Abstract
Objective:
To monitor the systemic immune responses of patients with multiple sclerosis (MS) under treatment with GNbAC1, a monoclonal antibody against the envelope protein of the MS- associated retrovirus, during a phase 2a trial.
Methods:
We analyzed the composition of immune cell subsets and the activation level of monocytes by flow cytometry and the response against viral and vaccine antigens by ELISpot.
Results:
None of the endpoints measured revealed any immunosuppressive effect of the therapeutic antibody. Activation of monocytes slightly decreased during treatment as predicted by the hypothesized mechanism of action of GNbAC1.
Conclusion:
These results support the conclusion that the antibody is safe for use in patients with MS.
Classification of evidence:
This study provides Class III evidence that in patients with MS GNbAC1 does not significantly affect several biomarkers of systemic immune response.
Both genetic and environmental factors have been discussed in the pathogenesis of multiple sclerosis (MS). Endogenous retroviruses fall between genetics and environment, having been integrated into the human genome long ago and now being inherited like other genes. Several studies indicate that an endogenous retrovirus, the MS-associated retrovirus (MSRV), might be connected to MS pathogenesis. MSRV has been isolated from brain tissue of patients with MS.1 Subsequently, different studies found increased viral copy numbers and/or transcripts in blood, CSF, or brains of patients with MS compared with controls.2–4 Detection of MSRV was also correlated with disease severity and disability progression.5,6 MSRV might influence the pathogenesis of MS in 2 different ways: by targeting immune cells and by interacting with oligodendrocytes. It has been shown that the envelope protein of MSRV (env) can act as a ligand of toll-like receptor 4 (TLR4) and can activate cells expressing this receptor, such as monocytes, leading to an aberrant upregulation of immune reactivity, thus contributing to autoimmune pathology.7 It has also been suggested that env might directly compromise oligodendrocytes, possibly also via interaction with TLR4.8,9 It was therefore speculated that blocking the interaction between env and immune cells and/or oligodendrocytes might be a novel therapeutic option in MS. Recently, results were reported from a phase 2a trial of GNbAC1, a humanized monoclonal IgG4/κ antibody against the extracellular domain of env.10 This trial showed a favorable safety and pharmacokinetic profile of the therapeutic antibody and showed that MSRV transcripts declined during GNbAC1 treatment, indicating a pharmacodynamic effect. The immunologic substudy reported here examined blood samples from patients enrolled in the previously published phase 2a trial to assess the impact of the therapeutic antibody on the immune system. Additional healthy volunteers were recruited for comparison.
