Abstract
Diabetes education to improve patient self-management is an important component of comprehensive diabetes care. Patients with low health literacy and numeracy may have difficulty translating information from traditional diabetes educational programs and materials into effective self-care. To address this potential barrier to successful diabetes teaching and counseling, we describe the development of the Diabetes Literacy and Numeracy Education Toolkit (DLNET) and opportunities for its use in clinical practice. The DLNET is composed of 24 interactive modules covering standard diabetes care topics that can be customized to individual patient needs and utilized by all members of the multidisciplinary diabetes care team. The material’s content and formatting aims to improve the ease of use for diabetes patients with low literacy and numeracy by adhering to a lower text reading level, using illustrations for key concepts, and color-coding and other accommodations to guide patients through instructions for self-care. Individual sections of the DLNET may be provided to patients for initial teaching, as well as for reinforcement. While designed for lower literacy and numeracy skills, the DLNET provides unique materials to facilitate diabetes education for all patients.
Introduction
Low health literacy and numeracy are very common in the United States, with estimates that over 90 million people have basic or below basic literacy skills and 110 million people have limited quantitative skills.1 Diabetes patients with poor literacy and numeracy skills may have difficulty interpreting glucose readings, calculating carbohydrate intake, adjusting medications, and performing other daily self-management tasks. In recent studies, lower health literacy has been associated with less diabetes knowledge2–4 and worse glycemic control.5 Recently, numeracy, the ability to understand and use numbers in daily life6, has also been shown to be associated with glycemic control.7 In a study of 398 patients with diabetes, although 83% had previous diabetes education, many patients demonstrated significant problems with numeracy related diabetes skills. For example, more than 25% of patients could not determine what glucose meter readings were within a normal range of 80–120 mg/dL; 56% of patients could not calculate the total carbohydrate content in a container of snack chips, and 59% could not accurately calculate an insulin dosage based on glucose level and carbohydrate intake.
Participation in a diabetes self management education program is recommended by the American Association of Diabetes Educators (AADE) and the American Diabetes Association for all people with diabetes at diagnosis and as needed thereafter.8, 9 When diabetes education is combined with appropriate medical management, glycemic control can improve significantly.10–12 However, health education materials, including diabetes education materials, are often written at high reading levels with poor usability characteristics for patients with lower literacy.13 Many people with diabetes may not receive the maximal benefit from current diabetes education materials. Recent studies suggest that a comprehensive diabetes management program that utilizes a multidisciplinary approach including addressing health literacy may be particularly beneficial for improving glycemic control in patients with lower literacy.14, 15 Additionally, the AADE advocates individualization of diabetes self-management education tailored to meet individual literacy level and learning style preferences.9
With the goal of improving diabetes self-management education for all patients, we developed a literacy and numeracy-sensitive toolkit to be used by patients and providers to address the many complex areas of diabetes care. The materials were simplified, categorized into modules, and created to be individualized to meet the needs of a heterogeneous group of patients. While the toolkit was designed to help patients with lower literacy or numeracy skills, we believe that the toolkit can benefit all patients with diabetes, regardless of their literacy level. This article describes the development, application and utility of the Diabetes Literacy and Numeracy Education Toolkit (DLNET). A complete version of the DLNET is available at: http://www.mc.vanderbilt.edu/diabetes/drtc/preventionandcontrol/tools.php.
Development of the Diabetes Literacy and Numeracy Education Toolkit
The Diabetes Literacy and Numeracy Education Toolkit (DLNET) was developed to facilitate the educational and medical management needs of patients with diabetes. The American Diabetes Association (ADA) and the American Association of Diabetes Educators (AADE) standards of care for diabetes education were the basis for determining the content of the DLNET.8 A multidisciplinary team, including experts in health literacy and numeracy, physicians, Certified Diabetes Educator (CDE) registered dietitians (RD), an Advanced Diabetes Management (BC-ADM) nurse practitioner, and a clinical pharmacist CDE, determined the specific content of the DLNET. Educators all had ten or more years of experience in diabetes education and management. Educational psychologists from Vanderbilt University Peabody College of Education, who were experts in providing instruction for persons with limited reading and math skills, provided additional feedback on the toolkit content and format. Patients with varying levels of literacy also provided assessment on the usability of the materials at both the initial and refinement stages of development of the DLNET.
