Abstract
OBJECTIVE
To define the frequency, risk factors, and outcomes of massive transfusion in obstetrics.
METHODS
The State Inpatient Dataset for New York (1998–2007) was used to identify all delivery hospitalizations for hospitals that reported at least one delivery-related transfusion per year. Multivariable logistic regression analysis was performed to examine the relationship between maternal age, race, and relevant clinical variables and the risk of massive blood transfusion defined as 10 or more units of blood recorded.
RESULTS
Massive blood transfusion complicated 6 of every 10,000 deliveries with cases observed even in the smallest facilities. Risk factors with the strongest independent associations with massive blood transfusion included abnormal placentation (1.6/10,000 deliveries, adjusted odds ratio [OR] 18.5, 95% confidence interval [CI] 14.7–23.3), placental abruption (1.0/10,000, adjusted OR 14.6, 95% CI 11.2–19.0), severe preeclampsia (0.8/10,000, adjusted OR 10.4, 95% CI 7.7–14.2), and intrauterine fetal demise (0.7/10,000, adjusted OR 5.5, 95% CI 3.9–7.8). The most common etiologies of massive blood transfusion were abnormal placentation (26.6% of cases), uterine atony (21.2%), placental abruption (16.7%), and postpartum hemorrhage associated with coagulopathy (15.0%). A disproportionate number of women who received a massive blood transfusion experienced severe morbidity including renal failure, acute respiratory distress syndrome, sepsis, and in-hospital death.
CONCLUSION
Massive blood transfusion was infrequent, regardless of facility size. In the presence of known risk for receipt of massive blood transfusion, women should be informed of this possibility, should deliver in a well-resourced facility if possible, and should receive appropriate blood product preparation and venous access in advance of delivery.
Massive blood transfusion is traditionally defined as transfusion of 10 or more units of packed red blood cells in less than 24 hours.1,2 In obstetrics, massive blood transfusion signifies major obstetric hemorrhage that requires extensive coordination of the obstetric, anesthesia, and blood bank teams and can significantly strain resources in small hospitals with limited delivery volume and blood bank resources. The workload encountered in these cases can be extreme, and individual clinical expertise is often insufficient without well-coordinated teams and systems of care. Institutional preparation is now recognized as essential to ensure effective clinical care in these emergencies.3,4 Clinical teams need leaders to develop, implement, and periodically review multidisciplinary obstetric hemorrhage protocols.
Although extensively studied in the trauma and general surgery setting, relatively little is known about the frequency, risk factors, and outcomes from massive transfusion in obstetrics. This information may be helpful in triaging high-risk patients to centers that can meet this demand,5-7 in motivating and informing systems changes in preparation for these emergencies, and in defining research priorities around this clinical issue. The need for this information is made more urgent by the escalating rate of postpartum hemorrhage in developed countries.8-10
Using data from a sample of New York State hospitals, the objectives of the present report are: 1) to evaluate antepartum conditions that can be associated with massive blood transfusion; 2) to define outcomes after massive blood transfusion; and 3) to ascertain trends in massive blood transfusion in the past decade.
MATERIALS AND METHODS
We conducted a retrospective cross-sectional study of hospitalizations for delivery using the 1998–2007 Healthcare Cost and Utilization Project State Inpatient Dataset for New York. The Healthcare Cost and Utilization Project is a federal–state–industry partnership sponsored by the Agency for Healthcare Research and Quality. The Statewide Planning and Research Cooperative System collects the data elements for the New York State Inpatient Data, including patient-level detail on patient characteristics, diagnoses, and treatments for every hospital discharge.11 Individual hospitals are required by state law to submit the data, which are subjected to a series of error checks and audits to ensure both accuracy and completeness. Monthly error reports back to the submitting facilities include information the facility needs to make any necessary corrections in their data submission. The corrected data are then resubmitted and are included in the facility’s cumulative database. Because New York State Inpatient Data exclude data elements that could directly and indirectly identify individuals, this research was considered exempt from review by the institutional review boards of participating authors’ institutions.
Among other variables, the New York State Inpatient Data capture age, race, hospital length of stay, disposition from the hospital (including in-hospital death), and diagnostic and procedural codes defined in the International Classification of Diseases 9th Edition, Clinical Modification.12 To select hospitalizations for delivery, we applied the coding algorithm described by Kuklina13 without selecting for any Diagnosis-Related Group codes, because these codes changed inconsistently within years and within hospitals during the study period.
