Abstract
Objective
The U.S. water fluoridation recommendations, which have been in place since 1962, were based in part on findings from the 1950s that children's water intake increased with outdoor temperature. We examined whether or not water intake is associated with outdoor temperature.
Methods
Using linked data from the National Health and Nutrition Examination Survey (NHANES) 1999–2004 and the National Oceanic and Atmospheric Administration, we examined reported 24-hour total and plain water intake in milliliters per kilogram of body weight per day of children aged 1–10 years by maximum outdoor temperature on the day of reported water intake, unadjusted and adjusted for age, sex, race/ethnicity, and poverty status. We applied linear regression methods that were used in previously reported analyses of data from NHANES 1988–1994 and from the 1950s.
Results
We found that total water intake was not associated with temperature. Plain water intake was weakly associated with temperature in unadjusted (coefficient 5 0.2, p=0.015) and adjusted (coefficient 5 0.2, p=0.013) linear regression models. However, these models explained little of the individual variation in plain water intake (unadjusted: R2=0.005; adjusted: R2=0.023).
Conclusion
Optimal fluoride concentration in drinking water to prevent caries need not be based on outdoor temperature, given the lack of association between total water intake and outdoor temperature, the weak association between plain water intake and outdoor temperature, and the minimal amount of individual variance in plain water intake explained by outdoor temperature. These findings support the change in the U.S. Public Health Service recommendation for fluoride concentration in drinking water for the prevention of dental caries from temperature-related concentrations to a single concentration that is not related to outdoor temperature.
In 2015, the U.S. Department of Health and Human Services (HHS) changed the recommended concentration for fluoride in drinking water to prevent dental caries to 0.7 milligrams per liter (mg/L) of drinking water,1 to replace the recommendations from 1962,2 which ranged from 0.7 mg/L for areas with average daily maximum temperatures in degrees Fahrenheit (°F) of 79.3°F–90.5°F through 1.2 mg/L for areas with temperatures of 50.0°F–53.7°F. One reason for the change was that the correlation between temperature and children's water intake found in the 1950s3–7 was not evident from studies of data collected in more recent decades.8–10
The 1962 recommendations included a range of fluoride concentrations because studies conducted during the 1950s found that children drank more water on warmer than on colder days.3–6 Galagan et al.6 collected data on water intake among children aged #10 years in two communities in Contra Costa County, California. Each participant contributed data for five consecutive weekdays (Monday–Friday) during the course of a year. The study found positive correlations between temperature and both total and drinking water intake, and negative correlations between temperature and intake of milk, carbonated beverages, and non-water-based beverages. By fitting a regression line to the mean values for water intake and daily maximum temperature (from U.S. Weather Bureau stations) for each of 39 weekly reporting periods, Galagan et al.6 found a direct association between water intake and temperature and developed the following estimation equation: ounces of water per pound of body weight = −0.038 + 0.0062 temperature. Galagan and Vermillion7 used this estimating equation to develop a table of optimum fluoride concentrations for six ranges of the daily maximum temperature averaged during at least a five-year period; the 1962 recommendations2 used this table.
More recent studies using nationally representative data did not find consistent associations between water intake and season, month, or monthly average for daily maximum temperature among regions of the United States.8–11 Two studies attributed their findings' lack of congruence with those from the 1950s to changes such as wider use of air-conditioning and lower levels of outdoor physical activity.9,10 Our previous unadjusted analysis of 1999–2004 National Health and Nutrition Examination Survey (NHANES) data did not find an association between total water intake and outdoor temperature among children aged 1–10 years.12
We used data from NHANES 1999–2004 to reexamine the relationship between water intake and outdoor temperature among children aged 1–10 years and consider the appropriateness of a recommendation for a single fluoride concentration in drinking water across the United States to prevent dental caries.
METHODS
NHANES data
We obtained public release data from the National Center for Health Statistics (NCHS) website for water intake (total and plain) from the NHANES 1999–2004 24-hour dietary interview and body measures examination, which were conducted at mobile examination centers (MECs).13 We used the NHANES definitions and variables for total and plain water intake for the first day of the dietary interview because public use data for the second day interview were not available for 1999–2002. Total water included plain water (i.e., tap water and noncarbonated bottled water), water from or mixed with other beverages (e.g., juice, soda, sports drinks, and dairy and nondairy milk), and water from or mixed with foods. We reported total and plain water intake in milliliters per kilogram of body weight per day (ml/kg/day). A parent or caregiver reported intake for children too young or otherwise unable to report for themselves, and may have assisted older children. The dietary interview and NHANES are described elsewhere.13–16
We used the NHANES public use demographic data for the participant's age, sex, race/ethnicity (i.e., non-Hispanic white, non-Hispanic black, Mexican American, and other), and poverty status (i.e., low income #130% federal poverty level [FPL], middle income 131%–350% FPL, and high income $351% FPL).13 For poverty status, the threshold is based on the number of people in the household and state of residence and is revised each year.14,17 Participants, or their parents or caregivers, reported their race/ethnicity using multiple-response questions. To compare our findings with a previous study,9 we restricted the analysis to children aged 1–10 years and used the NHANES III recoded race/ethnicity variable.13
National Weather Service data
We used the National Oceanic and Atmospheric Administration (NOAA) National Climatic Data Center dataset, National Weather Service Surface Land Daily Cooperative Summary of the Day, from which the daily maximum temperature was available from approximately 5,200 weather stations for each day during 1999–2005.18 (Some NHANES 2004 survey participants reported dietary intake for dates early in 2005.) We used data from 4,753 stations with data for daily maximum temperature. We averaged -temperature values from weather stations located within each county.19 The term “temperature” in this article refers to the daily maximum outdoor air temperature in °F. We did not use the Celsius scale because the 1962 fluoridation recommendations stated temperature ranges in Fahrenheit.2
Data linkage
NCHS Research Data Center staff merged the water intake and temperature datasets by restricted variables for NHANES participants' county of residence and date of reported dietary intake.
