Abstract
Osteoporosis is a major health problem affecting one in three women over the age of 50 and may not be detected until fractures occur. Since osteoporotic fractures are a health burden worldwide, identifying subjects with a high risk of osteoporosis and preventing osteoporosis-related mortality and morbidity are a very important health strategy. Women show an estrogen-related bone loss starting at menopause, predominantly occurring in trabecular bone. Diagnosis of osteoporosis is usually based on the bone mineral density measurement, but this is not a practical and economical technique for early detection. Therefore, investigators are interested in the possibility of detecting osteoporosis from the panoramic radiographs. Mandibular cortical bone undergoes resorptive activity in osteoporotic patients, leading to a decreased thickness and more porous inferior border. Therefore, studies have demonstrated the usefulness of cortical width and shape, determined from panoramic radiographs, in identifying elderly individuals with undetected osteoporosis, especially postmenopausal women. In conclusion, postmenopausal women with C3 category, Mental Index (MI) <3 mm, and panoramic mandibular index (PMI) <0.3 may be considered for further osteoporosis investigation.
Keywords: Mandibular indices, osteoporosis, panoramic-based indices, panoramic radiography, postmenopausal women, women
INTRODUCTION
Osteoporosis is a common metabolic bone disease characterized by low bone mass, microarchitectural weakening leading to bone fragility, and increased fracture risk.[1] Osteoporosis affects one in three women and one in five men over the age of 50 and may not be detected until symptoms or fractures occur.[2,3,4] White women over the age of 50 have a 50% chance of fracturing in their lifetime and these fractures result in increased morbidity and mortality risks. Approximately 40% of the patients with osteoporotic hip fractures die within 5 years after their fractures occur.[1,5] Osteoporosis is a preventable and treatable disease; but because of no signs present prior to a fracture, many people are not being diagnosed in time to receive effective therapy.[2] The National Osteoporosis Foundation has identified many risk and predisposing factors for osteoporosis and related fractures in postmenopausal women. Some of the important factors are: History of fractures in adulthood, smoking, estrogen deficiency at an early age, low body weight, poor health, low calcium intake, physical inactivity, little exposure to sunlight, alcohol abuse, and use of oral glucocorticoid therapy for more than 3 months.[2,6]
Osteoporosis predominantly affects elderly women.[4] While bone loss starts at about 35 years of age, the rate of bone loss increases after menopause in women.[7,8] Women show an estrogen-related bone loss starting at menopause, predominantly in trabecular bone, followed by a slower loss of both trabecular and cortical bones 4–8 years later. After this period, the rate of bone loss declines at a more gradual rate.[7,9,10,11,12] In women, changes related to age generally consist of disconnections of the trabecular network; but in men, thinning of the trabeculae is seen.[9]
Since osteoporotic fractures are a health burden worldwide, resulting in reduced physical activity, increased risk of mortality, and increased medical costs, health promotion strategies focus on identifying subjects at a high risk of the disease. Before a fracture occurs, osteoporosis is characterized by decreased bone mineral density (BMD) in the preclinical stage. BMD testing using dual-energy X-ray absorptiometry (DXA) is a vital component in the diagnosis and management of osteoporosis. According to the World Health Organization (WHO) criteria, BMD values are divided into the following diagnostic guidelines: Normal (T-score >−1.0), osteopenia (T-score between −1.0 and − 2.5), and osteoporosis (T-score <−2.5).[2,6,13,14]
FRAX® was also developed to calculate the 10-year probability of a major osteoporotic fracture taking into account femoral neck BMD and the clinical risk factors. FRAX is intended for postmenopausal women and men aged 50 and older; it is not intended for use in younger adults. Studies concluded that it is most useful in patients with low femoral neck BMD.[1,2]
Osteoporosis affects an enormous number of people, of both sexes and all races, and its prevalence increases as the population ages.[2] Since DXA is the gold standard for the diagnosis of osteoporosis worldwide, BMD testing for the entire elderly population by DXA may be an useful option for early detection of the disease.[14] However, this is not a practical method. Therefore, investigators are interested in the possibility of detecting osteoporosis from the dental radiographs, especially panoramic images.
