Abstract
Progesterone has been shown to have neuroprotective effects in multiple animal models of brain injury, whereas the efficacy and safety in patients with traumatic brain injury (TBI) remains contentious. Here, a total of seven randomized controlled trials (RCTs) with 2492 participants were included to perform this meta-analysis. Compared with placebo, there was no significant decrease to be found in the rate of death or vegetative state for patients with acute TBI (RR = 0.88, 95%CI = 0.70, 1.09, p = 0.24). Furthermore, progesterone was not associated with good recovery in comparison with placebo (RR = 1.00, 95%CI = 0.88, 1.14, p = 0.95). Together, our study suggested that progesterone did not improve outcomes over placebo in the treatment of acute TBI.
Traumatic brain injury (TBI) is a leading cause of death and disability and without effective treatment in children and young adults1,2,3. Despite improvement in outcome following brain injury in recent years, large numbers of patients remain disabled and dependent2,4. Previous animal studies suggested that progesterone could extenuate neural damage effectively by reducing free radicals, inflammatory cytokines, excitotoxicity, apoptosis, and vasogenic edema in the model of neurologic injury5,6,7. However, the relevant clinical trials of progesterone demonstrated different clinical benefits and discrepant conclusions for the treatment of patients with acute TBI8,9. Treatment recommendations may be misleading according to the results of any individual trial. Based on available data, we performed a meta-analysis of randomized clinical trials to compare progesterone with placebo for the treatment of patients with severe or moderate acute TBI. The overall evaluation was performed to accurately detail the efficacy and safety of progesterone.
Results
Study selection and characteristics
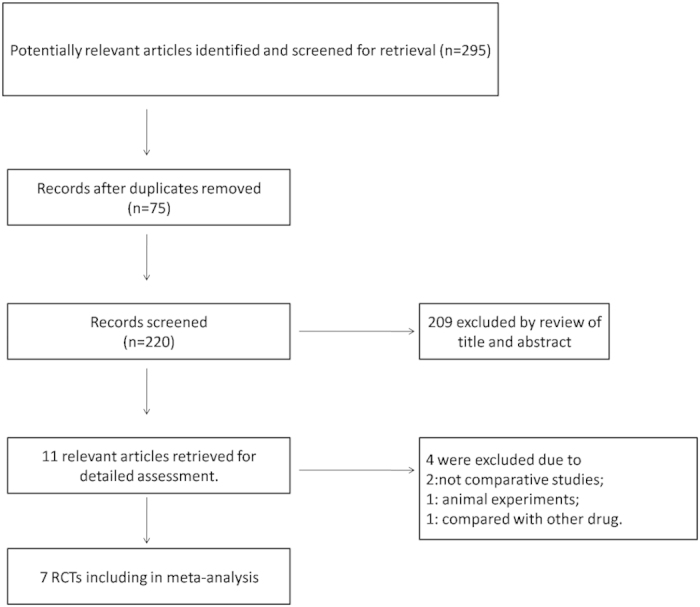
The detailed process of selection is shown in Fig. 1. In total, 295 potential studies were identified with a systematic search of databases. Seventy-five records were excluded as duplicates. We removed 209 apparently unsuitable articles including reviews, case reports and animal experiments after browsing titles and abstracts. The remaining studies were screened and assessed in detail by reviewing full texts. Four articles were excluded due to the following reasons: two excluded studies were not comparative trials, 1 study was an animal experiment, and 1 study involved comparison with another drug. Thus, 7 studies meeting our inclusion criteria were selected in this meta-analysis.
Figure 1. Flow chart of the selection process used for the randomized controlled trials.
These seven studies, with 2492 total participants (Sample size, from 40 to 1179), compared progesterone with placebo in the treatment of acute TBI. Of these, only patients with severe TBI (Glasgow Coma Scale (GCS) ≤8) were included in five studies8,9,10,11,12, and in another 2 studies patients were recruited with moderate-to-severe TBI (GCS ≤12)13,14. All female patients were excluded in one included study12. The primary characteristics and quality assessments of the included RCTs are summarized in Table 1 and 2, respectively.
