Abstract
A systematic review was conducted to assess the employment rate of people with schizophrenia. Additionally, information from the selected studies concerning factors associated with employment and health-related quality of life (HRQoL) was examined. Employment rates ranged from 4% to 50.4%. The studies differed considerably in design, patient settings, and methods of recruitment. The most frequently reported factors associated with employment were negative and cognitive symptoms, age of onset, and duration and course of the disease. Individual characteristics associated with unemployment were older age, lower education, and sex (female). Additionally, environmental factors, eg, the availability of welfare benefits and vocational support programs, seemed to play a role. Generally, being employed was positively associated with HRQoL. However, the causal direction of this association remained unclear, as studies on the bidirectional relationship between employment and HRQoL were lacking.
Keywords: health-related quality of life, employment, work, unemployment, mental illness, patient characteristics, environment
Introduction
On a patient level, employment plays a central role in providing financial income and nonfinancial gains, including social identity, social contacts and support, a means of structuring and occupying time, activity and involvement, and a sense of personal achievement.1 People with long-term mental illness, including schizophrenia, are sensitive to the negative effects of unemployment, and experience barriers to work, due to stigma, prejudice, and discrimination.1 Apart from these individual disadvantages, unemployment in people with schizophrenia is economically costly from a societal point of view. The estimated total societal cost of schizophrenia was 6.7 billion pounds in England for the year 2004–2005.2 Half of these costs were due to unemployment, absence from work, and premature mortality, amounting to 3.4 billion pounds.
Studies reporting on employment in people with schizophrenia show diverging figures. However, generally employment rates are low. Marwaha and Johnson were the first authors to publish a review on schizophrenia and employment.3 They concluded that there is a wide variation in reported employment rates. Additionally, their study showed that employment is correlated with positive outcomes in social functioning, symptom levels, quality of life (QoL), and self-esteem, but a clear causal relationship was not demonstrated.3
Increasingly, treatment models have focused on the subject of employment in people with schizophrenia. These treatment models strive, among other goals, to increase the individual’s own subjective view of well-being and satisfaction with his or her life. This development is in line with the shift in mental health services from an emphasis on treatment focused on reducing symptoms, based on a narrow notion of health and disease, to a more holistic approach that takes both well-being and functioning into consideration.4 However, for people with schizophrenia, there is still a lack of information on the subject of employment and associated health-related QoL (HRQoL).
A previous study has shown that being employed is associated with a markedly better HRQoL for people with schizophrenia.5 However, the relationship between being employed and HRQoL may be bidirectional. It is known that the type of employment plays a crucial role in the effect on HRQoL.5 For instance, having a voluntary job, in general, means a low income. This may result in relatively poor living conditions and inability to afford social activities. Consequently, this may lead to a diminished HRQoL.6,7 In addition, although intuitively being employed may lead to increased HRQoL, the converse reasoning is also defendable, that is, having a higher HRQoL indicates being happier, presumably resulting in better capacities to perform daily activities such as a (paid) job. So, there is still a need to further explore the association between employment and HRQoL in schizophrenia.
Firstly, this review assessed the prevalence of employment in people with schizophrenia. Next, we aimed to identify factors associated with being employed in this population. Lastly, we examined the interrelation between being employed and HRQoL that was assessed in the studies under review.
Methods
A literature search was conducted to identify the employment rate in people with schizophrenia. We applied a broad definition of employment as having any job, whether full-time or part-time, and whether competitive or supported employment. In addition, we screened the selected papers for factors associated with being employed and for the interrelationship between being employed and HRQoL.
Search strategy
A systematic literature search was performed in PubMed and PsychInfo, including studies from 2000 until July 1, 2013, including information on employment in representative (groups of) adults diagnosed with schizophrenia. We applied a broad search strategy for identifying studies. Consequently, no criteria concerning study design were applied. The search terms included the Medical Subject Headings (MeSH) terms and Field terms “schizophrenia”, “employment”, “unemployment”, “paid work”, and “work capacity” (Supplementary material). The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement was followed for the reporting of systematic reviews and meta-analyses.8
Selection strategy
The selection of the abstracts was independently performed by two researchers. Discrepancies concerning inclusion or exclusion of an abstract were resolved by discussing the eligibility criteria during plenary meetings. The selection criteria were:
Studies published in 2000 or later
Studies performed in Western countries, or in Japan or Hong Kong
Studies explicitly including people diagnosed with schizophrenia
Studies for which information on (un)employment or work was given in the Abstract
Case studies, editorial letters, comments, or conference proceedings were excluded
-
Studies reporting on vocational rehabilitation therapy and/or vocational support programs were excluded.
To determine the eligibility of the full-text articles, the same selection criteria were used. Additional exclusion criteria were:
Duplication of source data (ie, studies using samples of other included studies were excluded)
Unavailability of the full-text publication
Studies including selective samples, eg, the homeless, the convicted, or convenience samples, were excluded
Studies including study samples with <100 participants.
First, we presented the prevalence rates of employment in people with schizophrenia, derived from the review. In order to systematically describe the factors associated with employment, a simplified framework was used based on the model of Wilson and Cleary,9 which integrates health aspects with functional status and HRQoL. The basic domains of functional status that are commonly measured are physical”, “social”, “role”, and “psychological functioning”.10 We defined being employed (or unemployed) as part of the functional status. The symptoms are reflected in the disease characteristics of the disorder – these may reflect physical impairment as well as patients’ emotional or cognitive state. Schizophrenia can be described as a syndrome11,12 characterized by:
Positive symptoms
Negative symptoms
Cognitive symptoms
Affective symptoms.
Symptoms of schizophrenia are generally described in terms of a positive and a negative dimension. The Positive and Negative Syndrome Scale (PANSS) is, among other instruments, applied for measuring the severity of positive and negative symptoms.13 Positive symptoms indicate the occurrence of delusions and hallucinations, while negative symptoms indicate lack of motivation, reduction in spontaneous speech, and social withdrawal. Additionally, there may be a cognitive dimension (difficulties in memory, attention, and executive functioning) and a dimension of affective dysregulation (depression and manic symptoms).
Additionally, the disorder can be described in terms of the age at onset of the disease, the treatment setting, and the duration and course of the disease in terms of remission.
Finally, the functional status may be affected by the co-occurrence of substance and alcohol abuse. Substance abuse has been found to be substantially more prevalent among people with schizophrenia.14,15 However, prevalence rates of co-occurring dependence or abuse in people with schizophrenia may vary between countries.16 Substance abuse may worsen the impact of schizophrenia, leading to heightened social adjustment problems.17
The adapted model takes into account that characteristics of the individual as well as “characteristics of the environment” might impact the experience of symptoms, functional status, and HRQoL, and their relationships. Examples of individual characteristics are age, sex, personality, and individual expectations. With regard to being employed, specifically, motivation and “work readiness” are examples of characteristics of the individual that are probably of importance in finding and maintaining a paid job. Examples of environmental characteristics are social and vocational support, and social security programs. Finally, stigma is also a factor known to diminish the HRQoL of people with schizophrenia, even after recovery of the person.18
Overall QoL is preferably measured with a generic preference based instrument. In this way, the impact of a condition on HRQoL can be assessed in terms that are relevant to any individual.
Data extraction
Employment rates from the publications were independently extracted by two researchers. Additional data that were collected were the design of the study, the country, the sample size, exclusion criteria, the study setting, demographic information of the study population, clinical measures (eg, PANSS), length of illness, and comorbidity. Additionally, findings concerning associations with employment and concerning employment and HRQoL were recorded.
