Abstract
Objective
Despite evidence of elevated risk factors for suicidal thoughts and behavior in youth with Tourette syndrome and chronic tic disorders (CTD), few studies have actually examined that relationship. This study documented the frequency and clinical correlates of suicidal thoughts and behaviors in a sample of children and adolescents with CTD (N=196; range 6-18 years old).
Method
Youth and parents completed a battery of measures that assessed co-occurring psychiatric diagnoses, child emotional and behavioral symptoms, and impairment due to tics or co-occurring conditions.
Results
A structured diagnostic interview identified that 19 youths with CTD (9.7%) experienced suicidal thoughts and/or behaviors, which was elevated compared to three youths (3%) who experienced these thoughts in a community control sample (N=100; range 6-18 years old; p = 0.03). For youth with CTD, suicidal thoughts and behaviors were frequently endorsed in the context of anger and frustration. The Child Behavior Checklist (CBCL) anxious/depressed, withdrawn, social problems, thought problems, and aggressive behavior subscales, as well as the total internalizing problems scale were associated with the presence of suicidal thoughts and/or behaviors. Suicidal thoughts and/or behaviors were significantly associated with tic symptom severity, tic-related impairment, and obsessive-compulsive, depressive, anxiety, and attention-deficit/hyperactivity disorder symptom severity. CBCL anxiety/depression scores mediated the relationship between tic severity and suicidal thoughts and behaviors.
Conclusions
Findings suggest that about 1 in 10 youth with CTD experience suicidal thoughts and/or behaviors, which are associated with a more complex clinical presentation and often occur in the presence of anger and frustration.
Keywords: Tourette Syndrome, Tic disorder, Suicidal Ideation, Children, Assessment, Tics, Suicide
Many youth with Tourette syndrome (TS) and chronic tic disorder (CTD; TS and CTD are hereafter collectively referred to as CTD) experience a multitude of stressors beyond the burden of having tics including: psychiatric comorbidity,1 peer victimization,2, 3 social isolation and rejection,4, 5 illness-related stigma,6 and low self-esteem.7 Although stressors associated with CTD are well-documented risk factors for suicide,8-13 there has been limited examination of suicidal thoughts and behaviors in those with CTD, which was the purpose of this study.
In an archival review of an unreported number of child and adult patients seen consecutively between 1995 and 2008 at a CTD specialty clinic, all ten suicidal CTD patients exhibited significant comorbid psychopathology including affective disorders (e.g., depressive disorders, bipolar disorders, schizoaffective disorder), obsessive-compulsive spectrum disorders, and intermittent explosive disorder.14 Eight of the ten suicidal CTD patients exhibited severe tic intensity as well as coprophenomena (i.e., socially inappropriate verbal expressions and/or gestures) or echophenomena (i.e., repetition of another's words and/or actions), while four exhibited moderate or severe self-injurious behavior. In a retrospective examination of 333 patients ages 9-45 years,15 ~5% (n=17) of patients were classified as having “malignant Tourette Syndrome” (defined as the presence of severe tics, rage attacks, self-injury and/or suicidal ideation), with caseness associated with presence of OCD, coprophenomena, and pharmacotherapeutic resistance.
Despite the potential increase in risk for suicidal thoughts and behaviors among youth with CTD, there has been limited empirical examination. Thus, we examined the frequency and clinical correlates of suicidal thoughts and behaviors in children and adolescents with CTD. For the purpose of this research, suicidal thoughts and suicidal behavior was defined as presence of thoughts of death, suicidal ideation, suicidal plan, and/or past suicide attempts. We were interested in the following questions. First, what is the frequency of suicidal thoughts and behavior among youth with CTD relative to youth in the community without CTD? Given the increased prevalence of comorbidities and social stressors associated with CTD,2, 3, 16 we hypothesized that youth with CTD would be at increased risk for suicidal thoughts and behaviors compared to youth without CTD. Second, given previous associations of CTD with anger and rage, we predicted that youth with CTD who endorsed suicidal thoughts and/or behaviors would be more likely than controls to express these thoughts and behaviors when angry or frustrated. Third, we predicted that suicidal thoughts and behaviors would be associated with the presence of comorbid psychiatric disorders including ADHD, depression, oppositional defiant disorder, and generalized anxiety disorder, as well as with symptom severity ratings of tics, ADHD, depression, anxiety, and OCD.12, 17, 18 Given limited examination in previous studies of youth with CTD, we did not make any predictions concerning demographic characteristics (e.g., gender, age) although evidence suggests that suicidal thoughts and behaviors increase during adolescence,19 and are more common among females.10, 13, 20, 21 Fourth, we explored whether specific syndrome scales on a common childhood screening measure were associated with suicidal thoughts and behaviors. Finally, we considered whether tic symptom severity predicted suicidal thoughts and behaviors independently, or if other clinical factors influenced this relationship. Although we hypothesized that tic symptom severity would be associated with suicidal thoughts and behaviors, we predicted that youth's anxious and depressive symptoms would mediate this relationship due to the common association of these symptoms with suicidal thoughts and behaviors among youth without CTD.
Method
Participants
Table 1 details participant demographics. One hundred and ninety-six children and adolescents with TS (n=189) and CTD (n=7), participated. No participants with Tic Disorder-Not Otherwise Specified were included in this sample. Children and their parents were recruited from the normal patient flow at two specialty clinics: the University of South Florida (n=104; USF) and the University of Rochester (n=92; UR). There were no site differences with regard to gender (p=0.42), age (p=0.34), or tic severity (p=0.36). Both sites used the same inclusion criteria: 1) a diagnosis of TS or CTDϕ based on Diagnostic and Statistical Manual for Mental Disorders–Fourth Edition, Text Revision (DSM-IV-TR) criteria established by an expert clinician using consensus procedures; and 2) between 6-18 years of age. Exclusion criteria included presence of intellectual disability (1 youth with CTD was excluded due to this), psychosis, mania, or any other condition that would limit the child's (or parent's) ability to understand study measures (1 youth with CTD was excluded due an inability to understand study measures). Tic disorder consensus diagnoses were determined by a board certified child and adolescent psychiatrist (USF) or pediatric neurologist (UR) using all available information, including clinical interview with the family, examination of clinical records, review of completed study measures, and as needed, consultation with other clinicians. Community control participants (n=100) were recruited from the UR site through community pediatric practices, community advertisements, and online parenting forums, and used for comparative analyses. Inclusion criteria for community controls were that youth did not have a history of tics or a first degree relative with TS.
Table 1.
Demographic Characteristics for Youth with CTD and Community Control Participants
| Total Sample (N = 296) N (%) | Youth with CTD (n = 196) N (%) | Community Controls (n = 100) N (%) | |
|---|---|---|---|
| Male | 209 (71%) | 149 (76%) | 60 (59%) |
| Race/Ethnicity | |||
| Caucasian | 223 (75%) | 155 (79%) | 68 (68%) |
| Hispanic | 22 (7%) | 16 (8%) | 6 (6%) |
| Black | 19 (6%) | 5 (3%) | 14 (14%) |
| Asian American | 4 (1%) | 4 (2%) | 0 (0%) |
| Pacific Islander | 1 (0.3%) | 1(1%) | 0 (0%) |
| Other | 24 (8%) | 13 (7%) | 11 (11%) |
| Unknown race | 3 (1%) | 2 (1%) | 1(1%) |
| Children (6-11 years) | 166 (56%) | 109 (56%) | 57 (57%) |
| Adolescents (12-18 years) | 130(44%) | 87 (44%) | 43 (43%) |
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Age | 11.21 (2.87) | 11.29 (2.93) | 11.07 (2.75) |
Note: There was no significant difference in age between youth with CTD and community control participants, t(294)=0.61, p=0.54.
