Abstract
Aim
To quantify the relationship between 5-min Apgar scores and infant mortality for infants at the borderline of viability.
Methods
Cohort study of 7008 infants 23–25 weeks' gestation using 2002 US National Center for Health Statistics data. Using Cox proportional-hazards models, we quantified the relationship between Apgar score and infant mortality for all infants, and then infants surviving their first 24 h. Models were adjusted for gestational age, birth weight, gender, delivery method, plurality, maternal race, marital status and education.
Results
Within one year, 46% of infants died. Of the non-survivors, deaths within 24 h were more common among infants with Apgar scores 0–3 (83%) than among infants with Apgar scores 7–10 (13%). When including all infants and adjusting for potential confounders, each 1-point increase in Apgar score decreased the hazard of mortality by 0.82. However, after excluding infants who died within 24 h, the hazard ratio increased to 0.95; although statistically significant, the practical impact was negated.
Conclusions
For 23–25 week gestation infants surviving the first 24 h, the Apgar score loses clinical significance. Clinicians should be aware of the limitations of clinical assessments in the delivery room.
Keywords: Apgar score, Epidemiology, Neonatology, Prematurity
Introduction
When making decisions about initiating and continuing resuscitation for infants at the borderline of viability, international guidelines suggest that gestational age is the dominant feature. As a rule, resuscitation below 23 weeks gestation is considered futile and resuscitation above 25 weeks is routine (1–3). Beyond gestational age, other prognostic features available antenatally include birth weight, gender, multiple gestations and use of antenatal steroids (4). Nonetheless, many physicians have reported that ‘how the infant looks at birth’ or ‘how the infant responds to resuscitation’ will influence their decision to continue, or abort, resuscitative efforts after birth (5).
Apgar scores have been traditionally used by pediatricians as a measurement of ‘how an infant looks at birth’ and ‘how an infant responds to resuscitation’ (6). In term infants, Apgar scores have been shown to correlate with mortality, although fewer studies have evaluated the correlation between Apgar score and outcome in the earliest gestational age groups (7). Casey et al. (8) reported an inverse correlation between mortality and Apgar scores in a large hospital-based study of infants ranging from 26 to 36 weeks More recently, using US infant birth and death certificate data from the National Center for Health Statistics, Lee et al.(9) found that lower 5-min Apgar scores were associated with greater mortality risk at gestational ages from 24 to 36 weeks. However, not all studies have shown a correlation between Apgar score and outcome. Genzel-Boroviczény et al. (10) reported in a single-center study of 234 infants born between 23 and 26 weeks that 1-min Apgar scores of 0 or 1 were associated with increased mortality, but that no clear association was seen between any 1-min Apgar score >1 and mortality risk in this gestational age group. Similarly, Singh et al. (5) in a study of 102 infants 400-750 g admitted to a single center found that 1- or 5-min Apgar scores ≤3 were not significantly associated with increased risk of mortality or Bayley MDI or PDI < 70 at 2 years of age before or after adjustment for birth weight, gestational age, gender and race.
One possible reason for the discrepancy between findings of prior studies may lie in the timing of data collection. Large data sets likely capture all infants regardless of their time of death, including those who die in the delivery room or within hours of admission to a NICU. In contrast, clinical studies may only enroll infants after admission to the NICU, or those judged likely to survive the first hours of life. The prognostic value of Apgar score may differ between these two types of enrollment criteria. Such a difference in timing may have important implications for the prognostic value of the Apgar score as applied to counselling families of extreme preterm infants, both prenatally and after admission to the NICU.
The aim of the present study was to use a large national data set to investigate more thoroughly the relationship between low 5-min Apgar scores and mortality for infants born at the borderline of viability. Recognizing that time of death varies directly with gestational age, we hypothesized that infants with lower Apgar scores may also be more likely to die earlier, and consequently correlation of Apgar scores with infant mortality would disappear within the first 24 h of life. If confirmed, this recognition would help families understand more precisely how much to expect from a physician's clinical judgment of ‘how an infant looks’ in the delivery room.
Patients and Methods
Study population
We performed a retrospective cohort analysis of linked birth-infant death certificate records from the 2002 US National Center for Health Statistics. We included all births of US-born infants with gestational ages 23–25 weeks; to minimize the impact of inaccurate gestational age reporting, we included only those infants with birth weights within the 3rd–97th percentile for gestational age as identified by gestational age-specific growth charts (11). We excluded births outside of hospitals, lack of physician or midwife at delivery (as an experienced health care provider to assign Apgar scores), and births in California and Texas (these states do not report Apgar scores on birth certificates) (12).
