is one of the tertiary hospitals and a referral centre for primary and secondary health institutions in Malawi. The hospital also serves as a primary contact and, since the advent of the HIV epidemic, it has been managing a large number of PTB suspects, although the management of these patients has never previously been evaluated. This is an important issue, as HIV testing is now widely available in the country and a package of HIV care and treatment, including ART, is potentially available for the HIV-infected.
The aim of the current study was to determine the diagnostic management and outcomes of adult patients with cough for >2 weeks who were admitted to the general wards of the Central Hospital in Zomba, Malawi. Specific objectives were to determine 1) the number and proportion of PTB suspects admitted to hospital wards, 2) the proportion who had sputum smear and CXR examinations and their results, 3) the proportion who were diagnosed and treated appropriately, 4) the proportion who were tested for HIV, their results and any HIV treatment package offered, and 5) the final hospital diagnosis and hospital-based outcome.
METHODS
Design and setting
This was a retrospective, cross-sectional review of in-patient medical records conducted at the Zomba Central Hospital located in the southern region of Malawi, one of four tertiary hospitals in the country. This is a referral hospital catering for a population of 2.6 million living in the five districts of the south-east zone of Malawi. Of patients admitted to hospital medical wards in Malawi, between 10% and 20% may be suspected of having TB, especially PTB.6–8 According to the national guidelines,3 PTB suspects should first submit sputum specimens for smear examination for AFB, and those found to be sputum smear-positive are diagnosed as smear-positive PTB. Those with negative sputum smears should be referred for a CXR; patients with an abnormal CXR suggestive of TB who do not respond to antibiotics are diagnosed as smear-negative PTB by the medical or clinical officer. Once diagnosed with TB, the patients should immediately be referred to the district TB officer in the hospital for registration and start of anti-tuberculosis treatment.3
Participants
The study population included all adult patients (aged ≥15 years) admitted to medical, surgical, maternity and gynaecology wards for whom ‘chronic cough’ or cough >2 weeks was recorded in their medical files over a 3-month period from 1 July to 30 September 2010. These patients were designated PTB suspects.
Variables and data management
Descriptive variables that were collected from medical files included medical file number, patient name, age, sex and date of admission. Diagnostic variables included dates of ordering and collecting sputum specimens for smear examination, dates and results of sputum smear examination, dates and results of CXR examination, dates and results of TB diagnosis, patient TB category and dates and results of HIV testing (tested or not tested).
Treatment variables included TB treatment regimen, referral for ART for those found to be HIV-positive, final hospital diagnosis and hospital outcome, i.e., died, absconded with or without a diagnosis and discharged from the ward (either to home or to the TB ward).
Data for the study were extracted by the principal investigator from the in-patient case notes, the sputum laboratory register and the TB register. All data were collected into a structured pro-forma.
Analysis and statistics