Measures
Comorbid Psychiatric Disorders and Suicidal Thoughts and Behaviors
The Diagnostic Interview Schedule for Children-4th edition (DISC)22 is a highly structured psychiatric interview with parallel versions for parents of youth aged 6-18 years (DISC-P) and youth aged 9-18 years (DISC-Y). The DISC was used to assess DSM-IV criteria for comorbid conditions, including ADHD, OCD, oppositional defiant disorder (ODD), generalized anxiety disorder (GAD), separation anxiety disorder (SAD) and major depressive disorder (MDD). Most DISC-Y/P questions are designed so respondents can answer “yes,” “no,” or “sometimes/somewhat,” and is scored using a computer algorithm according to DSM-IV symptom criteria.23 The DISC-Y/P have demonstrated satisfactory reliability and validity for establishing that youth meet diagnostic criteria for specific psychiatric disorders.22, 24 In addition to psychiatric comorbidity, the DISC-Y/P also includes questions concerning the presence of suicidal thoughts and suicidal behavior as part of the depression module (Items 20-22; Table 2).
Table 2.
Participants that endorsed thoughts of death/dying, suicidal thoughts and/or behaviors
| Youth with CTD (n=196) | Community Controls (n=100) | |||||
|---|---|---|---|---|---|---|
| DISC-Y/P Questions | Children N (%) | Parents N (%) | κ | Children N (%) | Parents N (%) | κ |
| 20. In the last year, was there a time when [you/he/she] often thought about death or about people who had died or about being dead [your/him/herself?] | 10 (5%) | 12 (6%) | 0.43a | 0 (0%) | 0 (0%) | N/A |
| 21. In the last year, was there a time when [you/he/she] thought seriously about killing [your/him/herself?] | 8 (4%) | 7 (4%) | 0.32 | 3 (3%) | 3 (3%) | 1.00b |
| 22. For the next question, I would like you to think about [your/his/her] whole life. Has [you/he/she] ever, in [his/her] whole life, tried to kill [himself/herself] or made a suicide attempt? | 2 (1%) | 2 (1%) | 0.50 | 0 (0%) | 0 (0%) | N/A |
| CBCL Questions | ||||||
| 18. Deliberately harms self or attempts suicide | -- (--%) | 3 (2%) | N/A | -- (--%) | 3 (3%) | N/A |
| 91. Talks about killing self | -- (--%) | 8 (4%) | N/A | -- (--%) | 3 (3%) | N/A |
| MAVRIC-P Questions | ||||||
| 15b. Has your child been so angry that he or she thought about killing himself or herself? | -- (--%) | 18 (9%) | N/A | -- (--%) | 1 (1%) | N/A |
| 15d. Has your child been so angry that he or she tried to kill himself or herself? | -- (--%) | 2 (1%) | N/A | -- (--%) | 0 (0%) | N/A |
| Youth with CTD (n=196) | Community Controls (n=100) | Test Statistic | p-value | ES | |
|---|---|---|---|---|---|
| DISC-Y/P Item #20 | 16 (8%) | 0 (0%) | Fisher's exact test | 0.001 | 0.17 |
| DISC-Y/P Item #21 | 10 (5%) | 3 (3%) | Fisher's exact test | 0.31 | 0.05 |
| DISC-Y/P Item #22 | 3 (1.5%) | 0 (0%) | Fisher's exact test | 0.29 | 0.07 |
| Any DISC-Y/P Item #20-22 (endorsed #20, #21, and/or #22) | 19 (9.7%) | 3 (3%) | Fisher's exact test | 0.03 | 0.12 |
| CBCL Item #18* | 3 (1.6%) | 3 (3%) | Fisher's exact test | 0.33 | 0.05 |
| CBCL Item #91* | 8 (4%) | 3 (3%) | Fisher's exact test | 0.46 | 0.03 |
| CBCL Item #18 and/or #91* | 8 (4%) | 3 (3%) | Fisher's exact test | 0.46 | 0.03 |
| MAVRIC-P Item #15b** | 18 (10%) | 1 (1%) | Fisher's exact test | 0.003 | 0.16 |
| MAVRIC-P Item #15d** | 2 (1%) | 0 (0%) | Fisher's exact test | 0.44 | 0.06 |
| MAVRIC-P #15b and/or 15d** | 19 (10%) | 1 (1%) | Fisher's exact test | 0.002 | 0.16 |
| Positive response on any item on either DISC-Y/P (#20, #21, #22), CBCL (#18, #91), and MAVRIC-P (#15b, #15d) | 33 (17%) | 4 (4%) | Fisher's exact test | 0.001 | 0.18 |
| Positive response on any item on either DISC-Y/P (#21, #22), CBCL (#18, #91), and MAVRIC-P (#15b, #15d) | 29 (15%) | 4 (4%) | Fisher's exact test | 0.003 | 0.16 |
Note: N/A = Not applicable
p=0.07
p<0.001
Only 192 youth with CTD had complete CBCL data
Only 180 youth with CTD and 96 community controls had complete MAVRIC-P data
Clinician-Rated Tic Symptom Severity and Impairment
The Yale Global Tic Severity Scale (YGTSS)25 is a clinician-rated, semi-structured interview that assesses the presence and severity of motor and phonic tics over the preceding week. Endorsed motor and phonic tics are rated individually on a 0-5 point scale according to number, frequency, intensity, complexity and interference (range of severity=0-50). There is a one-item rating (range=0-50) of the degree of associated life impairment across interpersonal, academic, and/or occupational realms. The YGTSS demonstrates strong psychometric properties including excellent reliability,25, 26 validity,27 and treatment sensitivity.28, 29
Clinician-Rated Obsessive-Compulsive Symptom Severity
The Children's Yale-Brown Obsessive Compulsive Scale (CY-BOCS)30 is a clinician administered, semi-structured scale that measures the presence and severity of obsessive-compulsive symptoms over the previous week. The CY-BOCS consists of two subscales, obsession and compulsion severity, and a total severity score. The CY-BOCS has excellent reliability and validity.30-33
Tic-Related Impairment
The Child Tourette's Syndrome Impairment Scale-Parent Report (CTIM-P)34 assesses tic-related impairment or impairment due to a co-occurring problem (e.g., attention deficits, oppositional/defiant behaviors, obsessive-compulsive symptoms, etc.). The scale measures impairment occurring at school, home, or during social activities within the past month.