While the informational content of the DLNET is consistent with traditional diabetes education materials, the format and presentation of the information was created to ease its use for patients with lower literacy or numeracy skills. Design of the DLNET was based upon concepts of clear health communication including the following: (1) simple wording and short sentences with a goal reading level of 4th–6th grade (2) information limited to key points, and minimizing disease statistics, anatomy and physiology to only the basic information required to understand the key point (3) focus on key actions and desired behaviors (4) picture based information and (5) color-coding of tabular information to guide successful patient use of the materials.16, 17 The DLNET materials also emphasize patient concerns (i.e. what the patient may experience and what the patient should do instead of why he or she should do something). The DLNET promotes shared goal-setting between the patient and health care provider by encouraging patient-provider interaction and discussion about self-management behaviors and goals.
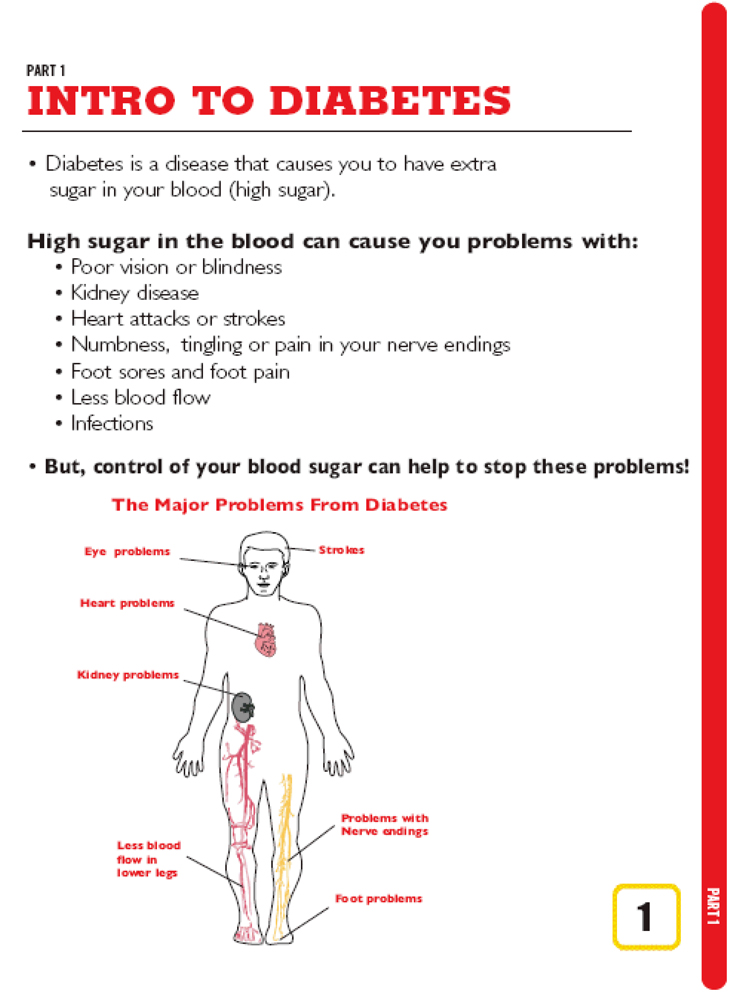
The DLNET contains 24 modules (see Table 1), including core modules that are provided to most patients, and other modules that are provided to patients on an as-needed basis. The modules are typically provided to the patients over multiple visits, and are maintained by the patient in a loose-leaf binder style notebook as a cornerstone of their educational portfolio. Core modules contain materials that are applicable and relevant to nearly all people with diabetes regardless of treatment regimen and are designed to be accessible for patients with lower literacy skills. For example, there is a picture-based description of complications of diabetes (See Figure 1), and picture and color-coded materials to educate patients about goal blood glucose range, and the symptoms and treatment of hypoglycemia. Core materials include information on self-blood glucose checking, exercise, performing a self-foot exam and introduction to diabetes nutrition. Other modules, such as education related to medical nutrition therapy, are comprised of materials representing a range of sophistication from very basic to more complex. The varying levels of complexity of the DLNET materials enable the provider or educator to move from simple to complex materials or vice versa as the patient’s characteristics, clinical concerns and medical needs mandate. The patient becomes an active learner adding additional materials to his or her toolkit as appropriate, continually building their educational portfolio to match their needs.
