Abstract
Background and Aims:
Analysis to correlate the measurements of optic nerve sheath diameter (ONSD) obtained by using ultrasound to magnetic resonance imaging (MRI) techniques in order to establish the accuracy of ocular sonography as a noninvasive modality for detecting raised intracranial pressure (ICP).
Materials and Methods:
A prospective, observational study was performed in 100 cases of adult meningoencephalitis patients admitted to Intensive Care Unit in whom MRI was performed for neurodiagnosis. ONSD was measured in such patients, 3 mm behind the globe in each eye. A mean binocular ONSD >4.6 mm in female and 4.8 mm in male was taken as cut-off values for diagnosing raised ICP. This was compared with ONSD measured on T2-weighted MRI image measured 3 mm behind the globe. The reading obtained from both the methods were compared with Bland–Altman analysis for correlation and the findings were tabulated.
Results:
The mean ONSD values measured with ultrasonography (USG) and MRI for female were 5.48 ± 0.43 mm and 5.68 ± 0.44 mm and for male were 5.40 ± 0.37 mm and 5.56 ± 0.38 mm, respectively. The mean age of the female and male was 53.90 ± 17.84 and 56.06 ± 15.67 years, respectively. On comparing ultrasound with MRI-derived ONSD values, we found acceptable agreement between both methods for measurements at a depth of 3 mm (r = 0.02, P < 0.001).
Conclusion:
In our study, we have found a good correlation between ocular USG and MRI of ONSD. The study has shown agreement with the fact that ocular sonography can be used as a noninvasive tool for detecting raised ICP with accuracy.
Keywords: Intensive Care Unit, magnetic resonance imaging, ocular sonography, optic nerve sheath diameter, raised intracranial pressure
Introduction
In recent years, monitoring of intracranial pressure (ICP) by noninvasive methods are being practiced with the use of bedside ocular sonography. In severe head injury, intracranial bleeding and idiopathic intracranial hypertension, several studies showed close association between optic nerve sheath diameter (ONSD) and raised ICP.[1,2,3] Raised ICP can be detected with an increase in ONSD due to the presence of continuity of meninges and subarachnoid space around the optic nerve.[4,5]
It is very important to detect and treat raised ICP in such crucial situations.[6,7] Intraventricular catheters have been considered as gold standard in measuring ICPs. Their usage is limited by cost and is associated with complications like infection and bleeding. Assessment of ICP and its monitoring with radiological imaging modalities requires transportation, which increases the risk and endangers the lives of critically ill patients.[8]
Ultrasound is a cost effective treatment modality which does not require transportation of the patient. It is helpful bedside noninvasive method in measuring ONSD. It can be repeated at regular intervals which help in close monitoring of ICP as well.
In the study, we tried to assess the numerical accuracy of the ocular sonography measurements by comparing with the readings obtained with magnetic resonance imaging (MRI) images.
Materials and Methods
After obtaining Institutional Review Board's permission, we conducted a prospective observational study of 100 adult patients between May 2013 and December 2014. We enrolled 50 male and female patients each admitted to Intensive Care Unit (ICU) who were diagnosed with meningoencephalitis. They underwent MRI of the brain as a part of their treatment strategy. Ocular sonography was performed on the same day as MRI. All these patients were examined in the supine position using a 10 MHz phased linear array probe on the closed eyelids. The structures of the eye were visualized to align the optic nerve directly opposite the probe, with the ONSD width perpendicular to the vertical axis of the scanning plane. A single ONSD was measured 3.00 mm behind the globe [Figure 1] in both the eyes. The ONSD measurements were obtained averaging three readings from each eye to create a binocular ONSD measurement by calculating their average.[5,9] The measurements above 4.6 mm and 4.8 mm in females and males were considered to have increased ICP.[10,11,12]
Figure 1.