Parent-rated Internalizing and Externalizing Symptoms
The Child Behavior Checklist (CBCL)35 is a parent-report questionnaire that assesses the frequency of behavioral and emotional problems in youth within the last 6 months. The CBCL contains two items specific to suicidal thoughts and/or behaviors (Item #18 and #91, see Table 2). Psychometric support for the CBCL has been established.35, 36
Parent-rated ADHD and ODD Symptom severity
The Swanson Nolan and Pelham Rating Scale-Fourth Revision (SNAP-IV)37 is a parent-rated measure of externalizing symptoms.38
Parent-Rated Aggression In Youth
The Measure of Aggression, Violence, and Rage in Children for Parents (MAVRIC-P)39 assesses the severity of reactive, impulsive aggression in youth aged 5-18 years. Items are answered according to their presence or absence, and assess both verbal and physical aggression directed towards people, themselves, or inanimate objects. Total scores range between 0-30, with higher scores indicating higher symptom severity. The MAVRIC-P contains two items specific to suicidal thoughts and/or behaviors (Item #15b and #15d, see Table 2). The MAVRIC-P has excellent reliability and validity.40
Child-Rated Depressive Symptom Severity
The Children's Depression Inventory-Short Form (CDI-S)41 is a child-report of presence and severity of cognitive, affective, or behavioral symptoms of depression over the previous two weeks, with higher scores suggesting increased severity.
Child-Rated Anxiety Symptom Severity
The Multidimensional Anxiety Scale for Children (MASC) is child-report of anxiety. For the purposes of this study, t-scores for youth under 8 years of age (n=20) were calculated using normative data from 8-11 year olds.
Procedures
Study procedures were identical across sites and were approved by a site-specific university institutional review board. Parents provided written consent and children provided written assent prior to participation. Thereafter, youth and their parent completed a 3-4 hour evaluation that consisted of a clinical interview with a board certified psychiatrist or neurologist, separate DISC-Y/P interviews, clinician-administered assessments (e.g., YGTSS, CY-BOCS), and self- and parent-report measures. The YGTSS and CY-BOCS were each jointly administered to parents and children by a trained, licensed psychologist or board-certified psychiatrist or neurologist. All clinicians underwent cross-site YGTSS and CY-BOCS rater reliability training using practice interviews, and were instructed on how to administer the DISC-Y/P. At both sites, trained research associates administered the DISC-Y/P to parents and youth aged 9 years and above, with only the DISC-P being administered to families with youth under 9 years of age. Families were compensated for participation. Responses on the DISC-P were used to identify the presence of comorbid psychiatric diagnoses.
The presence of suicidal thoughts and/or behavior was determined by responses from children and parents on DISC-Y/P depression items 20-22 (Table 2), which respectively assessed thoughts of death (20a-d), suicidal ideation (21a-e), suicidal plan (21f), and past suicide attempts (22a-g). Children with positive endorsements for any DISC-Y/P items 20-22 were classified as displaying suicidal thoughts and suicidal behaviors given the presence of thoughts about being dead, killing themselves, or having a history of suicide attempt(s). The frequency of endorsed suicidal items on the CBCL (Item #18, #91) and on the MAVRIC-P (Item #15b, 15d; see Table 2 for item content) were also reported, but not included in subsequent analyses due to preference for comprehensive and structured questioning associated with the DISC-Y/P relative to CBCL, and the specific time window of rating relative to MAVRIC-P (e.g., MAVRIC-P inquires about suicidal thoughts and/or behaviors in the context of 'most angry episode'). When endorsed by either parent or youth, suicidal thoughts or behaviors were immediately evaluated by a licensed psychologist or board certified child and adolescent psychiatrist and triaged appropriately to ensure the youth's well-being.
Data Analysis
Prior to analyses, cases were reviewed for missing data. When participants' ratings had less than 20% missing data, mean-item replacement imputations were utilized. This imputation strategy only impacted 14 cases in which participants were missing between 1-2 items per form (13 MASC, 1 CDI-S). When a participant's form had greater than 20% missing data, the form was excluded from analysis which impacted 13 participant's ratings scales. Descriptive statistics and one-tailed Fisher's exact tests were used to identify and compare the frequency of suicidal thoughts and/or behaviors endorsed on the DISC-Y/P, CBCL, and MAVRIC-P among youth with and without CTD due to small cell sizes. Five participants had incomplete and/or missing DISC-P, and were excluded from analyses on comorbid psychiatric disorders. Cohen's kappa evaluated agreement on the DISC between youth (DISC-Y) and parent report (DISC-P) of suicidal thoughts and/or behaviors when endorsed by at least one informant, as well as agreement between measures of suicidal thoughts and/or behaviors (DISC-Y/P, CBCL, MAVRIC-P).
Pearson's correlation examined the association between suicidal thoughts and/or behaviors and youth's age. A series of chi-square and independent sample t-tests examined the differences in demographics (i.e., age, sex, race/ethnicity), phenotypic presentation (i.e., presence of coprophenomena on the YGTSS symptom checklist), and clinical characteristics among youth with CTD experiencing and not experiencing suicidal thoughts and behaviors. For categorical comparisons, two-tailed Fisher exact tests were used when cell sizes were less than five. Cramer's V was calculated to ascertain the strength of association between categorical variables whereas Cohen's d was calculated to ascertain the strength of association between continuous and ordinal variables.
Independent logistic regression models were used to examine whether specific syndrome subscales on the CBCL predicted suicidal thoughts and/or behaviors on the DISC-Y/P. Bootstrapping mediation techniques were used to evaluate whether parent ratings of child anxiety and depressive symptoms (CBCL anxious/depressed scale) influenced the relationship between tic symptom severity on the YGTSS and the presence of suicidal thoughts and behaviors on the DISC-Y/P. Mediation was tested with 5,000 bootstrap samples and bias-corrected 95% confidence intervals (CI). Full mediation was considered when the indirect effect was significant (i.e., the CI did not include zero) and the c' path was not significant. Mediation calculations were completed using the SPSS macro INDIRECT.43
Results
Agreement on suicide-related items across informants and measures
Table 2 details the number of youth and parents who endorsed each item on the DISC-Y/P that involve thoughts about death/dying, suicidal thoughts, and suicidal behaviors, as well as respondent agreement. Poor to moderate agreement was observed between youth and parents across DISC-Y/P items, highlighting differences across respondents. Table 2 also provides responses to suicidal ideation items on the CBCL and MAVRIC-P. For community controls, there was poor agreement between the DISC-Y/P and the MAVRIC-P (kappa=−0.02, p=0.86) with no overlap in participants identified as experiencing suicidal ideations and/or behaviors. Meanwhile, there was moderate agreement between the DISC-Y/P and the CBCL items (kappa=0.66, p<0.001), with two participants identified by both the DISC-Y/P and CBCL, and one additional community control reportedly experiencing suicidal thoughts and/or behaviors on each measure alone. For youth with CTD, there was poor agreement between the DISC-Y/P and the MAVRIC-P (kappa=0.30, p<0.001), with 7 participants classified as experiencing suicidal thoughts and/or behaviors by both measures. However, 12 participants on the MAVRIC-P and 12 participants on the DISC-Y/P were identified as experiencing suicidal thoughts and/or behaviors without identification by the other measure. Similarly, there was poor agreement between the DISC-Y/P and the CBCL (kappa=0.33, p<0.001), with only 5 participants classified as experiencing suicidal thoughts and/or behaviors. Although 3 participants were positively identified by the CBCL who were not captured by the DISC-Y/P, 14 participants were identified as experiencing suicidal thoughts and/or behaviors by the DISC-Y/P that were missed by the CBCL.