Table 1.
Diabetes Literacy and Numeracy Education Toolkit Table of Contents
| Module (Module Number) | Description |
|---|---|
| Introduction (1 and 2) | Basics of self care, complications, hypoglycemia (adapted from Hypoglycemia by NovoNordisk (Novo Nordisk Inc. 100 College Road West Princeton,NJ, USA)), and rationale for good control |
| Testing Blood Sugar (2) | Rationale for testing, color-coded chart to interpret blood glucose numbers, steps required to test blood glucose |
| Exercise Plan (3) | Benefits of exercise, prescription for type, frequency and how to prevent hypoglycemia |
| Foot Care (4) | Instructions for prevention of foot ulcers (Foot Care Dos and Don’ts © by BD Medical (1 Becton Drive, Franklin Lakes, NJ USA ) |
| Nutrition Introduction (5) | Basic food groups, definition of carbohydrates and effect on blood sugar |
| Carbohydrates: Plate Method (6) | Instructions for portion size and carbohydrate content for meals. |
| Carbohydrates: Scoop Method (7) | Carbohydrate foods are listed alphabetically with each food assigned a specific color scoop. Scoops are color-coded measuring cups and each scoop of food contains approximately 15 grams of carb. |
| Carbohydrates: Scoops with Insulin (8) | For patients using a fixed insulin dose and the scoop meal planning method. |
| Carbohydrates: Carb Counting (9) | Specific instructions for how to calculate carbohydrate grams from food labels. Practice exercises using labels to assess patient’s ability. |
| Carbohydrates: Recipe (9) | Step by step guidelines on how to determine grams of carb from a recipe. |
| Carbohydrates: Carb Counting (Fixed) (9) | A fixed number of grams of carb is negotiated with each patient for each meal and snack. |