Analysis
Analyses included children of all racial/ethnic groups with complete data for water intake, temperature on the day of dietary intake, and body weight. Multiple regression models were limited to children who also had complete data for age, sex, race/ethnicity, and poverty status.
Children with total water intake beyond six standard deviations of the mean for their year of age were excluded for two reasons: (1) because the water intake for these children may be unreliable and (2) to support comparisons with a previous study9 that applied the same exclusion. Children who were breastfed were excluded because data on water intake from breastfeeding were not available. Children who lacked data for body weight were excluded because body weight was necessary to calculate the outcome measures of total and plain water intake in ml/kg of body weight per day. Children who lacked data for outdoor temperature on the day of water intake were excluded because the primary aim of this study was to assess the association of outdoor temperature with water intake.
We used the t-test to assess differences between the total and included survey participants, and between the included and excluded survey participants, for water intake, age, sex, race/ethnicity, and poverty status. We assessed whether or not exclusion was independent of sex, race/ethnicity, and poverty status using the chi-square test.20
We examined total and plain water intakes by age, sex, race/ethnicity, and poverty status. We used the t-test to assess differences in mean water intake between groups, and the Satterthwaite adjusted F-test21 to assess unadjusted associations between water intake and each categorical variable.
We used Pearson's correlation coefficient to assess the correlation between water intake and continuous variables (i.e., age and temperature), Spearman's Rank Order correlation coefficient to assess the correlation between water intake and poverty status,22 and -Hoeffding's D to assess departures from independence of water intake by sex and race/ethnicity.23
We fitted unadjusted linear regression models with total and plain water intake as response variables and temperature as the variable of interest. Adjusted models also included age, sex, race/ethnicity, and poverty status. We assessed the interaction between temperature and each of the other variables in the model. We assessed multicollinearity using condition indices and variance inflation factors. In these models, we used the t-test to assess whether or not model coefficients differed from 0 and the Satterthwaite corrections for the F-statistic to test the association between water intake and temperature.20,21
Using the analysis approach of Galagan et al.,6 we plotted and fit regression lines for mean total and plain water intake (in ml/kg/day) by temperature for 1999–2004. We plotted mean water intake only for temperatures with sufficient data to preserve anonymity.
We used SAS® release 9.3.224 for data management and SAS-callable SUDAAN® release 11.0.125 for statistical analyses. All analyses used the restricted variables for true strata and primary sampling unit to account for the clustered sample design, and survey weights provided by NCHS to account for unequal probabilities of selection. We computed standard errors (SEs) for means of continuous variables and percentages of categorical variables using the Taylor series expansion and 95% confidence intervals (CIs) using these SEs and the t-distribution with subgroup-specific degrees of freedom. Only statistically significant results (p≤0.05) are described, unless otherwise stated.
RESULTS
Of the 31,126 participants in NHANES 1999–2004, 6,498 were aged 1–10 years at the time of the interview; 5,545 were not breastfeeding and completed the dietary interview. Of the 5,545 respondents who completed the dietary interview, five were excluded for having reported total water intake values beyond six standard deviations of the mean for their year of age, 187 lacked data for body weight, and 901 lacked data for outdoor temperature on the day of water intake. The remaining 4,453 participants were included in descriptive analyses. Multiple regression analyses were restricted to 4,104 participants with complete data for variables used in the regression models (data not shown).
For included children, the mean total water intake was 78.4 ml/kg/day (95% CI 76.3, 80.5); mean plain water intake was 19.0 ml/kg/day (95% CI 17.6, 20.4). The excluded group was on average older than the included group (mean age 5 6.1 vs. 5.5 years, p=0.008). Sex (p=0.458), race/ethnicity (p=0.284), and poverty status (p=0.461) were not associated with exclusion overall (chi-square test); however, the excluded group had proportionately fewer Mexican American survey participants than the included group (t-test, p=0.012) (Table 1).
Table 1.
