Abstract
Objective:
In obese patients, the management of renal calculi presents a number of challenges for urologists. In this study, we aimed to evaluate the efficacy and safety of percutaneous nephrolithotomy (PNL) procedure in obese and morbidly obese patients.
Material and methods:
We retrospectively reviewed the medical files of 2360 patients treated with PNL between March 2002 and April 2013. The patients were stratified into four groups according to the World Health Organization (WHO) classification of body mass index (BMI): <25 kg/m2 (average), 25–29.9 kg/m2 (overweight), 30–39.9 kg/m2 (obese), and >40 kg/m2 (morbidly obese). Patients under 18 years of age and those with a body mass index under 18 kg/m2 were excluded from the study. Intra-, and postoperative outcomes of PNL were compared between groups.
Results:
A total of 2102 patients with a mean age of 43±13.62 years were enrolled in the study. The mean stone size, mean number of stones, staghorn stone rate and history of previous shock wave lithotripsy were similar in all groups. The overall stone-free rate was 82 percent. The mean operation time was longer in the morbidly obese group but it was not significantly different from that in the other groups. No differences were observed in hospital stay, complication or stone-free rate among four study groups.
Conclusion:
Percutaneous nephrolithotomy is a safe and effective treatment for renal stone disease. Body mass index does not affect the success or complication rate in PNL.
Keywords: Body mass index, kidney stone, percutaneous nephrolithotomy
Introduction
Because of increased prevalance of sedentary life, decrease in physical activity, and consumption of diets rich in higher fat content, obesity has become an important health problem worldwide.[1] Obesity which affects nearly 1.5 billion people according to World Health Organization, is strongly correlated with ischemic heart disease, hypertension, and diabetes mellitus as revealed by robust evidence.[2] Still in obese patients, probability of renal stone formation is higher seen relative to non-obese patients.[3,4]
In obese patients, renal stone treatment in obese patients poses some difficulties. Studies performed, have shown that success rates of extracorporeal shock wave lithotripsy (ESWL) decreased with enhanced body mass index (BMI).[5,6] Achievement of stone-free rates in patients with excess stone burden requires more than one ESWL session which restricted use of flexible ureterorenoscopy in obese patients especially with serious concomitant diseases.[7] Nowadays, even though percutaneous nephrolithotomy (PNL) is the most prevalent method used in the management of renal diseases in this patient group, only limited number of studies have examined PNL procedures in obese, and morbidly obese patients.
Herein, we aimed to present the impact of higher BMIs of the patients on the efficacy and safety of PNL procedures that were performed in our clinic.
Material and methods
In our clinic, data of 2360 PNL operations performed in our clinic between March 2002, and April 2013 were retrieved from our database, and retrospectively analyzed. BMI data found in medical records of the patients were divided into 4 groups based on the BMI classification of World Health Organization as follows: <25 kg/ m2 (Group 1, normal body weights), 25–29.9 kg/m2 (Group 2, overweight), 30–39.9 kg/m2 (Group 3, obese), and >40 kg/m2 (Group 4, morbidly obese).[8] Patients without BMI data, those with estimated BMIs <18 kg/m2, and patients younger than 18 years of age were excluded from the study.
Preoperatively, all patients were informed about treatment alternatives, and they undersigned informed consent forms. Preoperatively, whole blood count, creatinine, and serum electrolyte values, liver function test (ALT, and AST) results were evaluated. Besides, bleeding, and coagulation profiles (bleeding time, coagulation time, INR, PT, and aPTT), serologic tests (HbsAg, Anti-HCV, and Anti-HIV) results were analyzed. One week before the procedure, blood cultures obtained, and in cases of need, following appropriate antibiotherapy, PNL was performed. Preoperatively the patients were also assessed as for stone size, and potential urinary system pathologies using non-contrasted computed tomograpy (CT) and/or intravenous pyelography (IVP). Stone surface area was measured by multiplying the longest diameter of the stone by its intersecting vertical diameter as explained in EAU (European Association of Urology) guidelines.[9]
PNL Technique
After administration of general or epidural anesthesia with the patient in the lithotomy position a 5 F ureteral catheter was placed in the renal pelvis. Then the patient was laid in the prone position, and contrast agent was delivered through ureteral catheter, and pelvicalyceal system was visualized. Then with a 20 cm-long percutaneous access needle (18G Percutaneous Access Needle, Boston Scientific Corporation, Natick MA, USA) access into the suitable calyx was performed. For dilatation, high-pressure balloon dilator (NephroMaxTM Microvasive High Pressure Balloon Catheter, Boston Scientific, Boston, MA, USA) or Amplatz dilator set (Amplatz Renal Dilator Set, Cook Medical, IN, USA) was used. For all patients the same type of percutaneous access needle, and dilator set were used. Following entrance into pelvicalyceal system with a 26 F rigid nephroscope, the stones were fragmented with the aid of an ultrasonic lithotriptor (Swiss Lithoclast®, EMS, Nyon, Switzerland). Stone fragments were taken out using a stone forceps or basket (Perc-N Circle, Cook Medikal, IN, USA). A 14 F nephrostomy tube (Malecot Nephrostomy Catheter, Cook Medical) was placed in renal pelvis or suitable calyx for drainage. On the first postoperative day from all patients KUBs were obtained, and evaluated as for their stone-free states.