Results
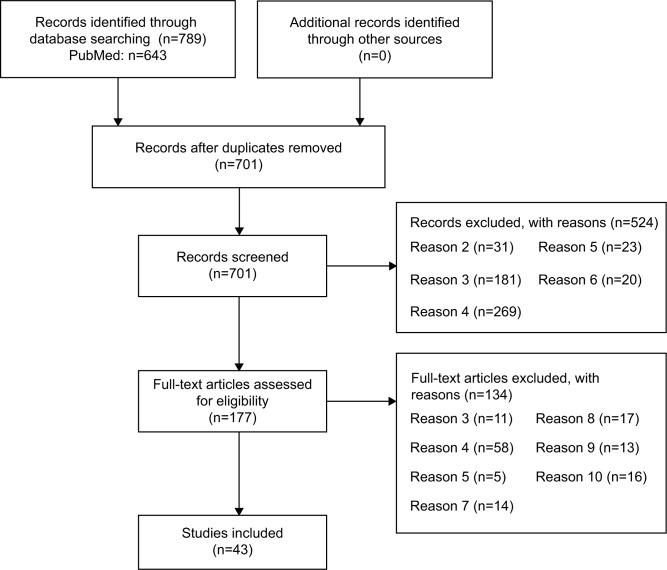
A total of 789 records were derived from the databases. After removal of duplicates, 701 abstracts were screened. In the search, six review studies were identified. Studies cited in these reviews that were not identified in our search and that met our selection criteria were added (Figure 1).
Figure 1.
Flow chart of the literature search.
Notes: Reasons for exclusion: 2= not performed in a Western country or Japan or Hong Kong; 3= people with schizophrenia not explicitly included; 4= no (un)employment rate described; 5= case study; 6= study on vocational rehabilitation therapy or vocational support programs; 7= duplicate sources; 8= full text publication unavailable; 9= studies including selective samples or convenience samples were excluded; 10= study sample had <100 subjects.
In total, 43 studies were eligible for analyzing the prevalence of employment (Table 1).
Table 1.
Studies reporting on employment in people diagnosed with schizophrenia
| Author | Study design | N | Country | Single/multicenter | Exclusion criteria | In-/outpatients | Study population characteristics | Employed (%) | Remark |
|---|---|---|---|---|---|---|---|---|---|
| Abdel-Baki et al19 | Cohort Baseline + FU | Baseline: n=142; 2-yr FU: n=111; 5-yr FU: n=97; 10-to 16-yr FU: n=78; 5-yr FU: n=78 | Canada | Multicenter | Schizoaffective and other psychotic disorders | In-and outpatients | Baseline: Age (median): 24.4 yrs Males: 71.1% Length of illness: close to illness onset Alcohol/substance abuse: 27.5% (at some point) PANSS: NR |
Baseline: 20.1%; 2-yr FU: 14.9%; 5-yr FU: 22.6%; 10-to 16-yr FU: 17.9% | Employment not specified |
| Alonso et al20 | Cohort Baseline | 9,340 | Denmark, France, Greece, Ireland, Italy, the Netherlands, Portugal, Spain, UK | Multicenter | NR | Outpatients | Age (mean): 40 yrs Males: 57.9% Length of illness: 11.3 yrs Alcohol/substance abuse: NR PANSS: NR |
19.7% | Paid employment, not further specified |
| Ascher-Svanum et al21 | Cohort Baseline + 3-yr FU | 2,175 | USA | Multicenter | NR | NR | Baseline: Age (mean): 42.1 yrs Males: 61.4% Length of illness: 21.6 yrs Alcohol/substance abuse: 27.1% PANSS neg: 18.3 PANSS pos: 16.1 |
Baseline: 21.1% 3-yr FU: 21.5% | Paid employment, not further specified |
| Barbui et al22 | RCT Baseline | 409 | UK, Italy, the Netherlands, Germany | Multicenter | Treatment by forensic psych services, alcohol/drug dependence, moderate/severe mental handicap | NR. Probably outpatients | Age (mean): 41.5 yrs Males: 59.9% Length of illness: NR Alcohol/substance abuse: NR PANSS: NR |
Unemployed 44.7% | Not specified |
| Bobes et al23 | Cross-sectional Baseline | 1,452 | Spain | Multicenter | NR | Outpatients receiving commonly used oral antipsychotic treatment | Age (mean): 40.7 yrs (range 18–74 yrs) Males: 60.9% Length of illness: 15.5 yrs Alcohol/substance abuse: NR PANSS neg: 20.6 PANSS pos: 14.8 |
Active 19.8% Sick leave 6.1% Disability pension 47.5%; unemployed 17% |
Employment not specified |
| Boyer et al24 | Cross-sectional Baseline | 113 | France | Single-center | Mental retardation, unstable condition 2 months before inclusion | Outpatients | Age (mean): 38.6 yrs Males: 69.9% Length of illness: 13.9 yrs Alcohol/substance abuse: NR PANSS: NR |
14.2% | Employment not specified |
| Caron et al25 | Cohort Baseline | 181 | Canada | Multicenter | Physical illness, neurological disorders; acute symptoms; treatment through mental health services <2 yrs | Outpatients + probably <10% inpatients | Age (mean): 40.3 yrs Males: 76% Length of illness: NR Alcohol/substance abuse: NR PANSS: NR |
7.2% | Patients with income from paid employment |
| Cechnicki et al26 | Cross-sectional Baseline | 202 | Poland | Multicenter | Presence of acute symptoms | In-and outpatients | Age (mean): 39.9 yrs Males: 49% Length of illness: NR Alcohol/substance abuse: NR PANSS: NR |
2% full time; 5.4% part time Sheltered job 5%; pension/disability 68.3% |
Employment not specified |
| Chwastiak et al27 | RCT Baseline | 1,424 | USA | Multicenter | First episode or history of only 1 episode; unstable medical condition, treatment refractory/resistance, schizoaffective disorder, mental retardation/other cognitive disorder; cardiac disorders | Both inpatients and outpatients | Age (mean): 40.6 yrs Males: 75% Length of illness: NR Alcohol/substance abuse: NR PANSS neg: 20.1 PANSS pos: 18.4 |
26% Earned income 14%; other vocational activity 12% | Employment rate = earned income or noncompetitive employment activities (volunteer work; workshop; prevocational programs) |
| Compton et al28 | Cross-sectional survey Baseline | 248 | USA | Multicenter | Other diagnoses than schizophrenia, schizophreniform disorder and schizoaffective disorder were excluded | In-and outpatients | Age (mean): 42.9 yrs Males: 64.3% Length of illness: NR Alcohol/substance abuse: 27.4% PANSS: NR |
Not working: 83% | Not further specified |
| Cuyún Carter et al29 | Cross-sectional Baseline | 1,635 | USA | Multicenter | Participating in clinical drug trial within 30 days prior to enrollment | In-and outpatients (93.5%) | Age (mean): 42.3 yrs Males: 61.2% Length of illness: NR Alcohol/substance abuse: 26.3% PANSS neg: 18.3 PANSS pos: 18.5 |
20.6% | Employment not specified |
| Giugiario et al30 | Cross-sectional | 253 | Italy | Single-center | Clinical unstable. Patients with other employment than competitive were excluded | Outpatients | Age (mean): 40.1 yrs Males: 57.9% Length of illness: 14.3 yrs Alcohol/substance abuse: NR PANSS neg: 19.6 PANSS pos: 14.5 |
30.0% | Competitive employment: Job paid min wage or higher, not contracted with a social service agency |
| Gureje et al31 | Cross sectional | 582 | Australia | NR | NR (Sample derived from data of the Australian National Survey of Mental Health and Wellbeing) | In-and outpatients | Age (mean): 38.7 yrs Males: 66.5% Length of illness: 14.8 yrs Alcohol/substance abuse: NR PANSS: NR |
Unemployed: 76.3%; On disability/sickness pension 79% | No definition reported |
| Hansson et al32 | RCT | 507 | Spain, the Netherlands, UK, Sweden, Germany, Switzerland | Multicenter | No severe organic psychiatric illness or primary substance abuse | Outpatients | Age (mean): 42.2 yrs Males: 66.2% Length of illness:15.9 yrs Alcohol/substance abuse: NR PANSS: NR |
Unemployed 36.0% | Not specified |
| Henry et al33 | Cohort FU (mean FU 6.9 yrs) | 361 | Australia | Single-center | Drug-/alcohol-induced psychosis | In-and outpatients | Baseline: Age (mean): 21.9 (baseline range 14–30 yrs) Males: 77% Length of illness: NR Alcohol/substance abuse: NR PANSS neg: NR PANSS pos: NR |
36.3% (part time or full time) Unemployed/Government benefits 57.6% | Employment not specified |
| Hofer et al34 | Cross sectional | 140 | Austria | Multicenter | Clinical unstable; suffering from any other axis I disorder, including substance abuse | Outpatients disorders | Age (mean): 40.2 yrs Males: 60% Length of illness: 11.2 yrs Alcohol/substance abuse: 0% PANSS neg: 15.7 PANSS pos: 11.2 |
8.6% (full time) 7.1% (part time) Supported employment 12.1%; training 7.9%; unemployed 65.7% | Competitive employment |
| Holthausen et al35 | Cohort 2-yr FU | 103 | the Netherlands | Multicenter | Severe mental retardation, systemic or neurological illness | NR | Baseline: Age (mean): 23.6 yrs Males: 74.8% Length of illness: onset within 2 yrs before inclusion Alcohol/substance abuse: 68% PANSS: NR |