Total and plain water intake and selected characteristics of children aged 1–10 years with valid water intake data from the NHANES 24-hour dietary interviews:a United States, 1999–2004
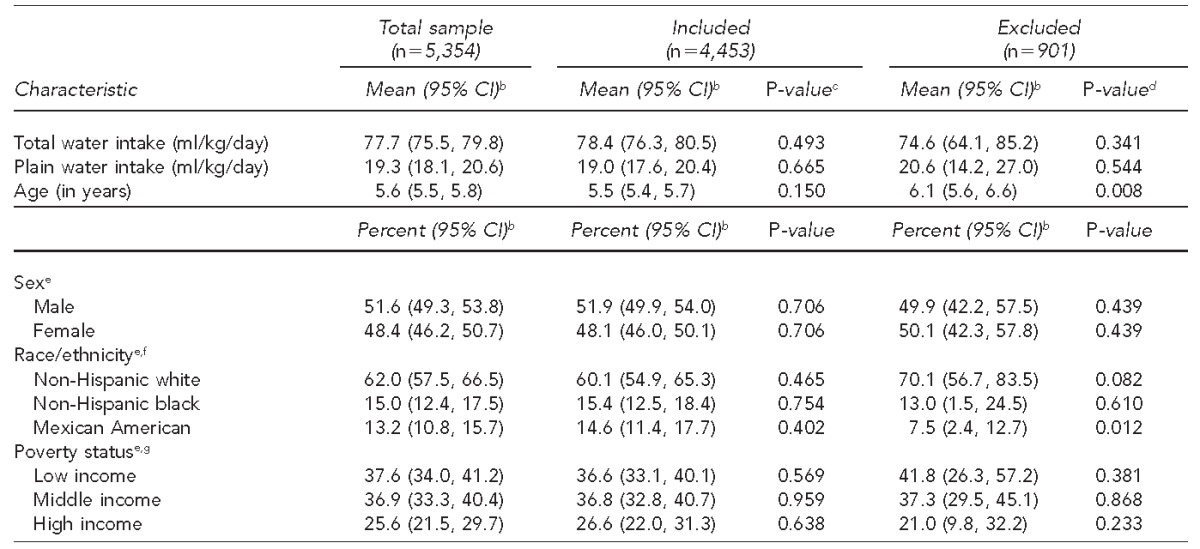
Included participants were children aged 1–10 years who completed the dietary interview, were not breastfed, had total water intake of <6 standard deviations of mean for age, had valid data for body weight, and had survey weights >0. Excluded participants were children aged 1–10 years who were excluded for the following reasons: they had total water intake ≥6 standard deviations of the mean for their year of age, were breastfed, lacked data for body weight, or lacked data for outdoor temperature on the day of water intake.
bCalculated from the t-distribution using subgroup-specific degrees of freedom.
cT-test for difference in means or proportions between the total sample and the included survey participants
dT-test for difference in means or proportions between the included and excluded survey participants
eP-values from chi-squared tests of independence of exclusion from sex (p=0.458), race/ethnicity (p=0.284), and poverty status (p=0.461)
fMultiracial participants and participants of other races or Hispanic ethnicity other than Mexican American were included in the analyses. However, estimates for these groups were not reported because NHANES 1999–2004 was not designed to support estimates for these groups.
gBased on the ratio of family income to the U.S. Department of Health and Human Services poverty threshold. Low income is ≤130% of the federal poverty level (FPL), middle income is 131%–350% FPL, and high income is ≥351% FPL. The threshold is based on the number of people in the household and the state of residence, and is revised each year.
NHANES = National Health and Nutrition Examination Survey
CI = confidence interval
In unadjusted analyses (Table 2), total water intake varied by age (p<0.001), race/ethnicity (p=0.012), and poverty status (p=0.001), while plain water intake varied by age (p<0.001). Total and plain water intake decreased with age (p<0.001). Mexican American children had higher total water intake (mean 5 82.3 ml/kg/day, 95% CI 78.8, 85.8) than non-Hispanic white (mean 5 77.3 ml/kg/day, 95% CI 74.1, 80.4, p=0.027) and non-Hispanic black (75.0 ml/kg/day, 95% CI 72.1, 78.0, p=0.005) children. Low-income children had higher total water intake (mean 5 84.0 ml/kg/day, 95% CI 79.8, 88.1) than their higher-income -counterparts (middle income: mean = 74.7 ml/kg/day, 95% CI 70.8, 78.5, p=0.003; high income: mean = 75.2 ml/kg/day, 95% CI 72.0, 78.4, p<0.001).
Table 2.
Mean total and plain water intake by selected characteristics among children aged 1–10 yearsa: United States, 1999–2004
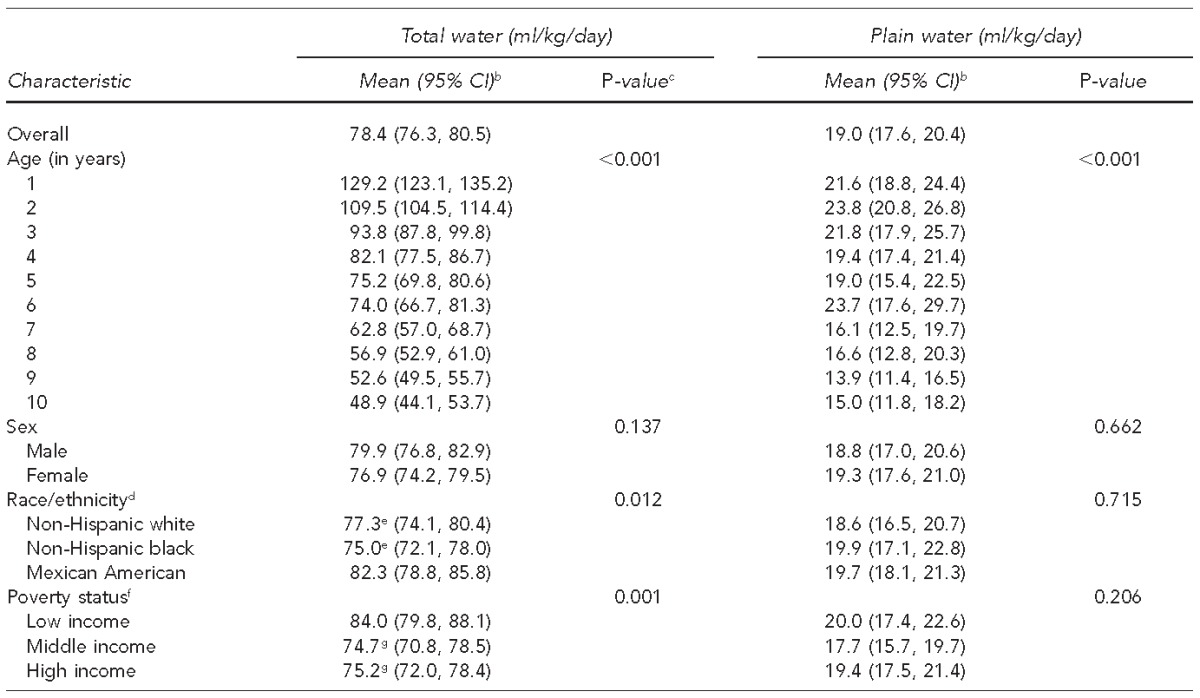
Children aged 1–10 years on date of National Health and Nutrition Examination Survey (NHANES) examination who completed the 24-hour dietary interview; were not breastfed; had total water intake <6 standard deviations of mean for year of age, valid data for body weight, and outdoor temperature in county of residence on date of dietary intake; and had survey weights >0.