Variables and categorization
The primary outcome was infant mortality, defined as death within the first year of life. Timing of death was categorized, per the convention of infant death certificate files, as occurring at <24 or ≥24 h of life. Apgar score was treated as an interval variable ranging from 0 to 9; Apgar scores of 9 and 10 were grouped together because of their low prevalence in this extremely preterm population. Potential confounders included clinical risk factors known prior to resuscitation (gestational age, birth weight, gender, singleton versus multiple births, delivery method), and maternal demographic factors that may impact decision-making regarding resuscitation (race, marital status, education).
Data analysis
We compared the distribution of 5-min Apgar scores and gestational age, as well as the gestational age-specific infant mortality, to other published neonatal research studies to assess the validity of using birth-certificate data at these gestational ages. We calculated the proportion of infants who died in <24 h by 5-min Apgar score at each gestational age. Next, we compared the relationship between 5-min Apgar score and infant mortality for (i) all infants in the study population and (ii) the subset of infants who survived the first 24 h of life. Chi-squared tests were used to compare differences in proportions. Finally, we generated a series of Cox proportional-hazards models to quantify the relationship between 5-min Apgar score and infant mortality for different groups: (i) all infants, Apgars 0–10; (ii) infants surviving the first 24 h, Apgars 0–10; (iii) infants 23–24 weeks, Apgars 0–10; and (iv) 23–24 week infants surviving the first 24 h, Apgars 0–10. These four models were then repeated for infants with Apgars 2–10. All analyses were conducted using STATA 11.0 or SAS 9.1.3. Statistical significance was accepted at p < 0.05.
Results
For inclusion in the study, 7132 infants were identified. Of those infants, 124 infants were missing Apgar score data. There were no statistically significant differences between infants missing Apgar scores and infants with recorded Apgar scores in gestational age, gender or race; infants delivered vaginally were somewhat more likely to be missing Apgar score on their birth certificate than infants delivered via cesarean section (2.71% versus 1.62%, p = 0.025).
Distribution of 5-min Apgar scores
Overall, low Apgar scores were common; 1203/7008 (17%) of infants had a 5-min Apgar score of 0–1, and 1825/7008 (26%) had a 5-min Apgar score of 0–3. Relationships between 5-min Apgar scores and other risk factors for infant mortality are shown in Table S1. Statistically significant differences in the distribution of 5-min Apgar scores were seen by infants' gestational age, birth weight, method of delivery and maternal education. More than 40% of 23-week infants, 14% of 24-week infants and 7% of 25-week infants had Ap-gar scores of 0–1. Infants born via vaginal delivery had higher proportions of lower Apgar scores than infants born via cesarean section.
Infant mortality
Of the 7008 infants, 3250 (46%) died in the first year of life. Table S2 summarizes overall infant mortality for the data set. The gestational age-specific infant mortality was within 1–4% points of mortality prior to NICU discharge reported by the Neonatal Research Network: for 23 weeks, 74% versus 78%; for 24 weeks, 45% versus 47%; for 25 weeks, 28% versus 29% (13). Higher rates of infant mortality were seen among younger gestation infants, male infants, multiples, infants born via vaginal delivery, infants born to non-Hispanic White and Hispanic mothers and infants born to married mothers.
5-min Apgar scores and timing of infant mortality
Of the 3250 non-survivors, 1553 (48%) died in <24 h. Figure S1 displays the relationship of 5-min Apgar score and the timing of death for those infants. At lower Apgar scores, greater proportions of non-survivors died before 24 h of life. 92% of all non-surviving infants with an Apgar of 0 or 1 (comprising 32% of all non-survivors) died before 24 h of life, whereas only 17% of non-surviving infants with Apgar scores ≥5 died before 24 h of life.