METHODS
Participants and design.
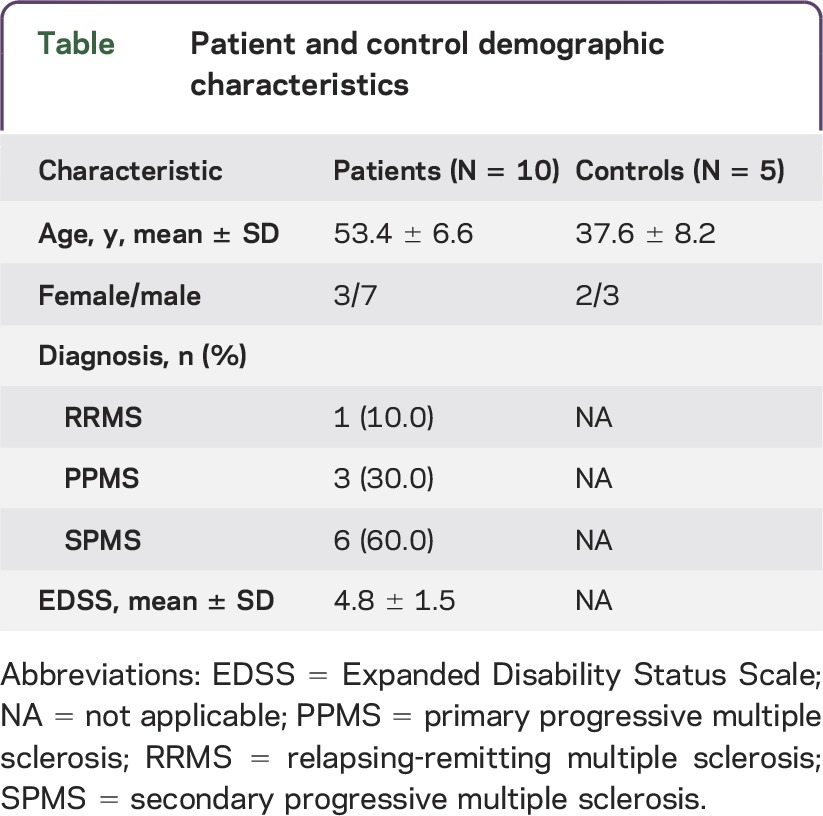
Blood samples were taken from the 10 patients involved in the phase 2a trial (5 from Basel, 5 from Geneva) and from 5 healthy volunteers recruited additionally for this immunologic substudy. Demographic details are provided in the table. Patients received monthly infusions of 2 or 6 mg/kg body weight over a period of 6 months. Blood was drawn on the day before the first administration of GNbAC1, on the first day after administration, 2 weeks after administration, and at the end of the 6-month treatment period. Two patients received placebo for the first time point. Blood from healthy controls was drawn at each time point on the same day as the patients and processed in parallel. A schematic of the study design is shown in figure e-1 at Neurology.org/nn.
Table.
Patient and control demographic characteristics
Standard protocol approvals, registrations, and patient consents.
The study protocol was approved by the ethics committees of both centers and the Swiss Medicine Agency, Swissmedic. All patients enrolled in this study gave written informed consent.
Assays.
Blood taken from participants in Basel was processed immediately. In Geneva, blood was drawn into cell preparation tubes (CPTs), transported to Basel by courier, and processed the same day. The primary research question was: How does the state of the immune system change following treatment with GNbAC1? This was addressed in 3 assays (Class III level of evidence): (1) proportions of various immune cell populations by flow cytometry to monitor the general state of the immune system; (2) interferon (IFN)-γ production in response to various antigens, using the Ready-SET-go human IFN-γ ELISpot kit (eBioscience, San Diego, CA) to measure physiologic immune reactivity; and (3) p38 mitogen-activated protein kinase (MAPK) phosphorylation by phospho-specific flow cytometry (clone 36/p38, BD Biosciences, San Jose, CA) as a measure of TLR4 stimulation in monocytes. Immune cell subpopulations and ELISpot results are not reported from the Geneva patients, whose peripheral blood mononuclear cells after retrieval from CPTs contained variable levels of erythrocytes, granulocytes, and other cell types, making comparisons unreliable. For the p38 MAPK phosphorylation, this problem was obviated by restricting flow cytometry to CD33-positive monocytes, and results are reported for all 10 patients and 4 controls.
RESULTS
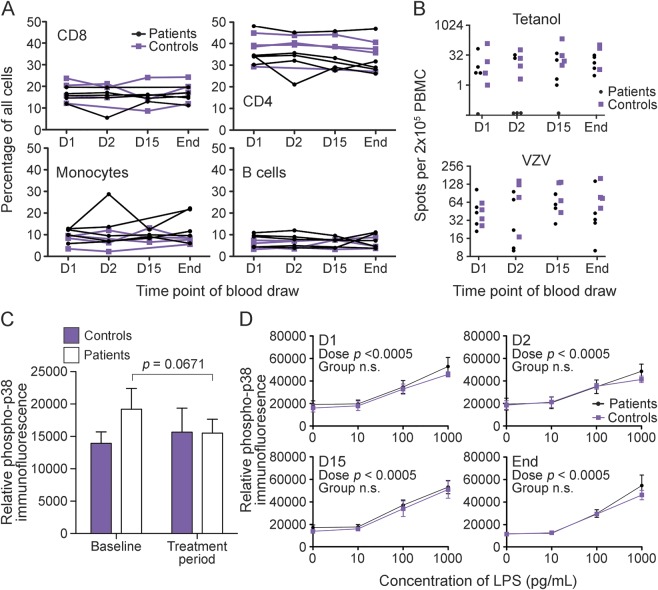
Using flow cytometry, we determined the frequencies of the main subfractions of lymphocytes during the trial. We could not detect a difference in the proportions of CD4+ and CD8+ T cells, B cells, and monocytes between patients and controls. There was also no change in the composition of lymphocytes during 6 months of treatment with GNbAC1 (figure 1A).
