Abstract
The Veteran's Health Administration (VHA) has launched a large-scale initiative to promote prolonged exposure (PE) therapy, an evidence-based treatment for PTSD. While existing randomized controlled trials (RCTs) unambiguously support the efficacy of PE in civilian and some military populations, there is a need to better understand the course of treatment for combat Veterans of the current wars receiving PE in normative mental healthcare settings. The current study investigates 65 Veterans receiving care at an urban VA medical center. All Veterans were diagnosed with PTSD via a structured interview and treated with PE. Measures of PTSD and depression were collected pre- and post-treatment and every two sessions during treatment. Dependent means t-tests were used to estimate pre- and post-treatment d-type effect sizes. Additionally, hierarchical linear models (HLM) were used to investigate treatment effects over time, relationships between patient characteristics and outcomes, and to provide estimates of R2-type effect sizes. Results indicate that PE in regular VA mental healthcare contexts can be as effective as when implemented in carefully conducted RCTs.
1. Introduction
As of December 2009 over two million Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) U.S. troops have been deployed overseas (Defense Manpower Data Center, 2009). Of those who have returned, as many as 20% appear to be suffering from mental health difficulties, inclusive of combat-related posttraumatic stress disorder (PTSD; Hoge et al., 2006; Army Surgeon General's MHAT-V, 2008; Rand Center for Military Health Policy, 2008); and as many as half of those meeting criteria for PTSD or depression seek mental healthcare (Rand, 2008). Within the next decade, there will likely be hundreds of thousands of Veterans seeking psychiatric services within the Veteran's Health Administration (VHA). In anticipation of this potential influx, the VHA has increased efforts to address the trauma-related symptoms of its Veterans, including large scale initiatives to train VA clinicians in the use of empirically supported treatments for PTSD (VA, 2009).
Existing studies support efficacy of exposure therapy for civilians (Foa et al., 1999; 2005; Marks et al., 1998; Resick et al., 2002) and Veterans (Cooper & Clum, 1989; Keane et al., 1989; Schnurr et al., 2007) with PTSD. The most recent VA/Department of Defense (DoD) Clinical Practice Guidelines identified exposure therapy as one of four evidence-based psychotherapies for PTSD (VA/DoD; 2004), and the Institute of Medicine recognized exposure therapies as the only treatment approach with sufficient efficacy data for combat-related PTSD (IOM, 2007). In this regard, exposure therapy is broadly considered the frontline intervention for combat-related PTSD.
Despite the evidence base for efficacy of exposure-oriented therapies, it has been noted that such interventions are not routinely incorporated into VA clinical practice. In a survey of six large VA Medical Centers (VAMCs), Rosen and colleagues (2004) found that use of psycho-education and coping skills training were frequently reported by VA clinicians. However, few clinicians (i.e., less than 5%) reported routine use of exposure-based interventions for PTSD. These study findings are consistent with the broader dissemination literature that suggests many public-sector settings do not adequately or consistently use evidence based practices, particularly with regard to the treatment of PTSD (Drake et al., 2001; Frueh et al., 2009; 2001; Hanson et al., 2002).
In light of the anticipated influx of returning Veterans with PTSD and VHA's recent initiatives to incorporate the use of empirically supported treatments for PTSD into clinical practice, there is a need to better understand how OEF/OIF Veterans receiving services at VAMC's will respond to empirically validated treatment. Few recent PTSD treatment outcome studies within the VA have included meaningful numbers of OEF/OIF Veterans (Frueh et al., 2007; Rauch et al., 2009; Ready et al., 2008; Schnurr et al., 2007; Tuerk et al., 2010). Beyond questions about how OEF/OIF Veterans, in particular, will respond to evidence-based treatment, there is also a need to ensure that empirically supported treatments, such as exposure therapy, can be effectively implemented in VA healthcare settings by VA providers. Such data would serve to bridge the longstanding gap between research and practice and assist Veterans to receive the best possible care for their trauma-related mental health needs.
The current study presents clinical outcome data on 65 OEF/OIF Veterans treated with the manualized Prolonged Exposure (PE) intervention for PTSD (PE; Foa et al., 2007) by VA clinicians. These data are timely as, to the authors’ knowledge, there are no published studies on the efficacy or effectiveness of exposure therapy for combat-related PTSD using an exclusive sample of OEF/OIF Veterans. However, given recent dissemination efforts within VA healthcare settings, we anticipate a number of effectiveness studies in the near future. The results of the current investigation, and of those to come, can be used to inform a broad understanding of the relative effectiveness of PE for OEF/OIF-related PTSD as well as an understanding of how patient characteristics may interact with treatment outcomes.