20.4% | Competitive employment or studying with a scholarship |
| Honkonen et al36 | Cohort 3-yr FU | 2,168 | Finland | Multicenter | NR. Included 3 cohorts of persons with schizophrenia 3 years after discharge from psychiatric hospital (discharged 1986, 1990, and 1994). Representing patients with long-term schizophrenia | NR | Age (mean): 39.2 Males: 66.5% Length of illness: NR Alcohol/substance abuse: NR PANSS: NR |
Overall after 3 yrs: 4% | Part-time or full-time competitive employment (including self-employed, farmers, farmers’ wives) |
| Karadayi et al37 | Cross-sectional | 102 | Turkey | Single-center | Hospitalized/having relapse within the last 3 months; severe physical disorder | Outpatients | Age (mean): 31.5 yrs Males: 59.8% Length of illness: 9.9 yrs Alcohol/substance abuse: 2% PANSS neg: 13.0 PANSS pos: 11.2 |
37.3% | Employment was a part-time or full-time working activity with payment or attending school |
| Kulkarni et al38 | Cohort Baseline + 3-yr FU | 347 276 | Australia | Multicenter | NR | In-and outpatients | Baseline: Age (mean) age: 33.8 yrs Males: 62% Length of illness: NR Alcohol/substance abuse: NR PANSS neg: 18.3 PANSS pos: 16.7 |
Baseline: 11% 3-yr FU 16% | Paid employment, not further specified |
| Lambert et al39 | Cohort Baseline | 2,960 | Germany | NR | Bipolar disorder, substance induced psychosis or psychosis due to medical condition | Outpatients | Age (mean): 42.3 yrs Males: 49.4% Length of illness: NR Alcohol/substance abuse: 19.7% PANSS: NR |
42.6% | Full or part time (not further specified) or attending school/university |
| Mackell et al40 | Cross-sectional | 332 | USA | NR | NR | NR. Probably outpatients | Age (mean): 39.6 yrs Males: 72.6% Length of illness: NR Alcohol/substance abuse: 5% PANSS: NR |
20.5% | Paid employment, not further specified |
| Marwaha et al41 | Cohort 2-yr FU | 1,086 | UK, Germany, France | Multicenter | Continuously in hospital for the previous 12 months; currently homeless | NR | Refer to Marwaha et al42 | 27.3% | Full-or part-time jobs, including sheltered employment and voluntary work |
| Marwaha et al42 | Cross-sectional Baseline | 1,208 | France, Germany, UK | Multicenter | Continuously in hospital for the previous 12 months; currently homeless | NR | Age (mean): 40.8 Males: 61.5% Length of illness: 14.4 Abuse: alcohol 2.9%; substance 1.1% PANSS neg: 15.8 PANSS pos: 12.4 |
21.5% (never employed 7.9%) | Full-or part-time jobs, including sheltered employment and voluntary work |
| Mausbach et al43 | Cross-sectional Baseline | 367 | USA | NR | NR (patients with Jewish background participating in genetic studies) | Outpatients or patients in residential treatment setting (10.6%) | Age (mean): 50.5 yrs (range 21–78 yrs) Males: 62.9% Length of illness: NR Alcohol/substance abuse: NR PANSS neg: 16.1 PANSS pos: 15.6 |
31.9% (sheltered employment 7.1%) | Employed is nonsheltered job for at least 20 hr per week |
| McCreadie44 | Cross-sectional | 316 | Scotland | Multicenter | NR | In-and outpatients | Age (mean): 45 yrs Males: 62% Length of illness: 8 yrs Abuse: alcohol 20%/substance 16% PANSS: NR |
8% | Paid employment, not further specified |
| Mechanic et al45 | Cross-sectional | 320 | USA | Multicenter | NR. Data were derived from the National Health Interview survey on disability 1994/95 | Outpatients | Age (mean): NR Males: NR Length of illness: NR Alcohol/substance abuse: NR PANSS: NR |
Employed 22.5% (CI: 18%–27%) (full-time employed) (≥35 hr) 12% (CI: 8%–16%) | Employed: have been working in the past 2 weeks and not laid off |
| Middelboe et al46 | Cross-sectional | 418 | Denmark, Sweden, Norway, Finland, Iceland | Multicenter | NR. (incl duration of ≥1 year since diagnosed; aged 25–55 years at inclusion; noninstitutional living situation) | Outpatients | Age (mean): 39 yrs Males: 65% Length of illness: 15 yrs Alcohol/substance abuse: NR PANSS: NR |
12% | Employment not specified |
| Mueser et al47 | RCT Baseline + FU | 313 | USA | Multicenter | Current/recent dependence on alcohol or drugs. Not willing to take fluphenazine decanoate injections | NR. Probably outpatients | Mean age: 29.6 yrs (range 19–55) Males: 66.1% Length of illness: NR Alcohol/substance abuse: 0% PANSS: NR |
Baseline: 9.7% (+6.8% other vocational activity, incl sheltered work, volunteer, vocational training, and casual labor) 1-yr FU: 23.3 2-yr FU 21.0 | Competitive employment |
| Ramsay et al48 | Cross-sectional | 181 | USA | Multicenter | No history of outpatient treatment for psychosis or prior hospitalization for psychosis more than 3 months before the admission | Inpatients at inclusion Aged 18–40 yrs | Age (mean): 23.36 yrs Males: 74% Length of illness: NR Alcohol/substance abuse: 55.3% PANSS neg: 21.3 PANSS pos: 23.8 |
Unemployed 65% | Unemployed during month prior to hospitalization |
| Resnick et al49 | RCT Baseline | 1,121 | USA | NR | NR | NR | Age (mean): 41 Males: 73.8% Length of illness: NR Abuse: alcohol 6.5%/substance 10% PANSS neg: 20.25 PANSS pos: 18.3 |
Full time 7.8% part time 10.2% | Paid employment Whether competitive, transitional or sheltered |
| Rosen and Garety50 | Cohort Baseline | 394 | UK | Multicenter | IQ <70, drug/alcohol abuse as primary problem | In-and outpatients | Age (mean): 28.8 yrs (range 16–45) Males: 58.4% Length of illness: NR Alcohol/substance abuse: 22.8% (current or earlier) PANSS: NR |
41.2% Students 11.6% | |
| Slade and Salkever51 | Cohort Baseline | 1,643 | USA | Multicenter | NR | NR. Probably in and outpatients | Age (mean) age: 42 yrs (range 18–78) Males: 63% Length of illness: NR Alcohol/substance abuse: NR PANSS: NR |
21.8% (11.6% nonsupported jobs 10.2% in sheltered or supported jobs) | Working for pay in last 4 weeks |
| Spellmann et al52 | Cohort Baseline + 1-yr FU | 211 | Germany | Multicenter | Major medical illness; alcohol or drug dependency | Baseline: treated as inpatients FU: probably all outpatients | (1-yr FU) Age (mean): 36.6 yrs Males: 52.6% Length of illness: 8.0 yrs Alcohol/substance abuse: 0% PANSS neg: 14.81 PANSS pos: 10.46 |
Baseline: 50.4% (unemployed 29.8%, retired 19.8%) 1-yr FU 43.1% (unemployed 34.1%; retired 16.1%) |
Employment not specified |
| Thornicroft et al53 | Cross-sectional | 404 | the Netherlands, Denmark, UK, Spain, Italy | Multicenter | Current residence in prison, secure residential services or hostels for long-term patients, mental retardation, dementia or severe organic disorder, extended inpatient treatment episode >1 yr | NR. Probably in and outpatients | Age (mean): 41.8 years Males: 57% Length of illness: NR Alcohol/substance abuse: NR PANSS: NR |
17%, sheltered work 4% | Employment (not specified) or student, sheltered work excluded |
| Thorup et al54 | RCT Baseline | 388 | Denmark | Multicenter | Patients with psychiatry symptoms due to organic condition | NR | Age (mean): NR Males: 60.6% Length of illness: NR Alcohol/substance abuse: 30.7% PANSS: NR |
19.6% | Job or education during the whole preceding year |
| Üçok et al55 | Cross-sectional Baseline | 295 | France, Belgium, Germany, Israel, Italy, Spain, Sweden, Turkey, UK | Multicenter | NR | NR | Age (mean): 43.7 years Males: 44.7% Length of illness: NR Alcohol/substance abuse: NR PANSS neg: 20.7 PANSS pos: 16.9 |
