Abstract
Setting: National Diabetes Centre, Tonga.
Objective: To describe the diabetes patient profile and disease spectrum, assess the impact of diabetic care and evaluate diabetes-attributable adverse outcomes.
Design: Retrospective descriptive study of patients registered in the National Diabetes Registry from its inception in May 2004 to 2012, and review of the National Deaths Registry (2011–2012).
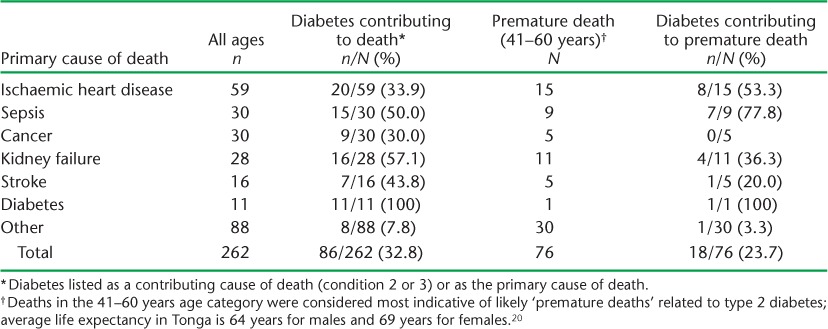
Results: Of 4653 patients with diabetes mellitus (DM) identified, 95.8% had type 2 DM, 0.2% type 1, 1.2% gestational DM and 2.9% pre-DM. Of the 4409 patients with type 2 DM, 64.7% were female, 82.7% were aged ⩾40 years, 25.3% had hypertension and 53.3% were obese. Among those in care for >2 years, no positive impact on body mass index or glycosylated haemoglobin could be demonstrated, but there was significant improvement in hypertension control. Morbidity included lower limb amputations in 272 (6.1%) patients. DM was listed as a contributory cause of death due to sepsis (15/30, 50.0%), kidney failure (16/28, 57.1%), stroke (7/16, 43.8%) and ischaemic heart disease (20/59, 33.9%).
Conclusion: DM was associated with high levels of morbidity and mortality. DM care improved hypertension control, but had little impact on other comorbid conditions. Enhanced monitoring and greater patient involvement should improve care; creative strategies are required to prevent and reduce obesity.
Keywords: diabetes, disease burden, disease spectrum, Tonga
Abstract
Contexte : Centre National du Diabète, Tonga.
Objectif : Décrire le profil des patients diabétiques et le spectre de la maladie, évaluer l'impact des soins et les résultats adverses attribuables au diabète (DM).
Schéma : Etude descriptive rétrospective des patients entrés dans le Registre National du Diabète depuis sa création en mai 2004 jusqu'en 2012; revue du Registre National des Décès (2011–2012).
Résultats : Au total, 4653 patients diabétiques ont été identifiés, 85,8% DM de type 2, 0,2% DM de type 1, 1,2%, avec un DM gestationnel et 2,9% un pré DM. Sur 4409 patients avec un DM de type 2, 64,7% étaient des femmes, 82,7% avaient ⩾40 ans, 25,3% avaient une hypertension et 53,3% étaient obèses. Parmi les patients soignés depuis plus de 2 ans, aucun effet positif n'a été démontré sur l'indice de masse corporelle ni sur l'HbA1c. Par contre, le contrôle de l'hypertension était significativement amélioré. La morbidité comprenait une amputation des membres inférieurs chez 272 patients (6,1%). Le DM a été signalé comme une contribution au décès par septicémie (15/30, 50%), par défaillance rénale (16/28, 57,1%), accident vasculaire cérébral (7/16, 43,8%) et maladie ischémique cardiaque (20/59, 33,9%).
Conclusion : Le DM était associé à un taux élevé de morbidité et de mortalité. Le prise en charge du DM améliorait le contrôle de l'hypertension mais avait peu d'impact sur le reste de la comorbidité. Un meilleur suivi et une plus grande implication des patients devraient améliorer cette prise en charge avec des stratégies créatives nécessaires à la prévention et à la diminution de l'obésité.
Abstract
Marco de referencia: El Centro Nacional de Diabetes de Tonga.