Osteoporosis and panoramic-based indices
Panoramic radiography is used for the early detection of osteoporosis due to its low cost and the large numbers of osteoporotic patients attending the dental clinics as a result of higher life expectancies. It would be economical and beneficial if the radiographs could be used for triaging individuals with undetected osteoporosis.[14] Another advantage of using these radiographs is that these are often taken repeatedly, with similar projection and exposure parameters, making them very suitable for comparison.[13,14]
It is well known that the mandibular cortical bone undergoes resorptive activity in osteoporotic patients, leading to a decreased thickness and more porous inferior border, characteristics that can be determined by panoramic radiographs.[10,11,14,15,16] Dutra et al.[4] also showed that a reduced skeletal BMD can alter the mandibular shape. Studies focusing on identifying the elderly individuals with osteoporosis, especially postmenopausal women, have demonstrated the usefulness of mandibular cortical indices from panoramic radiographs. Three indices were reported by most of the studies: Mandibular cortical shape [Mandibular Cortical Index (MCI) or Klemetti index (KI)] and width [Mental Index (MI)], and panoramic mandibular index (PMI).
MCI or KI refers to the appearance of the inferior cortex of the mandible and is classified as follows: C1: the endosteal margin of the cortex is even and sharp on both sides [Figure 1]; C2: The endosteal margin presents semilunar defects (lacunar resorption) and/or appears to form endosteal cortical residues on one or both sides [Figure 2]; and C3: The cortical layer forms heavy endosteal cortical residues and is clearly porous [Figure 3].[17] Some studies have reported that women with a mild to moderate and severe eroded cortex are considered to have an increased likelihood of osteoporosis.[1,11,18,19,20] However, others indicated no usefulness of the MCI.[8,21,22] A recent study showed that approximately 95% of Japanese women identified by trained dentists using cortical shape findings did have osteopenia or osteoporosis.[14] As a result, studies concluded that the sensitivity of MCI in the diagnosis of osteoporosis (T-score <−2.5) varied from 35.9 to 90.9%.[1,6,8,18,19,21,23,24,25,26] The differences among the results is considered to be due to the heterogeneity of the studies.[23]
Figure 1.

C1 category of MCI
Figure 2.

C2 category of MCI
Figure 3.

C3 category of MCI
MI or mandibular cortical width (MCW): Measurement of the cortical width at the mental foramen region is done according to the technique previously described [Figure 4].[27,28] The mental foramen is identified and a line is traced that passes perpendicular to the tangent of the lower border of the mandible and through the center of the mental foramen. The cortical width is measured at this point. The correlation between MI and skeletal BMD increases in the postmenopausal period owing to the rapid decrease in both MI and skeletal BMD after menopause.[29] In fact, studies showed a rapid decline in MI after the age of 50, which is the mean age of menopause worldwide.[30,31] Roberts et al.[29] revealed that cortical thinning normally starts in women at age 42.5 years and accelerates thereafter. In another study, it was found that the MI increased rapidly between 10 and 20 years and decreased rapidly between 50 and 60 years in females only.[31] The MI increases rapidly in the second decade in women, while it increases gradually from the second to third decade in men.[30] The maturation of the entire skeleton in young women, including jawbones, is influenced by several factors, such as the age of menarche, menstruation cycle, nutritional intake, and physical activity.[30] Since occlusal function due to the permanent teeth is established during the second decade, this might affect the formation of the cortical bone of the mandible locally and individually.
Figure 4.
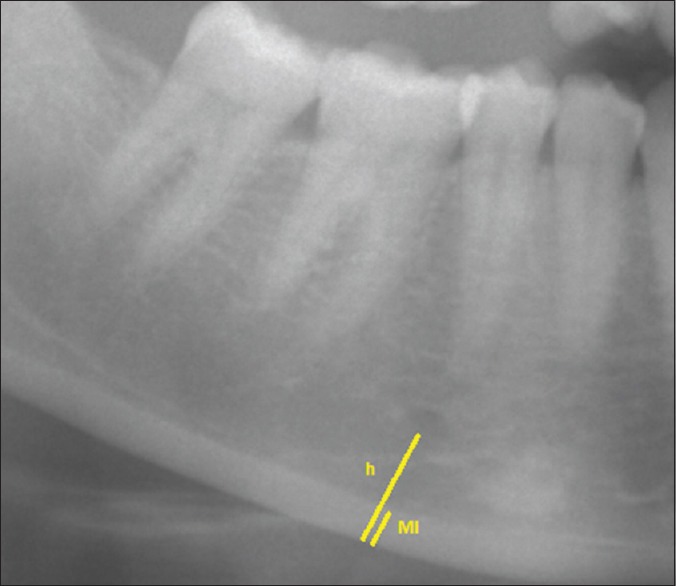
MI and PMI (MI/h)
The threshold values to find the highest sensitivity/specificity ranged from 2.69 to 5 mm.[8,20,29,30,31,32,33,34,35,36] While a few studies reported high sensitivity (>95%),[33,34,35] others did not find a sensitivity of even 20%.[32,36] Horner et al.[32] recommended that women having an MI below the mental foramen of less than 3 mm should be referred for investigation of osteoporosis. However, in another study which used a more lateral measurement site than mental foramen on the mandible, the threshold value was 2.75 mm.[29] Considering the results of the studies, asymptomatic dental patients with an MI of less than about 3 mm may be candidates for DXA testing.[19,20,33]
PMI is the ratio between the cortical width at the mental foramen region and the distance from the lower border to the inferior edge of the mental foramen (MI/h) [Figure 4].[37] A few studies investigated the accuracy of PMI in detecting reduced BMD. These studies considered the threshold value of 0.3 and the estimated sensitivity and specificity was higher than 70%.[8,20,38]
Linear measurements on the panoramic radiographs have limitations because of unequal magnification and geometric distortion arising from exposure parameters or settings between different panoramic machines.[23] Therefore, studies on standardized panoramic radiographs would be more reliable in detecting osteoporosis. However, this is not a practical method in clinical situation.