17.2% (unemployed 65.7%) | Employed: working in full-time or part-time paid job (students excluded) |
| Usall et al56 | Cohort Baseline | 239 | Spain | Multicenter | Primary diagnosis of alcohol/drug abuse; mental retardation; neurological disease or head trauma | Outpatients | Age (mean): 38.9 yrs Males: 64% Length of illness: 16.8 Alcohol/substance abuse: NR PANSS neg: 26.1 PANSS pos: 14.4 |
27.2% | Employment not specified |
| Uzun et al57 | Cohort Baseline | 116 | Turkey | Single-center | Concomitant neurological or organic brain syndrome or diagnosed with brief drug-related psychoses | Outpatients | Age (median): 59 yrs Males: 54.2% Length of illness: NR Alcohol/substance abuse: 5.2% PANSS: NR |
9.5% (students: 4.3%; unemployed: 86.2%) | Employment not specified |
| Waghorn et al58 | Cross-sectional | 385 | Australia | NA | Long stay hospital inpatients (≥9 weeks) | In-and outpatients | Age (mean): NR Males: 66.5% Length of illness: NR Alcohol/substance abuse: 43.1% (lifetime) PANSS: NR |
Employed 15.8% Unemployed, studying or retired: 84.2% | Employment part time or full time, not further specified |
| West et al59 | Cross-sectional Baseline | 151 | USA | Multicenter | NR | NR | Age (mean): NR Males: 66% Length of illness: NR Alcohol/substance abuse: 18% PANSS: NR |
20% (full-or part-time) Unemployed due to disability 75% Other(including students, retired) 5% | Employment not specified |
| Xie et al60 | RCT of care management Baseline + FU | 152 | USA | Multicenter | NR Note: This is a selective sample (dual diagnosis: schizophrenia or schizoaffective disorder and co-occurring substance abuse/dependence) | In-and outpatients | Baseline: Age (mean): 32.4 yrs Males: 77.6% Length of illness: NR Alcohol/substance abuse: Alcohol 82.7%; cannabis 45%; cocaine 15.2%; other drugs 17.2% PANSS: NR |
Baseline: 6%; FU 1 yr: 14%; FU 2 yrs: 15%; FU 3 yrs: 24% | Competitive job in preceding year, not further specified |
| Ye et al61 | Cohort Baseline + 1-yr FU | 258 | Japan | Multicenter | Patients not treated with risperidone | In-and outpatients | Age (mean): 42 yrs Males: 49.2% Length of illness: 14.1 yrs Alcohol/substance abuse: NR PANSS: NR |
Baseline: overall 9.4%; (outpatients 15.1% inpatients 2.6%) 1-yr FU: 14.4% (outpatients 21.3%; inpatients 6.5%) | Employment is working for pay |
Abbreviations: CI, confidence interval; FU, follow up; IQ, intelligence quotient; NR, not reported; PANSS, positive and negative syndrome scale; RCT, randomized controlled trial; hr, hour; incl, including; pos, positive; neg, negative.
Employment rate
Employment rates ranged from 4% to 50.4%.36,52 Generally, employment rates reported in the studies were based on different definitions of employment, eg, the employment in some studies was limited to competitive employment, while in other studies, respondents with supported or sheltered employment were counted too, and in a number of studies, students and/or housewives and those who had volunteer work were also counted as being employed. Additionally, in a number of studies, the definitions of employment that were applied were not reported. Five studies reported only unemployment figures. The studies differed considerably in design, patient settings, and methods of recruitment. Information on the time frame that was used for measuring employment was generally lacking. In the majority of studies, no distinction was made between respondents with schizophrenia, and schizophreniform or schizoaffective disorders. In addition, respondents may have been diagnosed on the basis of different criteria. This fragmented information limited a direct comparison of employment rates reported in these studies. Consequently, these results did not allow performance of a meta-analysis for estimating an average employment rate among people with schizophrenia.
Factors associated with employment
Disease characteristics
Positive symptoms
Marwaha et al41 examined employment status change during a 2-year European naturalistic study of people with schizophrenia. The researchers found that more positive psychotic symptoms were predictive of job loss.
Negative symptoms
Our review included three studies that reported on associations of negative symptoms and employment. Üçok et al55 reported significantly higher PANSS negative symptoms scores in unemployed respondents in comparison with employed respondents. In addition, regression analyses showed that the PANSS negative symptoms score was an independent predictor of unemployment. Bobes et al23 found that presence of poor rapport and social withdrawal (items of negative PANSS) increased the risk of unemployment. Marwaha et al41 found that besides characteristics of the onset and duration of the disorder, more severe negative symptoms (PANSS subscale) were significantly negatively associated with the chance of getting work during a 2-year follow-up study.
Cognitive symptoms
Associations of cognitive symptoms and employment were reported in three studies in our review. Giugiario et al30 reported significantly higher scores of verbal memory and more awareness of illness in respondents with competitive employment in comparison with unemployed subjects. In a longitudinal study, Holthausen et al35 found more problems of vocational functioning and significant lower chances of competitive employment in persons with cognitive deficits. Hofer et al34 found that poorer cognitive scores were associated with a reduced probability of competitive employment.
Treatment setting
Another, more indirect indicator of disease severity may be the setting in which people receive care, ie, in-or outpatient care. Most studies included both in-and outpatient treated people. A number of studies did not provide information on the treatment setting. Ten studies included only persons treated in an outpatient setting. Employment rates varied considerably, from 9.5% to 42.6%. No study was found exclusively focusing on inpatients. Only in the study of Ye et al61 were figures of employment rates for in-and outpatients separately presented. Both the baseline and follow-up employment rates in persons treated as outpatients were almost four times higher in comparison with the rates among inpatients.
Age at onset, course, and duration
Marwaha et al examined predictors of being employed during a 2-year follow-up, using cross-national data derived from Germany, France, and the UK.41 Later age of illness onset, longer duration of illness, and a continuous illness course were negatively associated with the chance of getting work. Üçok et al reported significantly higher remission rates among employed subjects in comparison with unemployed subjects, and longer duration of remission contributed positively to employment status.55 Fourteen studies in our review reported on the duration of the illness.20,21,23,24,30,34,36,37,42,44,46,52,56,61 A comparison of the employment rates and the duration of the disorder between these studies did not show a consistent pattern of declining rates with longer duration of the disorder. For example, McCreadie44 reported an employment rate of 8% in study participants, with an average duration of 8 years, while Middelboe et al46 reported an employment rate of 12% in participants, with an average duration of 15 years.