Preoperatively parameters including age, gender. BMI, concomitant diseases, stone size, and history of SWL were analyzed. Groups were also evaluated as for operative, and fluoroscopy times, intra-, and postoperative complications were also evaluated. Still in all groups, hospital stay, stone-free rate, pre-, and postoperative hemoglobin values were analyzed.
Statistical analysis
In this study, statistical analysis of the relevant data was performed using Statistical Package for the Social Sciences (SPSS) v. 13 package program. For the comparison of parameters among four groups ANOVA test, and in cases of need X2 test were employed. P<0.05 was accepted as the level of significance.
Results
Patients’demographic characteristics, and stone properties are summarized in Table 1. Mean age of a total of 2102 patients in all groups was 43±13.62 years (Group 1: 38.19±14.8, Group 2: 46.39±12.9, Group 3: 49.52±12.8, and Group 4: 50.22±11.1 yrs). Distribution of gender, and ASA (American Society of Anesthesiologists) scores was comparable in all groups, while mean age of the patients was relatively higher in the morbidly obese group. Mean stone size did not show differences between groups (Group 1: 7.6±5.70 mm2, Group 2: 7.84±5.56 mm2, Grup 3: 8.17±6.00 mm2, and Group 4: 8.15±5.92 mm2). Mean number of stones was not significantly different between groups (p:0.059). Obese, and morbidly obese patients had undergone least number of SWL procedures when compared with other groups, without any statistically significant difference between groups (p:0.840).
Table 1.
Preoperative characteristics of the patients, and renal stones
| Group 1 (n: 849) | Group 2 (n: 883) | Group 3 (n: 334) | Group 4 (n: 36) | p -value | |
|---|---|---|---|---|---|
| Mean age (years) | 38.19±14.8 | 46.39±12.9 | 49.52±12.8 | 50.22±11.1 | 0.001 |
| Gender | |||||
| Male | 490 | 510 | 217 | 20 | |
| Female | 359 | 373 | 117 | 16 | 0.102 |
| ASA score | |||||
| I | 378 | 412 | 141 | 16 | |
| II | 256 | 266 | 110 | 10 | 0.896 |
| III | 173 | 157 | 63 | 8 | |
| IV | 42 | 48 | 20 | 2 | |
| Number of stones | |||||
| Single | 375 | 392 | 121 | 15 | 0.059 |
| Multiple | 474 | 491 | 213 | 21 | |
| Stone size (mm2) | 7.6±5.70 | 7.84±5.56 | 8.17±6.00 | 8.15±5.92 | 0.124 |
| Staghorn stone frequency (%) (partial or complete) | 53 | 48 | 52 | 57 | 0.920 |
| Previous SWL | 25.3% | 26.7% | 25.0% | 22.2% | 0.840 |
ASA score: American Society of Anesthesiologists; SWL: shock wave lithotripsy
Mean fluoroscopy time, and number of intrarenal entries were comparable in all groups. Operative times increased in parallel with enhanced BMIs of the patients (Figure 1). Operative times were longer in morbidly obese patients (68.20±24.66 mins) when compared with other groups (Group 1: 64.44±26.93 mins, Group 2: 65.74±28.69 mins, and Group 3: 66.13±28.42 mins) without statistically significant difference between groups (p:0.638).
Figure 1.