bCalculated from the t-distribution using subgroup-specific degrees of freedom
cp-values from Satterthwaite adjusted F-test from unadjusted linear regression models
dMultiracial participants and participants of other races or Hispanic ethnicity other than Mexican American were included in the analyses. However, estimates for these groups were not reported because NHANES 1999–2004 was not designed to support estimates for these groups.
eStatistically significant difference (t-test) in mean total water intake between Mexican American children and non-Hispanic white (p=0.027) and non-Hispanic black (p=0.005) children
fBased on the ratio of family income to the U.S. Department of Health and Human Services poverty threshold. Low income is ≤130% of the federal poverty level (FPL), middle income is 131%–350% FPL, and high income is ≥351% FPL. The threshold is based on the number of people in the household and the state of residence, and is revised each year.
gStatistically significant difference (t-test) in mean total water intake between low-income children and middle-income (p=0.003) and high-income (p<0.001) children
ml/kg = milliliters per kilogram
CI = confidence interval
Linear regression models for total and plain water intake used water intake values at the individual level (Table 3). Interaction terms did not improve the models, so we only present main effects models. Correlations and multicollinearity were low among the variables included in the model. Temperature was associated with plain water intake in both unadjusted (coefficient 5 0.2, p=0.015) and adjusted (coefficient = 0.2, p=0.013) models. In adjusted models, age was inversely associated with total (coefficient 5 28.2, p<0.001) and plain (coefficient = 20.9, p<0.001) water intake. Poverty status was associated with total water intake (p=0.017). The adjusted models explained about 30% of the variation in total water intake (R2=0.311) but only about 2% of the variation in plain water intake (R2=0.023).
Table 3.
Linear regression models of total and plain water intake among children aged 1–10 years,a by daily maximum outdoor temperature in county of residence: United States, 1999–2004
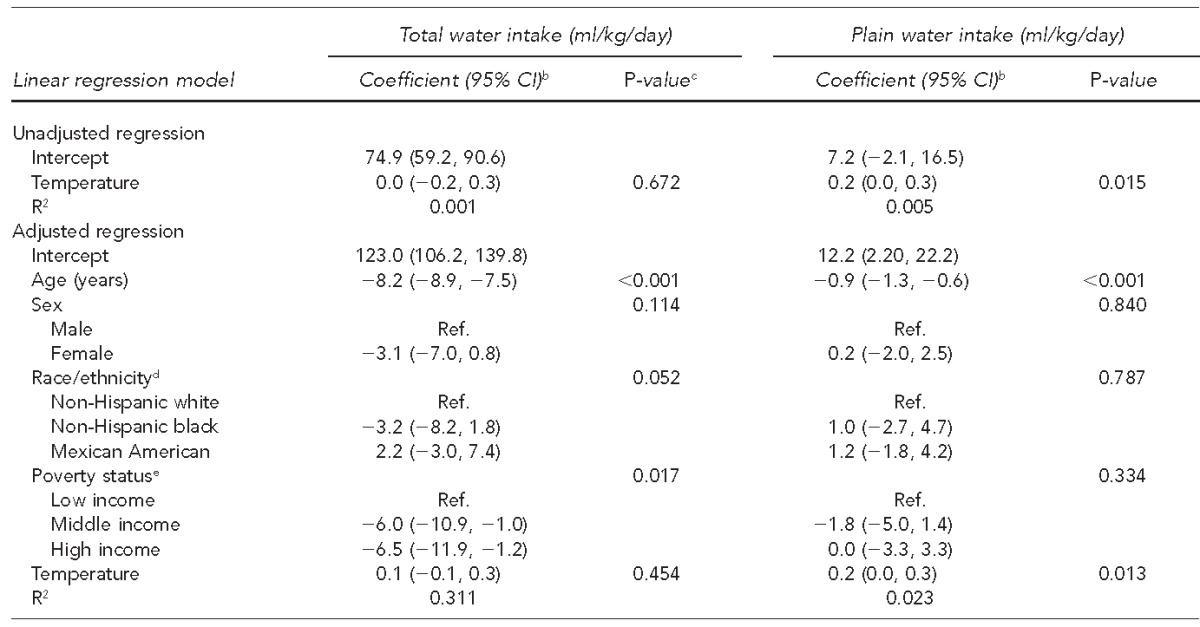
Children aged 1–10 years on date of National Health and Nutrition Examination Survey (NHANES) examination who completed the 24-hour dietary interview; were not breastfed; had total water intake <6 standard deviations of mean for year of age, valid data for body weight, outdoor temperature in county of residence on date of dietary intake, age, sex, race/ethnicity, and poverty status; and had survey weights >0.