2. Method
2.1 Study Overview
The current investigation is a post hoc effectiveness study using archival data from patients treated by a PTSD Clinical Team (PCT) in an urban VA Medical Center (VAMC). All Veterans were diagnosed with combat-related PTSD and treated with PE as part of their routine clinical care. Measures of PTSD and depression were collected pre- and post-treatment, as well as every two weeks during treatment. Veterans were not subject to protocol-driven exclusion criteria or given incentives to participate in treatment. This study was conducted with full approval from relevant Institutional Review Boards (IRBs).
2.2 Sample and Treatment Setting
The current sample consists of 65 OEF/OIF Veterans: 11% Female; 39% Black, 57% White; 5% Hispanic, mean age, 31.77 years (SD=8.19). Two outliers in the age distribution exerted disproportional influence on the mean age; the modal age of the sample was 27. Sixty-seven percent (67%) of the sample had a service-connected disability rating for PTSD or were in the process of applying for such disability compensation during treatment. Table one displays patient characteristics including military branch and the result of PTSD disability rating for those who applied. Patients were identified for treatment through referrals from primary care providers, general mental health providers, and case managers to the PCT. Patients were then formally assessed and a PTSD diagnosis via the Clinician Administered PTSD Scale (CAPS, Blake et al., 1995) was confirmed before assignment to treatment. Therapist assignment was based on provider availability in line with normative operating procedures of an outpatient psychotherapy clinic. The current sample represents all OEF/OIF patients with a combat-related trauma assigned to a PE provider between 8/3/07 and 10/28/09. All patients were treated by two clinical psychologists and one social worker (MSW) with specialized training in trauma work and in PE. Treatment sessions were not coded for treatment fidelity; however, therapists participated in weekly group supervision as part of routine clinical practice to guard against therapist drift in skills.
Table 1.
Sample demographics, characteristics, and baseline pathology
| n (%) | Age m (SD) | Baseline PCL-M m (SD) | Baseline BDI-II-II m (SD) | ||
|---|---|---|---|---|---|
| Gender: | Female | 7 (11%) | 29.6 (5.6) | 66.00 (5.35) | 31.00 (8.20) |
| Male | 58 (89%) | 32.0 (8.5) | 63.00 (9.13) | 28.94 (10.70) | |
| Race: | Black | 25 (39%) | 34.0 (8.4) | 65.84 (7.47) | 29.57 (10.42) |
| Hispanic | 3 (5%) | 29.3 (4.7) | 66.50 (9.19) | 40.50 (12.02) | |
| White | 37(57%) | 30.5 (8.1) | 61.42 (9.38) | 28.23 (10.30) | |
| Military Branch: | Air Force | 1 (2%) | |||
| Army | 43 (66%) | ||||
| Army National Guard | 5 (8%) | ||||
| Marines | 14 (22%) | ||||
| Navy | 2 (3%) | ||||
| Service Connection Disability Rating | None/Did not apply | 21 (32%) | |||
| 10% | 2 (3%) | ||||
| 30% | 23 (35%) | ||||
| 50% | 12 (19%) | ||||
| 70% | 4 (6%) | ||||
| 100% | 3 (5%) | ||||
| Total | 65 (100%) | 31.8 (8.2) | 63.33 (8.81) | 29.15 (10.44) | |
2.3 Intervention
Prolonged Exposure (PE; Foa et al., 2007) is a manualized, 90-minute, weekly, treatment protocol that consists of the following major components: (a) psycho-education regarding common reactions to trauma and a detailed rationale for treatment; (b) self assessment of anxiety using subjective units of distress (SUDs); (c) repeated in vivo exposure to situations avoided due to distress; and (d) repeated, prolonged imaginal exposure to traumatic memories followed by processing or discussion of the memories. In vivo exposure involves having the patient approach a hierarchy of feared, but safe, trauma-related situations as homework between sessions. Imaginal exposure involves assisting patients to repeatedly recount their traumatic event(s) in detail, while vividly imagining the event(s). Treatment sessions are audio-taped for patients to review between sessions for additional exposure. Because the current investigation is an effectiveness study of PE conducted with Veterans in the ecological context of a PCT clinic, the length of treatment varied by patient and was informed by ongoing psychometric assessment and collaborative evaluation of progress.