| Oral Medication (10) | Instructions for name of pill(s), number to take and time of day prescribed. |
| Drawing Up Insulin (11) | Instructions on insulin administration using a syringe (Eli Lilly Corporate Center Indianapolis, Indiana 46285 USA) |
| How To Use an Insulin Pen (12) | Instructions on how to use an insulin pen (generic instructions) |
| Insulin for Fixed Dose (13) | Instructions for how much “long lasting” and “short lasting” insulin to take and when to take it. |
| Insulin Fixed Dose + Correction (14) | Instructions for set dose of basal insulin (1–2 times daily) and varying dose of meal insulin based on blood sugar level. |
| Insulin Flexible Dose + Correction (15) | Instructions for set dose of basal insulin (1–2 times daily) and varying dose of meal insulin based on blood sugar level. |
| Flexible Insulin Dosing InsuCalc Wheel (16) | Use of InsuCalc Wheel ® (InsuCalc 174 F Street Salt Lake City, UT, USA )to calculate meal dose based on carb grams and blood sugar level |
| Titration of Basal Insulin (17) | Instructions in titrating basal insulin dose every 3 days based on fasting blood sugar level. |
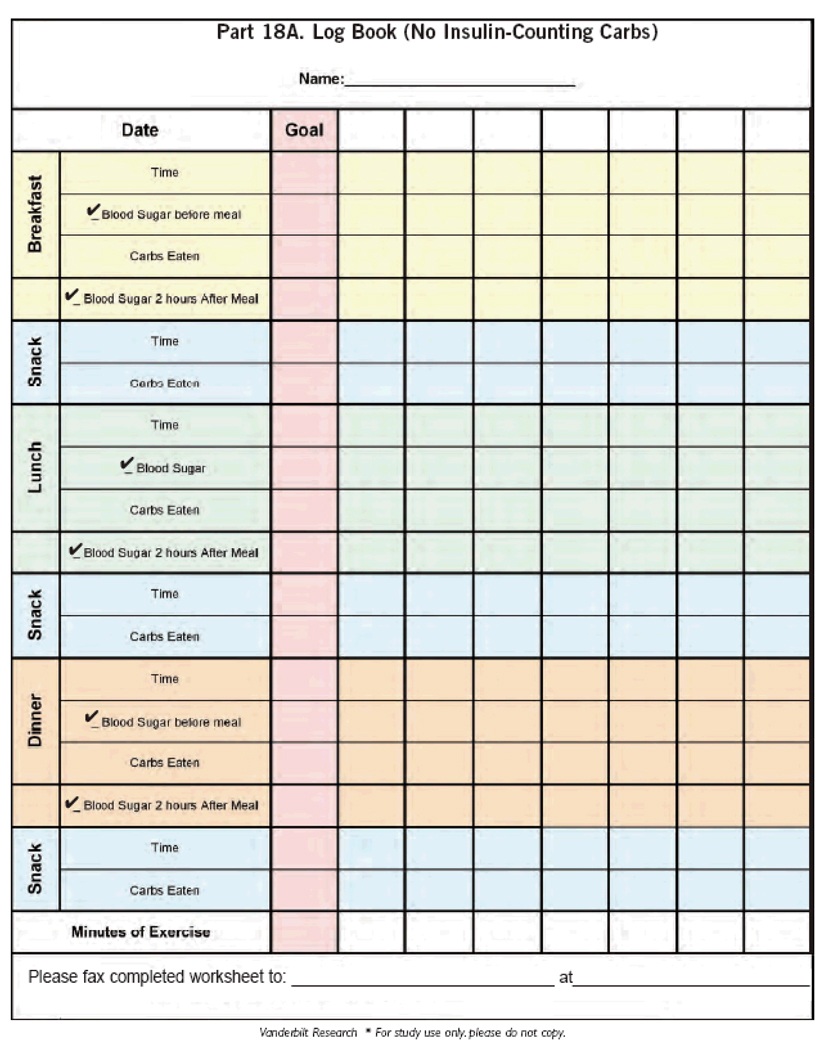
| Blood Glucose Log Sheets (18–21) | Log sheets suitable for testing before and 2-hours after meals, treatment with pills or insulin |
| Insulin for Snacks (22) | Instructions for taking a set dose of meal insulin with snacks before each meal and bedtime. |
| How to use Symlin: Type 1 or Type 2 DM (23) | Instructions for how to lower meal insulin and titrate Symlin dose at Type 1 and Type 2 DM dose ranges. |
| How to use Byetta (24) | Instruction in use of Byetta pen. |
Figure 1.
Example of picture-based DLNET materials
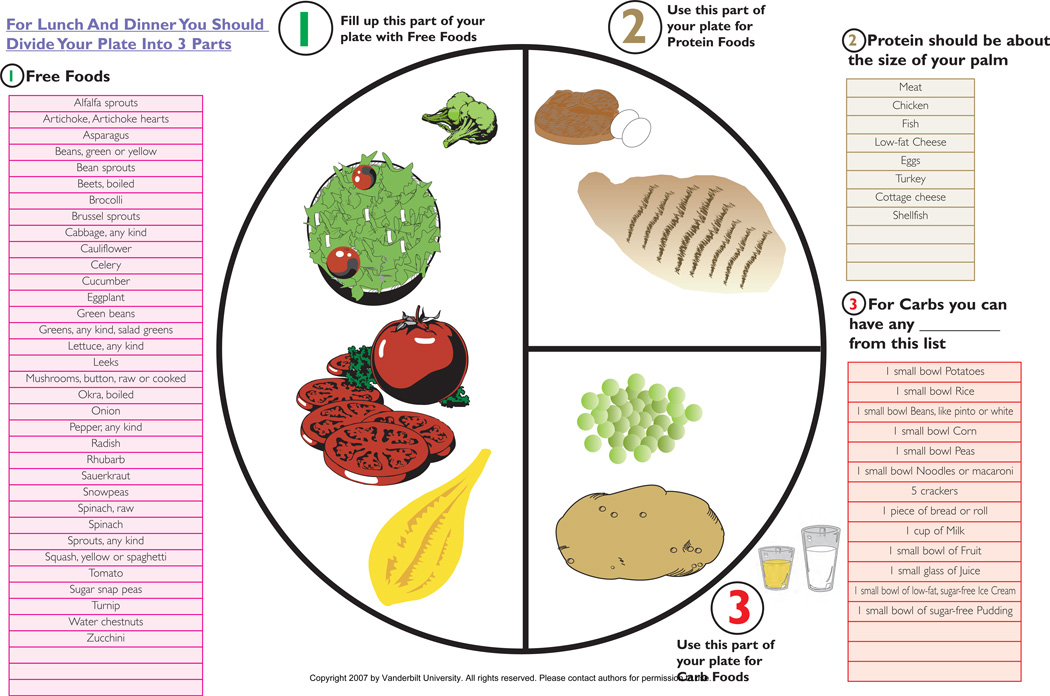
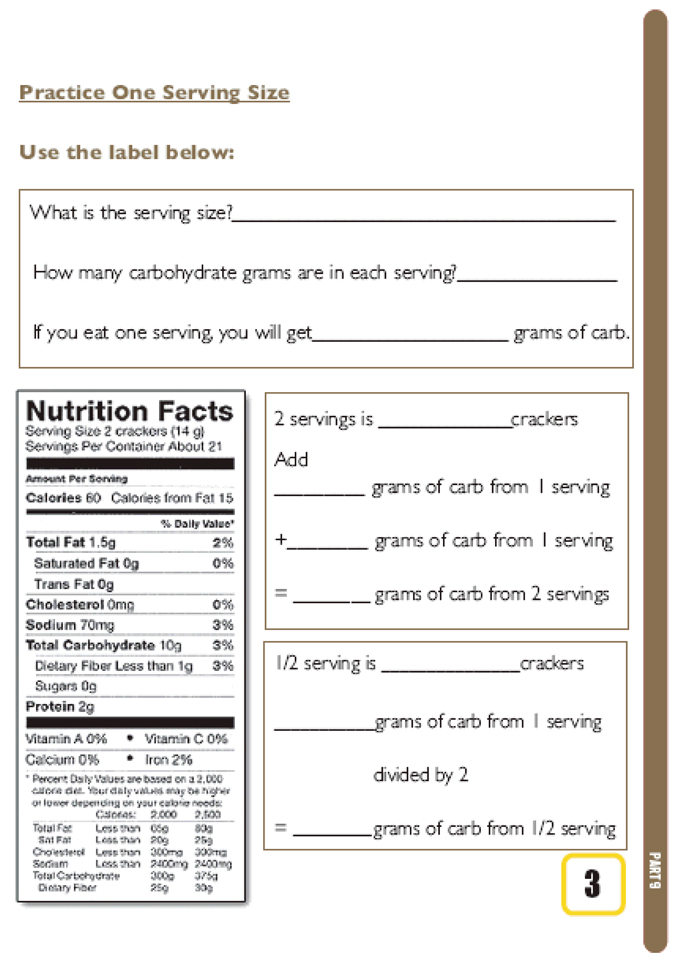