Data were double entered into and validated in EpiData (EpiData Association, Odense, Denmark) and analysed using Stata/SE 10 (Stata Corp, College Station, TX, USA). Descriptive statistics were used to summarise the data.
Ethics
The study was approved by the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease and the National Health Sciences Research Committee (NHSRC) in Malawi. Permission and a letter of support were also obtained from the hospital director of Zomba Central Hospital.
RESULTS
Patient journey from admission to diagnosis of TB
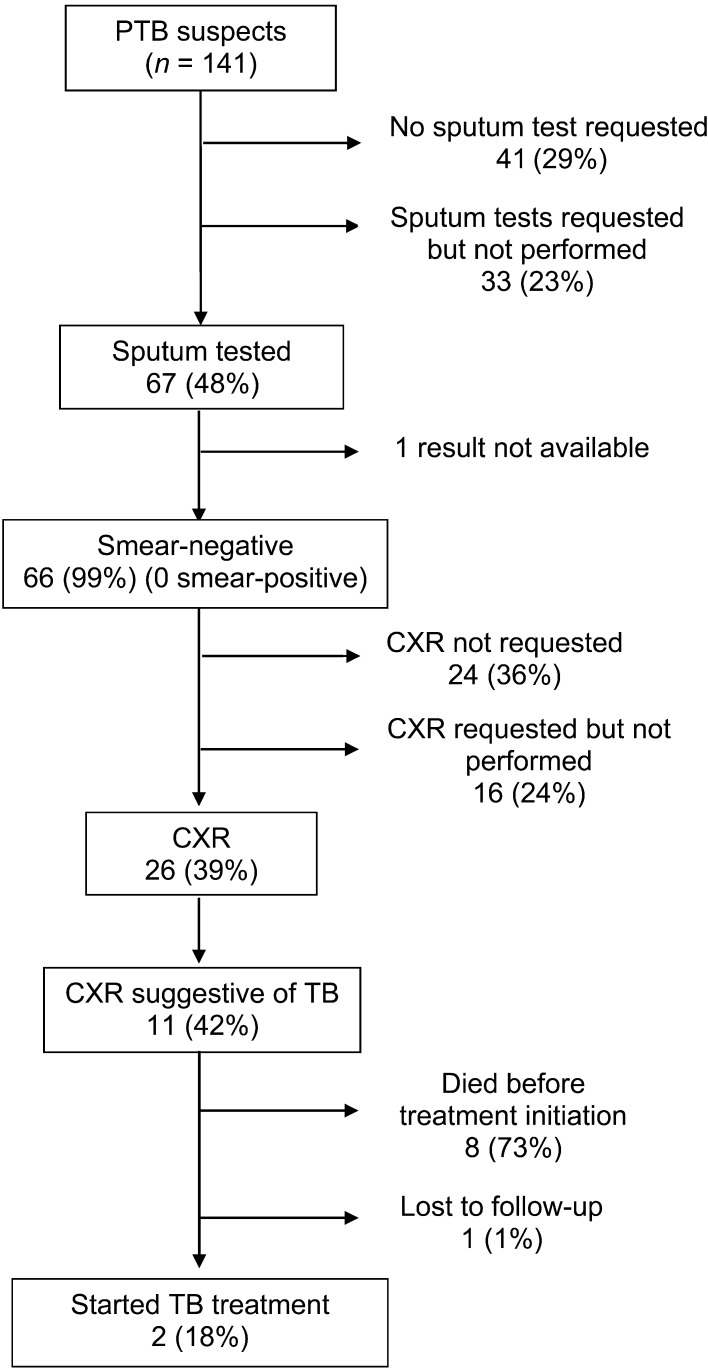
A summary of the patients’ journey from admission to a hospital diagnosis of TB is shown in the Figure. A total of 4423 records were reviewed from five wards; the distribution of PTB suspects according to the different wards is shown in Table 1. In all, there were 141 PTB suspects, of whom the majority were identified in the medical wards.
FIGURE.
Summary of results for sputum smear examination, chest X-ray and treatment at Zomba Central Hospital, Malawi. PTB = pulmonary tuberculosis; CXR = chest X-ray; TB = tuberculosis.
TABLE 1.
Number and proportion of admissions and pulmonary tuberculosis suspects identified in different wards, Zomba Central Hospital, Malawi, July–September 2010
| Ward | Admissions n | Suspects n (%) |
| Male medical | 1180 | 52 (4.4) |
| Female medical | 1693 | 76 (4.5) |
| Male surgical | 467 | 1 (0.2) |
| Female surgical | 532 | 6 (1.1) |
| Maternity and gynaecology | 551 | 6 (1.1) |
| Total | 4423 | 141 |
Sputum examination, chest X-rays and treatment
The results are shown in the Figure. Sputum examination was carried out for about half of the suspects. All sputum smears were AFB-negative (one result was not available). The median time between date of admission and date of sputum collection was 3 days (interquartile range [IQR] 5), and between sputum collection and sputum examination it was 1 day (IQR 1).
CXRs were carried out for 26 (39%) patients with negative sputum smears, 11 of whom had a CXR suggestive of PTB. Two of these patients were started on anti-tuberculosis treatment, and in both patients the correct regimen and correct dose of medication were given. The time between diagnosis and starting treatment was 10 days in one patient and was not known for the other patient.
HIV testing
HIV status was known for 50 patients (35% of all suspects) on admission, all of whom were known to be HIV-positive. HIV testing was requested in 37 patients, but was only carried out in 12, 5 of whom were positive. Only one patient was referred for ART. The median time between admission and HIV testing was 4 days (IQR 9).
Final diagnosis
A diagnosis of PTB was recorded for 11 (8%) of the 141 PTB suspects. Pneumonia with or without other conditions was recorded for 63 (45%) patients, followed by congestive cardiac failure (11%), malaria (6%), sepsis (4%), with a wide variety of other conditions being diagnosed in the remainder (32%).
Hospital outcomes
Table 2 shows the hospital outcomes of the 141 PTB suspects, including 41 (29%) deaths, with eight (6%) attributed to TB as a result of an abnormal and suggestive CXR. None of the eight patients had been started on anti-tuberculosis treatment; the reason for not being put on treatment indicated in three of the case files was ‘waiting for sputum results’. Thirty-three patients died with another diagnosis; of these only nine (27%) had sputum smears examined and four (12%) had a CXR.
TABLE 2.