Figure 1. Comparison of immune phenotype, antigen reactivity, and monocyte activation in blood of patients and controls.
(A) Cellular composition of peripheral blood mononuclear cells (PBMC) from 5 patients and 4 controls over time (immediately before first infusion: D1, the following day: D2, 2 weeks later: D15, and the conclusion of the study: End). Percentages of CD8+ T cells, CD4+ T cells, CD33+ monocytes, and CD19+ B cells in patients (black circles and lines) and controls (purple squares and purple lines) at the 4 time points. Results are only reported from Basel participants. Missing data points are indicated by omitted symbols. (B) Interferon (IFN)-γ response to a vaccine (Tetanol) and a viral antigen (varicella-zoster virus [VZV], Varilrix) throughout the trial in 5 patients and 4 controls. Each condition was assayed in triplicate wells with PBMC exposed to the stimulus using the human IFN-γ ELISpot Ready-SET-Go! (eBioscience, San Diego, CA), and this figure displays the medians from these triplicates at each time point for each of 5 patients and 4 controls. Results are only reported from Basel participants. Missing data points are indicated by omitted symbols. (C) Phosphorylation of p38 mitogen-activated protein kinase (MAPK) in monocytes from 10 patients before and during treatment and from 5 healthy controls at the same time points. Cryopreserved PBMC were permeabilized in methanol and then immunolabeled with anti-CD33 antibodies (eBioscience) to identify monocytes and anti–phospho-p38 MAPK antibodies (BD Biosciences, San Jose, CA) to measure phosphorylation. Vertical axis shows relative phospho-p38 immunofluorescence (arbitrary units). When values from more than 1 time point were available before or during the treatment period, these were averaged, producing 1 before-treatment and 1 during-treatment value for each patient. Time points at which patients were given placebo were included in the pretreatment condition. Error bars show SEM. Averaging for controls followed the patients to whom they were yoked, and the data were analyzed by repeated-measures 2-way analysis of variance comparing effects of group (i.e., patients vs controls) and time point (i.e., before vs during treatment). Neither the main effects nor the interaction were significant. Since the parameter of most interest was the comparison between before and during treatment within the patients, these data were also compared using a paired 2-tailed t test (p = 0.0671). (D) Phosphorylation of p38 MAPK in monocytes of 10 patients and 5 controls across the trial in response to lipopolysaccharide (LPS). Vertical axis is the median immunofluorescence in arbitrary units. Purple lines and squares represent healthy untreated controls. Black lines and circles represent patients. Each of the 4 panels shows results from 1 time point from blood exposed to a range of concentrations of LPS, as indicated. The effect of dose was analyzed by linear regression and found to be significant (p < 0.0005 for both patients and controls at each time point). This effect of dose (i.e., the slope of the dose-response regression lines) was compared between patients and controls and between time points, but neither the main effects nor the interaction were significant.
