Abstract
Setting: All provincial tuberculosis (TB) management units in the Solomon Islands.
Objective: To compare TB notifications, characteristics and treatment outcomes in urban vs. rural areas.
Design: A retrospective descriptive cohort study involving record review and data extraction from provincial TB and laboratory registers and treatment charts from 2000 to 2011.
Results: Of 4137 TB cases notified, 1364 (33%) were from urban and 3227 (67%) from rural areas. Notification rates per year of study were consistently higher in urban areas (104–150 per 100 000 population) than in rural areas (49–70/100 000). Cases in rural areas were more likely to have smear-negative pulmonary TB and less likely to have extra-pulmonary TB (P < 0.001). TB cases in rural areas were more likely to die from TB than those from urban areas (3.2% vs. 5.9%). In contrast, TB cases in rural areas were less likely to default (2.8% vs. 1.8%).
Conclusion: TB notification rates were much higher in urban than in rural areas in the Solomon Islands. Rural patients are more likely to die from the disease but are slightly less likely to default. Further research is required to explore the possibility of under-reporting in rural areas and to improve treatment outcomes.
Keywords: tuberculosis, urban, rural areas, Solomon Islands
Abstract
Contexte : Toutes les unités provinciales de prise en charge de la tuberculose (TB) dans les îles Salomon.
Objectif : Comparer la notification, les caractéristiques et les résultats du traitement de la TB dans les zones urbaines par rapport aux zones rurales.
Schéma : Etude rétrospective de cohorte impliquant une revue des dossiers et extraction de données des registres de TB provinciaux, ceux des laboratoires et les dossiers des patients (2000–2011).
Résultats : Un total de 4137 cas de TB ont été notifiés, dont 1364 (33%) venaient de zones urbaines et 3327 (67%) de zones rurales. Le taux de notification annuel était régulièrement plus élevé en zone urbaine (104–150/100 000) que dans les zones rurales (49–70/100 000). Les patients des zones rurales avaient plus souvent des frottis négatifs et moins souvent une TB extra pulmonaire (P < 0,001). Les patients ruraux mouraient plus souvent que les patients urbains (3,2% vs. 5.9%). Par contre, les patients ruraux abandonnaient moins souvent leur traitement (2,8% vs. 1,8%).
Conclusion : Les taux de notification de TB étaient plus élevés dans les zones urbaines que rurales dans les îles Salomon. Les patients ruraux mouraient plus souvent, mais abandonnaient moins souvent leur traitement. Des recherches plus avancées sont requises pour vérifier la possibilité de sous-notification dans les zones rurales et améliorer les résultats du traitement.
Abstract
Marco de referencia: Todas las unidades de tratamiento de la tuberculosis (TB) a escala de las provincias en las Islas Salomón.
Objetivo: Comparar el índice de notificación, las características de los pacientes y los desenlaces terapéuticos de la TB en las zonas urbanas y las zonas rurales.
Métodos: Fue este un estudio de cohortes descriptivo y retrospectivo, en el cual se analizaron las historias clínicas y se extrajeron datos de los registros de TB, los registros de laboratorio y las tarjetas de tratamiento de cada provincia (del 2000 al 2011).
Resultados: Se notificaron 4137 casos de TB, de los cuales 1364 provenían de zonas urbanas (33%) y 3227 de zonas rurales (67%). Las tasas de notificación por año fueron de manera constante más altas en las zonas urbanas (104–150/100 000) que en las zonas rurales (49–70/100 000). En los entornos rurales, fue más probable observar casos de TB pulmonar con baciloscopia negativa y menos probable encontrar casos de TB extrapulmonar (P < 0,001). La mortalidad fue más probable en los casos de TB delas zonas rurales que en los ámbitos urbanos (3,2% contra 5,9%). En contraste, fue menos frecuente el abandono del tratamiento en los pacientes aquejados de TB en medio rural (2,8% contra 1,8%).