Three different approaches to nutrition education are provided for medical nutrition therapy. For patients with very low literacy or numeracy skills, a modified plate method approach is provided (See Figure 2). This approach allows clinicians and educators to provide dietary education that helps patients to control their intake of carbohydrates and other macronutrients using basic literacy and numeracy skills. For patients with moderate literacy and numeracy skills, a color coded scoop system was developed. Each scoop is equal to a 15-gram serving of carbohydrate. This system allows patients to control carbohydrates by limiting intake to a certain number of scoops of carbohydrate foods per meal or snack. The health care provider works with the patient to determine the appropriate goal of “scoops” per meal. For example, a green labeled scoop would hold 1 cup of any food chosen from a specified list included within the toolkit, where 1-cup is equivalent to approximately 15 grams or 1 serving of carbohydrate. A red labeled scoop would hold ¼ cup of any food chosen from a list of foods for which ¼ cup is equivalent to approximately 15 grams of carbohydrate. Finally, for patients with more proficient literacy and numeracy skills, educational materials were developed to be used to teach patients to calculate carbohydrate intake from food labels, or from a recipe. This included “worksheets” so that patients could practice these skills and demonstrate mastery of this skill to the diabetes educator (See Figure 3). In particular, worksheets were designed to overcome common problems related to carbohydrate counting, such as how to calculate carbohydrate intake when one eats more or less than a single serving size.
Figure 2.
Example of DLNET nutritional therapy: Modified plate method
Figure 3.