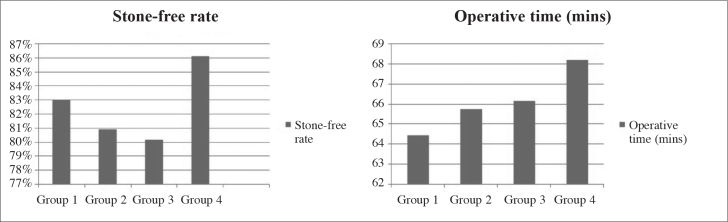
Parameters related to body mass index, stone-free rate, and operative time
Postoperative parameters of the patients used in their monitorization are given in Table 2. The highest stone-free state was achieved in the morbidly obese group. Hospital stay, nephrostomy time, and need for transfusion demonstrated similar characteristics in all groups. Complication rates were 6.00, 6.34, 8.38, and 8.33% in Groups 1, 2, 3, and 4 respectively, without any significant intergroup difference. In a total of 2 patients (one patient with normal BMI, and one overweight patient) with colonic perforation was detected who were treated with colostomic operations. Nephrectomy was performed on a total of 4 patients. In 2 patients intractable intraoperative bleeding necessitated nephrectomy. The remaining 2 patients underwent nephrectomy because of sudden drop in hemoglobin level during the immediate postoperative period (Figure 2).
Table 2.
Intra-, and postoperative values of 4 PNL groups categorized according to body mass indexes of the patients
| Group 1 | Group 2 | Group 3 | Group 4 | p -value | |
|---|---|---|---|---|---|
| Operative time (min) | 64.44±26.93 | 65.74±28.69 | 66.13±28.42 | 68.20±24.66 | 0.638 |
| Fluoroscopy time (min) | 8.55±5.12 | 8.45±4.78 | 8.39±5.41 | 9.04±3.66 | 0.416 |
| Number of accesses | |||||
| Single | 660 | 729 | 311 | 29 | |
| Multiple | 184 | 147 | 56 | 7 | 0.313 |
| Nephrostomy dwell time (days) | 2.78±1.58 | 2.70±1.59 | 2.73±2.09 | 2.69±0.86 | 0.803 |
| Transfusion requirement (%) | 11.8% | 13.02% | 12.12% | 7.14% | 0.772 |
| Complications | |||||
| *Sepsis | 6 | 6 | 3 | 0 | 0.933 |
| *PCS Perf. | 29 | 33 | 18 | 2 | 0.418 |
| *Pulmonary complications | 12 | 12 | 4 | 1 | 0.894 |
| *Cardiac complications | 2 | 2 | 2 | 0 | 0.697 |
| *Colonic perforation | 1 | 1 | 0 | 0 | 0.934 |
| *Nephrectomy | 1 | 2 | 1 | 0 | 0.902 |
| Hospital stay (days) | 2.86±1.56 | 2.90±1.93 | 2.70±1.58 | 2.81±0.98 | 0.337 |
| Stone-free rate | 710 (83%) | 714 (80.9%) | 268 (80.2) | 31 (86.1%) | 0.333 |
PCS perf: pelvicalyceal system perforation
Figure 2.
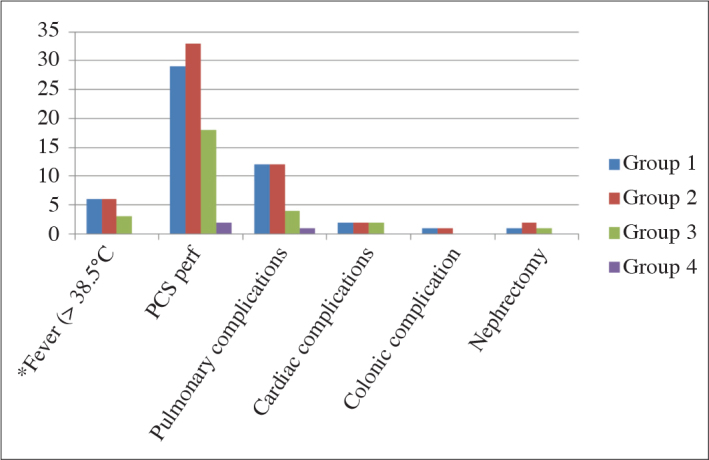
Groups categorized based on body mass indexes, and complication rates
Discussion
According to the definition of World Health Organization, obesity is accumulation of excess fat in the body which is harmful for health. In the last 20 years increasingly prevalent obesity, and morbid obesity are important etiological factors responsible for metabolic syndrome, cardiovascular diseases, malignancies, and renal stones.[10,11] In a survey study conducted by Binbay et al.[12] incidence of stone disease was indicated as 11.1%, and increased risk of urolithiasis was detected in the presence of metabolic syndrome components. Obese patients lead a sedentary life when compared with non-obese patients. Besides, higher prevalence of gout disease in obese patients, higher purine, carbonhydrate, and animal fat content in their diet contribute to stone formation. Impairment of ammonium metabolism as an outcome of insulin resistance, and dysfunctional transport in renal tubular cells facilitate formation of renal stones.[13]
Cardiovascular and/or respiratory disorders suffered by obese patients underline the importance of carrying out management of renal stones successfully if possible without anesthesia, and in a single session. SWL is the first-line treatment modality preferred for renal stones smaller than 2 cm.[14] Though application of SWL without requiring anesthesia seems to be an advantage at first glance, longer distance between the stone and the skin leads to a decrease in the effectiveness of SWL. Difficulty in fluoroscopic, and ultrasonographic focusing on the stone, and weight bearing capacity of the SWL are another factors restricting use of this method.[15] Some studies have demonstrated that in the treatment of renal stones in obese patients flexible ureterenoscopy (f-URS) can be a good alternative. However, in patients with greater stone burden its inapplicability, and longer operative times prevent widespread use of f-URS.[16]