New York State Inpatient Data are unique because they capture “the total number of pints of whole blood or units of packed red cells furnished to the patient.”11 Both products are reported in a single data element as the number of units of blood transfused. The data element does not record the quantity of transfused platelets, cryoprecipitate, or plasma; this information is not available for analysis. For the purpose of this analysis, we defined a massive blood transfusion for obstetric hemorrhage as a hospitalization with at least 10 units of blood recorded (ie, packed red blood cells or whole blood) and a coexisting diagnostic code indicating obstetric hemorrhage or a condition that typically leads to obstetric hemorrhage. These obstetric hemorrhage diagnostic codes were then used to characterize the most likely etiology of hemorrhage using a hierarchical algorithm that defined diagnoses in the following order: amniotic fluid embolism, uterine rupture, abnormal placentation (defined as retained placenta including placenta accreta, or placenta previa), abruption, coagulopathy, antepartum hemorrhage of other etiologies (ie, antepartum hemorrhage associated with coagulation defects, trauma, uterine leiomyoma, or unspecified conditions), uterine atony, obstetric trauma, and delayed postpartum hemorrhage.14 Risk factors for obstetric hemorrhage and major morbidities associated with massive blood transfusion were identified based on previously published diagnostic and procedural coding algorithms14,15 and included placental abruption, abnormal placentation, prior cesarean delivery, intrauterine fetal demise, chorioamnionitis, multiple gestation, uterine leiomyomas, severe preeclampsia, and medical induction of labor. Hospital identifiers were used to calculate hospital-level variables such as the annual delivery volume.
Because the number of units of blood transfused is a supplemental and voluntary data element, data may be incomplete. Therefore, we analyzed only those women who delivered at a hospital in which at least one woman received at least one unit of blood during the year of delivery. We further restricted the trend analysis to New York hospitals that consistently reported at least one unit transfused to at least one patient each year of the entire study period and compared the overall frequency for the years 1998–2002 with the frequency for the years 2003–2007 corresponding to the first and second halves of the study period.
Statistical analyses included χ2 to test for a difference in proportions and multivariable logistic regression analyses to examine the relationship among maternal age, race, and relevant clinical variables on the risk of massive blood transfusion. All variables were included in a single model. Additional logistic regression analyses were used to evaluate the strength of association between massive blood transfusion and severe morbidities, including acute renal failure, acute respiratory distress syndrome, sepsis, mechanical ventilation, and hysterectomy, and in-hospital maternal death adjusted for age. Results are presented as odds ratios and 95% confidence intervals (CIs). Frequencies of massive blood transfusion were calculated for each hospital and year combination, presented as mean event frequencies stratified by hospital delivery volume. Changes in the frequency of massive blood transfusion were compared using χ2. Statistical analyses were performed using IBM SPSS Statistics for Windows 19.0. and Stata Statistical Software 12. P values <.05 were used to define statistical significance for all analyses.