Nutrition label worksheet for calculating carbohydrate intake
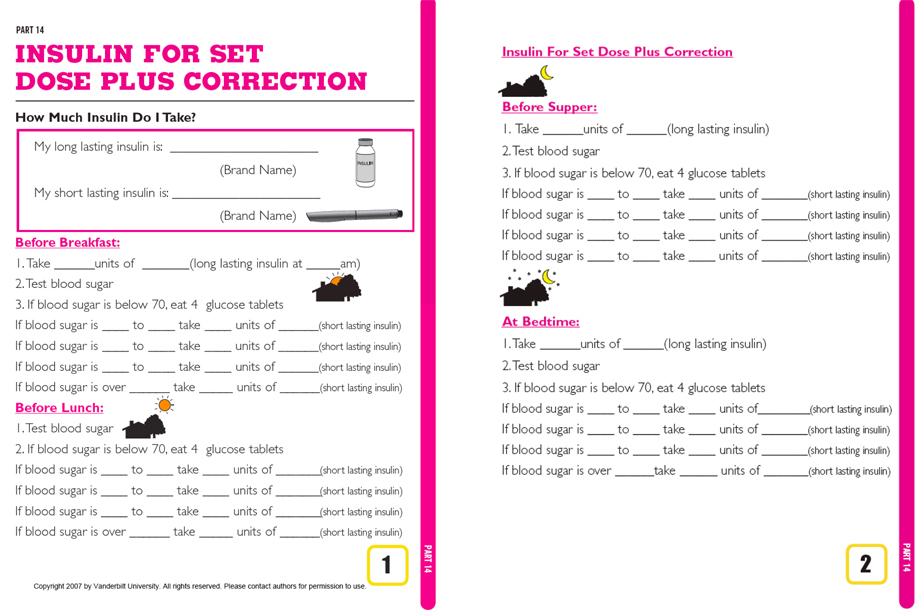
Many of the toolkit modules focus on medication management education. For oral medications, low literacy, simple instructions are provided. Pictures to represent the timing of medications (ex. morning, noon, or night) are included. For insulin, several modules focus on proper dosing. For example, for correction or sliding scale insulin, the amount of insulin for each possible blood sugar level is written out for the patient. This approach allows the provider to give specific recommendations for the total amount of insulin to be taken, including the normal fixed dosage plus the correction scale amount, so that the patient does not need to perform this calculation (See Figure 4). Modules describing techniques to calculate insulin intake based upon carbohydrate intake and blood glucose levels are also included and can be used to teach this skill as well as monitor performance.
Figure 4.
Customizable insulin dosing instructions for fixed dose plus correction
Finally, log sheets were developed to further aid patient self-management (See Figure 5). These log sheets include several advances over traditional log sheets. They are colored to emphasize each separate meal and each day of the week. There are different log sheets available depending on the patient’s treatment complexity. For patients who are counting carbohydrates or scoops, the log sheets provide a place for the health care provider to indicate the patient’s carbohydrate goals for each meal. The log sheets provide space for documentation of the number of units of insulin taken before each meal or at other times of the day, target blood glucose level as well as exercise goals and minutes of exercise completed. This worksheet can be used for shared goal setting and monitoring of progress for all patients with diabetes.
Figure 5.
Example of DLNET log worksheet
DLNET Clinical Applications
The DLNET materials may be used in diabetes education by providers such as nurses, registered dietitians, physicians or certified diabetes educators of any discipline. Although the DLNET materials have to date been used exclusively during 1:1 patient visits, the materials could feasibly be used in the setting of group diabetes classes as well. In most clinical settings the DLNET materials could be combined with materials already in use or could be substituted for the traditional materials. The timing of the delivery of the materials can be customized to the individual. For example, core modules may be given at the first visit and specific training modules can be delivered at subsequent visits when more detailed education about nutrition or medication administration is discussed. Or, for some patients, all materials may be given during the initial visit to enhance self-learning prior to follow-up encounters or if there is concern that follow-up visits are unlikely.
DISCUSSION
The DNLET is a comprehensive set of customizable diabetes educational materials designed with a low literacy and numeracy focus that can be utilized by a range of health care providers and diabetes educators, in a wide variety of clinical settings. The content is based on established guidelines for diabetes education and self management..9 The toolkit materials are designed to improve diabetes education for all patients but may be particularly beneficial for patients with lower literacy or numeracy skills.