2.4 Measures
PTSD Checklist – Military Version (PCL-M; Weathers et al., 1991)
The PCL-M is a 17-item self-report measure of PTSD symptoms based on DSM-IV criteria. Scores on the PCL-M range from 17 to 85 with higher scores reflecting greater PTSD severity. The instrument has good diagnostic efficiency (> .70) and robust psychometric properties (Blanchard et al., 1996)
Beck Depression Inventory-II (BDI-II-II; Beck et al.,1996)
The BDI-II is a 21-item self-report measure that assesses behavioral and affective symptoms of depression. Scores on the BDI-II range from 0 to 63 with higher scores reflecting greater depression severity. The BDI-II demonstrates adequate convergent validity, discriminant validity, test-retest reliability (r = .93), and good internal consistency (α < .92; Beck et al., 1996; Steer & Clark, 1997).
2.5 Statistical Analyses
Repeated measures, dependent means t-tests were used to compare pre-post treatment effects on the PCL-M and BDI-II for the entire intent-to-treat (ITT) sample and for the treatment completers sub-sample. Statistically significant differences were qualified using d-type effect sizes. In the current study, a treatment completer was defined as any patient who completed at least six sessions of PE. The six session benchmark was selected based on prior clinical experience with OEF/OIF patients, many of whom respond to treatment rapidly after the onset of exposure, and thus, do not remain in treatment after they experience significant symptom amelioration. In addition to analyzing pre-post differences with t-tests, hierarchical linear modeling (HLM) was used to analyze the ITT longitudinal data. HLM is a practical strategy for analyzing effectiveness data because the method does not assume equal numbers of observations or fixed time points of measurement and missing data do not cause special problems (Raudenbush & Bryk, 2002).
In the current study, HLM was used to investigate longitudinal PCL-M outcomes (level-one) nested within patients (level-two) to assess overall treatment response and response patterns over time. Additionally, to foster an understanding of PE-related treatment effects among OEF/OIF Veterans, exploratory analyses were used to investigate if patient characteristics, i.e., age, gender, race/ethnicity, service disability rating, and baseline pathology were significant predictors of treatment response. Variance components, sigma squared (σ2) and tao (τ), were estimated and used to calculate intraclass correlations. Statistically significant outcomes were qualified using between- and within-R2-type effect sizes in a manner consistent with recommended guidelines (Snijders & Bosker, 1994).
3. Results
3.1 Treatment Completion and Duration
Forty-three Veterans (66%) met criteria as treatment completers. The mean number of sessions for treatment completers was 10 (SD=4). The mean number of sessions for the total ITT sample was 7 (SD=5) with 52 patients (80%) attending 10 or fewer sessions, 61 patients (94%) attending 15 or fewer sessions, and 4 patients (6%) attending between 16 and 25 sessions. Twenty-two patients (34%) did not complete at least 6 sessions and were classified as non-completers, these patients were retained for analyses in the ITT sample. Patient characteristics, i.e., age, gender, race/ethnicity, disability rating, and baseline PCL-M and BDI-II severity scores were not predictors of treatment completion.
3.2 PCL-M & BDI-II Outcomes: t-tests
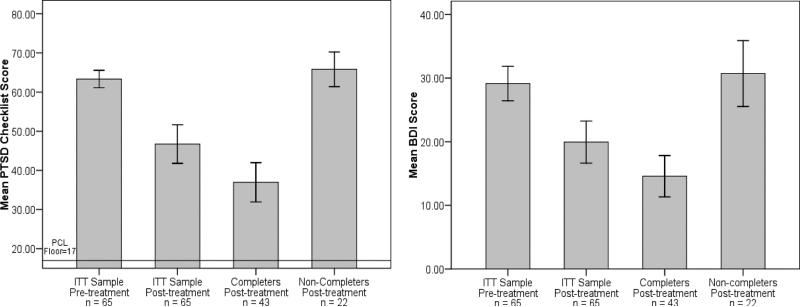
Mean pre- and post-treatment PCL-M scores for the ITT sample were 63.05 (SD=8.59) and 46.29 (SD=19.52). This difference is clinically and statistically significant (t=8.02, df=61, p< .001, d=1.19). Mean pre- and post-treatment PCL-M scores for the treatment completer sample were 61.80 (SD=8.30) and 36.66 (SD=15.95). This difference is also clinically and statistically significant (t =11.60, df=40, p< .001, d=2.07). Figure one displays the pre-post PCL-M means with 95% confidence intervals for the ITT sample and the post PCL-M means for treatment completers and non-completers. PCL-M standard deviations were notably larger at post-treatment than pre-treatment. Accordingly, using the pooled standard deviation to calculate d as a primary indicator of treatment outcome may obscure a sizable proportion of Veterans who reported remarkable symptom amelioration concurrent with treatment. For example, on average in the ITT sample, patients improved by over a standard deviation; however, 33% of the ITT sample and 50% of the treatment completers sample scored 30 or below on the PCL-M post-treatment, which is well below the clinical range.
Figure 1.
Pre-post outcomes with 95% confidence intervals for the ITT sample, treatment completers, and non-completers.