bCalculated from the t-distribution using subgroup-specific degrees of freedom
cSatterthwaite adjusted F-test of association between variable and water intake
dMultiracial participants and participants of other races or Hispanic ethnicity other than Mexican American were included in the analyses; however, NHANES 1999–2004 cannot support estimates for these groups.
eBased on the ratio of family income to the U.S. Department of Health and Human Services poverty threshold. Low income is ≤130% of the federal poverty level (FPL), middle income is 131%–350% FPL, and high income is ≥351% FPL. The threshold is based on the number of people in the household and the state of residence, and is revised each year.
ml/kg = milliliters per kilogram
CI = confidence interval
Ref. = reference group
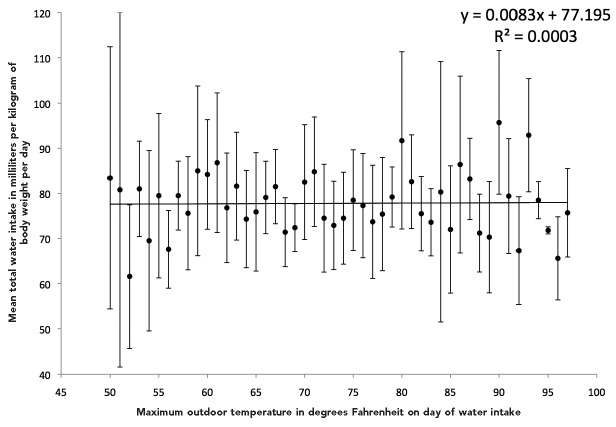
Using the analysis approach of Galagan et al.,6 temperature was not associated with total (Figure 1) or plain (Figure 2) water intake for days with maximum outdoor temperatures of 50°F–97°F.
Figure 1.
Mean total water intake among children aged 1–10 years by maximum outdoor temperature on day of reported water intake: United States, 1999–2004a,b
aA linear regression line through the points can be described by the equation y 5 77.195 1 0.0083x, where y is total water intake and x is temperature. The R-squared value is 0.0003. The p-value for the coefficient for temperature is p=0.91, indicating that outdoor temperature may not be associated with total water intake.
bChildren aged 1–10 years on date of the National Health and Nutrition Examination Survey examination with data for outdoor temperature in county of residence and water intake data from the 24-hour dietary interview
Figure 2.
Mean plain water intake among children aged 1–10 years by maximum outdoor temperature on day of reported water intake: United States, 1999–2004a,b
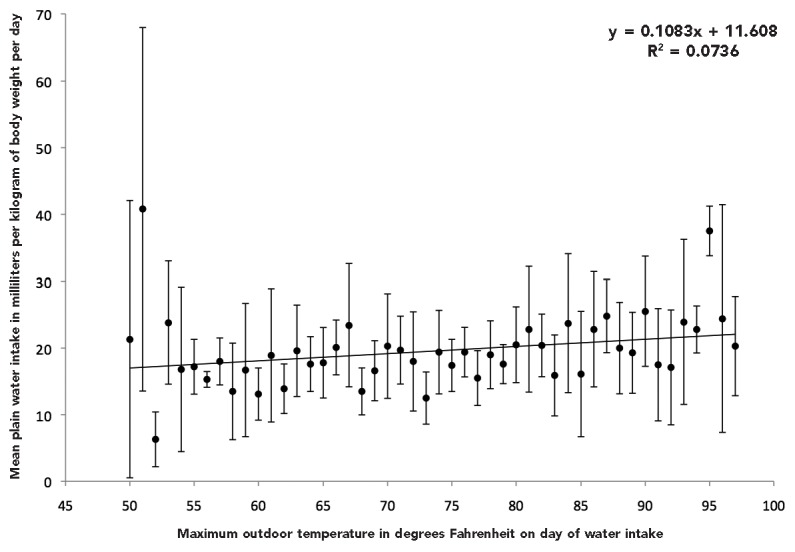
aA linear regression line through the points can be described by the equation y 5 11.608 + 0.1083x, where y is total water intake and x is temperature. The R-squared value is 0.0736. The p-value for the coefficient for temperature is p=0.06. On days with high temperatures <54°F or >94°F, a few points for mean plain water intake are further from the regression line than the points for mean plain water intake on days with high temperatures from 54°F–94°F. Together, this information suggests that outdoor temperature explains little of the variability in plain water intake.
bChildren aged 1–10 years on date of the National Health and Nutrition Examination Survey examination with data for outdoor temperature in county of residence and water intake data from the 24-hour dietary interview
DISCUSSION
Our adjusted regression model, which included outdoor temperature as an explanatory factor, explained only about 2% of the variance in plain water intake, far less than the 40% found in the 1950s studies on which the 1962 recommendations were based.6,9 From our model, for each 1°F increase in outdoor temperature, plain water consumption among children aged 1–10 years increased an estimated 0.2 ml/kg/day; thus, the expected difference in plain water intake between days with maximum outdoor temperatures of 60°F and 90°F (i.e., a 30°F difference) would be 6.0 ml/kg/day. No association was found between temperature and total water intake, before or after adjusting for age, sex, race/ethnicity, or poverty status.