Incidence of endorsed suicide-related items relative to community controls
Given the poor-to-moderate agreement between informants, suicide-related items were considered to be present when endorsed by either self- or parent-report on the DISC-Y/P. A site difference in terms of suicidal thoughts and/or behaviors endorsed was present (USF=16, UR=3; Fisher's exact test, p= 0.006, ES= 0.20). Collectively, there were 19 youth with CTD (9.7%) who experienced suicidal thoughts and/or behaviors as evidenced by a positive response to any of the 3 DISC-Y/P questions; this rate was significantly more often than community control participants (3%, Table 2). When examining individual items on the DISC-Y/P, 8% youth with CTD exhibited thoughts of death or dying over the past year (DISC-Y/P Item#20), which was significantly greater than among community controls (0%, Table 2). Suicidal thoughts (DISC-Y/P Item #21) were identified among 5% youth with CTD) versus 3%community control participants, which was not significantly different (Table 2). Three youth with CTD reported a history of suicidal behaviors (DISC-Y/P Item #22) compared to no community control youth that was not significantly different (Table 2). When examining other parent-report rating scales that included questions related to suicidal thoughts and/or behaviors, there was no significant difference in suicidal thoughts and/or behaviors for those youth with CTD that completed the CBCL and controls on CBCL Item #18 or Item #91 see Table 2). When examining items related to suicidal thoughts and/or behaviors on the MAVRIC-P, there was a significant difference between youth with CTD and community controls on item 15b (10% vs. 1%, Table 2). However, there was no significant difference between youth with CTD and community controls on item 15d (1% vs. 0%, Table 2). Across youth with CTD and community controls, there were 4 participants (3 CTD, 1 community control) who reported suicidal thoughts and/or behaviors on the CBCL (either item #18 or #91) and 13 participants (12 CTD, 1 community control) on the MAVRIC-P (either item #15b or #15d) that were not identified by the DISC-Y/P as experiencing suicidal thoughts and/or behaviors.
Characteristics of youth with suicidal thoughts and/or behaviors
Table 3 presents differences in demographic and clinical characteristics between youth with CTD who experienced suicidal thoughts and behaviors and youth with CTD who did not. Youth with suicidal thoughts and suicidal behaviors were more likely to experience clinically significant obsessive-compulsive symptoms, greater tic severity, tic-related impairment, hyperactivity/impulsivity, oppositional behavior, depressive symptom severity, and anxiety symptom severity. There was no difference in the frequencies of comorbid conditions assessed on the DISC between youth with suicidal thoughts and suicidal behaviors versus those without. Youth who experienced suicidal thoughts and behaviors were more likely express suicidal thoughts and behaviors within the context of anger. No significant association was observed between youth's age and suicidal thoughts and/or behaviors (r=0.11, p=0.13). Elevated T-scores on the anxious/depressed scale, withdrawn scale, social problems scale, thought problems scale, aggressive behavior scale, as well as the total internalizing problems scale were associated with the presence of suicidal thoughts and behaviors among youth with CTD (see Table 4). The remaining scales were not significantly associated with suicidal thoughts and behaviors among youth with CTD.
Table 3.
Difference in Demographic and Clinical Characteristics Among Youth with CTD with and without suicidal thoughts and/or behaviors (N = 196)
| Total Sample of Youth with CTD (n=196) | Youth with CTD and suicidal thoughts (n = 19) | Youth with CTD without suicidal thoughts (n = 177) | Test statistic Value (df) | p-value | ES | |
|---|---|---|---|---|---|---|
| Male | 149 (76%) | 15 (79%) | 134 (76%) | Fisher's | 1.00 | 0.02 |
| Coprophenomena (YGTSS) | 17 (9%) | 4 (21%) | 13 (7%) | Fisher's | 0.07 | 0.14 |
| Attention-deficit/hyperactivity disorder (DISCa) | 81 (41%) | 8 (42%) | 73 (41%) | Χ2 (1) = 0.03 | 0.85 | 0.01 |
| Oppositional defiant disorder (DISCa) | 62 (32%) | 9 (50%) | 53 (30%) | Χ2 (1) = 2.79 | 0.10 | 0.12 |
| Generalized anxiety disorder (DISCa) | 31(16%) | 5 (26%) | 26 (15%) | Χ2(1) = 1.95 | 0.16 | 0.10 |
| Social anxiety disorder (DISCa) | 1 (0.5%) | 1 (5%) | 0 (0%) | Fisher's | 0.09 | 0.23 |
| Major depressive disorder (single episode) (DISCa) | 12 (6%) | 3 (16%) | 9 (5%) | Fisher's | 0.09 | 0.14 |
| Obsessive-compulsive disorder (DISCa) | 53 (27%) | 3 (16%) | 50 (28%) | Χ2 (1) = 1.22 | 0.27 | 0.08 |
| Obsessive-compulsive disorder (CY-BOCS Score ≥ 16) | 86 (44%) | 14 (74%) | 72 (41%) | Χ2(1) = 7.59 | 0.007 | 0.20 |
| Anger-driven suicidal ideation/behavior (MAVRIC-P Item 15b) | 12 (6%) | 6 (32%) | 6 (3%) | Fisher's | < 0.001 | 0.80 |
| Suicide attempt due to anger (MAVRIC-P Item 15d) | 2 (1%) | 1 (5%) | 1 (0.5%) | Fisher's | 0.19 | 0.14 |
| Talks about killing self (CBCL Item #91) | 8 (4%) | 5 (26%) | 3 (2%) | Fisher's | < 0.001 | 0.37 |
| Harms self or attempts suicide (CBCL Item #18) | 3 (1.5%) | 2 (11%) | 1 (0.5%) | Fisher's | 0.03 | 0.24 |
| Mean (SD) | Mean (SD) | Mean (SD) | ||||
|---|---|---|---|---|---|---|
| Age | 11.29 (2.93) | 12.26 (3.21) | 11.18 (2.89) | t(194) =1.54 | 0.13 | 0.37 |
| Tic severity (YGTSS) | 21.66 (9.44) | 26.11(12.56) | 21.18 (8.95) | t(194)=2.18 | 0.03 | 0.53 |
| Tic impairment (YGTSS) | 15.51 (12.67) | 22.90 (14.07) | 14.72 (12.29) | t(193)=2.72 | 0.007 | 0.66 |
| Obsessive-compulsive symptom severity (CY-BOCS Total) | 12.20 (9.60) | 15.68 (9.42) | 11.83 (9.57) | t(194)=1.67 | 0.10 | 0.40 |
| Impulsive aggression (MAVRIC-P) | 7.01 (5.68) | 9.33 (6.62) | 6.77 (5.54) | t(189)=1.84 | 0.07 | 0.46 |
| Parent-reported tic impairment (CTIM-P) | 14.36 (15.43) | 20.82 (17.86) | 13.72 (15.07) | t(185)=1.82 | 0.07 | 0.46 |
| Parent-reported non-tic impairment (CTIM-P) | 22.24 (19.87) | 26.69 (14.65) | 21.82 (20.28) | t(182)=0.94 | 0.35 | 0.25 |
| Inattentive symptoms (SNAP-IV) | 1.43 (0.90) | 1.73 (0.95) | 1.40 (0.89) | t(189)=1.49 | 0.14 | 0.37 |
| Hyperactivity/Impulsivity score (SNAP-IV) | 1.08 (0.80) | 1.44 (0.99) | 1.05 (0.77) | t(189)=2.01 | 0.05 | 0.50 |
| Combined score (SNAP-IV) | 1.26 (0.77) | 1.58 (0.88) | 1.22 (0.76) | t(189)=1.89 | 0.06 | 0.47 |
| Oppositional score (SNAP-IV) | 0.97 (0.79) | 1.61 (0.94) | 0.90 (0.75) | t(189)=3.75 | < 0.001 | 0.93 |
| Depression symptom severity (CDI-S) | 48.08 (11.14) | 53.53 (10.77) | 47.48 (11.05) | t(189)=2.27 | 0.02 | 0.55 |
| Anxiety symptom severity (MASC) | 51.85 (10.82) | 56.94 (14.86) | 51.30 (10.19) | t(182)=2.12 | 0.04 | 0.53 |
Note: Fisher's = Fisher's exact test; CDI-S = Children's Depression Inventory-Short Form, CY-BOCS = Children's Yale–Brown Obsessive–Compulsive Scale, ES = Effect size, MASC = Multidimensional Anxiety Scale for Children, SNAP = Swanson Nolan and Pelham Rating Scale, YGTSS = Yale Global Tic Severity Scale.