Mean pre- and post-treatment BDI-II scores for the ITT sample were 29.15 (SD=10.44) and 20.75 (SD=12.91). This difference is clinically and statistically significant (t=6.17, df=59, p< .001,d=.72). Mean pre- and post-treatment BDI-II scores for the treatment completer sample were 28.08 (SD=10.05) and 15.38 (SD=10.32). This difference is also clinically and statistically significant (t=7.43, df=38, p<.001, d=1.25). Figure one displays the pre-post BDI-II means with 95% confidence intervals for the ITT sample and the post BDI-II means for treatment completers and non-completers.
3.3 PCL-M Outcomes: HLM Results
Posttraumatic Stress Checklist-Military Version (PCL-M)
Models of longitudinal PCL-M outcomes for the ITT sample were based on 200 points of measurement (level one) nested within 65 patients (level two). The unconditional model estimated variance components for level-one and level-two units (σ2 =186.39, τ =102.85). The value of τ was significantly different from zero (χ2=174.27, df=64, p.<.001), indicating the presence of patient-level effects on outcomes. The intra-class correlation (ICC) was .36, indicating that 36% of total PCL-M variance could be accounted for by factors associated with the patient (R2-between). Such factors could be related to personal characteristics (i.e., age or baseline pathology) or external factors that varied by patient (i.e., assigned therapist or seasonal effects). The remaining variance (64%) could be attributed to within-patient effects (R2-within), such as time in treatment or to other un-modeled factors.
The next sequential step in modeling involved adding time-in-treatment (i.e., occurrence of longitudinal measurement, or “session dose”) as a level-one within-patient predictor. Because measurements were taken every two weeks during the course of treatment, each unit of measurement translated into two sessions of PE. Time-in-treatment significantly predicted PCLM outcomes (σ2 = 80.31, τ =110.49, Χ2=362.25, df=64, p.<.001). The modeled coefficient indicated that each two-session unit was associated with a 6.98 point decrease in PCL-M symptoms (95% CI 5.38-8.40; t =−8.56, df=198, p<.001). The time-in-treatment effect accounted for 32% of the within-patient variance in outcomes (R2-within=.32).
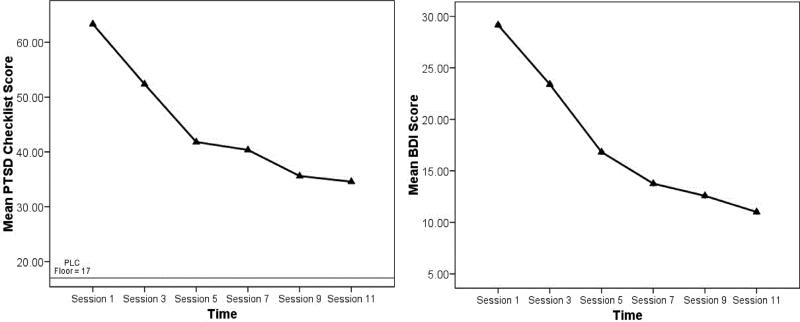
An examination of the plotted PCL-M means indicated a more rapid decline in symptoms early in treatment and then continued improvement at a slower pace. Accordingly, the next sequential step in modeling involved adding a quadratic time-in-treatment term to determine if treatment effects were consistent across time. The quadratic time-in-treatment term significantly predicted PCL-M outcomes (σ2=74.78, τ=101.57, Χ2=357.59, df=64, p.=.001). The modeled coefficient (1.15; t=3.66, df=197, p=.001) confirmed that treatment gains were more robust earlier in the treatment process and then leveled off. The quadratic effect accounted for 10% of the within patient variance in outcomes (R2-within=.10) over and above time in treatment alone.
3.4 Patient Characteristics and Outcomes
With overall treatment effects accounted for, the next step in the model involved adding patient characteristics to explore for potential disparities in outcomes. Age, gender, and service connected disability rating were not statistically significant predictors of treatment response. Veteran race significantly predicted PCL-M scores (σ2=76.19, τ=88.23, Χ2=296.11,df=60, p.<.001). The modeled coefficient (7.67; t=2.70, df=60, p=.009) indicated that treatment seeking Black OEF/OIF Veterans, on average, scored higher on the PCL-M than treatment seeking White OEF/OIF Veterans. The effect accounted for 7% of the variance in overall PCL-M scores. However, race-related differences diminished over time from baseline, with no clinically or statistically significant differences post treatment. Additionally, race was not a significant predictor of the slope of treatment effects over time. Accordingly, race was removed from the model as it had little effect on the outcome or course of treatment.