The analysis approach of Galagan et al.6 may have underestimated the variance of, and overestimated the correlation between, these two variables. Consequently, the amount of variance in water intake explained by temperature (R2=0.40) may have been overestimated.26 Although our adjusted model explained about 30% of the variance in total water intake, in our unadjusted individual and mean regression models, temperature explained little of the variance in total water intake. Although the mean regression model explained about 7% of the variance in plain water intake, regression models with individual intake explained at most about 2% of the variance in plain water intake.
Based on descriptive analyses of the 1994–1996 Continuing Survey of Food Intakes by Individuals, from the U.S. Department of Agriculture, Heller et al.10 found no apparent trend in water intake from colder to warmer months, but did not have the information needed to link outdoor temperature to water intake. Water intake among children aged #10 years fluctuated greatly throughout the year in the West,10 where water intake may be more similar to that in the two California communities in the study by Galagan et al.6 Our study included participants from all regions of the United States, as did Sohn and colleagues9 and Heller et al.;10 thus, it may better represent variation in water intake for the United States than did the study by Galagan et al.6
Heller et al.10 defined water intake similarly to -Galagan et al.6 (i.e., drinking water, infant formula, soups, and home-prepared beverages) and averaged two days of water intake, instead of five as Galagan et al.6 did. Sohn and colleagues9 and our study defined water intake as total and plain water intake in one 24-hour period (midnight to midnight). The definitions used by Heller et al.10 and Galagan et al.6 fall between the definitions we used for total and plain water intake. Data for a second day of water intake, which can be used to calculate usual water intake,15 were not available in NHANES 1999–2002.15,16
We found that plain water intake was about 25% of the total water intake, consistent with previous studies.6–11 We found unadjusted associations between total water intake (ml/kg/day) and age, race/ethnicity, and poverty status. In contrast with a study that used NHANES data from 2005–2006 for children aged 2–19 years,11 we did not find an association with sex. However, the adequate intake of water established by the National Research Council using data from NHANES III (1988–1994) differs by sex only for children and adolescents aged $9 years.27 Different age ranges of these studies may explain the contrasting findings.
Water intake from tap or bottled water or from drinks or juices prepared with water may be influenced by the availability of water from water fountains or vending machines at school, by family preferences,28–31 and by cultural and social values. Although studies have found a preference among Latino and Hispanic families for bottled water,28–31 this preference may not modify the relationship or lack thereof between water intake and outdoor temperature. The differences may be due in part to differences in the validity and -reliability of the dietary interview by race/ethnicity.32–34 However, the NHANES dietary interview was offered in both English and Spanish and included Hispanic dietary items.15,16 To the extent that income is correlated with parent or caregiver -education level, or the portion of the day spent at preschool or day care, it is possible that the dietary interview may have lower validity and reliability in lower-income groups.
Strengths
Our study exhibited several important strengths. Its analysis methods for assessing the effect of outdoor temperature on total water intake were consistent with earlier studies.9,10 Results also were similar despite different time periods and sample characteristics. Data analyzed in our study were collected using rigorous methods to measure water intake15,16 and better represent the water intake of the U.S. population as a whole, as well as contemporary lifestyle and environmental conditions, than data6 used to establish the USPHS 1962 recommendations.2 Our linear regression models better accounted for individual variation in water intake and other potential confounders or explanatory factors than the study6 used to establish the 1962 recommendations.2 Most importantly, we examined the relationship between reported 24-hour water intake and maximum outdoor temperature on the same day to improve our chances of detecting a relationship between water intake and temperature, if it existed. To our knowledge, ours is the first study to examine water intake and temperature from the same day using a nationally representative dataset.
Limitations
This study was also subject to several limitations. NHANES data used were not collected to test the hypothesis of an association between outdoor temperature and water intake. Outdoor temperatures measured at the county level may not reflect the true outdoor temperature at home or school during the day of water intake.35 Additionally, outdoor temperatures may not reflect the temperatures to which participants were exposed, because portions of the day were likely spent indoors. Logistics of the NHANES MECs limited the range of temperatures under which water intake could be measured, because examinations were primarily conducted in the coldest areas of the country only in the summer, while the hottest areas of the country were avoided in the summer.14 Outdoor temperature could be capturing the effect of other variables influencing water intake in children that were not included in the model, such as humidity, season, geographic region of residence, physical activity, availability of tap water, and individual response to the physiological need for water.