RESULTS
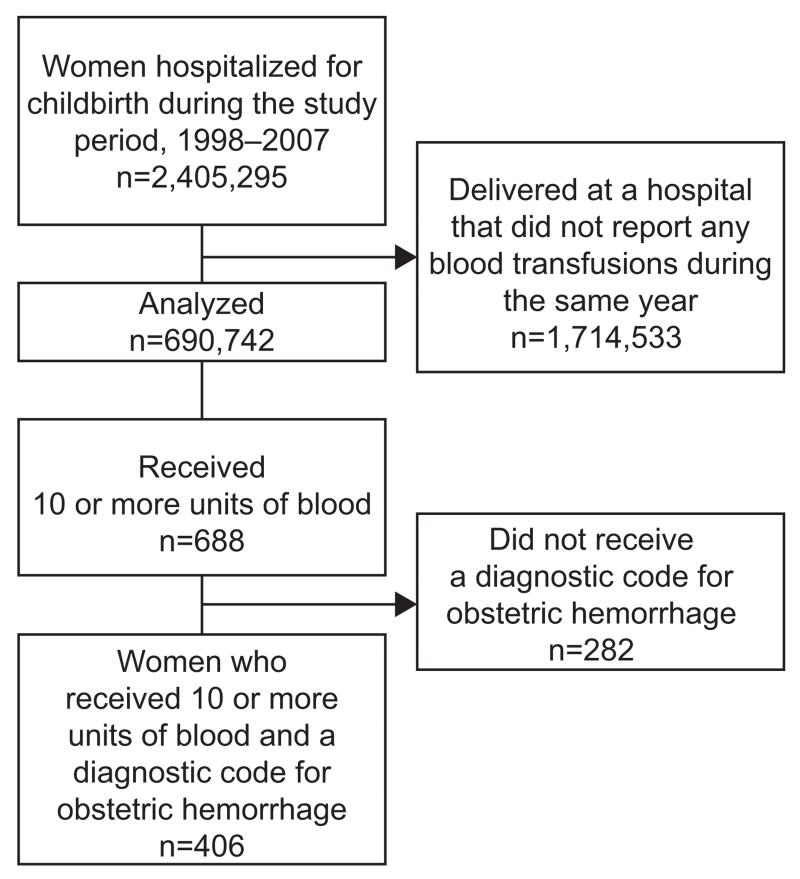
During the study period 1998–2007, there were 690,742 women who delivered in one of 57 unique hospitals in which at least one woman was reported to have received at least one unit of blood during the same year (Fig. 1). Comparison between these included women and those delivered elsewhere suggest little difference, except that those delivering in centers with fewer than 1,000 births per year were more likely to be excluded (Appendix 1, available online at http://links.lww.com/AOG/A444). Among the included sample, 21,620 (3.2%) individuals received at least one unit of blood for any indication, 4,187 (0.61%) received at least one unit of blood for obstetric hemorrhage, and 406 (0.06%) received a massive transfusion (10 or more units of blood) for obstetric hemorrhage. This corresponds to an event rate of 5.9 massive blood transfusions for obstetric hemorrhage per 10,000 deliveries. Another 282 women received 10 or more units of blood during the delivery admission but were not diagnosed with obstetric hemorrhage; the majority of these individuals delivered at large-volume centers (Appendix 2, available online at http://links.lww.com/AOG/A445). Altogether, 688 women received a massive blood transfusion for any indication, corresponding to a frequency of 10.0 per 10,000 deliveries (95% CI 9.2–10.7).
Fig. 1.
Patient flow diagram.
Table 1 shows the frequency of maternal demographic and clinical characteristics in the delivering cohort and the association with massive transfusion for obstetric hemorrhage. Women who received a massive blood transfusion were more likely to be black or Asian as opposed to non-Hispanic white and were more likely to be older or to display a known risk factor for antepartum or postpartum hemorrhage.
Table 1. Baseline Characteristics of Delivering Population.
| Characteristic | With Massive Transfusion (n=406) |
Without Massive Transfusion (n=690,336) |
P |
|---|---|---|---|
| Maternal age (y) | <.01 | ||
| Younger than 20 | 16 (3.9) | 44,261 (6.4) | |
| 20–34 | 229 (56.4) | 496,740 (72.0) | |
| 35–39 | 118 (29.1) | 119,620 (17.3) | |
| 40 or older | 43 (10.6) | 29,715 (4.3) | |
| Race | <.01 | ||
| Non-Hispanic white |
175 (43.1) | 371,440 (53.8) | |
| Non-Hispanic black |
92 (22.7) | 99,532 (14.4) | |
| Hispanic | 66 (16.3) | 113,430 (16.4) | |
| Asian or Pacific Islander |
32 (7.9) | 39,612 (5.7) | |
| Other or missing | 41 (10.1) | 66,322 (9.6) | |
| Antepartum conditions |
|||
| Placental abruption |
78 (19.2) | 6,096 (0.9) | <.01 |
| Abnormal placentation |
113 (27.8) | 10,034 (1.5) | <.01 |
| Prior cesarean delivery |
84 (20.7) | 95,718 (13.9) | <.01 |
| Intrauterine fetal demise |
45 (11.1) | 4,265 (0.6) | <.01 |
| Risk factors for atony | |||
| Chorioamnionitis | 21 (5.2) | 11,496 (1.7) | <.01 |
| Multiple gestation | 27 (6.7) | 16,328 (2.4) | <.01 |
| Leiomyomas | 24 (5.9) | 8,852 (1.3) | <.01 |
| Severe preeclampsia |
53 (13.1) | 6,387 (0.9) | <.01 |
| Medical induction of labor |
53 (13.1) | 86,914 (12.6) | .78 |
| Cesarean delivery | 265 (65.3) | 207,634 (30.1) | <.01 |
Data are n (%) unless otherwise specified.