Objetivo: Describir las características de los pacientes con diagnóstico de diabetes (DM) y definir el tipo de enfermedad, evaluar la repercusión de la atención de la DM y analizar los desenlaces desfavorables atribuibles a la enfermedad.
Método: Fue este un estudio retrospectivo de los pacientes inscritos en el Registro Nacional de Diabetes desde su inicio en mayo del 2004 hasta el 2012; se examinó también el Registro Nacional de Defunciones (del 2011 al 2012).
Resultados: Se registraron 4653 pacientes diabéticos, de los cuales el 95,8% presentaba DM de tipo 2, el 0,2% DM de tipo 1, el 1,2% DM gestacional y el 2,9% pre-DM. De los 4409 pacientes con DM de tipo 2, el 64,7% eran mujeres, el 82,7% tenía ⩾40 años de edad, el 25,3% eran hipertensos y el 53,3% eran obesos. En los pacientes que habían acudido a la consulta de la DM durante más de 2 años, no se observó ninguna repercusión positiva en el índice de masa corporal ni en la concentración de la HbA1c, pero se puso en evidencia una mejoría considerable en la estabilización de la hipertensión arterial. La morbilidad asociada consistió en la amputación de los miembros inferiores en 272 pacientes (6,1%). Se notificó la DM como una causa subyacente de muerte en los casos de septicemia (15/30; 50,0%), insuficiencia renal (16/28; 57,1%), accidente cerebrovascular (7/16; 43,8%) y cardiopatía isquémica (20/59; 33,9%).
Conclusión: La DM se asoció con altas tasas de morbilidad y mortalidad. La atención de la enfermedad mejoró la regulación de la hipertensión arterial, pero tuvo poco efecto sobre otras enfermedades concomitantes. Se podría mejorar la atención de la DM con un seguimiento reforzado y una mayor participación de los pacientes, además de la introducción de estrategias creativas dirigidas a prevenir y disminuir la obesidad.
Major demographic shifts and lifestyle changes underlie the relentless rise in non-communicable diseases (NCDs) that has become evident in recent years.1,2 Although initially considered to be a problem of high-income countries, the global nature of the NCD challenge was formally recognised by the United Nations in 2011.1 In reality, low- and middle-income countries are often worse affected, and in these settings, the NCD burden overlaps with infectious diseases and poverty.3,4 Diabetes mellitus (DM) in particular affects 382 million people globally. This number is predicted to rise to 592 million by 2035.5
The Pacific Island nations carry an exceptionally high burden of DM disease; of the 10 countries with the highest DM prevalence globally, six are in the Pacific.6 This is illustrated by the situation in Tonga, where the first population-based survey conducted in 1975 documented a prevalence of DM of 7.5%,7 which increased to 15.1% by 1998.8 The Secretariat of the Pacific Community (SPC) released a report based on preliminary findings from the first STEPS survey in Tonga reporting a DM prevalence of 18.0% among those aged 25–64 years;9 data from a follow-up STEPs survey completed in 2012 are currently being analysed. In 1992, the Tonga Medical Association recognised the need for specialised DM care. In 1993, a dedicated DM clinic was established in Tongatapu, the main island of Tonga, and became the National Diabetes Centre. To monitor and improve the care of DM patients, a National Diabetes Registry was established in 2004. The Prime Minister, Lord Tu'ivakano, declared DM and NCDs a national health priority in 2011, recognising an urgent need for improved prevention strategies and better public health data to guide services and resource allocation.10
Despite ongoing data collection, no formal assessment of the National Diabetes Registry has been made to date. This study aimed to document the number of patients treated at the National Diabetes Centre since its inception, describe the disease spectrum and patient profile observed, and assess DM-attributable adverse outcomes as well as the impact of DM care.
METHODS
We conducted a retrospective descriptive study including all patients entered into the Tonga National Diabetes Registry from its inception in May 2004 to December 2012. As the National Diabetes Registry does not capture mortality data, information on cause of death for 2011 and 2012 was extracted from the National Deaths Registry with the assistance of the Statistics Department of the Ministry of Health.