Additionally, the 24-hour dietary interview may not represent a typical dietary day, the preceding day's intake may not have been remembered or reported accurately, and parents or caregivers reporting on behalf of the child may not have observed the child's intake for portions of the day spent at school or day care.11,13,34 NHANES data, however, have been used -routinely to describe nutritional and meal patterns, as well as body weight effects among varying age cohorts.11,27 For example, the adequate intakes for total water were established using data from NHANES III (1988–1994).27 Although NHANES included data on other relevant variables, such as television and computer use, which may reduce time spent in physical activity or playing outdoors,36 they were not available for the full age range used in this analysis. More recent data on water intake are available from NHANES; however, the 1999–2004 time period was the most recent available dataset with sufficient sample size and comparable dietary interview protocol for the 1- to 10-year age group at the time review of the fluoridation recommendations began in 2007.
CONCLUSION
Optimal fluoride concentrations need not be based on outdoor temperature given the lack of association between total water intake and outdoor temperature, the weak association between plain water intake and outdoor temperature, and the minimal amount of individual variance in plain water intake explained by outdoor temperature. These findings support the change in the USPHS recommendation for fluoride concentration in drinking water to prevent dental caries from temperature-related concentrations to a single concentration that is not related to outdoor temperature.1
Footnotes
Analyses of the linked datasets were conducted within National Center for Health Statistics (NCHS) Research Data Center (RDC) facilities. Data collection for the National Health and Nutrition Examination Survey (NHANES) was approved by the NCHS Ethics Review Board (ERB). Analysis of de-identified data from the survey is exempt from federal regulations for the protection of human research participants. Analysis of restricted data through the NCHS RDC is also approved by the NCHS ERB.
Dr. Sohn's work was supported in part by an ORISE joint research fellowship from Oak Ridge Associated Universities.
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of RDC, NCHS, or the Centers for Disease Control and Prevention.
REFERENCES
- 1.Department of Health and Human Services (US), Federal Panel on Community Water Fluoridation. U.S. Public Health Service recommendation for fluoride concentration in drinking water for the prevention of dental caries. Public Health Rep. 2015;130:318–31. doi: 10.1177/003335491513000408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Public Health Service (US) Washington: Government Printing Office (US); 1962. Public Health Service drinking water standards 1962. Publication No. 956. [Google Scholar]
- 3.Levin MM, Cox GJ. Water consumption in relation to environmental temperature and its significance in the fluoridation of water supplies. J Dent Res. 1950;29:663. [Google Scholar]
- 4.Galagan DJ, Lamson GG., Jr Climate and endemic dental fluorosis. Public Health Rep. 1953;68:497–508. [PMC free article] [PubMed] [Google Scholar]
- 5.Stadt ZM. Résumé of dental benefits of fluoride ingestion. In: Shaw JH, editor. Fluoridation as a public health measure. Washington: American Association for the Advancement of Science; 1954. pp. 1–35. [Google Scholar]
- 6.Galagan DJ, Vermillion JR, Nevitt GA, Stadt ZM, Dart RE. Climate and fluid intake. Public Health Rep. 1957;72:484–90. [PMC free article] [PubMed] [Google Scholar]
- 7.Galagan DJ, Vermillion JR. Determining optimum fluoride concentrations. Public Health Rep. 1957;72:491–3. [PMC free article] [PubMed] [Google Scholar]
- 8.Ershow AG, Cantor KP. Total water and tapwater intake in the United States: population-based estimates of quantities and sources. Bethesda (MD): National Cancer Institute; 1989. [PubMed] [Google Scholar]
- 9.Sohn W, Heller KE, Burt BA. Fluid consumption related to climate among children in the United States. J Public Health Dent. 2001;61:99–106. doi: 10.1111/j.1752-7325.2001.tb03373.x. [DOI] [PubMed] [Google Scholar]
- 10.Heller KE, Sohn W, Burt BA, Eklund SA. Water consumption in the United States in 1994–96 and implications for water fluoridation policy [published erratum appears in J Public Health Dent 2000;60:4] J Public Health Dent. 1999;59:3–11. doi: 10.1111/j.1752-7325.1999.tb03228.x. [DOI] [PubMed] [Google Scholar]
- 11.Kant AK, Graubard BI. Contributors of water intake in US children and adolescents: associations with dietary and meal characteristics—National Health and Nutrition Examination Survey 2005–2006. Am J Clin Nutr. 2010;92:887–96. doi: 10.3945/ajcn.2010.29708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beltrán-Aguilar ED, Barker L, Sohn W. Lack of association between daily temperature and children's water intake in the United States—1999–2004 [cited 2014 May 6] Available from: URL: http://www.cdc.gov/fluoridation/factsheets/totalwaterintake.htm.
- 13.Johnson CL, Paulose-Ram R, Ogden CL, Carroll MD, Kruszon-Moran D, Dohrmann SM, et al. National Health and Nutrition Examination Survey: analytic guidelines, 1999–2010. Vital Health Stat. 2013;2(161) [PubMed] [Google Scholar]
- 14.Curtin LR, Mohadjer LK, Dohrmann SM, Montaquila JM, Kruszon-Moran D, Mirel LB, et al. The National Health and Nutrition Examination Survey: sample design, 1999–2006. Vital Health Stat. 2012;2(155) [PubMed] [Google Scholar]
- 15.National Center for Health Statistics (US) National Health and Nutrition Examination Survey: MEC in-person dietary interviewers procedures manual. Hyattsville (MD): Department of Health and Human Services (US); 2002. Also available from: URL: http://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/dietary_mec.pdf [cited 2014 Dec 3] [Google Scholar]
- 16.National Center for Health Statistics (US) National Health and Nutrition Examination Survey: dietary interviewers procedures manual. Hyattsville (MD): Department of Health and Human Services (US); 1999. (revised January 2000). Also available from: URL: http://www.cdc.gov/nchs/data/nhanes/dr-1-5.pdf [cited 2014 Dec 3] [Google Scholar]
- 17.Department of Health and Human Services (US), Office of the Assistant Secretary for Planning and Evaluation. Poverty guidelines, research, and measurement [cited 2015 Feb 25] Available from: URL: http://aspe.hhs.gov/poverty/index.cfm.