Event rates for each demographic category or clinical condition and results of the full multivariable model are listed in Table 2. Controlling for all clinical variables, risk was increased among women older than 34 years of age and across black, Hispanic, and Asian or Pacific Islander populations when compared with non-Hispanic whites. Clinical risk factors with the strongest independent associations with massive blood transfusion include placental abruption, abnormal placentation, intrauterine fetal demise, and severe preeclampsia. The magnitude of independent associations between massive transfusion and a history of cesarean delivery, chorioamnionitis, multiple gestation, and uterine leiomyomas was less impressive but statistically significant.
Table 2. Multivariate Model to Predict Massive Transfusion for Obstetric Hemorrhage.
| Characteristic | Rate of Massive Transfusion/10,000 Women With Each Condition (95% CI) |
Adjusted Odds Ratio (95% CI)* |
|---|---|---|
| Maternal age (y) | ||
| Younger than 20 | 3.6 (1.8–5.4) | 0.7 (0.4–1.2) |
| 20–34 | 4.6 (4.0–5.2) | Reference |
| 35–39 | 9.9 (8.1–11.6) | 1.8 (1.4–2.3) |
| 40 or older | 14.5 (10.1–18.8) | 2.1 (1.5–2.9) |
| Race | ||
| Non-Hispanic white |
4.7 (4–5.4) | Reference |
| Non-Hispanic black |
9.2 (7.3–11.1) | 1.7 (1.3–2.2) |
| Hispanic | 5.8 (4.4–7.2) | 1.5 (1.1–2.0) |
| Asian or Pacific Islander |
8.1 (5.3–10.9) | 2.0 (1.4–2.9) |
| Other | 6.2 (4.3–8.1) | 1.3 (0.9–1.9) |
| Antepartum conditions |
||
| Placental abruption |
126.3 (98.5–154.2) | 14.6 (11.2–19.0) |
| Abnormal placentation |
111.4 (90.9–131.8) | 18.5 (14.7–23.3) |
| Prior cesarean delivery |
8.8 (6.9–10.6) | 1.6 (1.2–2.0) |
| Intrauterine fetal demise |
104.4 (74.1–134.8) | 5.5 (3.9–7.8) |
| Risk factors for atony | ||
| Chorioamnionitis | 18.2 (10.4–26) | 1.6 (1.0–2.6) |
| Multiple gestation | 16.5 (10.3–22.7) | 1.4 (1.0–2.2) |
| Leiomyomas | 27.0 (16.2–37.8) | 2.3 (1.5–3.6) |
| Severe preeclampsia |
82.3 (60.2–104.4) | 10.4 (7.7–14.2) |
| Induction of labor | 6.1 (4.5–7.7) | 1.1 (0.8–1.5) |
CI, confidence interval.
Statistically significant associations (P<.05) are denoted by bold type.
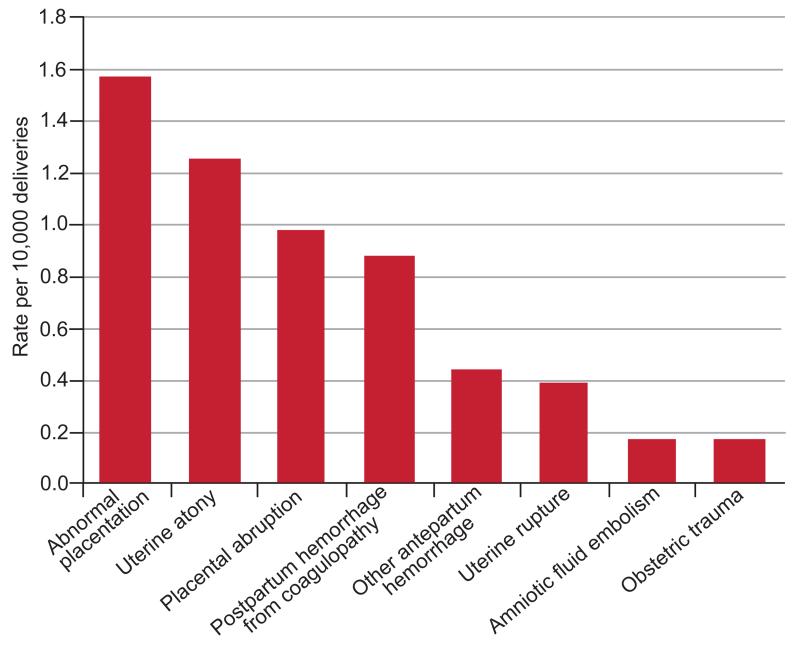
Etiologies of obstetric hemorrhage requiring massive transfusion are illustrated in Figure 2. The most common etiologies of massive blood transfusion were abnormal placentation (26.6% of cases), uterine atony (21.2%), placental abruption (16.7%), and postpartum hemorrhage associated with coagulopathy (15.0%).