Alcohol and substance abuse
In the study of Marwaha et al harmful use of alcohol at baseline was a significant predictor of job loss during a 2-year follow up.41 In our review, 22 studies included information about the proportion of respondents with alcohol or substance abuse. The study of Xie et al60 included only patients with co-occurring substance abuse. The employment rate was 6% at baseline and increased to 24% at 3-year follow up. In three studies, respondents with alcohol/substance abuse were excluded.34,47,52 Employment rates reported in these studies were 43.1% (1-year follow up), 27.8% (baseline), and 23.3% (1-year follow up), respectively. The figures presented in these studies are difficult to interpret given the different definitions of employment in these studies. In addition, in the study of Spellmann et al52 no definition of employment was stated.
Characteristics of the individual
Marwaha and Johnson3 reported on a number of demographic factors related to being employed in people with schizophrenia in their review, eg, sex, and marital and accommodation status. However, the authors reported that these associations were not consistently replicated between different studies. Among the studies in our review, Üçok et al55 found that younger age, more education, and sex (male) were independent positive predictors of employment. Hofer et al34 found that premorbid school functioning was positively correlated with competitive employment, and older age was found to be a significant negative predictor of employment.
Characteristics of the environment
Studies that examined environmental factors and the subject of employment were limited.
Marwaha et al42 conducted a study to compare employment patterns and associated environmental factors between and within three European countries: UK, France, and Germany. Variation in employment rate was found both between countries and between regional sites. The greatest variation was found on the national level, between centers rather than between countries. The authors suggested that social and vocational service factors within and between countries may contribute to this variation. One of these factors may be the availability of vocational services and placements, as was seen in Germany. In two other studies that were performed in Germany, relatively high employment rates were reported.39,52 The low employment rate among people with schizophrenia in the UK reported by Marwaha et al42 and Thornicroft et al53 was not confirmed by the study by Rosen and Garety.50 In the latter study, an employment rate of 41.2% (excluding 12% students) was reported.
In the study of Thornicroft et al53 including patients from five different European countries, relatively higher employment rates were found in southern countries (Spain and Italy) in comparison with Denmark and the Netherlands. The authors suggested that differences may be associated with differences in the availability of welfare benefits. Comparative low employment rates (12% in outpatients) in Scandinavian countries were also reported by Middelboe et al.46 In line with these findings, Giugiario et al30 reported a competitive employment rate of 30% in people with schizophrenia treated in an outpatient setting in Italy. Comparable figures were reported for outpatients in Spain (25.9% respectively 27.2%).23,56 Two studies were performed in Turkey.37,57 In the study of Karadayi et al37 employment was 37.3%. However, the employment rate, including students, reported by Uzun et al57 was substantially lower (13.8%). This may partly be explained by the relatively older sample of the study population (median age 59 years).
HRQoL
In total, 12 studies were found that investigated the HRQoL of people with schizophrenia. Eight studies20,24,25,53,62–65 used a disease-specific HRQoL instrument: the Subjective Quality of Life (S-QoL) (one study), Heinrichs–Carpenter Quality of Life (QoL) scale (three studies), Lancaster Quality of Life Profile (two studies), and Lehman’s Quality of Life Interview (QOLI) (two studies). Just one of the studies a generic HRQoL instrument was applied the Wisconsin Quality of Life Index (W-QLI) scale,25 and two studies applied a generic preference-based instrument (EQ-5D™ and Quality of Wellbeing).20,64 In nine of the 12 studies, the relationship between employment and HRQoL was studied (Table 2). All but one of the studies found a positive relationship between being employed and HRQoL. In the study by Xie et al60 which applied Lehman’s QOLI instrument, a nearly significant relationship (P=0.05) was established.
Table 2.
Employment and health-related quality of life
| Author | Cross-sectional design (Y/N) | N | Country | In/outpatients | Multi/single-center | HRQoL instrument | Type of HRQoL instrument | Result on relationship employment-HRQoL |
|---|---|---|---|---|---|---|---|---|
| Alonso et al20 | Y (cohort at baseline and follow-up) | 9,340 | Europe | Outpatients | Multicenter | EQ-5D™ | Generic, preference-based | Baseline utility scores were significantly higher (P<0.0001) for patients with paid employment compared with patients without. Also, paid employment was associated with greater improvement in utility score in the first and third year after treatment with antipsychotics |
| Boyer et al24 | Y | 113 | France | Outpatients | Single-center | S-QoL 18 | Disease-specific (for patients with schizophrenia) | Significant relationship between being employed and psychological well-being (based on multiple linear regression analysis) |
| Caron et al25 | Y (cohort at baseline) | 181 | Canada | Outpatients + probably <10% inpatients | Multicenter | Wisconsin QoL Index (CaW-QLI) | Generic, descriptive | Employed clients had higher QoL scores on the domains of physical health, social relation and support, and a higher global QoL score |
| Eklund et al62 | Y | 74 | Sweden | Outpatients | Single-center | Lancashire Quality of Life Profile | Disease-specific (for patients with severe psychiatric disorders) | Employed people had a significant better interviewer-rated HRQoL, self-rated HRQoL, and self-esteem |
| Marwaha et al63 | Y | 1,208 | Europe | Multicenter | Lehman’s QOLI | Disease-specific (for persons with severe mental illness) | Employment status was significantly associated with subjective QoL score (B=0.18, P=0.002) | |
| Palmer et al64 | Y | 82 | USA | Inpatients | QWB | Generic, preference-based | QWB total score was significantly correlated with being historically employed (r=0.27, P<0.05) | |
| Rosenheck et al65 | Y (cohort at baseline) | 1,424 | USA | In-and outpatients | Multicenter | Heinrichs-Carpenter QoL Scale | Disease-specific (for patients with schizophrenia) | Patients with competitive paid employment scored significantly higher (P<0.0001) on all domains of the QLS than did patients with other or no vocational activity On the domains “instrumental activity” and “object/activity”, patients with competitive employment scored higher than did patients in other kinds of employment who, in turn, scored higher than those not working |
| Thornicroft et al53 | Y | 404 | Europe | NR probably in and outpatients | Multicenter | Lancashire Quality of Life Profile | Disease-specific (for patients with severe psychiatric disorders) | Having work is a significant predictor of subjective HRQoL (not specified) |
| Xie et al60 | Y (QoL and employment at follow-up treatment study) | 152 | USA | In-and outpatients | Multicenter | Lehman’s QOLI | Disease-specific (for persons with severe mental illness) | No significant correlation (P=0.05) was found between QOLI-general life satisfaction score and having a competitive job in the past year |
Abbreviations: CaW-QLI, the Wisconsin Quality of Life Index-Canadian version; HRQoL, health-related quality of life; NR, not reported; QLS, quality of life scale; QoL, quality of life; QOLI, quality of life interview; QWB, quality of wellbeing; S-QoL, subjective quality of life.
Discussion
Our review study showed that employment rates in people with schizophrenia vary between 4.5% and over 50%. There were significant differences between the definitions of employment that were applied in the studies. Nevertheless, unemployment figures are even more difficult to interpret, since these rates may refer to only those looking for work, while other rates may include respondents with long-term disability benefits or pensions. The comparison of employment rates between studies is further limited by differences in study designs, recruitment methods, diagnostic instruments, clinical variables reported, and different time frames for measuring employment. However, generally, employment in people with schizophrenia is relatively low, as was reported in the study of Marwaha et al.42 In that study, employment rates were presented for people with schizophrenia in the UK (12.9%), France (11.5%), and Germany (30.2%) in comparison with employment rates in the general population of these countries (of 71.0%, 62.2%, and 65.4%, respectively). Due to the methodological differences between the studies, we were unable to make a valid estimation of an average employment rate.