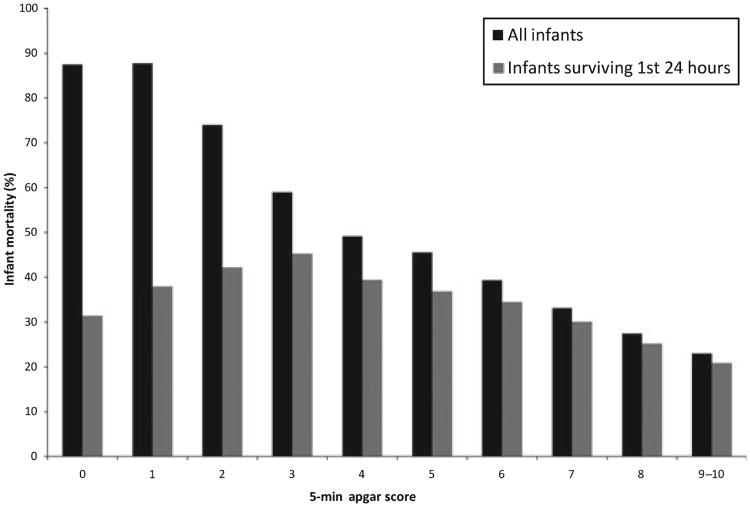
The relationship between 5-min Apgar score and infant mortality is depicted in Figure 1. When all infants were included, there was a strong inverse relationship between 5-min Apgar score and mortality, ranging from 88% of infants with Apgars 0–1 to 23% of infants with Apgars of 9. However, after omitting infants who died prior to 24 h, the relationship between Apgar score and mortality became much weaker. Infants with 5-min Apgar scores of 0–1 who survived the first 24 h had paradoxically lower subsequent mortality than infants with higher Apgar scores. To assess only the infants who had <90% mortality before 24 h, infants with Apgar scores of 2–10 were considered separately; again, the range of infant mortality narrowed substantially after excluding those who died before 24 h.
Figure 1.
Infant mortality by 5-min Apgar score, including and excluding infants who died within the first 24 h of life. Black bars indicate the proportion of infants at each Apgar score who died within the first year of life. Grey bars indicate infant mortality at each Apgar score only for the subset of infants who survived the first 24 h of life.
A series of Cox proportional-hazards models were fitted to quantify the relationship between Apgar score and mortality, and to compare the difference in this relationship when infants who died within 24 h were excluded. Models were adjusted for gestational age, as well as other significant risk factors including birth weight, gender, plurality, delivery method, maternal race, marital status and education. Potential confounders were entered into the model in for-ward-stepwise fashion. Results are shown in Table 1. Although the hazard of mortality for each 1-point increase in Apgar score was statistically significant in all models, the magnitude of effect was much smaller after excluding infants who died in the first 24 h of life (hazard ratio 0.82 versus 0.95). Results were nearly identical when including only infants with Apgar scores of 2–10, or including only 23–24 week infants.
Table 1. Hazard ratios for changing risk of mortality with each 1-point increase in Apgar score.
| n | Unadjusted | Adjusted | ||
|---|---|---|---|---|
|
| ||||
| Gestational age | Gestational age + risk factors | |||
| Apgar 0–10 | ||||
| ALL infants | 7008 | 0.76 | 0.80 | 0.82 |
| Survived 24 h | 5455 | 0.90 | 0.93 | 0.95 |
| Apgar 0–10 | ||||
| 23–24 week infants | 4053 | 0.79 | 0.81 | 0.84 |
| Survived 24 h | 2778 | 0.93 | 0.94 | 0.97+ |
| Apgar 2–10 | ||||
| ALL infants | 5805 | 0.79 | 0.82 | 0.84 |
| Survived 24 h | 5220 | 0.87 | 0.90 | 0.92 |
| Apgar 2–10 | ||||
| 23–24 week infants | 3050 | 0.81 | 0.83 | 0.85 |
| Survived 24 h | 2610 | 0.89 | 0.90 | 0.93 |
Results from a series of Cox proportional-hazards models to assess the relationship between 5-min Apgar score and infant mortality, including and excluding infants who died prior to 24 h of life. ‘All infants’ indicates all infants 23–25 weeks in the study group; ‘Survived 24 h’ excludes those who died prior to 24 h of life. ‘23–24 week infants’ indicates that 25 week infants were excluded. ‘Apgar 0–10’; includes each 5-min Apgar score; ‘Apgar 2–10’ excludes those with Apgar scores of 0 or 1. n indicates the number of infants retained in each model. ‘Unadjusted’ indicates the hazard of mortality without accounting for other clinical or maternal risk factors. ‘Adjusted’ refers to other risk factors included in the model: a) gestational age, b) gestational age, birth weight, gender, plurality, delivery method, maternal race, marital status and maternal education. All hazard ratios were statistically significant at p < 0.001 except as marked with a +, which had a p value of 0.013.