Baseline PCL-M scores were entered as a predictor of the time in treatment slope on PCL-M outcomes to investigate if there were differences in the course of treatment progress associated with baseline symptom severity. Baseline PCL-M was a statistically significant predictor of the slope of time on PCL-M outcomes (0.73; t=12.90, df=63, p.<.001). Although this effect was statistically significant, it accounted for practically none of the variance in outcomes (R2-between<.00). Accordingly, baseline PCL-M was removed from the model.
Overall, the final parsimonious HLM model (Table 2) partitions variance in PCL-M outcomes into a portion associated with patient-level factors (36%) and a portion associated with level-one longitudinal and/or other unmodeled factors (64%). Time in treatment, including a quadratic term indicative of a steeper slope of improvement earlier on in treatment, accounted for 42% of the variance in level-one outcomes. Although Veterans who were Black scored higher on the PCL-M at baseline, patient-level characteristics, including racial status, age, gender and service connected disability rating were not associated with overall treatment response or the slope of response over the course of treatment.
Table 2.
Longitudinal PCL-M outcomes during PE treatment (df within = 197, df between = 64)
| Fixed Effect | Coefficient | Standard Error | T-ratio | p |
|---|---|---|---|---|
| Intercept | 75.91 | 2.05 | 37.08 | < 0.001 |
| Time in Treatment | −13.96 | 1.92 | −7.26 | < 0.001 |
| Time in Treatment2 | 1.15 | 0.32 | 3.66 | < 0.001 |
| Random Effect | Variance Component | Chi-square | p |
|---|---|---|---|
| Intercept (u0) | 101.56 | 357.95 | < 0.001 |
| Level One (r) | 74.76 |
3.5 BDI-II Outcomes: HLM Results
The unconditional model estimated variance components for both level-one and level-two units (σ2=73.67, τ=62.24). The value of τ was significantly different from zero (χ2=217.72, df=64, p.<.001), indicating the presence of patient-level effects on outcomes. The intraclass correlation (ICC) was .46, indicating that 46% of all BDI-II variance could be accounted for by factors associated with the patient (R2-between).
Time-in-treatment significantly predicted BDI-II outcomes (σ2=38.63, τ=63.93, χ2=349.09, df=64, p.<.001). The time-in-treatment effect accounted for 25% of the within patient variance in outcomes (R2-within=.25). A quadratic time-in-treatment term significantly predicted BDI-II outcomes; however, the effect accounted for only 2% of the within patient variance (R2-within=.02) over and above time in treatment alone. Age, gender, race/ethnicity, and service connected disability rating were not significant predictors of pathology or treatment response.
4. Discussion
4.1 Summary
Results of the present study indicate that PE is an effective treatment for combat-related PTSD. Moreover, the study shows that PE can be effectively implemented in a VAMC setting with veterans of the wars in Iraq and Afghanistan. Treatment retention was adequate, suggesting that PE can be well tolerated by OEF/OIF Veterans. Treatment effect sizes for both the ITT sample and for the treatment completer group were statistically significant and large. Patient characteristics, including race, age, gender, baseline severity, and service connected disability rating were not meaningfully associated with treatment outcomes or the slope of outcomes over the course of treatment.
4.2 Effect Size & Completion Rate Comparison
Effect sizes reported in this effectiveness study (ITT sample d=1.19; treatment completer, d=2.07) are large and similar to effect sizes found in prior randomized controlled trials of PE in civilian populations [ITT, d=1.46; completer, d=1.92 (Foa et al., 1992), ITT, d=1.37; completer, d=3.31 (Foa et al., 2005), ITT, d=1.08; completer, d=1.94 (Resick et al., 2002)]. Moreover, pre- and post-treatment changes in PCL-M scores for the current sample of OEF/OIF Veterans (−16.8) are comparable to those found in a prior study of PE for female Veterans and active duty personnel (−16.6; Schnurr, 2007). These results suggest that PE conducted in routine VA mental healthcare settings can be as effective as when implemented in carefully controlled randomized trials.
Anecdotally, VAMC providers frequently note that OEF/OIF Veterans have poor rates of retention for mental health treatments in general. The rate found in the current investigation, 66%, can be considered high or low depending on one's perspective. From our perspective as direct providers of mental health services to Veterans, retaining two-thirds of an OEF/OIF sample for weekly, 90-minute sessions without direct compensation constitutes a reasonable success for a treatment modality. This retention rate is similar to what has been observed in RCTs of PE in civilian populations [(65%) Foa et al., 2005; (73%) Resick et al., 2002] and for female Veterans (62%; Schnurr et al., 2007); however, varying treatment completion criteria among studies makes direct comparisons difficult to interpret. In the current study, we modified completion criteria to match the pragmatic behaviors and historic symptom amelioration patterns of OEF/OIF patients in our clinic. Outcomes of this study provide initial support for that modification and the preference of OEF/OIF Veterans for shorter treatment time frames, as figure 2 indicates statistically significant diminished returns on treatment after session 5. Nevertheless, while patients, on average, continued to improve more slowly after the fifth session, longer treatment courses were necessary for some patients to reach sufficient symptom amelioration.