In addition to employment rates, we screened the papers on factors associated with employment, including the association of employment and HRQoL. The most frequently reported disease characteristics that were negatively associated with employment were negative symptoms and cognitive symptoms. This is in line with the earlier findings reported by of Marwaha and Johnson.3 Additionally, later age of disease onset, and the duration and continuous course of the disease may play a role in employment status of the person. Finally, employment rates were higher in people treated in an outpatient setting in comparison with rates among inpatients. It is not clear to what extent this finding is related to the severity of the disease. Both individual and environmental characteristics were found to be associated with employment rates. Individual characteristics associated with unemployment were (older) age, lower education, and sex (females). Additionally, employment rates were associated with a number of environmental factors. The large variation of employment rates between countries or regions seem to indicate that environmental characteristics, such as the availability of welfare benefits and the availability of vocational services and sheltered employment, may play an important role. Employment rates seem to be lower in countries with an increased level of social security, as was reported in the study of Thornicroft et al.53 Relatively higher employment rates were generally found in studies performed in southern European countries. It can be assumed that these higher rates may be associated with dependence on the financial support of family members. These findings are in line with the study of Kilian and Becker, of the macroeconomic indicators of labor force participation of people with schizophrenia.66 In addition, they found a close relation between general employment rates and employment rates of people with schizophrenia. In another study, a negative association was found between competitive employment and receipt of disability payment. Van der Wel et al reports that studies on the association of nonemployment among people with limiting longstanding illness and differences in welfare policies show equivocal results.67 More research is recommended for assessing associations of welfare policy and employment in patients with severe mental illness.
Several studies suggested that the availability of vocational service factors may contribute to employment in people with schizophrenia. Increased access to rehabilitation services was associated with participation in both competitive and noncompetitive employment.65
Generally, being employed and HRQoL were positively associated. A possible explanation for the association between being employed and HRQoL that was found in our review was indicated by Brekke et al68 who described self-esteem to be a mediating factor between being employed and HRQoL. A larger social network due to being employed, resulting in a better HRQoL, is being proposed as another potential explanation.25 Most studies applied a disease-specific HRQoL instrument. This seems in line with the current discussion about the validity of preference-based QoL instruments in people with schizophrenia. It is argued that generic preference-based instruments may not be appropriate for use in people with schizophrenia.69
The conceptual model of Wilson and Cleary was a helpful tool to describe the different factors associated with employment and HRQoL.9 The model has been widely applied to different patient populations.9 In the current review we found studies that reported on associations between disease characteristics, individual characteristics and environmental characteristics and employment. Another important question relates to the association between employment and HRQol. That is, while employment may increase QoL, it is likely that those with higher QoL are more likely to be employed. Currently, there is little literature adequately assessing the causal relationship between these two domains, leading to a methodological gap in the literature. A limitation of our study is that we focused our literature search primarily on employment rates rather than on factors associated with employment. Consequently, we did not perform separate searches for factors associated with employment. However, due to the broad approach that was applied for reviewing the literature, the number of missing studies is assumed to be limited. Finally, we excluded studies on Individual Placement and Support and other vocational support programs, as our primary goal was to assess the general employment rate in people with schizophrenia. Supported employment programs are evidence-based practices to enhance people with mental health disability to return to work. Employment rates of persons with schizophrenia included in supported employment trials may differ due to specific in-and exclusion criteria.
In conclusion, our review showed a great variation in employment rates in people with schizophrenia. However, the overall employment rate was low. Employment rates varied widely across and within countries. Generally, there was a positive association between being employed and HRQoL. Importantly, however, the causal direction of this association remained unclear. When aiming to improve employment participation and associated HRQoL among people diagnosed with schizophrenia, symptoms, functional status, demographic characteristics of the population, and environmental factors should be taken into account. A better understanding of the interrelations of these components could lead to more integrated and personalized health management, and outcome optimization, for people with schizophrenia.
Supplementary material
(“schizophrenia”[MeSH Terms]
OR “schizophrenia”[All Fields])
AND
(“employment”[MeSH Terms]
OR “employment”[All Fields])
OR (“unemployment”[MeSH Terms]
OR “unemployment”[All Fields])
OR (paid[All Fields]
AND
(“work”[MeSH Terms]
OR “work”[All Fields]))
OR ((“work”[MeSH Terms]
OR “work”[All Fields])
AND
capacity[All Fields])
OR “efficiency”[MeSH Terms]
OR “efficiency”[All Fields]
OR “productivity”[All Fields])
OR (“absenteeism”[MeSH Terms]
OR “absenteeism”[All Fields])
OR “presenteeism”[All Fields]
OR (“occupations”[MeSH Terms]
OR “occupations”[All Fields]
OR “occupation”[All Fields])
AND
((hasabstract[text]
AND
“loattrfull text”[sb])
AND
(“2000/01/01”[PDAT] : “2013/12/31”[PDAT])
AND
“humans”[MeSH Terms]
AND
English[lang]
AND
“adult”[MeSH Terms])
Acknowledgments
The study was financed through an unrestricted grant of F. Hoffmann-La Roche.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Boardman J, Grove B, Perkins R, Shepherd G. Work and employment for people with psychiatric disabilities. Br J Psychiatry. 2003;182:467–468. doi: 10.1192/bjp.182.6.467. [DOI] [PubMed] [Google Scholar]
- 2.Mangalore R, Knapp M. Cost of schizophrenia in England. J Ment Health Policy Econ. 2007;10(1):23–41. [PubMed] [Google Scholar]
- 3.Marwaha S, Johnson S. Schizophrenia and employment – a review. Soc Psychiatry Psychiatr Epidemiol. 2004;39(5):337–349. doi: 10.1007/s00127-004-0762-4. [DOI] [PubMed] [Google Scholar]
- 4.Gladis MM, Gosch EA, Dishuk NM, Crits-Christoph P. Quality of life: expanding the scope of clinical significance. J Consult Clin Psychol. 1999;67(3):320–331. doi: 10.1037//0022-006x.67.3.320. [DOI] [PubMed] [Google Scholar]
- 5.Priebe S, Warner R, Hubschmid T, Eckle I. Employment, attitudes toward work, and quality of life among people with schizophrenia in three countries. Schizophr Bull. 1998;24(3):469–477. doi: 10.1093/oxfordjournals.schbul.a033341. [DOI] [PubMed] [Google Scholar]