Discussion
Predicting outcomes for infants in the grey zone of viability is, by definition, problematic. Even after a decision has been made to initiate resuscitative efforts, physicians and parents often want to know when to consider withdrawal of intervention for infants who remain at high risk of mortality despite successful resuscitation. We investigated how much information is available from a 5-min Apgar score. We show here that for infants born between 23 and 25 weeks gestation, a low 5-min Apgar score is highly correlated with death. This was not unexpected. We have also shown that the vast majority of these deaths occur within 1 day. This too was anticipated. However, we have demonstrated here that the ability of an Apgar score to predict death among infants born at the margin of viability is drastically decreased within 1 day of life; that is, for the population of 23–25 week gestation infants who remain alive 24 h after birth, the 5-min Apgar score loses practical prognostic power.
This finding has two potential implications. First, it offers a possible clarification for the differences in results among studies published previously on this topic: population-based assessments of the predictive utility of the Apgar score likely capture all infants born in a hospital or health care system, whereas studies based on clinical trials likely capture infants who survived long enough to be enrolled in a clinical trial. Even if infants were enrolled in the first day of life, this may have an important effect on study findings in regards to mortality.
Secondly, these findings imply that the predictive value of clinical judgments of an infant's status may have a time-limited impact. For many infants born at the limit of viability with low Apgar scores, parental preferences and/or physician discretion may limit resuscitation efforts in the delivery room or early upon admission to the NICU (1–3,14). However, our data suggest that both parents and physicians should be cautious using 5-min Apgar scores to make prognostic pronouncements for infants who survive the first 24 h of life.
Some limitations of our study are clear. Analysis of birth certificate – infant mortality linked data does not permit assessment of a detailed medical course or later neurodevelopmental outcome. However, Singh et al. (5)'s single-center study evaluating infants who survived long enough to be enrolled in clinical trials suggests that infants with low Apgar scores who survive to NICU discharge do not have higher degrees of morbidity than infants of the same age and weight group who had higher Apgar scores at delivery. Multi-center studies of early predictors of neonatal morbidity at the limit of viability have found similarly weak correlation between Apgar score and survivors' neuro-developmental outcome. The EPICure study of 308 surviving children ≤25 weeks did not find Apgar score to be a significant independent predictor of morbidity at 30 months adjusted age (15). An NICHD study of 246 surviving infants <750 g and ≤24 weeks in 1993-1999 with 1-min Apgar scores <3 showed that 54% had MDI >70% and 33% had MDI >85; 64% had PDI >70 and 41% had PDI >85; this indicates a high degree of morbidity among surviving infants, but not much different than that reported for surviving infants ≤24 weeks overall in other NICHD studies (16,17).
Why study Apgar scores at all? The Apgar score was designed not as a predictive prognostication tool but rather a standardized first assessment of an infant's status and need for further resuscitation (6,18). The assignment of Apgar scores has been recognized to differ between caregivers and likely varies with physicians' opinions of the infant's chances of survival (18). Nevertheless, no other widely available tool captures the physiologic parameters that physicians would use when evaluating a response to resuscitation (6). A survey of several hundred US neonatologists in 2003 regarding resuscitation preferences for infants at the border of viability showed that almost half of physicians surveyed used ‘how an infant looked’ in the moments after delivery to help them make decisions regarding resuscitation versus comfort care (5). Apart from Apgar scores, a prospective study showed that physicians are poorly able to predict outcome based on observation in the delivery room (19). This present study extends the notion that the predicting outcomes for extremely preterm infants in the NICU based upon assessment in the delivery room is poorly supported by current evidence.
Another potential limitation of our study is that the data does not parse out whether resuscitation was limited at the request of either parent or physician, or whether infants died in spite of aggressive resuscitation. Cultural differences affect decision-making regarding resuscitation in this gestational age group; we have a limited ability to identify cultural differences in administrative data beyond information such as marital status, race/ethnic group and education. Details of the resuscitation are likewise unavailable in this data. Future research may be able to address these factors in a prospective study.