Although initial use of the DLNET has been in the context of 1:1 patient-provider interactions, it may also be appropriate for use in a group or class setting. To date, educators that have used the DLNET materials found that they helped create a more organized and systematic approach to diabetes self management education. All providers also found the materials to be user friendly, useful in a wide variety of clinical situations, and a significant aid to providing truly individualized diabetes care. Although there was initial time expenditure in becoming fluent with the materials, ultimately these clinicians reported that the DLNET improved efficiency. One notable disadvantage to the DLNET is the fact that it is only available in English. However, a Spanish language version is currently in development. We are currently in the process of rigorously analyzing the benefit of using the DLNET in two randomized controlled trials.
In addition to using the DLNET, health educators and clinicians may wish to identify or develop their own educational materials for patients with low literacy and numeracy. The following specific principles and guidelines focus on the use of Plain Language and other techniques that enhance clear communication.16–19
Organize information so that the most important points come first
Use the active voice
Avoid jargon
Use printed text of at least 12-point font in a simple script to enhance readability
Use headings and bulleted points to break up the text
Leave plenty of white space around margins and between sections to enhance readability
Keep sentences short and limit number of messages to enhance readability and comprehension
Supplement print with helpful visual images that will be familiar and culturally relevant to patient and convey a message (avoid simply “decorating” the page)
Focus on and clearly state desired actions and behaviors rather than underlying medical principles and explanations
Define technical terms when it is necessary to use them
Another important teaching strategy that can enhance clear communication is the use of “teach back” or “return demonstration” techniques.20 When this technique is used, the educator or clinician first communicates a message or demonstrates a skill to the patient utilizing Plain Language principles. Then, the patient is asked to repeat the message in his or her own words or return the demonstration of the skill. Any misconceptions, misinterpretations or misunderstandings can then be corrected by the clinician or educator. The patient can again be asked to repeat the message as they understand it and any remaining misunderstandings can be corrected. To avoid conveying disrespect or a patronizing intent, the clinician or educator can first explain that they may not have clearly communicated messages or new skills clearly and it is important that the educator or clinician know if he or she has been unclear in their presentation.
Conclusion
The DLNET provides clinicians and educators of diabetes patients with a collection of educational materials that are appropriate for patients with a wide range of reading and math skills and can be used with clear communication techniques to enhance diabetes education. These materials support an approach to teaching diabetes self management that is flexible and adaptable to each patient’s evolving educational needs as treatment regimens change or new skills are acquired. Although the format and presentation of the materials is unique, most CDEs will be familiar with the content and will find the DLNET is easy to integrate into existing educational programs, or to use as the foundation for a new approach to diabetes education.
Acknowledgement
This research is funded with support from the American Diabetes Association (Novo Nordisk Clinical Research Award), the Pfizer Clear Health Communication Initiative, and the Vanderbilt Diabetes Research and Training Center (NIDDK 5P60DK020593). Dr. Rothman is also currently supported by NIDDK Career Development Award (NIDDK 5K23DK065294). Dr. Cavanaugh is currently supported by a NIDDK Career Development Award (NIDDK 1 K23 DK080952-01) and the National Kidney Foundation.
Contributor Information
Kathleen Wolff, Vanderbilt University School of Nursing, Vanderbilt Diabetes Center, Nashville, TN.
Kerri Cavanaugh, Vanderbilt University, Department of Medicine, Nashville, TN.
Robb Malone, University of North Carolina, Department of Medicine, Chapel Hill, NC.
Victoria Hawk, University of North Carolina, Department of Medicine, Chapel Hill, NC.
Becky Pratt Gregory, Vanderbilt University Diabetes Center, Nashville, TN.
Dianne Davis, Vanderbilt University Diabetes Center, Nashville, TN.
Kenneth Wallston, Vanderbilt University School of Nursing, Nashville, TN.
Russell L. Rothman, Vanderbilt University, Departments of Medicine & Pediatrics, Nashville, TN.