Hospital-based outcome of pulmonary tuberculosis suspects at Zomba Central Hospital, Malawi
| Outcome | All suspects (n = 141) n (%) |
| TB diagnosed, treatment started* | 2 |
| Discharged | 92 (65) |
| Died | 41 |
| TB diagnosed | 8 |
| Other diagnosis | 33 (23) |
| Lost to follow-up | 5 |
1 patient diagnosed with TB was lost to follow-up.
DISCUSSION
This study showed that in Zomba Central Hospital, a tertiary referral centre in Malawi, the diagnostic management of patients with suspected PTB was poor, with most patients not undergoing timely or appropriate sputum smear examinations and CXRs, and consequently few patients being diagnosed with active PTB. HIV prevalence in this group of patients who had been HIV tested either before or after admission to the ward was high, and this may have been responsible for the high in-patient mortality.
Most of the patients suspected of PTB were correctly admitted to the medical wards, and this is where attention has to be paid to improve TB and HIV diagnostic practices. Sputum smears were either not requested or not collected from over half of the patients, and this finding is similar to those of previous studies conducted several years previously.6,7,9 Although attention was drawn to this deficiency in practice and recommendations were made for improvement several years ago, little progress appears to have been made. It is also surprising that no patients were found with smear-positive disease. This may be due either to patients with active TB being very immunosuppressed as a result of co-infection with HIV and therefore producing paucibacillary sputum, or to problems with laboratory investigation.10
Current guidelines recommend that CXR be carried out in smear-negative PTB suspects. Less than 40% of patients had a CXR ordered and performed, similar again to previous findings.6,7,9 In some patients, CXRs were never ordered, but in those where they were requested and not performed, one can only speculate on the reasons. These may include patients being too ill to go to the radiography department or not escorted by the hospital attendant, problems with the X-ray machine, X-ray films being out of stock or radiography technicians being away.
Approximately 40% of patients who had CXRs performed had abnormal findings suggestive of active TB, but only two patients were started on treatment, with most of the remainder dying in hospital without treatment initiation. We do not know the reasons for this, but it is possible that lives could have been saved with more timely initiation of anti-tuberculosis treatment.
While the Malawi government is committed to a joint national TB-HIV policy of scaling up HIV testing among TB patients, the study showed that few PTB suspects who did not know their HIV status at the time of admission were counselled and HIV tested. This is a huge missed opportunity. It has been suggested that in high TB-HIV burden settings such as Malawi, provider-initiated HIV testing and counselling (PITC) should be moved upstream and provided for PTB suspects as well as for patients with active and proven disease.11 A positive HIV test result will be an indication for cotrimoxazole preventive therapy, HIV care and consideration for ART. HIV infection in a PTB suspect with symptoms of cough, fever and weight loss should prompt careful clinical assessment and, if feasible, CD4-lymphocyte count measurements to determine eligibility for ART. Many of these HIV-positive PTB suspects with smear-negative sputum specimens are probably eligible for ART, and if this is so, ART can be started and will begin to reverse immune deficiency and perhaps reduce the high mortality in this group.
This was a study conducted at a central hospital and it is therefore representative of practices at other referral hospitals in the country. The study was operational in nature, with data being collected retrospectively from case files. It is possible that results were not properly recorded in these files, and we cannot therefore be sure of the completeness and accuracy of the data. Nevertheless, the study is an eye opener to the deficiencies at all stages, from TB diagnosis to start of treatment, at a central hospital. Delays in diagnosis and treatment not only threaten the lives of individual patients but also contribute to nosocomial TB transmission, which in previous studies has been found to be particularly high in the setting of a medical ward.12,13
What are the solutions? Clinicians need to improve on their performance of diagnosing and managing TB suspects, and the results of this current study should be shared with clinicians and nurses in the hospital to try and effect this change. A TB committee could be developed at the hospital with a view to conducting regular monitoring of the management of TB suspects in the wards. The hospital could also benefit from regular monthly death audits to see whether the deaths that have occurred were preventable. The capacity of health care workers needs to be strengthened by organising refresher training on TB diagnosis, treatment and control to foster better management of TB suspects in the hospital. Finally, there needs to be an assessment about whether new, improved diagnostic strategies could make a difference to more rapid and improved TB diagnosis, such as optimised smear microscopy, light-emitting diode (LED) fluorescent microscopy14 or the automated Xpert MTB/RIF assay (Cepheid, Sunnyvale, CA, USA), which can provide a TB diagnosis from untreated sputum in <2 h.15 These new tools need to be assessed for feasibility and effectiveness within the hospital setting, and further operational research is urgently needed in this area if lives are to be saved.
CONCLUSION
This study in a central referral hospital in Malawi has identified significant deficiencies in the diagnostic management of PTB suspects, but suggests that opportunities exist for improving diagnosis and care.