Total sample size for comorbid diagnoses on DISC-P is 191 (18 and 173 respectively). Reported percentages are adjusted accordingly.
Table 4.
Predictors of Suicidal Thoughts and/or Behaviors among Youth with CTD (N = 192)
| Child Behavior Checklist Subscale | B (SE) | Odds Ratio | 95% CI | p |
|---|---|---|---|---|
| Anxious/Depressed T-score | 0.06 (0.02) | 1.06 | 1.02, 1.11 | 0.005 |
| Withdrawn T-Score | 0.06 (0.03) | 1.07 | 1.01, 1.12 | 0.02 |
| Somatic T-score | −0.00 (0.03) | 1.00 | 0.95, 1.05 | 0.95 |
| Social Problems T-score | 0.05 (0.02) | 1.05 | 1.00, 1.10 | 0.05 |
| Thought Problems T-score | 0.07 (0.03) | 1.07 | 1.01, 1.14 | 0.02 |
| Attention Problems T-score | 0.03 (0.02) | 1.03 | 0.99, 1.08 | 0.19 |
| Rule Breaking T-Score | 0.02 (0.03) | 1.02 | 0.96, 1.09 | 0.56 |
| Aggressive Behavior T-Score | 0.05 (0.02) | 1.05 | 1.00, 1.10 | 0.04 |
| Total Internalizing Scale T-Score | 0.06 (0.03) | 1.06 | 1.00, 1.11 | 0.03 |
| Total Externalizing Scale T-Score | 0.04 (0.02) | 1.04 | 0.99, 1.09 | 0.08 |
Relationship between tic severity, suicidal thoughts and/or behaviors, and anxiety/depression
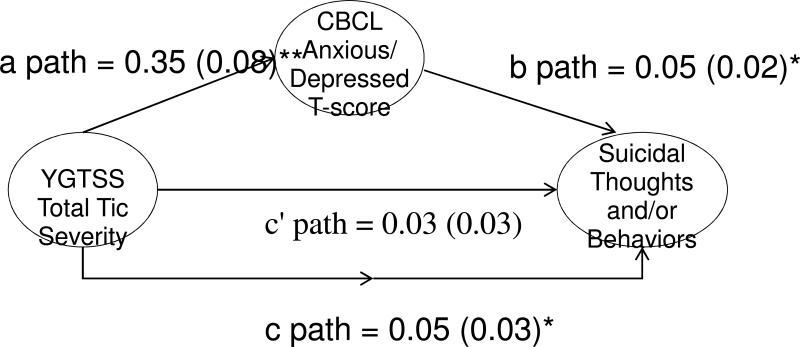
Figure 1 presents the effects for the proposed mediation relationship between tic severity, parent-ratings of child anxiety and depressive symptoms, and suicidal thoughts and behaviors. The CBCL Anxious/Depressed T-scores fully mediated the relationship between tic severity and suicidal thoughts and behaviors with a significant indirect effect (0.02, 95% CI: 0.002, 0.045).
Figure 1.
Parent-reported scores on the Child Behavior Checklist (CBCL) Anxious/Depressed scale mediated the relationship between tic severity and suicidal thoughts and/or behaviors. The c' path takes into account the purposed mediator while the C path does not. Path coefficients and standard error are reported for direct and indirect effects. The *p < 0.05, **p < 0.01
Discussion
Suicidal and death ideation among youth with CTD occurred with modest frequency (5% and 8%, respectively) with death ideation but not suicidal ideation being more frequent in youth with CTD than in community control youth. These estimates are lower than found in non-clinical settings, and lower than among youth with clinically significant anxiety,12 depressive,10, 11, 13 and behavioral disorders.10 Suicidal behaviors were relatively infrequent in youth with CTD with three youngsters (~1.5%) having attempted suicide. For youth with CTD, suicidal thoughts and behaviors frequently occurred in the context of anger/frustration relative to community controls. These rates of suicidal thoughts, behaviors, and attempts remain very concerning in a potentially vulnerable sample, providing strong evidence for careful clinical assessment for the presence of suicidality and associated risk factors among youth with CTD. Elevated responses on the CBCL anxious/depressed, withdrawn, social problems, thought problems, and aggressive behavior scales were associated with the presence of suicidal thoughts and behaviors suggesting potential variables that may be related to increased risk in this population. When administering this general screening measure among youth with CTD, clinicians should be advised to inquire about suicidal thoughts and behaviors for youth who report elevated ratings on these scales.
Frequency of suicidal thoughts and behaviors were associated with tic symptom severity, tic-related impairment, hyperactivity/impulsivity, oppositional behavior, depressive symptom severity, obsessive-compulsive symptom severity, and anxiety symptom severity. Consistent with others,15, 44 youth with coprophenomena were more likely to experience suicidal thoughts and suicidal behaviors, but this difference only trended towards statistical significance. There are several ways of understanding these relationships. First, increased tic symptom severity and related impairment may contribute to heightened distress, which translates into increased risk of suicidal thoughts and/or behaviors. Youth with more severe tics, including coprophenomena, are more likely to experience peer torment2 and struggle with social acceptance.45 These negative peer interactions coupled with more limited peer support may put youth with CTD at greater risk for suicidal thoughts and behaviors. Second, the direct association with externalizing behaviors may reflect a level of impulsiveness that manifests in suicidality. In some cases, this may reflect suicidal gestures being expressed in an impulsive manner when upset or distressed, which may pose a challenge for parents and clinicians in assessing the degree of intent. Third, direct associations with obsessive-compulsive, anxiety and depressive symptoms may reflect the impact of additional psychiatric morbidity on the affected child. As impairment and distress are compounded with the presence of additional psychiatric burden, youth with CTD may be more prone to experiencing suicidal thoughts and/or behavior. Interestingly, these patterns of relationships were not found when examining categorical diagnoses on the DISC. This may reflect limitations of non-dimensional measures and/or that those with a more severe symptom threshold may be most affected relative to youth who meet criteria for the disorder but may be more modestly affected.