- 6.Sullivan G, Wells KB, Leake B. Clinical factors associated with better quality of life in a seriously mentally ill population. Hosp Community Psychiatry. 1992;43(8):794–798. doi: 10.1176/ps.43.8.794. [DOI] [PubMed] [Google Scholar]
- 7.Lehman AF, Postrado LT, Rachuba LT. Convergent validation of quality of life assessments for persons with severe mental illnesses. Qual Life Res. 1993;2(5):327–333. doi: 10.1007/BF00449427. [DOI] [PubMed] [Google Scholar]
- 8.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA. 1995;273(1):59–65. [PubMed] [Google Scholar]
- 10.Coons SJ, Rao S, Keininger DL, Hays RD. A comparative review of generic quality-of-life instruments. Pharmacoeconomics. 2000;17(1):13–35. doi: 10.2165/00019053-200017010-00002. [DOI] [PubMed] [Google Scholar]
- 11.van Os J, Kapur S. Schizophrenia. Lancet. 2009;374(9690):635–645. doi: 10.1016/S0140-6736(09)60995-8. [DOI] [PubMed] [Google Scholar]
- 12.van Os J, Kenis G, Rutten BPF. The environment and schizophrenia. Nature. 2010;468(7321):203–212. doi: 10.1038/nature09563. [DOI] [PubMed] [Google Scholar]
- 13.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 14.Dixon L. Dual diagnosis of substance abuse in schizophrenia: prevalence and impact on outcomes. Schizophr Res. 1999;35(Suppl):S93–S100. doi: 10.1016/s0920-9964(98)00161-3. [DOI] [PubMed] [Google Scholar]
- 15.Westermeyer J. Comorbid schizophrenia and substance abuse: a review of epidemiology and course. Am J Addict. 2006;15(5):345–355. doi: 10.1080/10550490600860114. [DOI] [PubMed] [Google Scholar]
- 16.Carrà G, Johnson S, Bebbington P, et al. The lifetime and past-year prevalence of dual diagnosis in people with schizophrenia across Europe: findings from the European Schizophrenia Cohort (EuroSC) Eur Arch Psychiatry Clin Neurosci. 2012;262(7):607–616. doi: 10.1007/s00406-012-0305-z. [DOI] [PubMed] [Google Scholar]
- 17.Salyers MP, Mueser KT. Social functioning, psychopathology, and medication side effects in relation to substance use and abuse in schizophrenia. Schizophr Res. 2001;48(1):109–123. doi: 10.1016/s0920-9964(00)00063-3. [DOI] [PubMed] [Google Scholar]
- 18.Chan S, Yu Iu W. Quality of life of clients with schizophrenia. J Adv Nurs. 2004;45(1):72–83. doi: 10.1046/j.1365-2648.2003.02863.x. [DOI] [PubMed] [Google Scholar]
- 19.Abdel-Baki A, Lesage A, Nicole L, Cossette M, Salvat E, Lalonde P. Schizophrenia, an illness with bad outcome: myth or reality? Can J Psychiatry. 2011;56(2):92–101. doi: 10.1177/070674371105600204. [DOI] [PubMed] [Google Scholar]
- 20.Alonso J, Croudace T, Brown J, et al. Health-related quality of life (HRQL) and continuous antipsychotic treatment: 3-year results from the Schizophrenia Health Outcomes (SOHO) study. Value Health. 2009;12(4):536–543. doi: 10.1111/j.1524-4733.2008.00495.x. [DOI] [PubMed] [Google Scholar]
- 21.Ascher-Svanum H, Zhu B, Faries D, Peng X, Kinon BJ, Tohen M. Tardive dyskinesia and the 3-year course of schizophrenia: results from a large, prospective, naturalistic study. J Clin Psychiatry. 2008;69(10):1580–1588. doi: 10.4088/jcp.v69n1008. [DOI] [PubMed] [Google Scholar]
- 22.Barbui C, Kikkert M, Mazzi MA, et al. Comparison of patient and clinician perspectives in the assessment of antipsychotic medication adherence. Psychopathology. 2009;42(5):311–317. doi: 10.1159/000232973. [DOI] [PubMed] [Google Scholar]
- 23.Bobes J, Arango C, Garcia-Garcia M, Rejas J, CLAMORS Study Collaborative Group Prevalence of negative symptoms in outpatients with schizophrenia spectrum disorders treated with antipsychotics in routine clinical practice: findings from the CLAMORS study. J Clin Psychiatry. 2010;71(3):280–286. doi: 10.4088/JCP.08m04250yel. [DOI] [PubMed] [Google Scholar]
- 24.Boyer L, Aghababian V, Richieri R, et al. Insight into illness, neurocognition and quality of life in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2012;36(2):271–276. doi: 10.1016/j.pnpbp.2011.10.008. [DOI] [PubMed] [Google Scholar]
- 25.Caron J, Mercier C, Diaz P, Martin A. Socio-demographic and clinical predictors of quality of life in patients with schizophrenia or schizo-affective disorder. Psychiatry Res. 2005;137(3):203–213. doi: 10.1016/j.psychres.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 26.Cechnicki A, Angermeyer MC, Bielańska A. Anticipated and experienced stigma among people with schizophrenia: its nature and correlates. Soc Psychiatry Psychiatr Epidemiol. 2011;46(7):643–650. doi: 10.1007/s00127-010-0230-2. [DOI] [PubMed] [Google Scholar]
- 27.Chwastiak LA, Rosenheck RA, McEvoy JP, Keefe RS, Swartz MS, Lieberman JA. Interrelationships of psychiatric symptom severity, medical comorbidity, and functioning in schizophrenia. Psychiatr Serv. 2006;57(8):1102–1109. doi: 10.1176/ps.2006.57.8.1102. [DOI] [PubMed] [Google Scholar]
- 28.Compton MT, Rudisch BE, Weiss PS, West JC, Kaslow NJ. Predictors of psychiatrist-reported treatment-compliance problems among patients in routine U.S. psychiatric care. Psychiatry Res. 2005;137(1–2):29–36. doi: 10.1016/j.psychres.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 29.Cuyún Carter GB, Milton DR, Ascher-Svanum H, Faries DE. Sustained favorable long-term outcome in the treatment of schizophrenia: a 3-year prospective observational study. BMC Psychiatry. 2011;11:143. doi: 10.1186/1471-244X-11-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Giugiario M, Crivelli B, Mingrone C, et al. Cognitive function and competitive employment in schizophrenia: relative contribution of insight and psychopathology. Soc Psychiatry Psychiatr Epidemiol. 2012;47(4):553–561. doi: 10.1007/s00127-011-0367-7. [DOI] [PubMed] [Google Scholar]
- 31.Gureje O, Herrman H, Harvey C, Morgan V, Jablensky A. The Australian National Survey of Psychotic Disorders: profile of psychosocial disability and its risk factors. Psychol Med. 2002;32(4):639–647. doi: 10.1017/s0033291702005627. [DOI] [PubMed] [Google Scholar]
- 32.Hansson L, Svensson B, Björkman T, et al. What works for whom in a computer-mediated communication intervention in community psychiatry? Moderators of outcome in a cluster randomized trial. Acta Psychiatr Scand. 2008;118(5):404–409. doi: 10.1111/j.1600-0447.2008.01258.x. [DOI] [PubMed] [Google Scholar]
- 33.Henry LP, Amminger GP, Harris MG, et al. The EPPIC follow-up study of first-episode psychosis: longer-term clinical and functional outcome 7 years after index admission. J Clin Psychiatry. 2010;71(6):716–728. doi: 10.4088/JCP.08m04846yel. [DOI] [PubMed] [Google Scholar]
- 34.Hofer A, Bodner T, Kaufmann A, et al. Symptomatic remission and neurocognitive functioning in patients with schizophrenia. Psychol Med. 2011;41(10):2131–2139. doi: 10.1017/S0033291711000353. [DOI] [PubMed] [Google Scholar]
- 35.Holthausen EA, Wiersma D, Cahn W, et al. Predictive value of cognition for different domains of outcome in recent-onset schizophrenia. Psychiatry Res. 2007;149(1–3):71–80. doi: 10.1016/j.psychres.2005.07.037. [DOI] [PubMed] [Google Scholar]
- 36.Honkonen T, Stengård E, Virtanen M, Salokangas RK. Employment predictors for discharged schizophrenia patients. Soc Psychiatry Psychiatr Epidemiol. 2007;42(5):372–380. doi: 10.1007/s00127-007-0180-5. [DOI] [PubMed] [Google Scholar]
- 37.Karadayi G, Emiroğlu B, Uçok A. Relationship of symptomatic remission with quality of life and functionality in patients with schizophrenia. Compr Psychiatry. 2011;52(6):701–707. doi: 10.1016/j.comppsych.2010.11.012. [DOI] [PubMed] [Google Scholar]
- 38.Kulkarni J, de Castella AR, Filia KM, et al. Australian Schizophrenia Care and Assessment Programme: real-world schizophrenia: outcomes. Aust N Z J Psychiatry. 2007;41(12):969–979. doi: 10.1080/00048670701689410. [DOI] [PubMed] [Google Scholar]
- 39.Lambert M, Schimmelmann BG, Naber D, et al. Prediction of remission as a combination of symptomatic and functional remission and adequate subjective well-being in 2,960 patients with schizophrenia. J Clin Psychiatry. 2006;67(11):1690–1697. doi: 10.4088/jcp.v67n1104. [DOI] [PubMed] [Google Scholar]