Table 1. Basic characteristics of studies included in the meta-analysis.
| Study/Year | Trial design | No. of Patients | Age (y) | Male (%) | GCS on admission | Treatment | Follow-up (M) |
|---|---|---|---|---|---|---|---|
| Skolnick 2014 | RCT | 1179 | 16 to 70 | 927(78.63) | 4 to 8 | Intravenously 0.71 mg/kg for the first hour, then 0.50 mg/kg per hour for 119 hours | 6 |
| Shakeri 2013 | RCT | 76 | 18 to 60 | 76(100.00) | 3 to 8 | orally 1 mg/kg every 12 hours for 5 days | 3 |
| Xiao 2008 | RCT | 159 | 18 to 65 | 115(72.33) | ≤8 | intravenously 1.0 mg/kg every 12 hours for 5 days | 6 |
| Wright 2007 | RCT | 100 | old than 18 | 71(71.00) | 4 to 12 | intravenously 0.71 mg/kg for the first hour, 0.5 mg/kg per hour for the next 11 hours, then 0.5 mg/kg per hour every 12 hours for 60 hours | 1 |
| Wright 2014 | RCT | 882 | 17 to 94 | 650(73.70) | 4 to 12 | intravenously 0.71 mg/kg for the first hour, then 0.5 mg/kg for 71 hours, then 0.125 mg/kg per hour every 8 hours for 96 hours | 6 |
| Xiao 2007 | RCT | 56 | 15 to 65 | 33(58.93) | 5 to 8 | Intramuscularly 80 mg every 12 hours for 5 days | 3 |
| Aminmansour 2012 | RCT | 40 | 29.73* | 28(70.00) | ≤8 | intramuscularly 1 mg/kg of progesterone every 12 hours for 5 days | 3 |
RCT, randomized controlled trial; GCS, Glasgow Coma Scale; Y, year; M, month; *mean age.
Table 2. Risk of bias of the articles included in the meta-analysis.
| Study, year | Randomization method | Allocation concealment | Data collection blinded | Incomplete outcome data | Selective reporting |
|---|---|---|---|---|---|
| Skolnick 2014 | Low risk | Low risk | Low risk | Low risk | Low risk |
| Shakeri 2013 | Low risk | Unclear risk | High risk | Unclear risk | Low risk |
| Xiao 2008 | Low risk | Low risk | Low risk | Low risk | Unclear risk |
| Wright 2007 | Low risk | Low risk | Low risk | Low risk | Low risk |
| Wright 2014 | Low risk | Low risk | Low risk | Low risk | Low risk |
| Xiao 2007 | Low risk | Unclear risk | Unclear risk | Unclear risk | Unclear risk |
| Aminmansour 2012 | Low risk | Low risk | Unclear risk | Low risk | Low risk |
Meta-analysis outcomes
Death or vegetative state
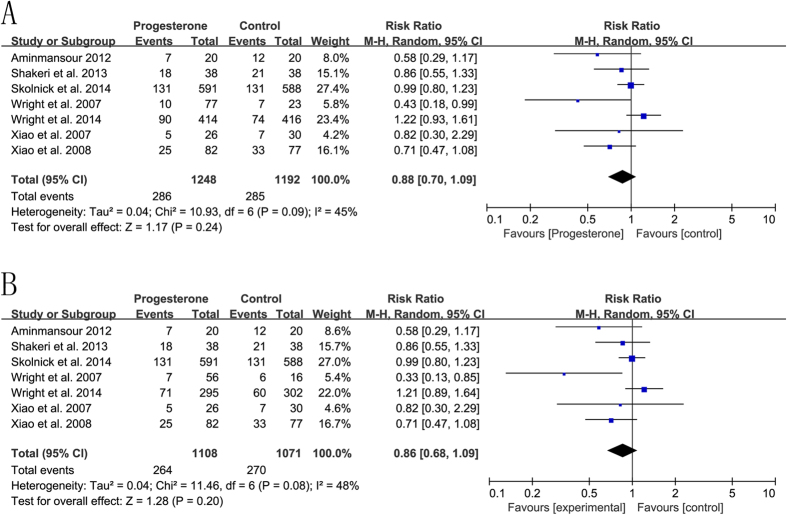