Conclusión: Las tasas de notificación de la TB en las Islas Salomón fueron mucho más altas en las zonas urbanas que en medios rurales. También fue más alta la mortalidad en los pacientes de medio rural, pero en zona rural fue menos probable el abandono del tratamiento. Se precisan nuevas investigaciones que examinen la posibilidad de subnotificación en zona rural y de lograr progresos en materia de desenlace terapéutico.
Solomon Islands is one of six countries in the Pa-cific region that have been identified as having a high burden of tuberculosis (TB), with more than 300 TB cases reported annually and notification rates of 74 per 100 000 population per year.1,2 The National TB Control Programme (NTP) began implementing the DOTS strategy in 1997 and countrywide coverage was achieved in 2000. The NTP reports treatment outcomes from the 10 provinces on a quarterly basis. Six provincial hospitals and two mission hospitals provide laboratory services, while 316 health centres provide DOTS services.
About 80% of the population of the Solomon Islands lives in rural areas. As the quality of care provided to patients depends on their access to health services, outcome is generally considered to be poorer in rural areas. Few studies have compared TB incidence in urban vs. rural areas. In Malawi, it was shown that the TB incidence rate was higher in urban areas.3
The aim of the present study was to assess if there are significant differences in the notification, patient characteristics and treatment outcomes of TB patients in urban compared to rural areas in the Solomon Islands.
METHODS
Study design
This was a retrospective, descriptive cohort study involving record review and extraction of data from provincial TB and laboratory registers and treatment charts.
Study setting
Solomon Islands is a double chain archipelago of more than 900 small scattered islands and six main islands. According to the 2009 census, the total population of Solomon Islands was about 515 870, of which more than 80% live in rural areas.4 Solomon Islands was classified as a lower middle-income country by the World Bank, with a gross national income of US$1110 per capita.5 The country is politically divided into 10 provinces: Central, Choiseul, Guadalcanal, Honiara City, Malaita, Makira, Renbel, Temotu, Western and Isabel.
Of the 10 provinces, six had provincial base hospitals, while the remaining four provinces (Guadalcanal, Central, Renbel and Honiara City) do not have provincial hospitals of their own, but use the National Referral Hospital as their base hospital for diagnosis and admission of TB patients for the initial phase of treatment. Two mission hospitals also provide laboratory services, and about 316 health centres provide DOTS services during the continuation phase of treatment.
Although the prevalence of human immunodefi-ciency virus (HIV) in Solomon Islands is low (<0.1%),2 and no case of TB-HIV co-infection has been reported, the burden of TB is said to be among the highest in the Pacific.1 All confirmed TB patients are diagnosed using sputum microscopy or clinical assessment, and have to spend 2 months in hospital for the initial phase of treatment before discharge to take another 4 months of treatment at home during the continuation phase under the supervision of health care workers at health centres. In each of the 10 provinces, data from the peripheral health units are collated into the provincial TB register, which is kept at the provincial management units (PMU). These collated provincial TB registers were used for this study. Each PMU was visited between late 2012 and early 2013 as part of routine NTP supervision.
Study participants
All TB cases diagnosed, registered and placed on anti-tuberculosis treatment from 2000 to 2011 were included in the study.
Data and statistical analysis
The following data were collected from the provincial TB and laboratory registers: age, sex, name and location of health centre that supervised the continuation phase of treatment, type of TB and treatment outcome. Each patient was registered and characterised as being treated in an urban or rural area based on the location of the health centre that supervised their continuation phase of treatment. An ‘urban area’ was defined as a DOTS centre located within a town or provincial centre, while a ‘rural area’ was defined as a DOTS centre located outside a town boundary or provincial centre. Data were then entered into EpiData Version 3.1 (EpiData Association, Odense, Denmark) and cross-checked for consistency. Population size by area was obtained from the 2009 census and extrapolated backwards and forwards for the years of the study using growth rates reported in the census for urban and rural areas. TB notification rates were then calculated separately for urban and rural areas.
Ethics approval
Ethics approval was obtained from the National Research and Ethics Committee of the Ministry of Health, Honiara, Solomon Islands and from the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease, Paris, France.