Figure 2.
PTSD Checklist (PCL) and Beck Depression Inventory-II (BDI) outcomes over the course of treatment.
In order to foster appropriate comparisons and an understanding of the effect sizes and treatment completion rates reported here, a reiteration of our intake process is merited. OEF/OIF Veterans are most often referred from primary care to the general mental health clinic for a mental health intake. Mental health providers then make referrals for specialized treatment to the PCT. Subsequently, Veterans are assigned a PCT-associated case manager who meets with them and coordinates an assessment appointment in which a CAPS is completed. Assignment to a PE therapist occurs only after the CAPS assessment confirms a PTSD diagnosis. Accordingly, before an OEF/OIF veteran begins PE treatment, he or she has most likely already come to three mental health-related appointments. Thus, OEF/OIF Veterans beginning treatment in our clinic have already demonstrated a track record of attending mental health-related appointments and may be more motivated for treatment than other populations of OEF/OIF Veterans. Moreover, we have little doubt that recidivism rates would be higher and effect sizes smaller if we took referrals without confirming a PTSD diagnosis via a structured assessment interview.
4.3 Limitations
There were several limitations of the current study. First, therapist fidelity to the PE protocol and patient compliance to the protocol were not assessed. Although need for fidelity checks is somewhat less central in effectiveness trials, all therapists were trained in PE as part of the VA national dissemination effort and participated in weekly group and individual supervision. Supervision was conducted by the primary author who is a national PE trainer for the VA and included limited tape review and problem solving regarding patient compliance. There were no differences in treatment outcomes among therapists. Second, all Veterans received treatment from one VAMC where therapists and patients enjoyed vigorous local institutional and structural support for providing evidence based treatments, including decreased patient case loads to accommodate 90-minute sessions, institutional purchasing of recording equipment and audio cassettes, and therapist control over their own clinic scheduling to facilitate the flexibility necessary to accommodate OEF/OIF patients for weekly appointments. It is unclear how well these results can generalize to other VAMCs with different resources, priorities, and cultures. Third, Veterans were not given the CAPS at the end of treatment to more formally examine the status of their PTSD diagnosis. However, end-point PCL-M results indicated that 32 Veterans (49% of the total sample and 74% of treatment completers) scored below the suggested PCL-M cutoff of 44 (Blanchard et al.,1996; Ruggiero, Del Ben, Scotti, & Rabalais, 2003) used in other recent investigations of OEF/OIF-related PTSD (Booth-Kewley, et al.,2010; McGhee, Maani, Garza, Gaylord, & Black, 2008). Finally, this study did not include a comparison control group or “patched-up” (Kazdin, 2002) control group. However, PE has been studied in numerous RCTs and has been shown to be superior to less-active treatments, accordingly, the need for a control group is somewhat mitigated. Moreover, the overarching aim of this effectiveness study is not to investigate how PE performs compared to treatment as usual, but rather, how it performs as treatment as usual in a VA setting.
4.4 Future Directions
The current study highlights several questions in need of further investigation. Results suggest that PE is equally effective for subgroups of OEF/OIF patient populations based on gender and racial status. Future studies should look more intentionally at how PE is received by combat Veterans from diverse racial and ethic backgrounds, including those with concurrent secondary or primary mental health-related diagnoses and traumatic brain injury (TBI). The current study also suggests that service connection disability status did not affect ability to improve with treatment. Although this finding is not sufficient to address long-standing questions regarding the role of secondary gain in Veteran health contexts, it does provide initial and promising evidence that PE can be effective for OEF/OIF Veterans regardless of service connection disability for PTSD. In addition, although there is no empirical evidence or substantiated reason to believe that PE treatment effects would significantly vary for veterans of different war eras, future studies should address this issue in regular treatment settings, especially because conventional wisdom and clinical lore in many VA settings often point to a disparaging prognoses for older veterans with chronic PTSD. Finally, while the retention rate in the current study was adequate, there is clearly a need to study ways to further optimize adherence and minimize attrition across all populations of Veterans with PTSD.