More broadly, the fact that an association between a risk factor (low Apgar score) and an outcome (mortality) disappears within 24 h speaks to the importance of considering time course in predicting neonatal outcomes. Many outcome studies evaluate overall mortality, or overall mortality with some degree of disability, as a function of features known at or around the time of birth (4, 13, 15). However, many families of infants in the NICU are interested in more than merely population-based assessments - rather, they would like physicians to take into account the response of their baby to neonatal intensive care before making individualized prognostic judgments (20). This study adds to the growing body of research directed at helping families and physicians assess the likely outcome of NICU infants, using the information that a time-limited trial of NICU intervention can provide (21-24). Apgar scores, it appears, provide very little help for infants who can survive more than 24 h. We continue to search for better prognostic features.
Supplementary Material
Figure S1 Proportion of non-surviving infants who died prior to 24 h of life, by 5-min Apgar score and gestational age. This figure displays the time of death for the 3250/7008 infants who died within the first year of life. Infants with lower Apgar scores died earlier than infants with higher Apgar scores; the majority of infants with Apgar scores ≤3 died in less than 24 h. Apgar scores of 9 and 10 were combined because of small n.
Table S1 Characteristics of study infants by 5-min Apgar score.
Table S2 Risk factors for infant mortality.
Key notes.
Higher 5-min Apgar scores decrease the risk of infant mortality among infants 23–25 weeks' gestation. However, there is no clinically significant relationship between Apgar scores and mortality among infants surviving the first 24 h of life. Clinicians should understand the limitations of their assessment of infants in the delivery room.
Footnotes
Supporting Information: Additional Supporting Information may be found in the online version of this article
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- 1.American Academy of Pediatrics, Committee on Bioethics. Guidelines on forgoing life-sustaining medical treatment. Pediatrics. 1994;93:532–6. [PubMed] [Google Scholar]
- 2.Rebagliato M, Cuttini M, Broggin L, Berbik I, de Vonderweid U, Hansen G, et al. Neonatal end-of-life decision-making: physicians' attitudes and relationship with self-reported practices in 10 European countries. JAMA. 2000;284:2451–9. doi: 10.1001/jama.284.19.2451. [DOI] [PubMed] [Google Scholar]
- 3.Lantos JD, Tyson JE, Allen A, Frader J, Hack M, Korones S, et al. Withholding and withdrawing life sustaining treatment in neonatal intensive care: issues for the 1990s. Arch Dis Child Fetal Neonatal Ed. 1994;71:F218–23. doi: 10.1136/fn.71.3.f218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tyson J, Parikh N, Langer J, Green C, Higgins RD. Intensive care for extreme prematurity – moving beyond gestational age. New Engl J Med. 2008;358:1672–81. doi: 10.1056/NEJMoa073059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singh JK, Fanaroff J, Andrews B, Caldarelli L, Lagatta J, Plesha-Troyke S, et al. Resuscitation in the “gray zone” of viability: determining physician preferences and predicting infant outcomes. Pediatrics. 2007;120:519–26. doi: 10.1542/peds.2006-2966. [DOI] [PubMed] [Google Scholar]
- 6.Apgar V. A proposal for a new method of evaluation of the newborn infant. Curr Res Anesth Analg. 1953;32:260–7. [PubMed] [Google Scholar]
- 7.Thorngren-Jerneck K, Herbst A. Low 5-minute Apgar score: a population-based register study of 1 million term births. Obstet Gynecol. 2001;98:65–70. doi: 10.1016/s0029-7844(01)01370-9. [DOI] [PubMed] [Google Scholar]
- 8.Casey BM, McIntyre DD, Leveno KJ. The continuing value of the Apgar score for the assessment of newborn infants. New Engl J Med. 2001;344:467–71. doi: 10.1056/NEJM200102153440701. [DOI] [PubMed] [Google Scholar]
- 9.Lee HC, Subeh M, Gould JB. Low Apgar score and mortality in extremely preterm neonates born in the United States. Acta Paediatr. 2010;99:1785–9. doi: 10.1111/j.1651-2227.2010.01935.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Genzel-Boroviczény O, Hempelman J, Zoppelli L, Martinez A. Predictive value of the 1-minute Apgar score for survival at 23– 26 weeks gestational age. Acta Paediatr. 2010;99:1790–4. doi: 10.1111/j.1651-2227.2010.01937.x. [DOI] [PubMed] [Google Scholar]