The meta-analysis of seven RCTs with a random-effects model demonstrated that progesterone did not significantly reduce the rate of death or vegetative state in patients with acute TBI between the two groups (RR = 0.88, 95%CI = 0.70, 1.09, p = 0.24, I2 = 45%) (Fig. 2A). Subgroup meta-analysis was performed (Table 3). Due to the limited number of available studies, meta-regression was not pursued further. A similar result was observed in patients with severe TBI (RR = 0.86, 95%CI = 0.68, 1.09, p = 0.20, I2 = 48%) (Fig. 2B). The sensitivity analysis was performed to examine the influence of different models on the pooled estimates. There were no significant changes to be found with a fixed-effects model (RR = 0.97, 95%CI = 0.84, 1.11, p = 0.65; RR = 0.95, 95%CI = 0.82, 1.10, p = 0.50).
Figure 2. The efficacy of progesterone in reducing the rate of death or vegetative state in comparison to placebo.
(A) acute traumatic brain injury; (B) acute severe traumatic brain injury.
Table 3. Subgroup analysis for RCTs evaluating the efficacy in reducing death or vegetative state of patients with acute TBI.
| N | RR | 95% CI | Heterogeneity test(I2) | |
|---|---|---|---|---|
| Date of publication | ||||
| Before 2010 | 3 | 0.67 | 0.47, 0.94 | 0% |
| After 2010 | 4 | 0.99 | 0.80, 1.23 | 38% |
| Sample size | ||||
| ≤100 | 4 | 0.70 | 0.50, 0.96 | 0% |
| >100 | 3 | 0.99 | 0.77, 1.28 | 56% |
| Follow-up | ||||
| 1 m | 1 | 0.43 | 0.18, 0.99 | — |
| 3 m | 3 | 0.77 | 0.54, 1.10 | 0% |
| 6 m | 3 | 0.99 | 0.77, 1.28 | 56% |
| Administration | ||||
| Intravenously | 4 | 0.90 | 0.67, 1.22 | 65% |
| Intramuscularly | 2 | 0.67 | 0.37, 1.19 | 0% |
| Orally | 1 | 0.71 | 0.39, 1.27 | — |
m, month; N, number of studies; CI: confidence interval; RR: risk ratios.
Good recovery
In total, five of the included RCTs had an assessment of good recovery (GOS = 5) at the end of follow-up. No significant heterogeneity was observed in TBI (I2 = 0%). Compared with placebo, the combined data using a fixed-effects model did not show that progesterone significantly increased the rate of good recovery (RR = 1.00, 95%CI = 0.88, 1.14, p = 0.95) (Fig. 3A). There was also no evidence to indicate that progesterone could improve the outcome for a good recovery in severe TBI (RR = 1.04, 95%CI = 0.91, 1.19, p = 0.54, I2 = 0%) (Fig. 3B).
Figure 3. The efficacy of progesterone in improving outcomes (good recovery) in comparison with placebo.
(A) acute traumatic brain injury; (B) acute severe traumatic brain injury.
Adverse events
Two studies were included in the meta-analysis of adverse events. A fixed-effects model was used according to heterogeneity. There were no statistically significant differences in pneumonia or sepsis between the two groups (RR = 0.95, 95%CI = 0.85, 1.07, p = 0.42, I2 = 0%; RR = 1.10, 95%CI = 0.76, 1.60, p = 0.61, I2 = 0%) (Fig. 4).
Figure 4. Safety of progesterone in the treatment of traumatic brain injury.