Study setting
Tonga is a Pacific archipelago consisting of 170 islands, of which 36 are inhabited. There are five main island groups: Tongatapu, on which the capital Nuku'alofa is located, Vava'u, Ha'apai, ‘Eua and the Niuas. Of the total population (103 036; 2011 census), 70% live on the main island of Tongatapu, with Polynesians being the dominant ethnic group (97.0%).11
The National Diabetes Centre, where the registry is maintained, is located in Vaiola Hospital, the main referral hospital for Tonga, which provides free health care for Tongan citizens. Patients are referred from other hospitals, health centres, private practitioners or may present themselves. Outreach services provide DM care for the outer islands, but most patients seen at the National Diabetes Centre are from the main island. All patients diagnosed with DM, gestational DM or pre-DM are entered into the electronic National Diabetes Registry, and additional information is captured during follow-up visits. Data are entered by a clerk who transcribes information from the physician's clinical notes.
Definitions
Patients were categorised as having diabetes if they had 1) fasting glucose ⩾7 mmol/l (126 mg/dl), 2) random blood glucose ⩾11.1 mmol/l (200 mg/dl) with classical symptoms of DM (polyuria or polydipsia) or 3) if they had failed a standard glucose tolerance test (plasma glucose ⩾11.1 mmol/l 2 h after a 75 g glucose load). The type of DM was assigned by the treating physician; type 1 DM was considered in patients aged <20 years and confirmed by glutamic-acid decarboxylase autoantibodies or c-peptide assay. All other patients were classified as type 2 DM, unless they were found to be pregnant. Pregnant women were considered to have gestational DM if they had not been diagnosed with DM before the pregnancy and failed a standard glucose tolerance test (as above). Pre-DM included patients with impaired fasting glucose or glucose tolerance, defined as fasting plasma glucose of 6.1–6.9 mmol/l or 7.8–11.1 mmol/l 2 h after a standard glucose challenge.12,13 Patients were managed according to the International Diabetes Foundation (IDF, Brussels, Belgium) and the International Society for Pediatric and Adolescent Diabetes (ISPAD, Berlin, Germany) IDR/ISPAD 2011 Global Guideline for Diabetes in Childhood and Adolescence.14
Data analysis
Data routinely entered into the National Diabetes Registry were imported into EpiData version 6 (EpiData Association, Odense, Denmark) for analysis. Variables included age, sex, family history, type of DM, blood pressure, body mass index (BMI) and measures of DM control. To analyse changes in selected variables, we constructed a study group of patients who had been in care for at least 2 years and who had visited the clinic between 1 June 2011 and 31 May 2012, the last full year for which data were available. We compared data from their most recent visit with data recorded at the time of their first visit. For DM control, we compared the first and most recent glycosylated haemoglobin (HbA1c) readings in 625 patients for whom at least two readings, taken at least 6 months apart, were available. For comparative analysis, categorical variables were compared using the χ2 test and paired continuous variables (i.e., HbA1c) using the paired t-test. Levels of significance were set at 5%.
Ethics
Ethics approval was obtained from the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease (The Union), Paris, France, and from the National Ethics and Research Committee, Tonga (102/12).
RESULTS
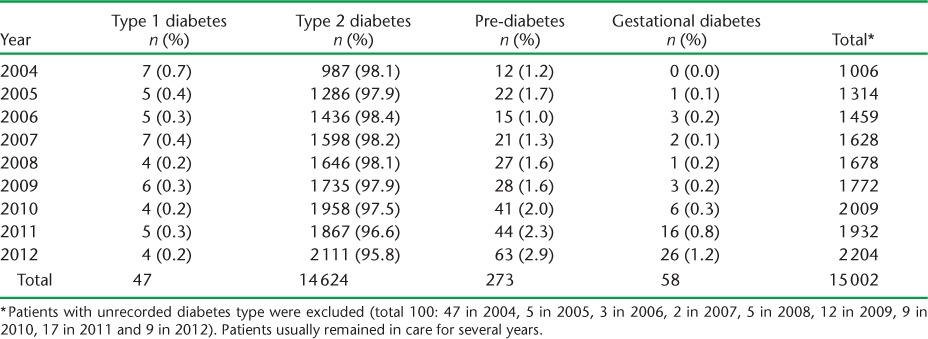
The National Diabetes Centre provided DM care to 1006 patients in the year of its inception (1993); this slowly increased to around 2000 patients in recent years. In total, 4653 patients received care during the study period. The Figure includes the number of individual patients who attended and the total number of patient visits recorded each year. The median number of visits per patient was 9 (range 1–42). More than 95% of patients were diagnosed with type 2 DM and very few (<1%) with type 1 DM. The full spectrum of disease, including gestational DM and pre-DM, is reflected in Table 1. In total, 3% of the population of Tongatapu received care for DM (type 1, type 2 or gestational) during 2012, using population estimates from the 2011 census, with an additional 0.1% being identified with pre-DM.