Nowadays, PNL has been most frequently resorted treatment modality in obese, and morbidly obese patients with renal stones, however urologists are confronted with many problems during the procedure.[17] Positioning of the patient requires the help of several health care personnel. Besides, as an important measure, pressure points of the body should be supported with pads to refrain from development of pressure sores.[18] Especially during PNL procedures which are performed while the patient is in the prone position, lungs are exposed to compressive forces which lead to respiratory problems in patients with restricted lung capacity with potential retention of carbon dioxide. Compression on vena cava inferior decreases venous return which might trigger cardiac problems. Opinions favouring application of PNL in the supine position may decrease cardiac, and respiratory problems but this suggestion has not been fully elucidated.[19] Gofrit et al.[20] indicated that lateral decubitus position could overcome adverse effects of obesity on respiratory, and cardiac functions.
Increased BMI complicates PNL procedures with respect to both anesthesic risks, and technical maneuvers. Because of supranormal thickness of subcutaneous adipose tissue, length of nephroscope or Amplatz sheath may not permit access into renal collecting system or contact with the stone. Curtis et al.[21] incised, and retracted skin, and subcutaneous adipose tissue to gain extra distance. According to another recommended alternative technique, a nephrostomy tube is inserted into the kidney with a stone, and PNL is performed a week later when an access tract is formed between the skin and the kidney.[22] However Giblin et al.[23] passed a 27 cm-long gynecological laparoscope through a 32 F Amplatz sheath to fragment renal stones. In our clinical practice, if required, we are fixating Amplatz sheath with silk sutures to the skin or we are applying the method described by Curtis et al.[21] Despite unfavourable effects of obesity on PNL, many current studies have revealed success, and safety of PNL in this patient group. Carson et al.[24] compared 44 obese patients with 226 non-obese ones, and couldn’t detect any significant difference between groups as for operative times, stone-free, and complication rates. However Pearle et al.[25] considered cases with a BMI >30 kg/m2 as obese patients, and performed PNL operations on a total of 236 patients (57 obese, and 279 non-obese patients) with a mean stone size of 14.5±8.7 mm2. They detected comparatively longer PNL operative times in obese patients with comparable success, and complication rates between both groups. El-Assmy et al.[8] detected mean stone size of 2.5±0.85 cm2 in their patients. Still Alyami et al.[27] operated on patients with stones smaller than 3 cm in diameter. Both investigators couldn’t detect any correlation between body mass index, and stone-free rates. In our study, mean stone size was calculated as 7.81±5.70 cm. However Fearber et al.[26] evaluated 93 morbidly obese patients among a total of 530 patients, and detected higher complication rates in morbidly obese patients relative to those with normal BMIs (37 vs 16%). Still in our study, when groups categorized as for BMIs of the patients were compared, comparable success, and complication rates were found between groups. In our series, a total of 4 patients underwent nephrectomies because of intractable bleeding, and 2 patients experienced colonic ruptuıre who were treated with colostomy operations. Pelvicalyceal system injury was the most frequently encountered intraoperative complication, and all of these patients were managed by nephrostomy tube or D-J stent placement. Though statistically insignificant, we attribute higher operative success rates in the morbidly obese patients to extra efforts of the surgeons to obtain stone-free status so as to eliminate the need for a SWL or a second surgical intervention.