Different studies revealed different intraobserver or interobserver agreement to detect osteoporosis using these panoramic indices.[11,12,20,21,28,29,30,31,32,33,34,35,36,38] As none of these indices showed perfect intraoberserver or interobserver agreement, it has been suggested to assess all of these indices.
Menopause is the major factor contributing to the rapid decrease in the BMD of the skeleton including the jaws in the elderly women. In the mandible, local factors such as the number of teeth and mastication influence the bone to some degree.
CONCLUSION
In conclusion, all three mandibular cortical indices (MCI, MI, and PMI) discussed in this review are useful tools to detect low BMD. Their limitations are mainly related to the panoramic radiographs or agreement between different observers. Postmenopausal women with C3 category, MI <3 mm, and PMI <0.3 may be considered for further osteoporosis investigation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Yamada S, Uchida K, Iwamoto Y, Sugino N, Yoshinari N, Kagami H, et al. Panoramic radiography measurements, osteoporosis diagnoses and fractures in Japanese men and women. Oral Dis. 2015;21:335–41. doi: 10.1111/odi.12282. [DOI] [PubMed] [Google Scholar]
- 2.Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, et al. Clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25:2359–81. doi: 10.1007/s00198-014-2794-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dutra V, Yang J, Devlin H, Susin C. Radiomorphometric indices and their relation to gender, age, and dental status. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:479–84. doi: 10.1016/j.tripleo.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 4.Dutra V, Devlin H, Susin C, Yang J, Horner K, Fernandes AR. Mandibular morphological changes in low bone mass edentulous females: Evaluation of panoramic radiographs. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:663–8. doi: 10.1016/j.tripleo.2006.02.023. [DOI] [PubMed] [Google Scholar]
- 5.Lee YK, Lee YJ, Ha YC, Koo KH. Five-year relative survival of patients with osteoporotic hip fracture. J Clin Endocrinol Metab. 2014;99:97–100. doi: 10.1210/jc.2013-2352. [DOI] [PubMed] [Google Scholar]
- 6.Gaur B, Chaudhary A, Wanjari PV, Sunil MK, Basavaraj P. Evaluation of panoramic radiographs as a screening tool of osteoporosis in post menopausal women: A cross sectional study. J Clin Diagn Res. 2013;7:2051–5. doi: 10.7860/JCDR/2013/5853.3403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Horner K, Devlin H. The relationship between mandibular bone mineral density and panoramic radiographic measurements. J Dent. 1998;26:337–43. doi: 10.1016/s0300-5712(97)00020-1. [DOI] [PubMed] [Google Scholar]
- 8.Drozdzowska B, Pluskiewicz W, Tarnawska B. Panoramic-based mandibular indices in relation to mandibular bone mineral density and skeletal status assessed by dual energy X-ray absorptiometry and quantitative ultrasound. Dentomaxillofac Radiol. 2002;31:361–7. doi: 10.1038/sj.dmfr.4600729. [DOI] [PubMed] [Google Scholar]
- 9.Hassasni-Nejad A, Ahlqwist M, Hakeberg M, Jonasson G. Mandibular trabecular bone as fracture indicator in 80-year-old men and women. Eur J Oral Sci. 2013;121:525–31. doi: 10.1111/eos.12087. [DOI] [PubMed] [Google Scholar]
- 10.Gomes CC, de Rezende Barbosa GL, Bello RP, Bóscolo FN, de Almeida SM. A comparison of the mandibular index on panoramic and cross-sectional images from CBCT exams from osteoporosis risk group. Osteoporos Int. 2014;25:1885–90. doi: 10.1007/s00198-014-2696-3. [DOI] [PubMed] [Google Scholar]