FIGURE.
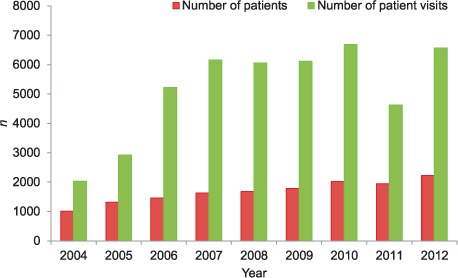
Number of patients in care and patient visits to the National Diabetes Centre in Tonga. Patients usually remain in care for several years.
TABLE 1.
Diabetes disease spectrum observed at the National Diabetes Centre, Tonga
The demographic profile and risk factors in people newly diagnosed with DM are included in Table 2. Data on lifestyle factors such as physical activity, smoking, alcohol consumption and diet, were poorly recorded. More than 50% of patients diagnosed with type 2 DM were obese (BMI > 30 kg/m2), but a substantial subgroup (n = 575, 12.8%) had low to normal BMI values (<25 kg/m2). Complications associated with DM were common. A relatively high percentage (272/4480, 6.1%) of type 2 DM patients required limb amputations during the study period, mostly of the lower leg, equating to 30 DM-associated amputations per year. Cataracts were recorded in 3.3% (149/4480) of patients and retinal abnormalities (combined non-proliferative and proliferative DM retinopathy and maculopathy) were present in 4.5% (203/4480). Serum creatinine was assessed in 99.5% of patients; the level recorded at the time of the most recent visit was normal (⩽120 umol/l) in 84% of patients, mildly elevated (120–240 umol/l) in 13% and severely elevated (>240 umol/l) in 3%. Tests for protein or micro-albumin in the urine were not routinely performed. Dialysis is not currently available in Tonga. Some Tongan DM patients are undergoing dialysis treatment outside Tonga, but no accurate data are available.
TABLE 2.
Patient demographics and risk factors in patients with type 1, type 2 and pre-diabetes during their first visit to the National Diabetes Centre, Tonga (n = 4481 * )
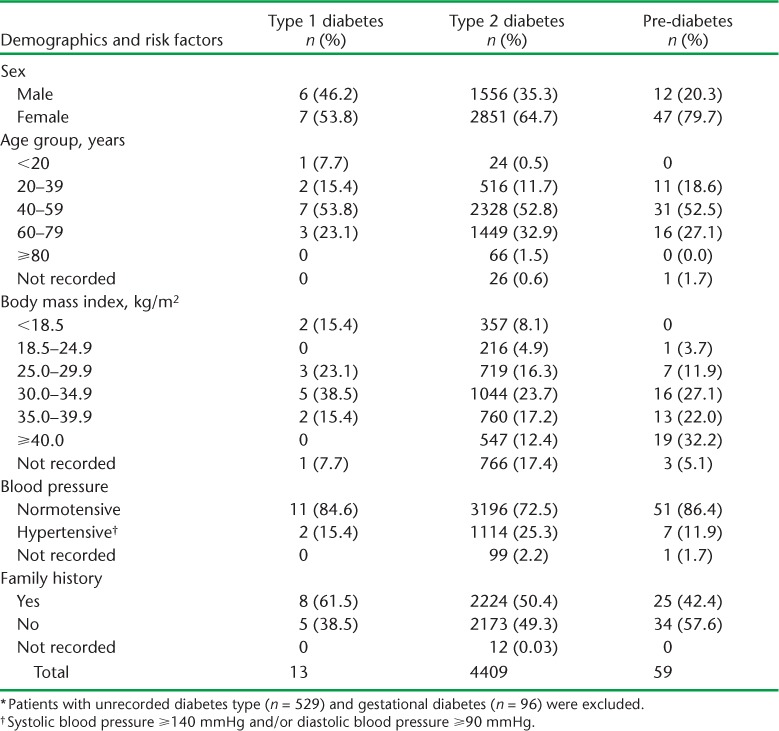