RESULTS
During the period from 2000 to 2011, a total of 4137 TB cases were notified, of whom 1364 (33%) were from urban and 2773 (67%) from rural areas. The trend in notification rates over the 11-year period showed that these were consistently higher in urban (range 104–155/100 000) than in rural areas (range 49–70/100 000) (Figure 1).
FIGURE 1.
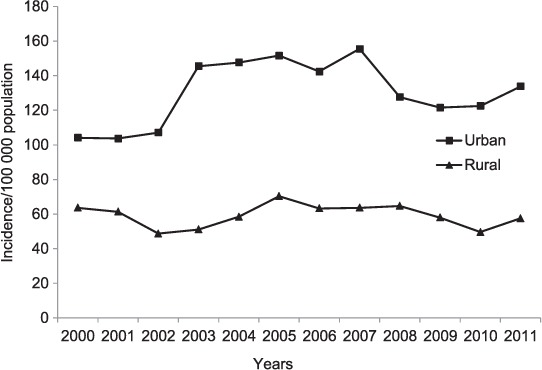
Trends in TB notification rates (all types) by year in urban vs. rural areas, Solomon Islands, 2000–2011. TB = tuberculosis.
Overall, approximately 50% of cases were males, with minor but significant differences between urban and rural patients (Table 1). There were also significant differences in terms of age: while the proportion of children was similar, a larger proportion of cases were aged 15–44 years in urban areas and fewer were older adults. However, these differences were consistent with the different age structures of the rural and urban populations reported in the census (data not shown).
TABLE 1.
Characteristics and disease pattern of 4137 TB patients in urban vs. rural areas, Solomon Islands, 2000–2011
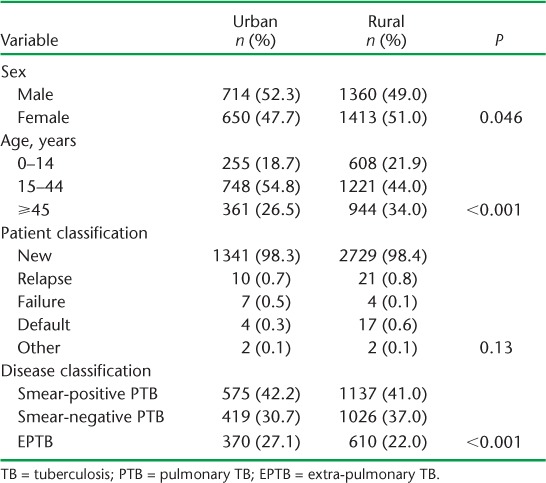
Almost all (>98%) cases in both rural and urban areas had newly diagnosed pulmonary TB. While respectively 42% and 41% of the TB cases in urban and rural areas were sputum smear-positive, those in rural areas were more likely to have smear-negative pulmonary TB and less likely to have extra-pulmonary TB (EPTB) (P < 0.001).
Overall, TB cases in rural areas were more likely to die than those from urban areas (3.2% vs. 5.9%) (Table 2). This difference was relatively consistent across the years of the study (Figure 2), and was most prominent in cases with EPTB. In contrast, TB cases in rural areas were less likely to default (2.8% vs. 1.8%), while TB cases in urban areas were more likely to be transferred out than those from rural areas (Table 2).
TABLE 2.
Treatment outcomes of TB patients in urban vs. rural areas, Solomon Islands, 2000–2011
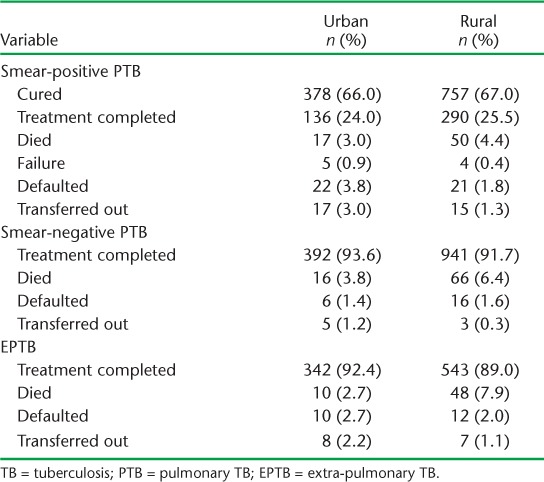
FIGURE 2.