Fig. 2.
Etiologies of hemorrhage. *Frequency of massive blood transfusion from delayed postpartum hemorrhage, not shown, to protect patient privacy and to comply with the data use agreement to report only groups that include more than 10 individuals.
Massive blood transfusion was also associated with severe complications including hysterectomy, acute renal failure, acute respiratory distress syndrome, sepsis, and the need for mechanical ventilation (Table 3). Massive blood transfusion was strongly associated with in-hospital maternal death with a mortality frequency of 3.4% compared with 1 in 10,000 in the general delivering population.
Table 3. Outcomes in Patients With Massive Transfusion.
| Outcome | With Massive Transfusion |
Without Massive Transfusion |
OR (95% CI)* |
|---|---|---|---|
| Acute renal failure |
37 (9.1) | 225 (0.03) | 265 (184–384) |
| Acute respiratory distress syndrome |
39 (9.6) | 238 (0.03) | 261 (182–373) |
| Sepsis | 12 (3) | 246 (0.04) | 82 (46–148) |
| Mechanical ventilation |
84 (20.7) | 368 (0.05) | 432 (331–563) |
| Hysterectomy | 152 (37.4) | 522 (0.08) | 722 (573–911) |
| In-hospital death |
14 (3.4) | 58 (0.01) | 361 (198–659) |
OR, odds ratio; CI, confidence interval.
Data are n (%) unless otherwise specified.
Age-adjusted.
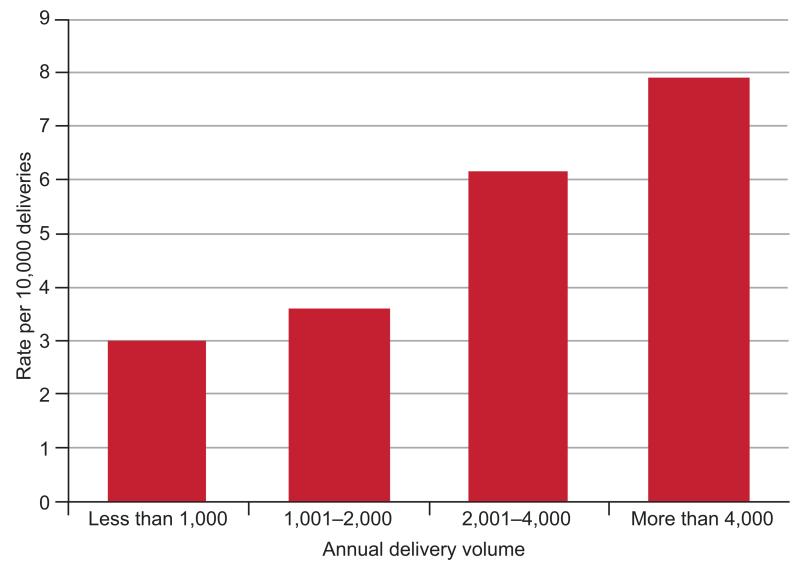
Figure 3 illustrates that the frequency of massive blood transfusion increased with increasing annual delivery volume but still occurred with a frequency of 3.0 in 10,000 deliveries at the smallest hospitals. After adjusting for the covariates displayed in Table 2, hospitals with 2,001–4,000 deliveries no longer had a significantly lower frequency of massive blood transfusion than the largest hospitals; the difference persisted for hospitals with 1,001–2,000 deliveries and less than 1,000 deliveries (P<.05).
Fig. 3.
Frequency of massive transfusion per 10,000 deliveries, stratified by hospital annual delivery volume.
Among 11 hospitals that documented at least one blood transfusion for each year of the study, the frequency of massive blood transfusion was 6.2 per 10,000 deliveries during the years 1998–2002 (95% CI 4.9–7.8) and 7.3 per 10,000 deliveries in the years 2003–2007 (95% CI 5.9–8.9), a difference that was not statistically significant (P=.32).