In the present study, although patients who underwent PNL procedures in our clinic were classified according to their BMIs, and the impact of obesity on the success, and complication rates of PNL in different patient categories was analyzed, our study had some limitations. Firstly, data of 2360 patients were screened, while only a total of 2012 patients could be included in the study. Secondly, operations were not performed by the same surgeon. So diverse surgical experiences might effect the outcomes obtained. However if we consider that our clinic is providing training for urology residents, this approach should be accepted as a natural process. Besides, only patients’ BMIs were taken into account as an influentual factor on operative times, a multivariate analysis on location, and size of the stones was not performed.
As a concluding remark of our study we can say that PNL is an effective, safe, and reliable method with higher success and acceptable complication rates in the management of stone disease in overweight, obese, and morbidly obese patients.
Footnotes
Ethics Committee Approval: Due to its retrospective nature, ethics committee approval was not required.
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - A.Ş., F.Ö.; Design - O.K., Y.B.; Supervision - A.Y.M., Y.B.; Funding - Ö.S.; Materials - Ö.S.; Data Collection and/or Processing - M.B.; Analysis and/or Interpretation - A.Ş., F.Ö., O.K., M.B., M.F.A.; Literature Review - A.Ş., F.Ö.; Writer - A.Ş., F.Ö., M.F.A.; Critical Review - Ö.S., Y.B., A.Y.M., Other - A.Ş., F.Ö.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–7. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 2.Raebel MA, Malone DC, Conner DA, Xu S, Porter JA, Lanty FA. Health services use and health care costs of obese and nonobese individuals. Arch Intern Med. 2004;164:2135–40. doi: 10.1001/archinte.164.19.2135. [DOI] [PubMed] [Google Scholar]
- 3.Taylor EN, Stampfer MJ, Curhan GC. Dietary factors and the risk of incident kidney stones in men: new insights after 14 years of follow-up. J Am Soc Nephrol. 2004;15:3225–32. doi: 10.1097/01.ASN.0000146012.44570.20. [DOI] [PubMed] [Google Scholar]
- 4.Taylor EN, Stampfer MJ, Curhan GC. Diabetes mellitus and the risk of nephrolithiasis. Kidney Int. 2005;68:1230–5. doi: 10.1111/j.1523-1755.2005.00516.x. [DOI] [PubMed] [Google Scholar]
- 5.Thomas R, Cass AS. Extracorporeal shock wave lithotripsy in morbidly obese patients. J Urol. 1993;150:30–2. doi: 10.1016/s0022-5347(17)35389-2. [DOI] [PubMed] [Google Scholar]
- 6.Al-Hayek S, Schwen ZR, Jackman SV, Averch TD. The impact of obesity on urine composition and nephrolithiasis management. J Endourol. 2013;27:379–83. doi: 10.1089/end.2012.0275. [DOI] [PubMed] [Google Scholar]
- 7.Andreoni C, Afane J, Olweny E, Clayman RV. Flexible ureteroscopic lithotripsy: first line therapy for proximal ureteral and renal calculi in the morbidly obese and superobese patient. J Endourol. 2001;15:493–8. doi: 10.1089/089277901750299285. [DOI] [PubMed] [Google Scholar]
- 8.El-Assmy AM, Shokeir AA, El-Nahas AR, Shoma AM, Eraky I, El-Kenawy MR, et al. Outcome of percutaneous nephrolithotomy: effect of body mass index. Eur Urol. 2007;52:199–204. doi: 10.1016/j.eururo.2006.11.049. [DOI] [PubMed] [Google Scholar]
- 9.Akman T, Binbay M, Ugurlu M, Kaba M, Akcay M, Yazıcı O, et al. Outcomes of retrograde intrarenal surgery compared with percutaneous nephrolithotomy in elderly patients with moderate-size kidney stones: a matched-pair analysis. J Endourol. 2012;26:625–9. doi: 10.1089/end.2011.0526. [DOI] [PubMed] [Google Scholar]
- 10.Kurzer E, Leveillee R, Bird V. Obesity as a risk factor for complications during laparoscopic surgery for renal cancer: multivariate analysis. J Endourol. 2006;20:794–9. doi: 10.1089/end.2006.20.794. [DOI] [PubMed] [Google Scholar]