- 11.Oken E, Kleinman KP, Rich-Edwards J, Gillman MW. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatr. 2003;3:6. doi: 10.1186/1471-2431-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Center for Health Statistics. Birth cohort linked birth and infant death data set. Hyattsville, MD: National Center for Health Statistics; 2002. [Google Scholar]
- 13.Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126:443–56. doi: 10.1542/peds.2009-2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kattwinkel J, Perlman JM, Aziz K, Colby C, Fairchild K, Gallagher G, et al. Neonatal resuscitation: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Pediatrics. 2010;126:e1400–13. doi: 10.1542/peds.2010-2972E. [DOI] [PubMed] [Google Scholar]
- 15.Wood NS, Costeloe K, Gibson AT, Hennessy EM, Marlow N, Wilkinson AR, et al. The EPICure study: associations and antecedents of neurological and developmental disability at 30 months of age following extremely preterm birth. Arch Dis Child Fetal Neonatal Ed. 2005;90:F134–40. doi: 10.1136/adc.2004.052407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shankaran S, Johnson Y, Langer JC, Vohr BR, Fanaroff AA, Wright LL, et al. Outcome of extremely-low-birth-weight infants at highest risk: gestational age ≤24 weeks, birth weight ≤750 g, and 1-minute Apgar ≤3. Am J Obstetr Gynecol. 2004;191:1084–91. doi: 10.1016/j.ajog.2004.05.032. [DOI] [PubMed] [Google Scholar]
- 17.Wilson-Costello D, Friedman H, Minich N, Fanaroff AA, Hack M. Improved survival rates with increased neurodevelopmental disability for extremely low birth weight infants in the 1990s. Pediatrics. 2005;115:997–1003. doi: 10.1542/peds.2004-0221. [DOI] [PubMed] [Google Scholar]
- 18.Hegyi T, Carbone T, Anwar M, Ostfeld B, Hiatt M, Koons A, et al. The Apgar score and its components in the preterm infant. Pediatrics. 1998;101:77–81. doi: 10.1542/peds.101.1.77. [DOI] [PubMed] [Google Scholar]
- 19.Manley BJ, Dawson JA, Kamlin OF, Donath SM, Morley CJ, Davis PG. Clinical assessment of extremely premature infants in the delivery room is a poor predictor of survival. Pediatrics. 2010;125:e559–64. doi: 10.1542/peds.2009-1307. [DOI] [PubMed] [Google Scholar]
- 20.Partridge JC, Martinez AM, Nishida H, Boo NY, Tan KW, Ye-ung CY, et al. International comparison of care for very low birth weight infants: parents' perceptions of counseling and decision-making. Pediatrics. 2005;116:e263–71. doi: 10.1542/peds.2004-2274. [DOI] [PubMed] [Google Scholar]
- 21.Meadow W, Frain L, Ren Y, Lee G, Soneji S, Lantos J. Serial assessment of mortality in the neonatal intensive care unit by algorithm and intuition: certainty, uncertainty, and informed consent. Pediatrics. 2002;109:878–86. doi: 10.1542/peds.109.5.878. [DOI] [PubMed] [Google Scholar]
- 22.Meadow W, Lagatta J, Andrews B, Caldarelli L, Keiser A, La-porte J, et al. Just, in time: ethical implications of serial predictions of death and morbidity for ventilated premature infants. Pediatrics. 2008;121:732–40. doi: 10.1542/peds.2006-2797. [DOI] [PubMed] [Google Scholar]
- 23.Ambalavanan N, Carlo WA, Bobashev G, Mathias E, Liu B, Poole K, et al. Prediction of death for extremely low birth weight neonates. Pediatrics. 2005;116:1367–73. doi: 10.1542/peds.2004-2099. [DOI] [PubMed] [Google Scholar]
- 24.Lagatta J, Andrews B, Caldarelli L, Schreiber M, Plesha-Troyke S, Meadow W. Early NICU therapy improves predictive power for the outcomes of ventilated ELBW infants. J Pediatr. doi: 10.1016/j.jpeds.2011.02.014. Epub ahead of Print. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Proportion of non-surviving infants who died prior to 24 h of life, by 5-min Apgar score and gestational age. This figure displays the time of death for the 3250/7008 infants who died within the first year of life. Infants with lower Apgar scores died earlier than infants with higher Apgar scores; the majority of infants with Apgar scores ≤3 died in less than 24 h. Apgar scores of 9 and 10 were combined because of small n.
Table S1 Characteristics of study infants by 5-min Apgar score.
Table S2 Risk factors for infant mortality.