- 18.National Oceanic and Atmospheric Administration, National Climatic Data Center. Data documentation for data set 3200 (DSI-3200): surface land daily cooperative summary of the day. Asheville (NC): NOAA; 2009. Also available from: URL: http://www1.ncdc.noaa.gov/pub/data/documentlibrary/tddoc/td3200.pdf [cited 2014 May 6] [Google Scholar]
- 19.Wei L, Barker L. Creating county-level estimates from National Weather Service data [cited 2014 May 6] Available from: URL: http://analytics.ncsu.edu/sesug/2008/st-142.pdf.
- 20.Rao JNK, Scott AJ. The analysis of categorical data from complex sample surveys: chi-squared tests for goodness of fit and independence in two-way tables. J Am Stat Assoc. 1981;76:221–30. [Google Scholar]
- 21.Satterthwaite FE. An approximate distribution of estimates of variance components. Biometrics. 1946;2:110–4. [PubMed] [Google Scholar]
- 22.Zar JH. Biostatistical analysis. 3rd ed. Upper Saddle River (NJ): Prentice Hall; 1996. [Google Scholar]
- 23.Hoeffding W. A non-parametric test of independence. Ann Math Stat. 1948;19:546–57. [Google Scholar]
- 24.SAS Institute, Inc. Cary (NC): SAS Institute, Inc.; 2012. SAS®: Release 9.3.2. [Google Scholar]
- 25.Research Triangle Institute. Research Triangle Park (NC): Research Triangle Institute; 2012. SUDAAN®: Release 11. [Google Scholar]
- 26.Mtz-Vara De Rey C, Galindo MPG, Arias Velarde MA. Effects of using mean scores in regression models: an example from environmental psychology. Qual Quan. 2001;35:191–202. [Google Scholar]
- 27.National Research Council. Dietary reference intakes for water, potassium, sodium, chloride, and sulfate. Washington: National Academies Press; 2005. [Google Scholar]
- 28.Hobson WL, Knochel ML, Byington CL, Young PC, Hoff CJ, Buchi KF. Bottled, filtered, and tap water use in Latino and non-Latino children. Arch Pediatr Adolesc Med. 2007;161:457–61. doi: 10.1001/archpedi.161.5.457. [DOI] [PubMed] [Google Scholar]
- 29.Gorelick MH, Gould L, Nimmer M, Wagner D, Heath M, Bashir H, et al. Perceptions about water and increased use of bottled water in minority children. Arch Pediatr Adolesc Med. 2011;165:928–32. doi: 10.1001/archpediatrics.2011.83. [DOI] [PubMed] [Google Scholar]
- 30.Park S, Sherry B, O'Toole T, Huang Y. Factors associated with low drinking water intake among adolescents: the Florida Youth Physical Activity and Nutrition Survey, 2007. J Am Diet Assoc. 2011;111:1211–7. doi: 10.1016/j.jada.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 31.Huerta-Saenz L, Irigoyen M, Benavides J, Mendoza M. Tap or bottled water: drinking preferences among urban minority children and adolescents. J Community Health. 2012;37:54–8. doi: 10.1007/s10900-011-9415-1. [DOI] [PubMed] [Google Scholar]
- 32.Kristal AR, Feng Z, Coates RJ, Oberman A, George V. Associations of race/ethnicity, education, and dietary intervention with the validity and reliability of a food frequency questionnaire: the Women's Health Trial Feasibility Study in Minority Populations [published erratum appears in Am J Epidemiol 1998;148:820] Am J Epidemiol. 1997;146:856–69. doi: 10.1093/oxfordjournals.aje.a009203. [DOI] [PubMed] [Google Scholar]
- 33.Fulgoni VL., III Limitations of data on fluid intake. J Am Coll Nutr. 2007;26(5 Suppl):588S–91S. doi: 10.1080/07315724.2007.10719663. [DOI] [PubMed] [Google Scholar]
- 34.National Cancer Institute (US) NCS dietary assessment literature review [cited 2014 Dec 3] Available from: URL: http://appliedresearch.cancer.gov/assess_wc/review.
- 35.Xiaopeng Q, Liang W, Barker L, Lekiachvili A, Xingyou Z. Comparison of ArcGIS and SAS geostatistical analyst to estimate population-weighted monthly temperature for US counties. J Resour Ecol. 2012;3:220–9. doi: 10.5814/j.issn.1674-764x.2012.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Juster FT, Ono H, Stafford FP. Changing times of American youth: 1981–2003. Ann Arbor (MI): University of Michigan, Institute for Social Research; 2004. Also available from: URL: http://ns.umich.edu/releases/2004/nov04/teen_time_report.pdf [cited 2014 May 5] [Google Scholar]