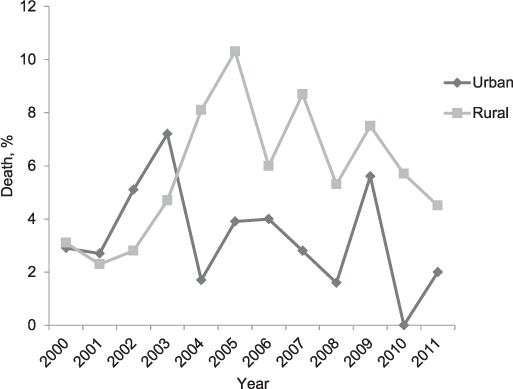
Trends in TB deaths among notified TB cases (all types) by year in urban vs. rural areas, Solomon Islands 2000–2011. TB = tuberculosis.
DISCUSSION
This study has shown that TB notification rates have been consistently higher in urban than in rural areas. Higher notification rates and worse outcomes of respiratory diseases in urban areas have also been reported from industrialised countries.5 A key question, noting that notified cases are identified through passive case detection, is whether the finding of different notification rates by location reflects the true situation.6 At least a part of the explanation may be that there is less access to diagnostic facilities in rural areas.7 It should be noted that the DOTS programme is not fully established in rural areas in Solomon Islands.
The study also found that patients in urban areas were more likely to transfer out. It is not surprising to find that TB patients from urban areas were more likely to transfer out or move from place to place to find better health care services or return to their home village. It is this migration issue that contributes to their slightly increased likelihood of defaulting from treatment.
We also observed some differences in patient characteristics, type of TB and treatment outcomes between urban and rural areas. Specifically, there were minor differences in age and sex, patients in rural areas were more likely to have smear-negative pulmonary TB and less likely to have EPTB, and patients in rural areas were slightly less likely to default but more likely to die. The higher mortality rate among TB cases in rural areas may be related to poor access to health care, leading to late presentation, although diagnostic delay was not associated with increased mortality in a study from Viet Nam,8 and distance travelled to a diagnostic facility was not associated with TB mortality in South Africa.9 Apart from HIV, predictors of TB mortality that were identified are multidrug resistance and treatment completion;10 the Mycobacterium tuberculosis strain may have played a role in treatment outcomes.11 As has been reported elsewhere,12 treatment completion rates were not worse in rural areas in Solomon Islands, and rural TB patients were less likely to default. Further studies are required to fully understand why there is higher mortality in TB patients from rural areas in Solomon Islands.
The strengths of the study are that we included countrywide data extracted from all provincial TB and laboratory registers, and its large size, which enabled analysis of treatment outcomes according to urban vs. rural areas. Furthermore, as census data were readily available to provide population denominators for the calculation of notification rates, they are likely to reflect the operational reality.
Some limitations of the study are that TB cases who were non-residents or immigrants from other countries could not be traced to verify whether or not they had completed treatment. We were also unable to verify if there had been changes in some rural facilities to semi-urban or urban areas; however we did maintain the definition of rural and urban in the settings. Some important variables mentioned were not available, as they were not recorded in the TB registers as part of the routine programme information, and these could not be verified.
The prevalence of HIV and TB-HIV co-infection was quite low and the NTP has not reported any cases of multidrug resistance.9 As noted above, the NTP has no access to reports from countries where passive case finding is seen as a limitation.
CONCLUSION
This study has identified some significant differences between TB patients from rural and those from urban areas, especially in TB notification rates and treatment outcomes. These results can help guide the NTP to focus its management strategies on areas that need closer attention; however, further operational research is required to identify the reasons for our study findings and to improve TB control strategies in the Solomon Islands.
Acknowledgments
This research was supported through an operational research course that was jointly developed by the Centre for Operational Research, International Union Against Tuberculosis and Lung Disease (The Union), Paris, France, and the Médecins Sans Frontières, Brussels-Luxembourg, and run in the South Pacific by The Union and the Public Health Division of the Secretariat of the Pacific Community, Nouméa, New Caledonia.