We monitored antigen-specific responses by IFN-γ ELISpot. We detected robust immune responses against varicella-zoster virus and tetanus vaccine (Tetanol) throughout the study. The responses were highly variable between individuals and across time but not obviously different between patients and controls (figure 1B). The presence of robust antivaccine and antiviral responses and the absence of antigen-independent IFN-γ production at similar levels before and after treatment suggest that there was no adverse activation or suppression of the protective immune response. We also tested the T cell response against an established autoantigen in MS, myelin basic protein (MBP). The response against MBP was low in patients and healthy controls and did not significantly change over time (data not shown).
To monitor TLR4 activation in monocytes, we determined the phosphorylation of p38, a key component of the signaling pathway downstream of TLR4, using a phospho-specific anti–p38 MAPK antibody in flow cytometry. We were able to detect the effect of lipopolysaccharide (LPS) down to 100 pg/mL (figure 1D), a level of sensitivity comparable to the gold standard Limulus amebocyte lysate endotoxin test. Primarily, we examined phosphorylation of p38 in naive monocytes (without exogenous LPS) before and during treatment. The pattern we observed was consistent with the hypothesis underlying the proposed mechanism of action of GNbAC1, i.e., before the trial, p38 phosphorylation was higher in patients with MS than in healthy controls, and treatment reduced the p38 phosphorylation in patients (figure 1C). However, this did not reach statistical significance. We also tracked p38 phosphorylation across the trial in naive monocytes and in response to various doses of LPS and observed that the response to this exogenous TLR4 ligand was similar between patients and controls and stable across the trial (figure 1D).
DISCUSSION
These results are consistent with the previously published report of the phase 2a trial in that no evidence was obtained that GNbAC1 administration interferes with the normal functioning of the immune system. This apparent evidence of safety should be interpreted in light of the small size and limited duration of the trial. Flow cytometry of phospho-p38 in monocytes has potential as a biomarker for monitoring response to treatment with this antibody or any other agent targeting the TLR signaling system. Larger studies will be required to corroborate these findings and elucidate the relationship between monocyte activation and clinical response.
GLOSSARY
- CPT
cell preparation tube
- env
envelope protein of MSRV
- IFN
interferon
- LPS
lipopolysaccharide
- MAPK
mitogen-activated protein kinase
- MBP
myelin basic protein
- MS
multiple sclerosis
- MSRV
MS-associated retrovirus
- TLR4
toll-like receptor 4
Footnotes
Supplemental data at Neurology.org/nn
AUTHOR CONTRIBUTIONS
Study concept and design: M.Z., N.S.R.S., M.R., P.H.L., R.L.P.L., T.D. Acquisition of data: M.Z., N.S.R.S., M.R., P.H.L. Analysis and interpretation: M.Z., N.S.R.S., M.R., A.B.L., F.C., T.D. Critical revision of the manuscript for important intellectual content: M.Z., N.S.R.S., M.R., P.H.L., A.B.L., F.C., R.L.P.L., L.K., T.D. Study supervision: P.H.L., R.L.P.L., L.K., T.D. Statistical analysis: N.S.R.S.
STUDY FUNDING
This work was supported by GeNeuro, SA, Plan-les-Ouates/Geneva, Switzerland.