- 11.Halling A, Persson GR, Berglund J, Johansson O, Renvert S. Comparison between the Klemetti index and heel DXA BMD measurements in the diagnosis of reduced skeletal bone mineral density in the elderly. Osteoporos Int. 2005;16:999–1003. doi: 10.1007/s00198-004-1796-x. [DOI] [PubMed] [Google Scholar]
- 12.Koh KJ, Kim KA. Utility of the computed tomography indices on cone beam computed tomography images in the diagnosis of osteoporosis in women. Imaging Sci Dent. 2011;41:101–6. doi: 10.5624/isd.2011.41.3.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mulligan R, Sobel S. Osteoporosis: Diagnostic testing, ınterpretation, and correlations with oral health-ımplications for dentistry. Dent Clin North Am. 2005;49:463–84. doi: 10.1016/j.cden.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 14.Taguchi A. Triage screening for osteoporosis in dental clinics using panoramic radiographs. Oral Dis. 2010;16:316–27. doi: 10.1111/j.1601-0825.2009.01615.x. [DOI] [PubMed] [Google Scholar]
- 15.Lee BD, White SC. Age and trabecular features of alveolar bone associated with osteoporosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:92–8. doi: 10.1016/j.tripleo.2004.11.020. [DOI] [PubMed] [Google Scholar]
- 16.Zlatarić DK, Celebić A. Clinical bone densitometric evaluation of the mandible in removable denture wearers dependent on the morphology of the mandibular cortex. J Prosthet Dent. 2003;90:86–91. doi: 10.1016/s0022-3913(03)00171-9. [DOI] [PubMed] [Google Scholar]
- 17.Klemetti E, Kolmakov S, Kröger H. Pantomography in assessment of the osteoporosis risk group. Scand J Dent Res. 1994;102:68–72. doi: 10.1111/j.1600-0722.1994.tb01156.x. [DOI] [PubMed] [Google Scholar]
- 18.Taguchi A, Suei Y, Ohtsuka M, Otani K, Tanimoto K, Ohtaki M. Usefulness of panoramic radiography in the diagnosis of postmenopausal osteoporosis in women width and morphology of inferior cortex of the mandible. Dentomaxillofac Radiol. 1996;25:263–7. doi: 10.1259/dmfr.25.5.9161180. [DOI] [PubMed] [Google Scholar]
- 19.Taguchi A, Tsuda M, Ohtsuka M, Kodama I, Sanada M, Nakamoto T, et al. Use of dental panoramic radiographs in identifying younger postmenopausal women with osteoporosis. Osteoporos Int. 2006;17:387–94. doi: 10.1007/s00198-005-2029-7. [DOI] [PubMed] [Google Scholar]
- 20.Gulsahi A, Özden S, Cebeci AI, Kucuk NO, Paksoy CS, Genc Y. The relationship between panoramic radiomorphometric ındices and the femoral bone mineral density of edentulous patients. Oral Radiol. 2009;25:47–52. [Google Scholar]
- 21.Horner K, Karayianni K, Mitsea A, Berkas L, Mastoris M, Jacobs R, et al. The mandibular cortex on radiographs as a tool for osteoporosis risk assessment: The OSTEODENT Project. J Clin Densitom. 2007;10:138–46. doi: 10.1016/j.jocd.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 22.Cakur B, Dagistan S, Sahin A, Harorli A, Yilmaz A. Reliability of mandibular cortical index and mandibular bone mineral density in the detection of osteoporotic women. Dentomaxillofac Radiol. 2009;38:255–61. doi: 10.1259/dmfr/22559806. [DOI] [PubMed] [Google Scholar]
- 23.Calciolari E, Donos N, Park JC, Petrie A, Mardas N. Panoramic measures for oral bone mass in detecting osteoporosis: A systematic review and meta-analysis. J Dent Res. 2015;94(Suppl):17S–27. doi: 10.1177/0022034514554949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leite AF, Figueiredo PT, Guia CM, Melo NS, de Paula AP. Correlations between seven panoramic radiomorphometric indices and bone mineral density in postmenopausal women. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:449–56. doi: 10.1016/j.tripleo.2009.02.028. [DOI] [PubMed] [Google Scholar]