DISCUSSION
There are few data on massive hemorrhage and transfusion in the obstetric setting. This population-level analysis found that massive blood transfusion complicated 6 of every 10,000 deliveries with the incidence ranging between 3 per 10,000 in the smallest facilities to 8 per 10,000 in the facilities with delivery volume greater than 4,000 births per year. Even in the largest delivery centers, massive blood transfusion remains an infrequent event. This rarity reinforces the message that institutional multidisciplinary hemorrhage protocols and simulation are necessary at all levels of care to supplement and reinforce individual clinician experience for this rare event and to optimize system performance in response to an actual emergency.3,4,16,17
Abnormal placentation demonstrated the strongest association with massive blood transfusion. Including placenta accreta, placenta previa, and retained placenta, abnormal placentation was diagnosed in approximately 1.5% of deliveries. This proportion is consistent with previous work that has suggested placenta accreta complicates approximately 0.2% of pregnancies,18,19 placenta previa between 0.4% and 0.8%,20,21 and retained placenta between 1% and 3%.22,23 In our study, among women with a diagnosis of abnormal placentation, 1.4% required massive blood transfusion during their hospitalization for delivery. A previous analysis of the Nationwide Inpatient Sample suggested that abnormal placentation underlies 50% of all peripartum hysterectomies in the United States between 1994 and 2007,14 for a cause-specific hysterectomy frequency of 3.6 per 10,000 deliveries. A report of single-institution experience from Columbia Medical Center in New York between 1994 and 2008 confirms that approximately 40% of women (n=26/66) who undergo peripartum hysterectomy with pathologic evidence of placenta accreta require a massive blood transfusion, defined as 10 or more units of packed red blood cells.24 In our data, 152 (22.6%) of all women who underwent a peripartum hysterectomy required a massive blood transfusion. Placenta accreta likely introduces greater risk for massive blood transfusion when compared with other indications for peripartum hysterectomy. Maternal morbidity may be reduced when women with placenta accreta or other indication for peripartum hysterectomy deliver in tertiary care centers with multidisciplinary care.5,6
Our study identified several additional obstetric conditions associated with a heightened risk of massive blood transfusion, including placental abruption, intrauterine fetal demise, and severe preeclampsia. Women with any of these conditions might benefit from delivery in a facility with capacity to provide massive blood transfusion, although acute clinical presentation may preclude safe transfer in individual cases. Regardless, clinicians should ensure sufficient venous access and blood products before delivery.
A certain percentage of hemorrhage cases cannot be predicted from antepartum risk factors.8 The identified frequency of massive blood transfusion in the lowest volume delivery centers may underestimate catastrophic hemorrhage because many smaller facilities do not have a blood bank to support a massive transfusion before hospital transfer. Hemorrhage protocols must be adapted in birth centers and hospital facilities without the capacity to deliver large-volume blood transfusion. Official transport policies are necessary to ensure that time is not lost in negotiating a hospital bed.25 Finally, regional consolidation of birthing units may be possible in some markets.26
We recognize several limitations in our study. First, our definition of massive blood transfusion was based only on the number of units transfused with no reference to the time period over which the blood was transfused. Second, the number of units transfused is not a mandatory reporting element in New York State. Thus, generalizability of our results may be somewhat compromised because only hospitals that reported transfusion practice consistently were included in our study. Third, administrative data are susceptible to underascertainment and misclassification. There were 282 patients in the database who received massive blood transfusion during their hospitalization for delivery but did not have a diagnosis of obstetric hemorrhage and were excluded from our analysis; the etiologies of hemorrhage in these cases are unclear but likely represent either uncoded obstetric etiologies or fall outside of the obstetric etiologies that we defined for this analysis. Four of five women who received at least one unit of blood during the hospitalization for delivery did not receive a diagnosis for obstetric hemorrhage, suggesting high rates of either peripartum anemia, uncoded obstetric hemorrhage, or both. Fourth, the multivariable analysis did not consider mode of delivery for two reasons: first, confounding by indication could explain any association between cesarean delivery and massive blood transfusion; and second, administrative data do not reliably capture whether a woman labored before cesarean delivery or the level of urgency of cesarean delivery, so meaningful comparisons are not possible. Fifth, the Healthcare Cost and Utilization Project State Inpatient Dataset for New York collects the total number of units of blood (whether packed red blood cells or whole blood) but does not collect the number of units of other blood products transfused. So it was not possible to explore the effect of transfusion ratios among plasma, platelets, and packed red blood cells on outcomes for women receiving massive blood transfusion in this data. Sixth, relevant clinical variables are not captured in this data set, including obesity, prior postpartum hemorrhage, and neonatal birth weight. Finally, as a result of the cross-sectional nature of our data, we can only examine associations between massive blood transfusion and selected characteristics and cannot draw inferences about causal relationships. For example, both massive blood transfusion and severe obstetric morbidities likely both represent the consequences of massive maternal hemorrhage. Because the actual blood lost is unknown, the contribution of transfusion toward the development of maternal end-organ injury is impossible to quantify. Nevertheless, the strong association observed suggests that patients receiving massive blood transfusion are a very high-risk group.