DISCLOSURE
M. Zimmerman reports no disclosures. N.S.R. Sanderson received research support from Swiss National Science Foundation and Swiss Multiple Sclerosis Society. M. Rasenack reports no disclosures. P.H. Lalive is on the scientific advisory board for Biogen-Idec and Novartis and received travel funding and/or speaker honoraria from Biogen-Idec, Teva, and Merck Serono. A.B. Lang is employed by GeNeuro. F. Curtin is employed by GeNeuro. R.L.P. Lindberg received research support from Swiss Multiple Sclerosis Society, Swiss National Science Foundation, and Roche Postdoctoral Fellowship Program. L. Kappos is on the editorial board for Multiple Sclerosis Journal, Multiple Sclerosis and Related Disorders, and Journal of Neurology and received research support from Actelion, Addex, Almirall, Bayer, Biogen-Idec, Biotica, CSL Behring, Genetech, GeNeuro, Genzyme, Merck Serono, Mitsubishi, Novartis, Octapharma, Ono Pharma, Pfizer, Receptos, Roche, Sanofi-Aventis, Santhera, Siemens, Teva, UCB, Xenoport, Swiss National Research Foundation, European Union, Swiss MS Society, and Novartis and Roche Research Foundations. T. Derfuss is on the scientific advisory board for Biogen-Idec, Novartis Pharma, Genzyme, Merck Serono, Bayer Schering, Octapharma, GeNeuro, and Roche; received travel funding and speaker honoraria from Bayer Schering, Biogen-Idec, Merck Serono, Novartis Pharma, and Genzyme; is on the editorial board of PLoS One; is a member of steering committees by Mitsubishi Pharma and GeNeuro; is on the executive board of ECTRIMS; received research support from Novartis Pharma, Merck Serono, Biogen-Idec, Swiss National Foundation, and Swiss MS Society; and his spouse is employed by Novartis Pharma. Go to Neurology.org/nn for full disclosure forms.
REFERENCES
- 1.Perron H, Lalande B, Gratacap B, et al. Isolation of retrovirus from patients with multiple sclerosis. Lancet 1991;337:862–863. [DOI] [PubMed] [Google Scholar]
- 2.Arru G, Mameli G, Astone V, et al. Multiple sclerosis and HERV-W/MSRV: a multicentric study. Int J Biomed Sci 2007;3:292–297. [PMC free article] [PubMed] [Google Scholar]
- 3.Dolei A, Serra C, Mameli G, et al. Multiple sclerosis-associated retrovirus (MSRV) in Sardinian MS patients. Neurology 2002;58:471–473. [DOI] [PubMed] [Google Scholar]
- 4.Mameli G, Astone V, Arru G, et al. Brains and peripheral blood mononuclear cells of multiple sclerosis (MS) patients hyperexpress MS-associated retrovirus/HERV-W endogenous retrovirus, but not Human herpesvirus 6. J Gen Virol 2007;88:264–274. [DOI] [PubMed] [Google Scholar]
- 5.Sotgiu S, Arru G, Mameli G, et al. Multiple sclerosis-associated retrovirus in early multiple sclerosis: a six-year follow-up of a Sardinian cohort. Mult Scler 2006;12:698–703. [DOI] [PubMed] [Google Scholar]
- 6.Sotgiu S, Mameli G, Serra C, Zarbo IR, Arru G, Dolei A. Multiple sclerosis-associated retrovirus and progressive disability of multiple sclerosis. Mult Scler 2010;16:1248–1251. [DOI] [PubMed] [Google Scholar]
- 7.Rolland A, Jouvin-Marche E, Viret C, Faure M, Perron H, Marche PN. The envelope protein of a human endogenous retrovirus-W family activates innate immunity through CD14/TLR4 and promotes Th1-like responses. J Immunol 2006;176:7636–7644. [DOI] [PubMed] [Google Scholar]
- 8.Antony JM, van Marle G, Opii W, et al. Human endogenous retrovirus glycoprotein-mediated induction of redox reactants causes oligodendrocyte death and demyelination. Nat Neurosci 2004;7:1088–1095. [DOI] [PubMed] [Google Scholar]
- 9.Kremer D, Schichel T, Forster M, et al. Human endogenous retrovirus type W envelope protein inhibits oligodendroglial precursor cell differentiation. Ann Neurol 2013;74:721–732. [DOI] [PubMed] [Google Scholar]
- 10.Derfuss T, Curtin F, Guebelin C, et al. A phase IIa randomised clinical study of GNbAC1, a humanised monoclonal antibody against the envelope protein of multiple sclerosis-associated endogenous retrovirus in multiple sclerosis patients. Mult Scler 2015;21:885–893. [DOI] [PubMed] [Google Scholar]