A sustained and vigorous effort needs to be made to effectively disseminate exposure therapy and other evidence based treatments into routine healthcare. The VA has taken significant and meaningful steps towards this by providing 4-day workshop trainings in PE to VA clinicians, including support for rigorous and meaningful follow-up supervision. However, questions remain about how these training efforts will impact the routine mental health treatment of Veterans. While the current study was not an investigation of the PE dissemination program, it does provide unambiguous support for the rationale of large-scale efforts to promote the use of exposure therapy within veteran mental health settings. Doing so will help to ensure that the next generation of returning war Veterans will receive the quality care they deserve.
Funding Acknowledgements
Dr. Tuerk is supported by Veterans Health Administration, Office of Research and Development, Clinical Sciences Research and Development Award, CDA-2-0003; and by the South Carolina Clinical & Translational Research Institute, Medical University of South Carolina's CTSA, NIH/NCRR Grant Number UL1RR029882.; Dr. Grubaugh is supported by a Veterans Health Administration, Health Services and Research and Development CDA-2 Award, Dr. Acierno is supported by VA HSR&D Merit grant IIR-04-421 (PI: Egede) and Department of Defense grant W81XWH-07-PTSD-IIRA (PI: Acierno).The contents are solely the responsibility of the authors and do not necessarily represent the official views of the VA, NIH, NCRR, or the DoD.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Beck A, Steer R, Brown G. Manual for Beck Depression Inventory-II. Psychological Corporation; San Antonio, Tex: 1996. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL-M). Behaviour Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Booth-Kewley S, Larson G, Highfill-McRoy R, Garland C, Gaskin T. Correlatesof posttraumatic stress disorder symptoms in Marines back from war. Journal of Traumatic Stress. 2010;23(1):69–77. doi: 10.1002/jts.20485. [DOI] [PubMed] [Google Scholar]
- Cooper NA, Clum BA. Imaginal flooding as a supplemental treatment for PTSD in combat veterans: A controlled study. Behavior Therapy. 1989;20:381–391. [Google Scholar]
- Defense Manpower Data Center Contingency Tracking System. 2009 Retrieved from https://www.dmdc.osd.mil/appj/dwp/getLinks.do?category=dod&subCatdataInq&tab=3&clOn=dod.
- Drake RE, Goldman HH, Leff HS, Lehman AF, Dixon L, Mueser KM, et al. Implementing evidence-based practices in routine mental health service settings. Psychiatric Services. 2001;52:179–182. doi: 10.1176/appi.ps.52.2.179. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Auchterlonie JL, Millikin CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. Journal of the American Medical Association. 2006;295:1023–1032. doi: 10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis I disorders. Biometrics Research Department, New York State Psychiatric Institute; New York: 1996. [Google Scholar]
- Foa EB, Dancu CV, Hembree EA, Jaycox LH, Meadows EA, Street GP. A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical Psychology. 1999;67(2):194–200. doi: 10.1037//0022-006x.67.2.194. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, Rothbaum BO. Prolonged Exposure Therapy for PTSD: Emotional Processing of Traumatic Experiences, Therapist Guide. Oxford University Press; New York, NY: 2007. [Google Scholar]
- Foa EB, Hembree EA, Cahill SP, Rauch SA, Riggs DS, Feeny NC, et al. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical Psychology. 2005;73:953–964. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- Frueh BC, Cusack KJ, Hiers TG, Monogan S, Cousins VC, Cavenaugh SD. Improving public mental health services for trauma victims in South Carolina. Psychiatric Services. 2001;52:812–814. doi: 10.1176/appi.ps.52.6.812. [DOI] [PubMed] [Google Scholar]
- Frueh BC, Grubaugh AL, Cusack KJ, Elhai JD. Disseminating evidence-basedpractices for adults with PTSD and severe mental illness in public-sector mental health agencies. Behavior Modification. 2009;33:66–81. doi: 10.1177/0145445508322619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frueh BC, Monnier J, Yim E, Grubaugh AL, Hamner MB, Knapp RG. A randomized trial of telepsychiatry for post-traumatic stress disorder. Journal of Telemedicine & Telecare. 2007;13:142–147. doi: 10.1258/135763307780677604. [DOI] [PubMed] [Google Scholar]
- Hanson TC, Hesselbrock M, Tworkowski SH, Swan S. The prevalence and management of trauma in the public domain: An agency and clinician perspective. Journal of Behavioral Health Services Research. 2002;29:365–380. doi: 10.1007/BF02287344. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine Treatment of PTSD: An assessment of the evidence. Report Brief, October, 2007. 2007 Retrieved from http://www.iom.edu/~/media/Files/ Report%20Files /2007/Treatment-of-PTSD-An-Assessment-of-The Evidence/PTSDReportBriefFINAL2.ashx.