Table 3 shows changes in blood pressure, BMI, HbA1c and treatment in patients who had been in care for >2 years. There was a significant (P < 0.001) improvement in blood pressure control in those diagnosed with hypertension during their first visit: mean systolic pressure decreased from 149 mmHg (range 140–180) to 139 mmHg (range 90–210) and mean diastolic pressure from 92.2 mmHg (range 90–120) to 81.4 mmHg (range 60–110); 49.3% (67/136) retained an elevated systolic blood pressure (⩾140 mmHg) and 24.7% (24/97) an elevated diastolic blood pressure (⩾90 mmHg). In general, antihypertensive treatment provided at the National Diabetes Centre included an angiotensin converting enzyme (ACE) inhibitor as first-line treatment, with diuretics (thiazides and frusemide) and calcium channel (mainly nifedipine), or beta blockers added as required, taking into account patient co-morbidities and risk factors. There was little change in BMI profile over the 2-year period, with 41% of patients being obese at their first visit and 43% at their last visit.
TABLE 3.
Changes observed in people with diabetes who had been in care for at least 2 years (n = 347)
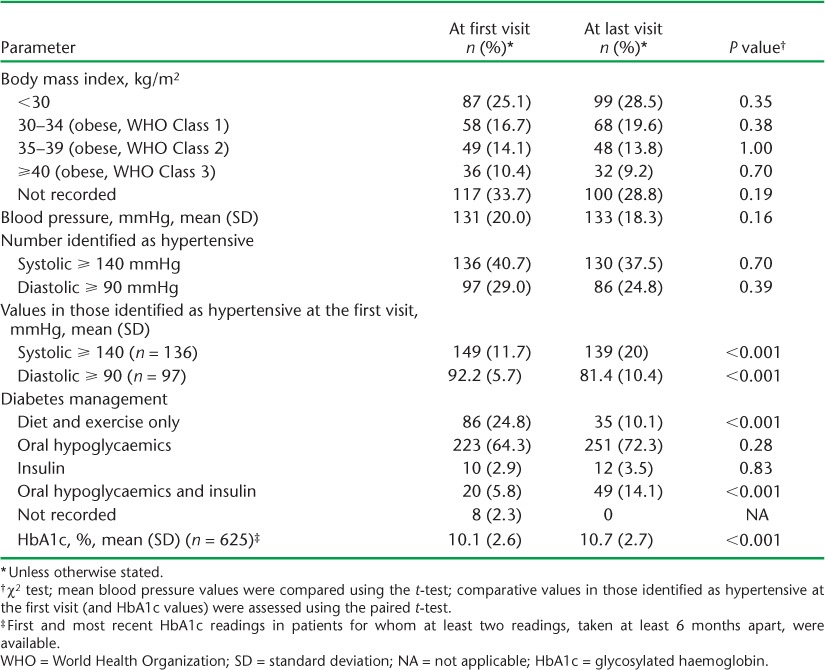
Due to initial poor availability of HbA1c testing, only 17 patients had a measurement performed at their first and their most recent visits, with no difference in mean values. For a more comprehensive overview of DM control, we performed an additional assessment of all patients who had two HbA1cs readings taken at least 6 months apart. In 625 patients with two HbA1c readings more than 6 months apart, the mean HbA1c value at the most recent reading (10.7%) was significantly higher than the first reading (10.1%; P < 0.001). Although more patients were on a combination of oral hypoglycemics and insulin treatment at the time of their most recent visit, its impact on glucose control could not be established. The use of ACE inhibitors and lipid lowering drugs were, however, well documented; 50.9% were on ACE inhibitors and 1.1% on lipid lowering drugs at their most recent visit.