- 11.Neligan PJ. Metabolic syndrome: anesthesia for morbid obesity. Curr Opin Anaesthesiol. 2010;23:375–83. doi: 10.1097/aco.0b013e328338caa0. [DOI] [PubMed] [Google Scholar]
- 12.Binbay M, Yuruk E, Akman T, Sari E, Yazici O, Ugurlu IM, et al. Updated epidemiologic study of urolithiasis in Turkey II: role of metabolic syndrome components on urolithiasis. Urol Res. 2012;40:247–52. doi: 10.1007/s00240-011-0447-x. [DOI] [PubMed] [Google Scholar]
- 13.Asplin JR. Obesity and urolithiasis. Adv Chronic Kidney Dis. 2009;16:11–20. doi: 10.1053/j.ackd.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 14.Bhojani N, Lingeman JE. Shockwave lithotripsy-new concepts and optimizing treatment parameters. Urol Clin North Am. 2013;40:59–66. doi: 10.1016/j.ucl.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 15.El-Nahas AR, El-Assmy AM, Mansour O, Sheir KZ. A prospective multivariate analysis of factors predicting stone disintegration by extracorporeal shock wave lithotripsy: the value of high-resolution noncontrast computed tomography. Eur Urol. 2007;51:1688–93. doi: 10.1016/j.eururo.2006.11.048. [DOI] [PubMed] [Google Scholar]
- 16.Vujovic A, Keoghane S. Management of renal stone disease in obese patients. Nat Clin Pract Urol. 2007;4:671–6. doi: 10.1038/ncpuro0988. [DOI] [PubMed] [Google Scholar]
- 17.Koo BC, Burtt G, Burgess NA. Percutaneous stone surgery in the obese: outcome stratified according to body mass index. BJU Int. 2004;93:1296–9. doi: 10.1111/j.1464-410X.2004.04862.x. [DOI] [PubMed] [Google Scholar]
- 18.Sergeyev I, Koi PT, Jacobs SL, Godelman A, Hoenig DM. Outcome of percutaneous surgery stratified according to body mass index and kidney stone size. Surg Laparosc Endosc Percutan Tech. 2007;17:179–83. doi: 10.1097/SLE.0b013e318051543d. [DOI] [PubMed] [Google Scholar]
- 19.Valdivia Uria JG, Valle Gerhold J, Lopez Lopez JA, Villarroya Rodriquez S, Ambroj Navarro C, Ramirez Fabian M, et al. Technique and complications of percutaneous nephroscopy: experience with 557 patients in the supine position. J Urol. 1999;160:1975–8. doi: 10.1016/s0022-5347(01)62217-1. [DOI] [PubMed] [Google Scholar]
- 20.Gofrit ON, Shapiro A, Donchin Y, Bloom AL, Shenfeld OZ, Landau EH, et al. Lateral decubitus position for percutaneous nephrolithotripsy in the morbidly obese or kyphotic patient. J Endourol. 2002;16:383–6. doi: 10.1089/089277902760261437. [DOI] [PubMed] [Google Scholar]
- 21.Curtis R, Thorpe AC, Marsh R. Modification of the technique of percutaneous nephrolithotomy in the morbidly obese patient. Br J Urol. 1997;79:138–40. doi: 10.1046/j.1464-410x.1997.129135.x. [DOI] [PubMed] [Google Scholar]
- 22.Segura JW. Role of percutaneous procedures in the management of renal calculi. Urol Clin North Am. 1990;17:207–16. [PubMed] [Google Scholar]
- 23.Giblin JG, Lossef S, Pahira JJ. A modification of Standard percutaneous nephrolithotripsy technique for the morbidly obese patient. Urology. 1995;46:491–3. doi: 10.1016/S0090-4295(99)80260-X. [DOI] [PubMed] [Google Scholar]
- 24.Carson CC, Danneberger JE, Weinerth JL. Percutaneous lithotripsy in morbid obesity. J Urol. 1988;139:243–5. doi: 10.1016/s0022-5347(17)42375-5. [DOI] [PubMed] [Google Scholar]
- 25.Pearle MS, Nakada SY, Womack JS, Kryger JV. Outcomes of contemporary percutaneous nephrostolithotomy in morbidly obese patients. J Urol. 1998;160:669–73. doi: 10.1016/S0022-5347(01)62750-2. [DOI] [PubMed] [Google Scholar]
- 26.Faerber GJ, Goh M. Percutaneous nephrolithotripsy in the morbidly obese patient. Tech Urol. 1997;3:89–95. [PubMed] [Google Scholar]
- 27.Alyami FA, Skinner TA, Norman RW. Impact of body mass index on clinical outcomes associated with percutaneous nephrolithotomy. Can Urol Assoc J. 2012;15:1–5. doi: 10.5489/cuaj.11229. [DOI] [PMC free article] [PubMed] [Google Scholar]