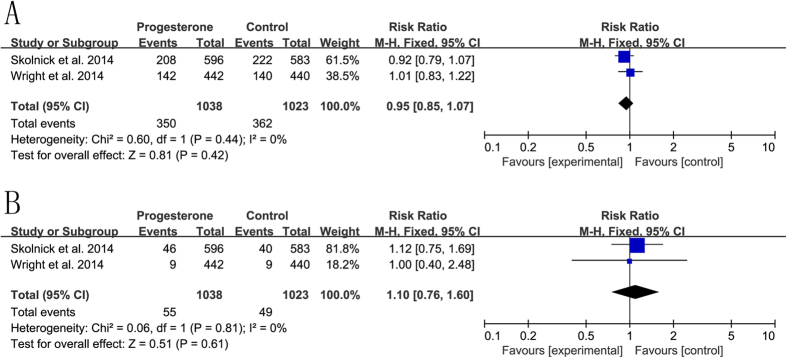
(A) pneumonia; (B) sepsis.
Publication bias
There was no evidence of publication bias (Begg’s test, P = 0.90; Egg’s test, P = 0.059).
Discussion
The pathophysiology of acute TBI is a complex, interwoven and multifactorial process, which includes primary and secondary injury15,16. TBI-induced secondary injury has been considered to be a potential target for therapeutic intervention involving reduction and prevention of inflammation, calcium flux, oxidative stress, necrosis, and apoptosis17,18. Based on the efficacy and safety in animal models, progesterone has been regarded to be a potent candidate for the treatment of TBI19,20,21,22. However, the relevant clinical trials of progesterone came to inconsistent conclusions10,12,14. The previous review of progesterone for the treatment of TBI included only three small-scale and low-quality studies23. In this current study, we selected 7 relevant RCTs including 2492 patients (progesterone: 1276 cases, placebo: 1216 cases) hospitalized for acute TBI to assess the efficacy of progesterone therapy on the Glasgow Outcome Scale (GOS) score and for adverse events.
Some previous clinical studies demonstrated that progesterone was a neuroprotective agent and improved outcomes for patients with acute severe TBI8,10. However, we found no significant difference between the progesterone-treated group and the placebo group in the rate of death or vegetative state. Moreover, our results showed that progesterone was not associated with good recovery at the end of the follow-up period. To date, various drugs have been investigated in clinical trials, yet none has been proven to reduce mortality significantly at the confirmatory stage24,25,26,27. The trauma of individual patients could not be controlled well in comparison with the animal model. The heterogeneity and variability of TBI may be one of the important reasons14,28. This classification scheme of patients may be relatively insensitive using the Glasgow Coma Scale (GCS) or the Glasgow Outcome Scale-Extended (GOSE)28,29.
Some limitations must be noted in this present study. First, one included study excluded female patients as a result of side effects on the menstrual cycle12. Second, due to the lack of available data, we did not analyze other clinical outcomes except mortality and good recovery. It was unknown whether progesterone promoted the recovery of motor and sensory skills. Finally, the follow-up was short-term and varied across the studies. Thus, an appropriate dosage and a long-term follow-up may be necessary to further investigate the efficacy of progesterone in the treatment of acute TBI.
In conclusion, the pooled data did not support the idea that progesterone was superior to placebo in the treatment of acute TBI. Progesterone may be not effective in lowering the incidence of death or vegetative state in patients with acute TBI.
Methods
Search strategy
Our electronic search was conducted in PubMed, Embase, and the Cochrane Library databases until May 10, 2015. The core terms included “progesterone” and “head injury,” “traumatic brain injury,” “TBI,” “random,” and “random*”. There was no language limitation. We also searched Google Scholar and checked the reference lists of the included studies to identify any additional eligible articles.
Inclusion criteria
Studies were included if they met the following criteria: (1) adults (older than 18 years) with a diagnosis of acute TBI, (2) progesterone compared with placebo (or no progesterone), and (3) randomized controlled trials. Duplicate articles, reviews, case reports, and studies without extractable data were excluded.