Data from the National Deaths Registry were reviewed to supplement the limited outcome data contained in the National Diabetes Registry. These indicated that type 2 DM was a common contributing factor (listed as condition 2 or 3) in patients who died due to ischaemic heart disease (33.9%), sepsis (50.0%), stroke (43.8%) and kidney failure (57.1%). Its contribution to premature death in the 41–60 years age group was most pronounced in those dying due to sepsis (77.8%), ischaemic heart disease (53.3%) and kidney failure (36.3%), although far fewer people died in this age category (Table 4).
TABLE 4.
Diabetes as contributing cause of death as recorded in the National Death Registry
DISCUSSION
The 2004 STEPS survey estimated that 16.4% of Tongans have an elevated fasting blood glucose level (⩾7.0 mmol/l).15 Based on our study findings, approximately 3% of persons living with DM accessed care via the National Diabetes Centre during 2011–2012, demonstrating large gaps in awareness and service delivery. Although patients have been encouraged to seek care at local health centres in recent years and patients seen in the outer islands are not registered with the National Diabetes Centre, there remains a large portion of people with pre-DM and DM in the community who fail to access care.
The majority of patients had type 2 DM, which affected people of all ages, including children; however, most patients were aged >40 years and obese (BMI ⩾ 30). Interestingly, a substantial subgroup had low or normal weight. This has been described before,16,17 but probably included some misclassification by the attending clinician. With 68.7% of the nation considered obese,15 the rising numbers of people with type 2 DM is of real concern, and their care is likely to stretch already limited resources. Collective, creative and innovative efforts are required to address the problem, which is likely to be a challenge, as food occupies a special place in the Tongan culture. Addressing obesity is nevertheless the most promising means of reducing the DM disease burden in Tonga.
Associated morbidity included high rates of lower limb amputation. In the Ministry of Health annual report, there were 44 DM-related amputations in 2010 alone.18 Amputation has a wide ranging impact on individuals, their families and society as a whole. Amputation places a tremendous burden on the health care system, as these patients require ongoing care, while their reduced mobility has a major impact on those around them and on their own level of functioning.19 DM was frequently listed as a contributing cause of death, particularly associated with sepsis, kidney failure, ischaemic heart disease and stroke. These conditions may have contributed to the reduced life expectancy of Tongans from 72 years between 2005 and 2009 to 64 in males and 69 in females, as stated in Hufanga's study in 2012.20
Blood pressure control, which is essential for the prevention of and/or delaying complications such as nephropathy, retinopathy and stroke, improved significantly among patients in care. This was achieved despite a lack of evidence for positive lifestyle change, indicating the effectiveness of first-line hypertension treatment. This indicates that successful chronic disease management is possible with the use of effective oral medication and patient appreciation of its importance. In contrast, there was no evidence of improvement in glycaemic control. This disparity may be attributed to the fact that glycaemic control is heavily influenced by diet and less easily achieved by oral medication alone. Some patients with poor glycaemic control consistently refuse to go onto subcutaneous insulin injections, despite being on maximal oral hypoglycaemic treatment. Insulin pens are not available in Tonga, and insulin delivery using needles and syringes is less attractive to patients.
Adherence to dietary advice, medication and follow-up appointments is essential for good glycaemic control, while patients need to be actively involved in the management of their disease and take responsibility for their own health. Most Tongan patients regard the absence of symptoms as being disease-free and have little regard for the importance of chronic medication and dietary or lifestyle changes if they are not feeling unwell.21 Unfortunately, patients with type 2 DM become symptomatic only at an advanced stage of disease. Alternative strategies should be considered to engage patients more effectively and encourage ownership of their disease even in the absence of symptoms. Lifestyle changes are notoriously difficult to achieve, but novel approaches should be considered, with strengthening of public health aspects to prevent and reduce the burden of DM and other NCDs. DM is no longer just the responsibility of the clinician; it has become a major public health problem requiring interventions across a wide range of disciplines and sectors that take into account the wider social determinants of disease and the cultural drivers of obesity.