- 40.Mackell JA, Harrison DJ, McDonnell DD. Relationship between preventative physical health care and mental health in individuals with schizophrenia: a survey of caregivers. Ment Health Serv Res. 2005;7(4):225–228. doi: 10.1007/s11020-005-7454-x. [DOI] [PubMed] [Google Scholar]
- 41.Marwaha S, Johnson S, Bebbington PE, et al. Predictors of employment status change over 2 years in people with schizophrenia living in Europe. Epidemiol Psichiatr Soc. 2009;18(4):344–351. [PubMed] [Google Scholar]
- 42.Marwaha S, Johnson S, Bebbington P, et al. Rates and correlates of employment in people with schizophrenia in the UK, France and Germany. Br J Psychiatry. 2007;191:30–37. doi: 10.1192/bjp.bp.105.020982. [DOI] [PubMed] [Google Scholar]
- 43.Mausbach BT, Depp CA, Bowie CR, et al. Sensitivity and specificity of the UCSD Performance-based Skills Assessment (UPSA-B) for identifying functional milestones in schizophrenia. Schizophr Res. 2011;132(2–3):165–170. doi: 10.1016/j.schres.2011.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McCreadie RG, Scottish Comorbidity Study Group Use of drugs, alcohol and tobacco by people with schizophrenia: case-control study. Br J Psychiatry. 2002;181:321–325. doi: 10.1192/bjp.181.4.321. [DOI] [PubMed] [Google Scholar]
- 45.Mechanic D, Blider S, McAlpine DD. Employing persons with serious mental illness. Health Aff (Millwood) 2002;21(5):242–253. doi: 10.1377/hlthaff.21.5.242. [DOI] [PubMed] [Google Scholar]
- 46.Middelboe T, Mackeprang T, Hansson L, et al. The Nordic Study on schizophrenic patients living in the community. Subjective needs and perceived help. Eur Psychiatry. 2001;16(4):207–214. doi: 10.1016/s0924-9338(01)00566-1. [DOI] [PubMed] [Google Scholar]
- 47.Mueser KT, Salyers MP, Mueser PR. A prospective analysis of work in schizophrenia. Schizophr Bull. 2001;27(2):281–296. doi: 10.1093/oxfordjournals.schbul.a006874. [DOI] [PubMed] [Google Scholar]
- 48.Ramsay CE, Stewart T, Compton MT. Unemployment among patients with newly diagnosed first-episode psychosis: prevalence and clinical correlates in a U.S. sample. Soc Psychiatry Psychiatr Epidemiol. 2012;47(5):797–803. doi: 10.1007/s00127-011-0386-4. [DOI] [PubMed] [Google Scholar]
- 49.Resnick SG, Rosenheck RA, Canive JM, et al. Employment outcomes in a randomized trial of second-generation antipsychotics and perphenazine in the treatment of individuals with schizophrenia. J Behav Health Serv Res. 2008;35(2):215–225. doi: 10.1007/s11414-007-9101-3. [DOI] [PubMed] [Google Scholar]
- 50.Rosen K, Garety P. Predicting recovery from schizophrenia: a retrospective comparison of characteristics at onset of people with single and multiple episodes. Schizophr Bull. 2005;31(3):735–750. doi: 10.1093/schbul/sbi017. [DOI] [PubMed] [Google Scholar]
- 51.Slade E, Salkever D. Symptom effects on employment in a structural model of mental illness and treatment: analysis of patients with schizophrenia. J Ment Health Policy Econ. 2001;4(1):25–34. [PubMed] [Google Scholar]
- 52.Spellmann I, Riedel M, Schennach R, et al. One-year functional outcomes of naturalistically treated patients with schizophrenia. Psychiatry Res. 2012;198(3):378–385. doi: 10.1016/j.psychres.2011.12.047. [DOI] [PubMed] [Google Scholar]
- 53.Thornicroft G, Tansella M, Becker T, et al. EPSILON Study Group The personal impact of schizophrenia in Europe. Schizophr Res. 2004;69(2–3):125–132. doi: 10.1016/s0920-9964(03)00191-9. [DOI] [PubMed] [Google Scholar]
- 54.Thorup A, Petersen L, Jeppesen P, et al. Gender differences in young adults with first-episode schizophrenia spectrum disorders at baseline in the Danish OPUS study. J Nerv Ment Dis. 2007;195(5):396–405. doi: 10.1097/01.nmd.0000253784.59708.dd. [DOI] [PubMed] [Google Scholar]
- 55.Üçok A, Gorwood P, Karadayı G, EGOFORS Employment and its relationship with functionality and quality of life in patients with schizophrenia: EGOFORS Study. Eur Psychiatry. 2012;27(6):422–425. doi: 10.1016/j.eurpsy.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 56.Usall J, Araya S, Ochoa S, Busquets E, Gost A, Márquez M, Assessment Research Group in Schizophrenia (NEDES) Gender differences in a sample of schizophrenic outpatients. Compr Psychiatry. 2001;42(4):301–305. doi: 10.1053/comp.2001.24582. [DOI] [PubMed] [Google Scholar]
- 57.Uzun O, Cansever A, Basoğlu C, Ozşahin A. Smoking and substance abuse in outpatients with schizophrenia: a 2-year follow-up study in Turkey. Drug Alcohol Depend. 2003;70(2):187–192. doi: 10.1016/s0376-8716(02)00362-9. [DOI] [PubMed] [Google Scholar]
- 58.Waghorn G, Chant D, Jaeger J. Employment functioning and disability among community residents with bipolar affective disorder: results from an Australian community survey. Bipolar Disord. 2007;9(1–2):166–182. doi: 10.1111/j.1399-5618.2007.00417.x. [DOI] [PubMed] [Google Scholar]
- 59.West JC, Wilk JE, Olfson M, et al. Patterns and quality of treatment for patients with schizophrenia in routine psychiatric practice. Psychiatr Serv. 2005;56(3):283–291. doi: 10.1176/appi.ps.56.3.283. [DOI] [PubMed] [Google Scholar]
- 60.Xie H, McHugo GJ, Helmstetter BS, Drake RE. Three-year recovery outcomes for long-term patients with co-occurring schizophrenic and substance use disorders. Schizophr Res. 2005;75(2–3):337–348. doi: 10.1016/j.schres.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 61.Ye W, Fujikoshi S, Nakahara N, Takahashi M, Ascher-Svanum H, Ohmori T. Improved outcomes following a switch to olanzapine treatment from risperidone treatment in a 1-year naturalistic study of schizophrenia patients in Japan. Psychiatry Clin Neurosci. 2012;66(4):313–321. doi: 10.1111/j.1440-1819.2012.02351.x. [DOI] [PubMed] [Google Scholar]
- 62.Eklund M, Hansson L, Bejerholm U. Relationships between satisfaction with occupational factors and health-related variables in schizophrenia outpatients. Soc Psychiatry Psychiatr Epidemiol. 2001;36(2):79–83. doi: 10.1007/s001270050293. [DOI] [PubMed] [Google Scholar]
- 63.Marwaha S, Johnson S, Bebbington P, et al. EuroSC Study Group Correlates of subjective quality of life in people with schizophrenia: findings from the EuroSC study. J Nerv Ment Dis. 2008;196(2):87–94. doi: 10.1097/NMD.0b013e318162aa9c. [DOI] [PubMed] [Google Scholar]
- 64.Palmer BW, Heaton RK, Gladsjo JA, et al. Heterogeneity in functional status among older outpatients with schizophrenia: employment history, living situation, and driving. Schizophr Res. 2002;55(3):205–215. doi: 10.1016/s0920-9964(01)00218-3. [DOI] [PubMed] [Google Scholar]
- 65.Rosenheck R, Leslie D, Keefe R, et al. CATIE Study Investigators Group Barriers to employment for people with schizophrenia. Am J Psychiatry. 2006;163(3):411–417. doi: 10.1176/appi.ajp.163.3.411. [DOI] [PubMed] [Google Scholar]
- 66.Kilian R, Becker T. Macro-economic indicators and labour force participation of people with schizophrenia. J Ment Health. 2007;16(2):211–222. [Google Scholar]
- 67.van der Wel KA, Dahl E, Thielen K. Social inequalities in ‘sickness’: European welfare states and non-employment among the chronically ill. Soc Sci Med. 2011;73(11):1608–1617. doi: 10.1016/j.socscimed.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 68.Brekke JS, Levin S, Wolkon GH, Sobel E, Slade E. Psychosocial functioning and subjective experience in schizophrenia. Schizophr Bull. 1993;19(3):599–608. doi: 10.1093/schbul/19.3.599. [DOI] [PubMed] [Google Scholar]
- 69.Papaioannou D, Brazier J, Parry G. How valid and responsive are generic health status measures, such as EQ-5D and SF-36, in schizophrenia? A systematic review. Value Health. 2011;14(6):907–920. doi: 10.1016/j.jval.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]