Massive transfusions continue to haunt even the smallest delivery centers; multidisciplinary protocols for comprehensive hemorrhage management are central to the safe practice of modern obstetrics, regardless of the facility size or population served.
Supplementary Material
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Presented at the Society of Obstetric Anesthesia and Perinatology meeting, May 2–5, 2012, Monterey, California.
Financial Disclosure
The authors did not report any potential conflicts of interest.
REFERENCES
- 1.Sharpe JP, Weinberg JA, Magnotti LJ, Croce MA, Fabian TC. Toward a better definition of massive transfusion: focus on the interval of hemorrhage control. J Trauma Acute Care Surg. 2012;73:1553–7. doi: 10.1097/TA.0b013e3182660119. [DOI] [PubMed] [Google Scholar]
- 2.Mitra B, Cameron PA, Gruen RL, Mori A, Fitzgerald M, Street A. The definition of massive transfusion in trauma: a critical variable in examining evidence for resuscitation. Eur J Emerg Med. 2011;18:137–42. doi: 10.1097/MEJ.0b013e328342310e. [DOI] [PubMed] [Google Scholar]
- 3.Skupski DW, Lowenwirt IP, Weinbaum FI, Brodsky D, Danek M, Eglinton GS. Improving hospital systems for the care of women with major obstetric hemorrhage. Obstet Gynecol. 2006;107:977–83. doi: 10.1097/01.AOG.0000215561.68257.c5. [DOI] [PubMed] [Google Scholar]
- 4.Shields LE, Smalarz K, Reffigee L, Mugg S, Burdumy TJ, Propst M. Comprehensive maternal hemorrhage protocols improve patient safety and reduce utilization of blood products. Am J Obstet Gynecol. 2011;205:368, e1–8. doi: 10.1016/j.ajog.2011.06.084. [DOI] [PubMed] [Google Scholar]
- 5.Eller AG, Bennett MA, Sharshiner M, Masheter C, Soisson AP, Dodson M, et al. Maternal morbidity in cases of placenta accreta managed by a multidisciplinary care team compared with standard obstetric care. Obstet Gynecol. 2011;117:331–7. doi: 10.1097/AOG.0b013e3182051db2. [DOI] [PubMed] [Google Scholar]
- 6.Wright JD, Herzog TJ, Shah M, Bonanno C, Lewin SN, Cleary K, et al. Regionalization of care for obstetric hemorrhage and its effect on maternal mortality. Obstet Gynecol. 2010;115:1194–200. doi: 10.1097/AOG.0b013e3181df94e8. [DOI] [PubMed] [Google Scholar]
- 7.Mhyre JM, Bateman BT, Leffert LR. Influence of patient comorbidities on the risk of near-miss maternal morbidity or mortality. Anesthesiology. 2011;115:963–72. doi: 10.1097/ALN.0b013e318233042d. [DOI] [PubMed] [Google Scholar]
- 8.Bateman BT, Berman MF, Riley LE, Leffert LR. The epidemiology of postpartum hemorrhage in a large, nationwide sample of deliveries. Anesth Analg. 2010;110:1368–73. doi: 10.1213/ANE.0b013e3181d74898. [DOI] [PubMed] [Google Scholar]
- 9.Callaghan WM, Kuklina EV, Berg CJ. Trends in postpartum hemorrhage: United States, 1994–2006. Am J Obstet Gynecol. 2010;202:353, e1–6. doi: 10.1016/j.ajog.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 10.Knight M, Callaghan WM, Berg C, Alexander S, Bouvier-Colle MH, Ford JB, et al. Trends in postpartum hemorrhage in high resource countries: a review and recommendations from the International Postpartum Hemorrhage Collaborative Group. BMC Pregnancy Childbirth. 2009;9:55. doi: 10.1186/1471-2393-9-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.New York State Department of Health Statewide Planning and Research Cooperative System (SPARCS) Available at: http://www.health.ny.gov/statistics/sparcs/. Retrieved September 14, 2013.