This study presents the first comprehensive review of DM care in Tonga, and includes data from more than 4000 patients. It is limited by its retrospective nature and the fact that many data points were poorly recorded in the National Diabetes Register. However, it represents real-life programme data, and provides an overview of management practices in a Pacific Island nation that ranks among the countries with the world's highest prevalence of DM. The study highlights the need to improve the quality of data collection, ensuring consistent collection of key variables. The use of standardised patient evaluation sheets during the first and subsequent visits would facilitate capture of key variables, encourage consistent data collection and facilitate data entry. Data should be entered on a continuous basis and be reviewed weekly to improve the completeness and quality of the data collected and to provide physician feedback. Cause of death data should be captured in the National Diabetes Registry, specifying primary and contributory causes of death in a standardised fashion.
In conclusion, type 2 DM was strongly associated with obesity, comorbidities and mortality. DM care improved hypertension management, but had no impact on glycaemic control or levels of obesity. Patient education, strengthened social support, enhanced monitoring and greater physician involvement may change this. Creative strategies such as the addition of obesity clinics to existing health services, teaching communities about healthier cooking methods and healthy lifestyle choices, are urgently needed. There should be greater emphasis on the prevention of DM (and associated risk factors) given the associated morbidity and mortality, as well as the difficulty of managing these patients in a remote Pacific Island setting.
Acknowledgments
The authors wish to thank all the patients, clinicians and health care personnel at the Tonga National Diabetes Centre; P Vivili, L Fonua, S Hufanga and the staff at the Health Information System Department, Ministry of Health; as well as J Vaha'i for his invaluable support. This research was supported through an operational research course jointly developed by the Centre for Operational Research, The International Union Against Tuberculosis and Lung Disease (The Union), Paris, France, and Médecins Sans Frontières, Brussels-Luxembourg, and run in the South Pacific by The Union and the Public Health Division of the Secretariat of the Pacific Community, Nouméa, New Caledonia.
Additional support for running the course was provided by the School of Population Health, The University of Auckland, Auckland, New Zealand; the College of Medicine, Nursing and Health Sciences, Fiji National University, Suva, Fiji; the Division of TB Elimination, Centers for Disease Control and Prevention, Atlanta, GA, USA; Regional Public Health, Hutt Valley District Health Board, Lower Hutt, New Zealand; the National TB Programme, Fiji Ministry of Health, Suva, Fiji; the Sydney Emerging Infections and Biosecurity Institute, The University of Sydney, Sydney, NSW, Australia; and the Dunedin School of Medicine, The University of Otago, Dunedin, New Zealand. Funding for the course was provided by the Global Fund to Fight AIDS, TB and Malaria, Geneva, Switzerland, the World Diabetes Foundation, Gentofte, Denmark, and the Australian Agency for International Development, Canberra, ACT, Australia.
Footnotes
Conflict of interest: none declared.