- 25.Al-Dam A, Blake F, Atac A, Amling M, Blessmann M, Assaf A, et al. Mandibular cortical shape index in non-standardised panoramic radiographs for identifying patients with osteoporosis as defined by the German Osteology Organization. J Craniomaxillofac Surg. 2013;41:e165–9. doi: 10.1016/j.jcms.2012.11.044. [DOI] [PubMed] [Google Scholar]
- 26.Ferreira Leite A, de Souza Figueiredo PT, Ramos Barra F, Santos de Melo N, de Paula AP. Relationships between mandibular cortical indexes, bone mineral density, and osteoporotic fractures in Brazilian men over 60 years old. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:648–56. doi: 10.1016/j.tripleo.2011.06.014. [DOI] [PubMed] [Google Scholar]
- 27.Taguchi A, Tanimoto K, Suei Y, Yamada T, Ohtsuka M, Sumida M. Diagnosis of postmenopausal osteoporosis by panoramic radiographs. J Jpn Soc Bone Morphom. 1994;4:113–8. [Google Scholar]
- 28.Ledgerton D, Horner K, Devlin H, Worthington H. Radiomorphometric indices of the mandible in a British female population. Dentomaxillofac Radiol. 1999;28:173–81. doi: 10.1038/sj/dmfr/4600435. [DOI] [PubMed] [Google Scholar]
- 29.Roberts M, Yuan J, Graham J, Jacobs R, Devlin H. Changes in mandibular cortical width measurements with age in men and women. Osteoporosis Int. 2011;22:1915–25. doi: 10.1007/s00198-010-1410-3. [DOI] [PubMed] [Google Scholar]
- 30.Taguchi A, Sugino N, Miki M, Kozai Y, Mochizuki N, Osanai H, et al. Detecting young Japanese adults with undetected low skeletal bone density using panoramic radiographs. Dentomaxillofac Radiol. 2011;40:154–9. doi: 10.1259/dmfr/30045588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Taguchi A, Tanimoto K, Suei Y, Wada T. Tooth loss and mandibular osteopenia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79:127–32. doi: 10.1016/s1079-2104(05)80088-5. [DOI] [PubMed] [Google Scholar]
- 32.Horner K, Devlin H, Harvey L. Detecting patients with low skeletal bone mass. J Dent. 2002;30:171–5. doi: 10.1016/s0300-5712(02)00010-6. [DOI] [PubMed] [Google Scholar]
- 33.Devlin H, Allen PD, Graham J, Jacobs R, Karayianni K, Lindh C, et al. Automated osteoporosis risk assessment by dentists: A new pathway to diagnosis. Bone. 2007;40:835–42. doi: 10.1016/j.bone.2006.10.024. [DOI] [PubMed] [Google Scholar]
- 34.Ezoddini Ardakani F, Owlia M, Hesami S, Hosseini P. Digital panoramic radiography as a useful tool for detection of bone loss: A comparative study. Acta Med Iran. 2013;51:94–100. [PubMed] [Google Scholar]
- 35.Muramatsu C, Matsumoto T, Hayashi T, Hara T, Katsumata A, Zhou X, et al. Automated measurement of mandibular cortical width on dental panoramic radiographs. Int J Comput Assist Radiol Surg. 2013;8:877–85. doi: 10.1007/s11548-012-0800-8. [DOI] [PubMed] [Google Scholar]
- 36.Mansour S, Alghamdi AS, Javed F, Marzouk H, Khan EA. Panoramic radiomorphometric indices as reliable parameters in predicting osteoporosis. Am J Med Sci. 2013;346:473–8. doi: 10.1097/MAJ.0b013e3182972148. [DOI] [PubMed] [Google Scholar]
- 37.Benson BW, Prihoda TJ, Glass BJ. Variations in adult cortical bone mass as measured by a panoramic mandibular index. Oral Surg Oral Med Oral Pathol. 1991;71:349–56. doi: 10.1016/0030-4220(91)90314-3. [DOI] [PubMed] [Google Scholar]
- 38.Marandi S, Bagherpour A, Imanimoghaddam M, Hatef M, Haghighi A. Panoramic-based mandibular indices and bone mineral density of femoral neck and lumbar vertebrae in women. J Dent (Tehran) 2010;7:98–106. [PMC free article] [PubMed] [Google Scholar]