References
- 1.Kutner M, Greenberg E, Baer J. A first look at the literacy of America's adults in the 21st century. Jessup, MD: National Center for Education Statistics; 2005. Dec, [Google Scholar]
- 2.Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003 Nov;51(3):267–275. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 3.Rothman RL, Malone R, Bryant B, et al. The Spoken Knowledge in Low Literacy in Diabetes scale: a diabetes knowledge scale for vulnerable patients. Diabetes Educ. 2005 Mar-Apr;31(2):215–224. doi: 10.1177/0145721705275002. [DOI] [PubMed] [Google Scholar]
- 4.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients' knowledge of their chronic disease. A study of patients with hypertension and diabetes. Arch Intern Med. 1998 Jan 26;158(2):166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 5.Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. Jama. 2002 Jul 24–31;288(4):475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 6.Rothman RL, Housam R, Weiss H, et al. Patient understanding of food labels: the role of literacy and numeracy. Am J Prev Med. 2006 Nov;31(5):391–398. doi: 10.1016/j.amepre.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 7.Cavanaugh K, Huizinga MM, Wallston KA, et al. Association of numeracy and diabetes control. Ann Intern Med. 2008 May 20;148(10):737–746. doi: 10.7326/0003-4819-148-10-200805200-00006. [DOI] [PubMed] [Google Scholar]
- 8.Funnell MM, Brown TL, Childs BP, et al. National standards for diabetes self-management education. Diabetes Educ. 2007 Jul-Aug;33(4):599–600. 602–594, 606 passim. doi: 10.1177/0145721707305880. [DOI] [PubMed] [Google Scholar]
- 9.AADE position statement. Individualization of diabetes self-management education. Diabetes Educ. 2007 Jan-Feb;33(1):45–49. doi: 10.1177/0145721706298308. [DOI] [PubMed] [Google Scholar]
- 10.Brown AW, Wolff KL, Elasy TA, Graber AL. The role of advanced practice nurses in a shared care diabetes practice model. Diabetes Educ. 2001 Jul-Aug;27(4):492–496. 498–500, 502. doi: 10.1177/014572170102700404. [DOI] [PubMed] [Google Scholar]
- 11.Ellis SE, Speroff T, Dittus RS, Brown A, Pichert JW, Elasy TA. Diabetes patient education: a meta-analysis and meta-regression. Patient Educ Couns. 2004 Jan;52(1):97–105. doi: 10.1016/s0738-3991(03)00016-8. [DOI] [PubMed] [Google Scholar]
- 12.Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002 Jul;25(7):1159–1171. doi: 10.2337/diacare.25.7.1159. [DOI] [PubMed] [Google Scholar]
- 13.Hill-Briggs F, Smith AS. Evaluation of diabetes and cardiovascular disease print patient education materials for use with low-health literate populations. Diabetes Care. 2008 Apr;31(4):667–671. doi: 10.2337/dc07-1365. [DOI] [PubMed] [Google Scholar]
- 14.Rothman R, Malone R, Bryant B, Horlen C, DeWalt D, Pignone M. The relationship between literacy and glycemic control in a diabetes disease-management program. Diabetes Educ. 2004 Mar-Apr;30(2):263–273. doi: 10.1177/014572170403000219. [DOI] [PubMed] [Google Scholar]
- 15.Rothman RL, DeWalt DA, Malone R, et al. Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. JAMA. 2004 Oct 13;292(14):1711–1716. doi: 10.1001/jama.292.14.1711. [DOI] [PubMed] [Google Scholar]
- 16.National Institutes of Health. [Accessed September 30, 2008];Clear Communication: An NIH Health Literacy Initiative. http://www.nih.gov/icd/od/ocpl/resources/clearcommunication/healthliteracy.htm. Available at: http://www.nih.gov/icd/od/ocpl/resources/clearcommunication/healthliteracy.htm.
- 17.National network of Libraries of Medicine. [Accessed September 30, 2008];Health Literacy. http://nnlm.gov/outreach/consumer/hlthlit.html.
- 18.U.S. Department of Health and Human Services. With Understanding and Improving Health and Objectives for Improving Health. 2nd ed. 2 s. Washington, DC: U.S. Government Printing Office; 2000. Nov, Healthy People 2010. Available at: www.health.gov/healthypeople. [Google Scholar]
- 19.IOM. Health Literacy: A Prescription to End Confusion. Washington, D.C: National Academies Press; 2004. [PubMed] [Google Scholar]
- 20.Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003 Jan 13;163(1):83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]