- Kazdin AE. Research design in clinical psychology. 4th ed. Allyn & Bacon; Boston: 2002. [Google Scholar]
- Keane TM, Fairbank JA, Caddell JM, Zimering RT. Implosive (flooding) therapy reduces symptoms of PTSD in Vietnam combat veterans. Behavior Therapy. 1989;20:245–260. [Google Scholar]
- Kreft I, De Leeuw J. Introducing multilevel modeling. Sage; London: 1998. [Google Scholar]
- McGhee L, Maani C, Garza T, Gaylord K, Black I. The correlation between ketamine and posttraumatic stress disorder in burned service members. The Journal of Trauma. 2008;64(2 Suppl):S195. doi: 10.1097/TA.0b013e318160ba1d. Retrieved from MEDLINE database. [DOI] [PubMed] [Google Scholar]
- Marks I, Lovell K, Noshirvani H, Livanou M, Thrasher S. Treatment of posttraumatic stress disorder by exposure and/or cognitive restructuring: A controlled study. Archives of General Psychiatry. 1998;55:317–325. doi: 10.1001/archpsyc.55.4.317. [DOI] [PubMed] [Google Scholar]
- Office of the Surgeon General United States Army Medical Command, Mental Health Advisory Team (MHAT)-V OIF 06-08: Iraq, OEF 2008 Retrieved from http://www.armymedicine.army.mil/news/mhat/mhat_v/MHAT_V_OIFandOEFRedacted.pdf.
- Rand Center for Military Health Policy . Invisible Wounds of War: Summary and Recommendations for Addressing Psychological and Cognitive Injuries. (Document:MG-720/1-CCF;ISBN/EAN:9780833044532) U.S; Arlington, VA: 2008. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2nd edition Sage; Newbury Park, CA: 2002. [Google Scholar]
- Rauch SAM, Defever E, Favorite T, Duroe A, Garrity C, Martis B, et al. Prolonged exposure for PTSD in a veterans health administration PTSD clinic. Journal of Traumatic Stress. 2009;22:60–64. doi: 10.1002/jts.20380. [DOI] [PubMed] [Google Scholar]
- Ready DJ, Thomas KR, Worley V, Backscheider AG, Harvey LAC, Baltzell D, et al. A field test of group based exposure therapy with 102 veterans with war-related posttraumatic stress disorder. Journal of Traumatic Stress. 2008;21:150–157. doi: 10.1002/jts.20326. [DOI] [PubMed] [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology. 2002;70:867–879. doi: 10.1037//0022-006x.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen CS, Chow HC, Finney JF, Greenbaum MA, Moos RH, Sheikh JI, et al. VA practice patterns and practice guidelines for treating posttraumatic stress disorder. Journal of Traumatic Stress. 2004;17:213–222. doi: 10.1023/B:JOTS.0000029264.23878.53. [DOI] [PubMed] [Google Scholar]
- Ruggiero K, Del Ben K, Scotti J, Rabalais A. Psychometric Properties of the PTSD Checklist—Civilian Version. Journal of Traumatic Stress. 2003;16(5):495. doi: 10.1023/A:1025714729117. Retrieved from Psychology and Behavioral Sciences Collection database. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Chow BK, et al. Cognitive behavioral therapy for posttraumatic stress disorder in women: A randomized controlled trial. Journal of the American Medical Association. 2007;297:820–830. doi: 10.1001/jama.297.8.820. [DOI] [PubMed] [Google Scholar]
- Snijders T, Bosker R. Modeling variance in two-level models. Sociological Methods and Research. 1994;22:342–363. [Google Scholar]
- Steer RA, Clark DA. Psychometric characteristics of the Beck Depression Inventory-II with college students. Measurement and Evaluation in Counsel and Development. 1997;30:128–136. [Google Scholar]
- Tuerk PW, Yoder M, Ruggiero KJ, Gros DF, Acierno R. A Pilot Study of Prolonged Exposure Therapy for Posttraumatic Stress Disorder Delivered via Telehealth Technology. Journal of Traumatic Stress. 2010;23(1):116–123. doi: 10.1002/jts.20494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U. S. Department of Veterans Affairs, Research and Development Press Release Retrieved from http://www.research.va.gov/resdev/news/press_releases/ptsd-101807.cfm.
- U. S. Department of Veterans Affairs & Department of Defense . VA/DoD clinical practice guidelines for the management of post-traumatic stress. VA/DoDO; Washington, DC.: 2004. [Google Scholar]
- Weathers FW, Huska J, Keane T. The PTSD Checklist-Military Version. National Center for PTSD; Boston, MA: 1991. [Google Scholar]
- Weathers FW, Keane TM, Davidson JR. Clinician-Administered PTSD Scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]