Youth with CTD with and without suicidal thoughts and behavior did not differ in terms of sex, age, and certain clinical constructs (e.g., inattention). These non-significant relationships may suggest that these variables are not strongly associated with suicidal thoughts and behaviors in youth with CTD. Regarding age, some evidence suggests that suicidal thoughts and behaviors increase in frequency during adolescence;19 however, no significant association with age was present among youth with CTD. Sex was not associated with suicidal thoughts and behavior, which differs from findings in youth without CTD.10, 13 On balance, our sample was predominately male and further exploration of sex differences may be warranted.
Parent-child agreement on the presence of suicidal thoughts and behaviors was poor, which is consistent with others.46, 47 This may reflect differential accuracy of reporters. In some instances, children may be more accurate reporters than their parents of internalizing symptoms – including suicidal ideation – given their covert nature.48 Many youth with tics exhibit anger attacks during which suicidal expressions may be made; although the child may not experience such statements as reflecting suicidality, parents may endorse this as such. Consistent with best practice guidelines for the assessment and treatment of suicidal behaviors,49, 50 the poor parent-child agreement reflects the need for both parents and children to be interviewed to comprehensively assess the presence or absence of suicidal thoughts and suicidal behaviors.
There are several study limitations. First, it would have been preferable to use a more comprehensive, multi-method approach to assessing suicidal thoughts and behaviors, versus the use of the DISC-Y/P. This highlights the need for future studies to employ more comprehensive measures of suicidal thoughts and behaviors in studies of CTD. Second, the treatment seeking nature and sociodemographic characteristics (e.g., primarily Caucasian, male subjects) of the sample potentially limits results generality. Third, the cross-sectional nature of this study does not allow a prospective analysis of the development of suicidal thoughts and behaviors. Fourth, given the increased prevalence of comorbidities and social stressors associated with CTD, we utilized one-tailed tests for our a priori hypothesis that youth with CTD would have a greater endorsement of suicidal thoughts and/or behaviors relative to controls. Although a possible limitation due to the directional nature of this test, we reexamined the data using a conservative two-tailed test (that does not assume directionality) with results trending toward significance (p=0.058). Fifth, a site difference in terms of suicidal thoughts and/or behaviors endorsed was present with lower rates of suicidal thoughts and/or behaviors at UR, which was also the site that recruited community control subjects. On balance, the DISC is a computer administered scale and thus, differences are not believed due to differences in scale administration. Finally, comorbid diagnoses relied on a structured diagnostic interview (i.e., DISC-Y/P). Although reliable and valid, these diagnoses ratings did not incorporate all available clinical information, which may partially account for the varied associations between suicidal thoughts and behaviors and diagnosis versus dimensional symptom assays.
Within these limitations, these data have important clinical implications and indicate directions for future study. With regards to assessment, a significant number of youth with CTD experienced suicidal thoughts and behavior. While evidence-based assessment of suicidal thoughts and behavior should be conducted with every patient,49, 50 clinicians should be aware of potential risk factors that may elevate risk in this cohort, specifically when tics are most severe and impairing, and in the presence of elevated anxiety, depressive, obsessive-compulsive, and externalizing symptoms.
Pertaining to treatment, pharmacological and behavioral interventions for children and adolescents with CTD are largely geared towards reduction in tic severity. Yet, for many youngsters, it is not the tics that are most problematic but rather the co-occurring problems many youth experience.51 Consistent with treatment recommendations for CTD,51 co-occurring conditions should be identified and may need to be the primary focus of treatment depending on relative impairment. Directly addressing stressors may also prove useful.52 For example, it may be beneficial to interface with school personnel to mitigate peer torment, educate youth about CTD,53 and promote adaptive peer relationships. On the other hand, it may be that improvements in tic symptom severity translate into reduced distress inclusive of suicidal thoughts and behavior. This phenomenon has been demonstrated using behavioral treatment for children and adolescents with CTD in which positive response was associated with decreased anxiety, disruptive behavior, family strain, and social impairment.52 A critical difference, however, is that the magnitude of response and the percentage of overall responders to behavioral therapy seems to be greater in youth affected by OCD relative to CTD54-57 making it unclear if a similar pattern of results would emerge in youth with CTD.
Acknowledgments
This work was supported by cooperative agreements to the third and last authors from the Centers for Disease Control and Prevention (U01DD000509-01). The authors would like to acknowledge the contributions of Leah Jung, Nicole Walsh, and all of the participating families. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
This study was carried out prior to the publication of the Diagnostic and Statistical Manual for Mental Disorders, 5th edition (DSM-5). Youth with Tic Disorder-NOS (n=7) were not included in these analyses due to the sub-chronic nature of their tics (duration ≤1 year at time of evaluation).
References
- 1.Gaze C, Kepley HO, Walkup JT. Co-occurring psychiatric disorders in children and adolescents with Tourette syndrome. J Child Neurol. 2006;21(8):657–664. doi: 10.1177/08830738060210081301. [DOI] [PubMed] [Google Scholar]
- 2.Storch EA, Murphy TK, Chase RM, Keeley M, Goodman WK, Murray M, Geffken GR. Peer victimization in youth with Tourette's syndrome and chronic tic disorder: relations with tic severity and internalizing symptoms. J Psychopath Behav Assess. 2007;29(4):211–219. [Google Scholar]
- 3.Zinner SH, Conelea CA, Glew GM, Woods DW, Budman CL. Peer victimization in youth with Tourette syndrome and other chronic tic disorders. Child Psychiatry Human Dev. 2012;43(1):124–136. doi: 10.1007/s10578-011-0249-y. [DOI] [PubMed] [Google Scholar]