References
- 1.United Nations General Assembly. Political declaration of the high-level meeting of the General Assembly on the prevention and control of non-communicable disease. New York, NY, USA: UN; 2011. www.who.int/nmh/events/un_ncd_summit2011/political_declaration_en.pdf. Accessed January 2014. [Google Scholar]
- 2.Murray C J, Vos T, Lozano R et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013;380:2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 3.Bygbjerg I C. Double burden of non-communicable; and infectious diseases in developing countries. Science. 2012;337:1499–1501. doi: 10.1126/science.1223466. [DOI] [PubMed] [Google Scholar]
- 4.Marais B, Lönnroth K, Lawn S et al. Tuberculosis comorbidity with communicable and non-communicable diseases: integrating health services and control efforts. Lancet Infect Dis. 2013;13:436–448. doi: 10.1016/S1473-3099(13)70015-X. [DOI] [PubMed] [Google Scholar]
- 5.International Diabetes Federation. IDF Diabetes Atlas. 6th ed. Belgium, Brussels: IDF; 2013. www.idf.org/diabetesatlas/5e/the-global-burden. [Google Scholar]
- 6.International Diabetes Federation. IDF Diabetes Atlas. 5th ed. Belgium, Brussels: IDF; 2012. 2012 Update. www.idf.org/diabetesatlas/5e/update2012. [Google Scholar]
- 7.Finau S A, Stanhope J M, Prior I A M, Joseph J G, Puloka S T, Leslie P N. The Tonga cardiovascular and metabolic study: design, demographic aspects and medical findings. Community Health Stud. 1983;7:67–77. doi: 10.1111/j.1753-6405.1983.tb00393.x. [DOI] [PubMed] [Google Scholar]
- 8.Colaguiri S, Colaguiri R, Na'ati S, Muimuiheata S, Zariful H, Palu T. The prevalence of diabetes in the Kingdom of Tonga. Diabetes Care. 2002;25:1378–1383. doi: 10.2337/diacare.25.8.1378. [DOI] [PubMed] [Google Scholar]
- 9.Secretariat of the Pacific Community. NCD statistics for the Pacific Island countries and territories. Nouméa, New Caledonia: SPC; 2010. www.spc.int/hpl/index.php?option=com_docman&task=doc_download&gid=67 Accessed January 2014. [Google Scholar]
- 10.United Nations News Centre. Pacific Island leaders call at UN for greater efforts against lifestyle-related diseases. New Yourk, NY, USA: UN; 2011. www.un.org/apps/news/story.asp?NewsID=39774#.Uh.Pdhs3vGA. Accessed January 2014. [Google Scholar]
- 11.Tonga Ministry of Finance and National Planning. 2nd National Millennium Development Goals Report, Tonga. Status and Progress between 1990–2010. Nuku'alofa, Tonga: Ministry of Finance and National Planning; 2011. [Google Scholar]
- 12.International Diabetes Federation. Global guideline for type 2 diabetes. Brussels, Belgium: IDF; 2012. www.idf.org/sites/default/files/IDF-Guideline-for-Type-2-Diabetes.pdf. Accessed January 2014. [Google Scholar]
- 13.Scott G M. Pre-diabetes, metabolic syndrome, and cardiovascular risk. J Am Coll Cardiol. 2012;59:635–643. doi: 10.1016/j.jacc.2011.08.080. [DOI] [PubMed] [Google Scholar]
- 14.International Diabetes Federation. Global IDF/ISPAD guideline for diabetes in childhood and adolescence. Brussels, Belgium: IDF; 2011. [Google Scholar]
- 15.Kingdom of Tonga. NCD risk factors STEPS Report. Manila, The Philippines: World Health Organization Western Pacific Region; 2012. [Google Scholar]
- 16.Vaag A, Lund S S. Non-obese patients with type 2 diabetes and pre-diabetic subjects: distinct phenotypes requiring special diabetes treatment and (or) prevention? Appl Physiol Nutr Metab. 2007;32:912–920. doi: 10.1139/H07-100. [DOI] [PubMed] [Google Scholar]
- 17.Arner P, Pollare T, Lithell L. Different aetiologies of type 2 (non-insulin dependent) diabetes mellitus in obese and non-obese subjects. Diabetologia. 1991;34:483–487. doi: 10.1007/BF00403284. [DOI] [PubMed] [Google Scholar]
- 18.Ministry of Health, Kingdom of Tonga. Annual Report, 2010. Tongatapu, Tonga: MoH; 2010. http://www.health.gov.to/Annualreport_Public. Accessed January 2014. [Google Scholar]
- 19.Peters E J G, Childs M R, Wunderlich R P, Harkless L B, Armstrong D G, Lavery L A. Functional status of persons with diabetes-related lower extremity amputations. Diabetes Care. 2001;24:1799–1804. doi: 10.2337/diacare.24.10.1799. [DOI] [PubMed] [Google Scholar]
- 20.Hufanga S, Carter K L, Rao C, Lopez A, Taylor R. Mortality trends in Tonga: an assessment based on a synthesis of local data. Popul Health Metr. 2012;10:14. doi: 10.1186/1478-7954-10-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leslie H Y. Producing what in transition? Health messaging and cultural constructions of health in Tonga. Pacific Health Dialogue. 2003;9:296–302. [PubMed] [Google Scholar]