Additional support for running the course was provided by the School of Population Health, The University of Auckland, Auckland, New Zealand; the College of Medicine, Nursing and Health Sciences, Fiji National University, Suva, Fiji; the Division of TB Elimination, Centers for Disease Control and Prevention, Atlanta, GA, USA; Regional Public Health, Hutt Valley District Health Board, Lower Hutt, New Zealand; the National TB Programme, Fiji Ministry of Health, Suva, Fiji; the Sydney Emerging Infections and Biosecurity Institute, The University of Sydney, Sydney, NSW, Australia and Dunedin School of Medicine, The University of Otago, Dunedin, New Zealand. Funding for the course was provided by the Global Fund to Fight AIDS, TB and Malaria, Geneva, Switzerland, the World Diabetes Foundation, Gentofte, Denmark, and the Australian Agency for International Development, Canberra, ACT, Australia.
Footnotes
Conflict of interest: none declared.
References
- 1.O'Connor J, Wiegandt A, Viney K. Tuberculosis surveillance in the Pacific Island countries and territories. Noumea, New Caledonia: Secretariat of the Pacific Community; 2010. [Google Scholar]
- 2.World Health Organization. Global Tuberculosis Report, 2012. Geneva, Switzerland: WHO; 2012. [Google Scholar]
- 3.Banerjee A, Harries A D, Salaniponi F M. Differences in tuberculosis incidence rates in township and in rural populations in Ntcheu District, Malawi. Trans R Soc Trop Med Hyg. 1999;93:392–393. doi: 10.1016/s0035-9203(99)90128-1. [DOI] [PubMed] [Google Scholar]
- 4.Solomon Islands National Statistics Office. Solomon Islands Population and Housing Census 2009. Honiara, Solomon Islands: Solomon Islands National Statistics Office; 2009. [Google Scholar]
- 5.O'Reilly G, O'Reilly D, Rosato M, Connolly S. Urban and rural variations in morbidity and mortality in Northern Ireland. BMC Public Health. 2007;7:123. doi: 10.1186/1471-2458-7-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Touray K, Adetifa I M, Jallow A et al. Spatial analysis of tuberculosis in an urban west African setting: is there evidence of clustering? Trop Med Int Health. 2010;15:664–672. doi: 10.1111/j.1365-3156.2010.02533.x. [DOI] [PubMed] [Google Scholar]
- 7.Huong N T, Vree M, Duong B D et al. Delays in the diagnosis and treatment of tuberculosis patients in Vietnam: a cross-sectional study. BMC Public Health. 2007;7:110. doi: 10.1186/1471-2458-7-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vree M, Huong N T, Duong B D et al. High mortality during tuberculosis treatment does not indicate long diagnostic delays in Viet Nam: a cohort study. BMC Public Health. 2007;7:210. doi: 10.1186/1471-2458-7-210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barker R D, Nthangeni M E, Millard F J. Is the distance a patient lives from hospital a risk factor for death from tuberculosis in rural South Africa? Int J Tuberc Lung Dis. 2002;6:98–103. [PubMed] [Google Scholar]
- 10.Pablos-Mendez A, Sterling T R, Frieden T R. The relationship between delayed or incomplete treatment and all-cause mortality in patients with tuberculosis. JAMA. 1996;276:1223–1228. doi: 10.1001/jama.1996.03540150025026. [DOI] [PubMed] [Google Scholar]
- 11.Parwati I, Alisjahbana B, Apriani L et al. Mycobacterium tuberculosis Beijing genotype is an independent risk factor for tuberculosis treatment failure in Indonesia. J Infect Dis. 2010;201:553–557. doi: 10.1086/650311. [DOI] [PubMed] [Google Scholar]
- 12.Abubakar I, Crofts J P, Gelb D, Story A, Andrews N, Watson J M. Investigating urban-rural disparities in tuberculosis treatment outcome in England and Wales. Epidemiol Infect. 2008;136:122–127. doi: 10.1017/S0950268807008333. [DOI] [PMC free article] [PubMed] [Google Scholar]