- 4.McGuire JF, Hanks C, Lewin AB, Storch EA, Murphy TK. Social deficits in children with chronic tic disorders: Phenomenology, clinical correlates and quality of life. Comp Psychiatry. 2013;54(7):1023–1031. doi: 10.1016/j.comppsych.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 5.Bawden HN, Stokes A, Carol S, Carol S, Camfield PR, Salisbury S. Peer relationship problems in children with Tourette's disorder or diabetes mellitus. J Child Psychol Psychiatry. 1998;39(5):663–668. [PubMed] [Google Scholar]
- 6.Davis KK, Davis JS, Dowler L. In motion, out of place: the public space(s) of Tourette Syndrome. Social Science Med. 2004;59(1):103–112. doi: 10.1016/j.socscimed.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 7.Thibert AL, Day HI, Sandor P. Self-concept and self-consciousness in adults with Tourette syndrome. Canadian J Psychiatry. 1995;40(1):35–39. doi: 10.1177/070674379504000109. [DOI] [PubMed] [Google Scholar]
- 8.Brent DA, Perper JA, Moritz G, Allman C, Friend A, Roth C, Schweers J, Balach L, Baugher M. Psychiatric risk factors for adolescent suicide: a case-control study. J Am Acad Child Adol Psychiatry. 1993;32(3):521–529. doi: 10.1097/00004583-199305000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. J Child Psychol Psychiatry. 2006;47(3-4):372–394. doi: 10.1111/j.1469-7610.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- 10.Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, Kessler RC. Prevalence, Correlates, and Treatment of Lifetime Suicidal Behavior Among AdolescentsResults From the National Comorbidity Survey Replication Adolescent SupplementLifetime Suicidal Behavior Among Adolescents. JAMA Psychiatry. 2013;70(3):300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beautrais AL, Joyce PR, Mulder RT. Risk factors for serious suicide attempts among youths aged 13 through 24 years. J Am Acad Child Adol Psychiatry. 1996;35(9):1174–1182. doi: 10.1097/00004583-199609000-00015. [DOI] [PubMed] [Google Scholar]
- 12.Carter R, Silverman WK, Allen A, Ham L. Measures matter: the relative contribution of anxiety and depression to suicidal ideation in clinically referred anxious youth using brief versus full length questionnaires. Depress Anxiety. 2008;25(8):E27–35. doi: 10.1002/da.20468. [DOI] [PubMed] [Google Scholar]
- 13.Esposito CL, Clum GA. Psychiatric symptoms and their relationship to suicidal ideation in a high-risk adolescent community sample. J Am Acad Child Adol Psychiatry. 2002;41(1):44–51. doi: 10.1097/00004583-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Davila G, Berthier ML, Kulisevsky J, Jurado Chacon S. Suicide and attempted suicide in Tourette's syndrome: a case series with literature review. J Clin Psychiatry. 2010;71(10):1401–1402. doi: 10.4088/JCP.09l05669blu. [DOI] [PubMed] [Google Scholar]
- 15.Cheung MY, Shahed J, Jankovic J. Malignant Tourette syndrome. Mov Disord. 2007;22(12):1743–1750. doi: 10.1002/mds.21599. [DOI] [PubMed] [Google Scholar]
- 16.Conelea CA, Woods DW, Zinner SH, Budman C, Murphy T, Scahill LD, Compton SN, Walkup J. Exploring the impact of chronic tic disorders on youth: results from the Tourette Syndrome Impact Survey. Child Psychiatry Human Devel. 2011;42(2):219–242. doi: 10.1007/s10578-010-0211-4. [DOI] [PubMed] [Google Scholar]
- 17.Impey M, Heun R. Completed suicide, ideation and attempt in attention deficit hyperactivity disorder. Acta Psychiatrica Scandinavica. 2012;125(2):93–102. doi: 10.1111/j.1600-0447.2011.01798.x. [DOI] [PubMed] [Google Scholar]
- 18.Storch EA, Bussing R, Jacob ML, Nadeau JM, Crawford E, Mutch PJ, Mason D, Lewin AB, Murphy TK. Frequency and Correlates of Suicidal Ideation in Pediatric Obsessive-Compulsive Disorder. Child Psychiatry Human Devel. 2014:1–9. doi: 10.1007/s10578-014-0453-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shah A. The relationship between suicide rates and age: an analysis of multinational data from the World Health Organization. Int Psychogeriatr. 2007;19(6):1141–1152. doi: 10.1017/S1041610207005285. [DOI] [PubMed] [Google Scholar]
- 20.Beautrais AL. Suicide and serious suicide attempts in youth: a multiple-group comparison study. Am J Psychiatry. 2003;160(6):1093–1099. doi: 10.1176/appi.ajp.160.6.1093. [DOI] [PubMed] [Google Scholar]
- 21.Foley DL, Goldston DB, Costello EJ, Angold A. Proximal psychiatric risk factors for suicidality in youth: the Great Smoky Mountains Study. Arch Gen Psychiatry. 2006;63(9):1017–1024. doi: 10.1001/archpsyc.63.9.1017. [DOI] [PubMed] [Google Scholar]
- 22.Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adol Psychiatry. 2000;39(1):28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 23.SAS . SAS Version 9.2. SAS Institute Inc.; Cary, NC: 2008. [Google Scholar]
- 24.Silverman WK, Saavedra LM, Pina AA. Test-Retest Reliability of Anxiety Symptoms and Diagnoses With the Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions. J Am Acad Child Adol Psychiatry. 2001;40(8):937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- 25.Leckman JF, Riddle MA, Hardin MT, Ort SI, Swartz KL, Stevenson J, Cohen DJ. The Yale Global Tic Severity Scale: initial testing of a clinician-rated scale of tic severity. J Am Acad Child Adol Psychiatry. 1989;28(4):566–573. doi: 10.1097/00004583-198907000-00015. [DOI] [PubMed] [Google Scholar]
- 26.Storch EA, Murphy TK, Geffken GR, Sajid M, Allen P, Roberti JW, Goodman WK. Reliability and validity of the Yale Global Tic Severity Scale. Psychol Assess. 2005;17(4):486. doi: 10.1037/1040-3590.17.4.486. [DOI] [PubMed] [Google Scholar]
- 27.Walkup JT, Rosenberg LA, Brown J, Singer HS. The validity of instruments measuring tic severity in Tourette's syndrome. J Am Acad Child Adol Psychiatry. 1992;31(3):472–477. doi: 10.1097/00004583-199205000-00013. [DOI] [PubMed] [Google Scholar]
- 28.Jeon S, Walkup JT, Woods DW, Peterson A, Piacentini J, Wilhelm S, Katsovich L, McGuire JF, Dziura J, Scahill L. Detecting a clinically meaningful change in tic severity in Tourette syndrome: A comparison of three methods. Cont Clinical Trials. 2013;36(2):414–420. doi: 10.1016/j.cct.2013.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Storch EA, De Nadai AS, Lewin AB, McGuire JF, Jones AM, Mutch PJ, Shytle RD, Murphy TK. Defining treatment response in pediatric tic disorders: a signal detection analysis of the Yale Global Tic Severity Scale. J Child Adol Psychopharm. 2011;21(6):621–627. doi: 10.1089/cap.2010.0149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Scahill L, Riddle MA, McSwiggin-Hardin M, Ort SI, King RA, Goodman WK, Cicchetti D, Leckman JF. Children's Yale-Brown obsessive compulsive scale: reliability and validity. J Am Acad Child Adol Psychiatry. 1997;36(6):844–852. doi: 10.1097/00004583-199706000-00023. [DOI] [PubMed] [Google Scholar]