Data extraction and outcome measures
Two authors (CL and HQH) independently extracted the following data from each included study in the standard form: (1) study characteristics (author’s name, date of publication, study design, sample size), (2) characteristics of participants (age and gender), (3) interventions (administration, duration, and dosage), and (4) outcomes (GOS and adverse events). Any discrepancies were discussed and resolved by the research team when necessary. The efficacy outcome was assessed with death or vegetative state (GOS = 1 or 2) and good recovery (GOS = 5) at the 6 months after TBI or end of the follow-up period. Adverse events included pneumonia and sepsis.
Quality assessment
The eligible studies were evaluated according to the Cochrane Collaboration’s tool30. The domains were as follow: selection bias (random method and allocation concealment), performance and detection bias (blinding of participants, personnel and outcome assessment), attrition bias (incomplete outcome data), and reporting bias (selective reporting).
Statistical analysis
The data were analyzed with the Cochrane Review Manager 5.3 and STATA 11.0 software according to the preferred reporting items for systematic reviews and meta-analysis (PRISMA) statement31,32. Risk ratios (RR) were calculated and pooled with a 95% confidence interval (CI) for dichotomous variables. The heterogeneity was estimated using the I2 test, which was considered to be low heterogeneity when I2 ≤ 25%. A fixed-effects random effects model was used if the I2 was ≤25%. Otherwise, a random effects model was applied. We used the funnel plot and Eger’s test to assess potential publication bias33.
Additional Information
How to cite this article: Lin, C. et al. Efficacy of progesterone for moderate to severe traumatic brain injury: a meta-analysis of randomized clinical trials. Sci. Rep. 5, 13442; doi: 10.1038/srep13442 (2015).
Acknowledgments
This study was supported by grants from the National Natural Science Foundation of China (No. 81471269 (BA14)).
Footnotes
Author Contributions C.L. and H.-H.Q. designed the experiments. C.L. and Z.L. performed the experiments. C.-H.L. analyzed the data. C.L. and J.J. wrote the manuscript. Critical revision, final drafting and text approval were performed by L.-Y.L., C.L. and N.L.
References
- Ghajar J. Traumatic brain injury. Lancet 356, 923–929 (2000). [DOI] [PubMed] [Google Scholar]
- Maas A. I., Stocchetti N. & Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol 7, 728–741 (2008). [DOI] [PubMed] [Google Scholar]
- Coronado V. G. et al. Trends in Traumatic Brain Injury in the U.S. and the public health response: 1995-2009. J Safety Res 43, 299–307 (2012). [DOI] [PubMed] [Google Scholar]
- Langlois J. A., Rutland-Brown W. & Wald M. M. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil 21, 375–378 (2006). [DOI] [PubMed] [Google Scholar]
- Stein D. G., Wright D. W. & Kellermann A. L. Does progesterone have neuroprotective properties. Ann Emerg Med 51, 164–172 (2008). [DOI] [PubMed] [Google Scholar]
- Pascual J. L. et al. Neuroprotective effects of progesterone in traumatic brain injury: blunted in vivo neutrophil activation at the blood-brain barrier. Am J Surg 206, 840–845 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Si D. et al. Progesterone treatment improves cognitive outcome following experimental traumatic brain injury in rats. Neurosci Lett 553, 18–23 (2013). [DOI] [PubMed] [Google Scholar]
- Xiao G., Wei J., Yan W., Wang W. & Lu Z. Improved outcomes from the administration of progesterone for patients with acute severe traumatic brain injury: a randomized controlled trial. Crit Care 12, R61 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skolnick B. E. et al. A clinical trial of progesterone for severe traumatic brain injury. N Engl J Med 371, 2467–2476 (2014). [DOI] [PubMed] [Google Scholar]
- Xiao G. M. et al. [Clinical study on the therapeutic effects and mechanism of progesterone in the treatment for acute severe head injury]. Zhonghua Wai Ke Za Zhi 45, 106–108 (2007). [PubMed] [Google Scholar]