- 12.Centers for Disease Control and Prevention International classification of diseases, 9th revision, clinical modification (ICD-9-CM) Available at: http://www.cdc.gov/nchs/icd/icd9cm.htm. Retrieved September 13, 2013.
- 13.Kuklina EV, Whiteman MK, Hillis SD, Jamieson DJ, Meikle SF, Posner SF, et al. An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Matern Child Health J. 2008;12:469–77. doi: 10.1007/s10995-007-0256-6. [DOI] [PubMed] [Google Scholar]
- 14.Bateman BT, Mhyre JM, Callaghan WM, Kuklina EV. Peripartum hysterectomy in the United States: nationwide 14 year experience. Am J Obstet Gynecol. 2012;206:63, e1–8. doi: 10.1016/j.ajog.2011.07.030. [DOI] [PubMed] [Google Scholar]
- 15.Kuklina EV, Meikle SF, Jamieson DJ, Whiteman MK, Barfield WD, Hillis SD, et al. Severe obstetric morbidity in the United States: 1998–2005. Obstet Gynecol. 2009;113:293–9. doi: 10.1097/AOG.0b013e3181954e5b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Young PP, Cotton BA, Goodnough LT. Massive transfusion protocols for patients with substantial hemorrhage. Transfus Med Rev. 2011;25:293–303. doi: 10.1016/j.tmrv.2011.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.California Maternal Quality Care Collaborative (CMQCC) Ob hemorrhage Toolkit. Available at: http://www.cmqcc.org/ob_hemorrhage. Retrieved September 13, 2013.
- 18.Wu S, Kocherginsky M, Hibbard JU. Abnormal placentation: twenty-year analysis. Am J Obstet Gynecol. 2005;192:1458–61. doi: 10.1016/j.ajog.2004.12.074. [DOI] [PubMed] [Google Scholar]
- 19.Balayla J, Bondarenko HD. Placenta accreta and the risk of adverse maternal and neonatal outcomes. J Perinat Med. 2013;41:141–9. doi: 10.1515/jpm-2012-0219. [DOI] [PubMed] [Google Scholar]
- 20.Faiz AS, Ananth CV. Etiology and risk factors for placenta previa: an overview and meta-analysis of observational studies. J Matern Fetal Neonatal Med. 2003;13:175–90. doi: 10.1080/jmf.13.3.175.190. [DOI] [PubMed] [Google Scholar]
- 21.Roberts CL, Algert CS, Warrendorf J, Olive EC, Morris JM, Ford JB. Trends and recurrence of placenta praevia: a population-based study. Aust N Z J Obstet Gynaecol. 2012;52:483–6. doi: 10.1111/j.1479-828X.2012.01470.x. [DOI] [PubMed] [Google Scholar]
- 22.Cheung WM, Hawkes A, Ibish S, Weeks AD. The retained placenta: historical and geographical rate variations. J Obstet Gynaecol. 2011;31:37–42. doi: 10.3109/01443615.2010.531301. [DOI] [PubMed] [Google Scholar]
- 23.Rogers J, Wood J, McCandlish R, Ayers S, Truesdale A, Elbourne D. Active versus expectant management of third stage of labour: the Hinchingbrooke randomised controlled trial. Lancet. 1998;351:693–9. doi: 10.1016/S0140-6736(97)09409-9. [DOI] [PubMed] [Google Scholar]
- 24.Stotler B, Padmanabhan A, Devine P, Wright J, Spitalnik SL, Schwartz J. Transfusion requirements in obstetric patients with placenta accreta. Transfusion. 2011;51:2627–33. doi: 10.1111/j.1537-2995.2011.03205.x. [DOI] [PubMed] [Google Scholar]
- 25.Hankins GD, Clark SL, Pacheco LD, O’Keeffe D, D’Alton M, Saade GR. Maternal mortality, near misses, and severe morbidity: lowering rates through designated levels of maternity care. Obstet Gynecol. 2012;120:929–34. doi: 10.1097/AOG.0b013e31826af878. [DOI] [PubMed] [Google Scholar]
- 26.Kyser KL, Lu X, Santillan DA, Santillan MK, Hunter SK, Cahill AG, et al. The association between hospital obstetrical volume and maternal postpartum complications. Am J Obstet Gynecol. 2012;207:42, e1–17. doi: 10.1016/j.ajog.2012.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.