- 31.Storch EA, Murphy TK, Geffken GR, Soto O, Sajid M, Allen P, Roberti JW, Killiany EM, Goodman WK. Psychometric evaluation of the Children's Yale–Brown Obsessive-Compulsive Scale. Psychiatry Research. 2004;129(1):91–98. doi: 10.1016/j.psychres.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 32.Storch EA, Murphy TK, Geffken GR, Bagner DM, Soto O, Sajid M, Allen P, Killiany EM, Goodman WK. Factor Analytic Study of the Children's Yale–Brown Obsessive–Compulsive Scale. J Clin Child Adol Psychol. 2005;34(2):312–319. doi: 10.1207/s15374424jccp3402_10. [DOI] [PubMed] [Google Scholar]
- 33.Lewin AB, Piacentini J, De Nadai AS, Jones AM, Peris TS, Geffken GR, Geller DA, Nadeau JM, Murphy TK, Storch EA. Defining clinical severity in pediatric obsessive-compulsive disorder. Psychol Assess. 2014;26(2):679–684. doi: 10.1037/a0035174. [DOI] [PubMed] [Google Scholar]
- 34.Storch EA, Lack CW, Simons LE, Goodman WK, Murphy TK, Geffken GR. A measure of functional impairment in youth with Tourette's syndrome. J Ped Psychol. 2007;32(8):950–959. doi: 10.1093/jpepsy/jsm034. [DOI] [PubMed] [Google Scholar]
- 35.Achenbach TM. Manual for the ASEBA School-Age Forms and Profiles. University of Vermont; Burlington: 2001. [Google Scholar]
- 36.Achenbach TM, Dumenci L, Rescorla LA. DSM-oriented and empirically based approaches to constructing scales from the same item pools. J Clin Child Adol Psychol. 2003;32(3):328–340. doi: 10.1207/S15374424JCCP3203_02. [DOI] [PubMed] [Google Scholar]
- 37.Swanson JM. School-based assessments and interventions for ADD students. KC Publishing; Irvine, CA: 1992. [Google Scholar]
- 38.Swanson JM, Kraemer HC, Hinshaw SP, Arnold LE, Conners CK, Abikoff HB, Clevenger W, Davies M, Elliott GR, Greenhill LL. Clinical relevance of the primary findings of the MTA: success rates based on severity of ADHD and ODD symptoms at the end of treatment. J Am Acad Child Adol Psychiatry. 2001;40(2):168–179. doi: 10.1097/00004583-200102000-00011. [DOI] [PubMed] [Google Scholar]
- 39.Bass J, Geenens D, Popper C. Measure of aggression, violence, and rage in children (MAVRIC).. Paper presented at: Proceedings of the Annual Meeting of the American Academy of Child and Adolescent Psychiatry; San Francisco, CA. 1993. [Google Scholar]
- 40.Goodman G, Bass JN, Geenens DL, Popper CW. The MAVRIC–C and MAVRIC–P: A Preliminary Reliability and Validity Study. J Pers Assess. 2006;86(3):273–290. doi: 10.1207/s15327752jpa8603_04. [DOI] [PubMed] [Google Scholar]
- 41.Kovaks M. Children's depression inventory. Psychopharm Bull. 1985;21:995–998. [PubMed] [Google Scholar]
- 42.March JS, Parker JD, Sullivan K, Stallings P, Conners CK. The Multidimensional Anxiety Scale for Children (MASC): factor structure, reliability, and validity. J Am Acad Child Adol Psychiatry. 1997;36(4):554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- 43.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Beh Res Meth. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 44.Freeman RD, Fast DK, Burd L, Kerbeshian J, Robertson MM, Sandor P. An international perspective on Tourette syndrome: selected findings from 3500 individuals in 22 countries. Devel Med Child Neurology. 2000;42(7):436–447. doi: 10.1017/s0012162200000839. [DOI] [PubMed] [Google Scholar]
- 45.Leckman JF, Bloch MH, Scahill L, King RA. Tourette syndrome: the self under siege. J Child Neurology. 2006;21(8):642–649. doi: 10.1177/08830738060210081001. [DOI] [PubMed] [Google Scholar]
- 46.Klaus NM, Mobilio A, King CA. Parent-Adolescent Agreement Concerning Adolescents' Suicidal Thoughts and Behaviors. J Clin Child Adol Psychol. 2009;38(2):245–255. doi: 10.1080/15374410802698412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Prinstein MJ, Nock MK. Parents under-report children's suicide ideation and attempts. Evidence Based Mental Health. 2003;6(1):12–12. doi: 10.1136/ebmh.6.1.12. [DOI] [PubMed] [Google Scholar]
- 48.Engel NA, Rodrigue JR, Geffken GR. Parent-child agreement on ratings of anxiety in children. Psychol Rep. 1994;75(3 Pt 1):1251–1260. doi: 10.2466/pr0.1994.75.3.1251. [DOI] [PubMed] [Google Scholar]
- 49.AACAP. Shaffer D, Pfeffer CR, Bernet W, Arnold V, Beitchman J, Benson RS, Bukstein O, Kinlan J, McClellan J, Rue D, Shaw J. Practice parameter for the assessment and treatment of children and adolescents with suicidal behavior. J Am Acad Child Adol Psychiatry. 2001;40(7 Supplement) [Google Scholar]
- 50.Mann JJ, Apter A, Bertolote J, Beautrais A, Currier D, Haas A, Hegerl U, Lonnqvist J, Malone K, Marusic A, Mehlum L, Patton G, Phillips M, Rutz W, Rihmer Z, Schmidtke A, Shaffer D, Silverman M, Takahashi Y, Varnik A, Wasserman D, Yip P, Hendin H. Suicide prevention strategies: a systematic review. JAMA. 2005;294(16):2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 51.Murphy TK, Lewin AB, Storch EA, Stock S, AACAP-CQI Practice parameter for the assessment and treatment of children and adolescents with Chronic Tic Disorders. J Am Acad Child Adol Psychiatry. 2013;52(12):1341–1359. doi: 10.1016/j.jaac.2013.09.015. [DOI] [PubMed] [Google Scholar]
- 52.Woods DW, Piacentini JC, Scahill L, Peterson AL, Wilhelm S, Chang S, Deckersbach T, McGuire J, Specht M, Conelea CA, Rozenman M, Dzuria J, Liu H, Levi-Pearl S, Walkup JT. Behavior therapy for tics in children: acute and long-term effects on psychiatric and psychosocial functioning. J Child Neurol. 2011;26(7):858–865. doi: 10.1177/0883073810397046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Woods DW, Marcks BA. Controlled evaluation of an educational intervention used to modify peer attitudes and behavior toward persons with Tourette's Syndrome. Beh Mod. 2005;29(6):900–912. doi: 10.1177/0145445505279379. [DOI] [PubMed] [Google Scholar]
- 54.Piacentini J, Bergman RL, Chang S, Langley A, Peris T, Wood JJ, McCracken J. Controlled comparison of family cognitive behavioral therapy and psychoeducation/relaxation training for child obsessive-compulsive disorder. J Am Acad Child Adol Psychiatry. 2011;50(11):1149–1161. doi: 10.1016/j.jaac.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Piacentini J, Woods DW, Scahill L, Wilhelm S, Peterson AL, Chang S, Ginsburg GS, Deckersbach T, Dziura J, Levi-Pearl S, Walkup JT. Behavior therapy for children with Tourette disorder: a randomized controlled trial. JAMA. 2010;303(19):1929–1937. doi: 10.1001/jama.2010.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wilhelm S, Peterson AL, Piacentini J, Woods DW, Deckersbach T, Sukhodolsky DG, Chang S, Liu H, Dziura J, Walkup JT, Scahill L. Randomized trial of behavior therapy for adults with Tourette syndrome. Archi Gen Psychiatry. 2012;69(8):795–803. doi: 10.1001/archgenpsychiatry.2011.1528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McGuire JF, Piacentini J, Brennan EA, Lewin AB, Murphy TK, Small BJ, Storch EA. A meta-analysis of behavior therapy for Tourette Syndrome. J Psychiatric Res. 2014;50:106–112. doi: 10.1016/j.jpsychires.2013.12.009. [DOI] [PubMed] [Google Scholar]