- Aminmansour B. et al. Comparison of the administration of progesterone versus progesterone and vitamin D in improvement of outcomes in patients with traumatic brain injury: A randomized clinical trial with placebo group. Adv Biomed Res 1, 58 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakeri M. et al. Effect of progesterone administration on prognosis of patients with diffuse axonal injury due to severe head trauma. Clin Neurol Neurosurg 115, 2019–2022 (2013). [DOI] [PubMed] [Google Scholar]
- Wright D. W. et al. ProTECT: a randomized clinical trial of progesterone for acute traumatic brain injury. Ann Emerg Med 49, 391–402 (2007). [DOI] [PubMed] [Google Scholar]
- Wright D. W. et al. Very early administration of progesterone for acute traumatic brain injury. N Engl J Med 371, 2457–2466 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maas A. I., Stocchetti N. & Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol 7, 728–741 (2008). [DOI] [PubMed] [Google Scholar]
- Mustafa A. G. & Alshboul O. A. Pathophysiology of traumatic brain injury. Neurosciences (Riyadh) 18, 222–234 (2013). [PubMed] [Google Scholar]
- Park E., Bell J. D. & Baker A. J. Traumatic brain injury: can the consequences be stopped? CMAJ 178, 1163–1170 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margulies S. & Hicks R. Combination therapies for traumatic brain injury: prospective considerations. J Neurotrauma 26, 925–939 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drew P. D. & Chavis J. A. Female sex steroids: effects upon microglial cell activation. J Neuroimmunol 111, 77–85 (2000). [DOI] [PubMed] [Google Scholar]
- He J., Hoffman S. W. & Stein D. G. Allopregnanolone, a progesterone metabolite, enhances behavioral recovery and decreases neuronal loss after traumatic brain injury. Restor Neurol Neurosci 22, 19–31 (2004). [PubMed] [Google Scholar]
- Cutler S. M. et al. Progesterone improves acute recovery after traumatic brain injury in the aged rat. J Neurotrauma 24, 1475–1486 (2007). [DOI] [PubMed] [Google Scholar]
- Li Z. et al. Progesterone increases circulating endothelial progenitor cells and induces neural regeneration after traumatic brain injury in aged rats. J Neurotrauma 29, 343–353 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma J., Huang S., Qin S. & You C. Progesterone for acute traumatic brain injury. Cochrane Database Syst Rev 10, CD008409 (2012). [DOI] [PubMed] [Google Scholar]
- Narayan R. K. et al. Clinical trials in head injury. J Neurotrauma 19, 503–557 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schouten J. W. Neuroprotection in traumatic brain injury: a complex struggle against the biology of nature. Curr Opin Crit Care 13, 134–142 (2007). [DOI] [PubMed] [Google Scholar]
- Loane D. J. & Faden A. I. Neuroprotection for traumatic brain injury: translational challenges and emerging therapeutic strategies. Trends Pharmacol Sci. 31, 596–604 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maas A. I., Roozenbeek B. & Manley G. T. Clinical trials in traumatic brain injury: past experience and current developments. Neurotherapeutics 7, 115–126 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manley G. T. & Maas A. I. Traumatic brain injury: an international knowledge-based approach. JAMA 310, 473–474 (2013). [DOI] [PubMed] [Google Scholar]
- Wilson J. T., Pettigrew L. E. & Teasdale G. M. Structured interviews for the Glasgow Outcome Scale and the extended Glasgow Outcome Scale: guidelines for their use. J Neurotrauma 15, 573–585 (1998). [DOI] [PubMed] [Google Scholar]
- Higgins J. P. et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343, d5928 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 151, W65–94 (2009). [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J. & Altman D. G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6, e1000097 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M., Davey S. G., Schneider M. & Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–634 (1997). [DOI] [PMC free article] [PubMed] [Google Scholar]