Acknowledgments
This research was supported through an operational research course, which was jointly developed and run by the Centre for Operational Research, International Union Against Tuberculosis and Lung Disease, France, and the Operational Research Unit, Médecins Sans Frontières, Brussels.
Many thanks are due to Dignitas International and the Zomba Central Hospital for the opportunity given to LGG to attend the course. Thanks again to hospital staff (in the wards and laboratory) for allowing the authors to review patient records.
References
- 1.World Health Organization. Global tuberculosis control 2009. Epidemiology, strategy, financing. WHO/HTM/TB/2009.411. Geneva, Switzerland: WHO; 2009. http://www.who.int/tb/publications/global_report/2009/en/index.html Accessed August 2011. [Google Scholar]
- 2.Harries A D, Zachariah R, Corbett E L, et al. The HIV-associated tuberculosis epidemic—when will we act? Lancet. 2010;375:1906–1919. doi: 10.1016/S0140-6736(10)60409-6. [DOI] [PubMed] [Google Scholar]
- 3.Ministry of Health and Population, Malawi. Manual of the National Tuberculosis Control Programme of Malawi. 6th ed. Lilongwe, Malawi: Ministry of Health and Population; 2008. [Google Scholar]
- 4.Porskrog A, Bjerregaard-Andersen M, Oliveira I, et al. Enhanced tuberculosis identification through one month follow-up of smear-negative tuberculosis suspects. Int J Tuberc Lung Dis. 2011;15:459–464. doi: 10.5588/ijtld.10.0353. [DOI] [PubMed] [Google Scholar]
- 5.Dimairo M, MacPherson P, Bandason T, et al. The risk and timing of tuberculosis diagnosed in smear-negative TB suspects: a 12-month cohort study in Harare, Zimbabwe. PLoS One. 2010;5:e11849. doi: 10.1371/journal.pone.0011849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harries A D, Kemp J R, Salaniponi F M L. Developing operational research capacity in hospital tuberculosis control officers in Malawi. Int J Tuberc Lung Dis. 2003;7:266–270. [PubMed] [Google Scholar]
- 7.Friend J H, Mason S, Harries A D, Salaniponi F M, Neuhann F. Management and outcome of TB suspects admitted to the medical wards of a central hospital in Malawi. Trop Doctor. 2005;35:93–95. doi: 10.1258/0049475054037165. [DOI] [PubMed] [Google Scholar]
- 8.Weismuller M M, Meijnen S, Claessens N J M, Salaniponi F M, Harries A D. AIDS and tuberculosis in medical inpatients in Malawi. Trop Doctor. 2003;33:167–168. doi: 10.1177/004947550303300317. [DOI] [PubMed] [Google Scholar]
- 9.Clive S. Sputum smear examination on a medical ward. Malawi Med J. 1992;9:17–18. [Google Scholar]
- 10.Hargreaves N J, Kadzakumanja O, Phiri S, et al. What causes smear-negative pulmonary tuberculosis in Malawi, an area of high HIV seroprevalence? Int J Tuberc Lung Dis. 2001;5:113–122. [PubMed] [Google Scholar]
- 11.Harries A D. Paying attention to tuberculosis suspects whose sputum smears are negative. Int J Tuberc Lung Dis. 2011;15:427–428. doi: 10.5588/ijtld.11.0051. [DOI] [PubMed] [Google Scholar]
- 12.Harries A D, Kamenya A, Namarika D, et al. Delays in diagnosis and treatment of smear-positive tuberculosis and the incidence of tuberculosis in hospital nurses in Blantyre, Malawi. Trans Roy Soc Trop Med Hyg. 1997;91:15–17. doi: 10.1016/s0035-9203(97)90376-x. [DOI] [PubMed] [Google Scholar]
- 13.Harries A D, Nyirenda T E, Banerjee A, Boeree M J, Salaniponi F M. Tuberculosis in health care workers in Malawi. Trans Roy Soc Trop Med Hyg. 1999;93:32–35. doi: 10.1016/s0035-9203(99)90170-0. [DOI] [PubMed] [Google Scholar]
- 14.Van Kampen S, Ramsay A R, Anthony R M, Klatser P R. Retooling national TB control programmes (NTPs) with new diagnostics: the NTP perspective. PLoS One. 2010;5:e11649. doi: 10.1371/journal.pone.0011649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boehme C C, Nabeta P, Hillemann D, et al. Rapid molecular detection of tuberculosis and rifampin resistance. N Eng J Med. 2010;363:1005–1015. doi: 10.1056/NEJMoa0907847. [DOI] [PMC free article] [PubMed] [Google Scholar]