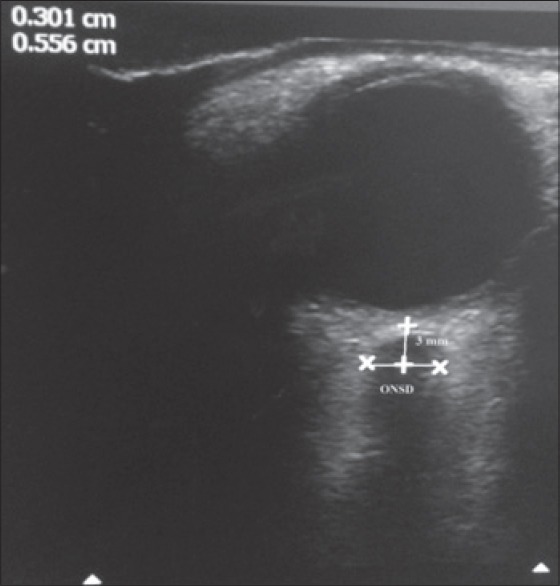
Measurement of optic nerve sheath diameter by ocular ultrasonography
All MRI examinations were performed using 1.5T MRI system (GE Healthcare, Milwaukee, WI, USA) equipped with a maximum field gradient strength of 22 mT/m and using a quadrature head coil. The MRI sequences used in this study are described below: Fluid-attenuated inversion recovery (FLAIR) (TE = 84 ms, TR = 8000 ms, inversion time 2000 ms, and bandwidth = 20.83 Hz). FLAIR were acquired in the axial plane with a field of view (FOV) 240 mm × 240 mm, matrix size 256 × 224 and 5 mm slice thickness with slice gap of 1.5 cm. Axial T2-weighted MRI using a single-shot spin echo echo-planar-imaging sequence. The sequence covered the whole brain with 20 contiguous slices that were acquired as two interleaved series of four repeats; that is, 5.0 mm thick slices with 1.5 mm gaps. Other parameters were set as TR = 8000 ms, TE = 88 ms, acquisition matrix 96 × 96, FOV = 24 cm, and resulted in in-plane resolution of 2.5 mm.
The ONSD was measured just behind the optic globe. The retrobulbar area was zoomed to 300×, and then ONSD was measured in an axis perpendicular to the optic nerve, 3 mm behind the globe using an electronic caliper [Figure 2]. The finding of MRI was reported by the on-site radiologist, and they were correlated with bedside ONSD measurement by ocular sonography.
Figure 2.
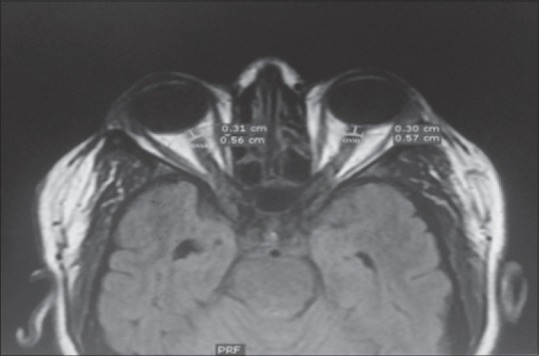
Measurement of optic nerve sheath diameter on T2-weighted magnetic resonance imaging
Patients with a history of optic neuritis, arachnoid cyst of the optic nerve, high myopia, optic nerve trauma, and anterior orbital or cavernous sinus mass are excluded from the study. The variables used were age, sex, ONSD ultrasound, and ONSD-MRI.
Statistical analysis
Statistical analyses were performed using the standard statistical software. Categorical variables were summarized through the calculation of frequency and relative frequency. Continuous variables were summarized through the calculation of mean and standard error. The statistical method employed for the study was Bland-Altman analysis and the mean difference (d) and standard deviation (SD) of the difference were calculated. From these data, the limits of agreement were calculated (SD, 95% confidence intervals [CIs]). Furthermore, correlation analyses was performed with Pearson's correlation coefficient (r) to quantify the strength of agreement.
Results
We conducted a prospective observational study on 100 patients with 50 male and 50 female subjects. The mean age of the female and male was 53.90 ± 17.84 and 56.06 ± 15.67 years, respectively [Table 1]. The mean ONSD of USG and MRI for a female was 5.48 ± 0.43 mm and 5.68 ± 0.44 mm while for males it was 5.40 ± 0.37 mm and 5.56 ± 0.38 mm, respectively [Table 2]. Both ONSD-USG and ONSD-MRI were compared. In females 95% CI was 0.825–0.993, T = −9.06, P < 0.001 where as in male 95% CI was 0.959–0.99, T= −16.914, P < 0.001 as shown in [Table 2]. Bland-Altman analysis was done to show agreement between both methods of measurement of ONSD, the analysis showed a correlation between ocular sonography and MRI [Figure 3]. The mean difference was −0.1912, the regression coefficient of 0.02, and P < 0.001 [Table 3].
Table 1.
Demographic data
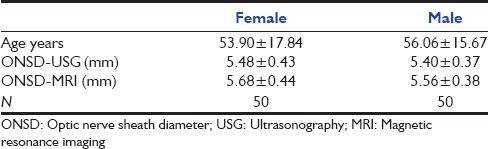
Table 2.
Comparison of ONSD between USG and MRI in gender
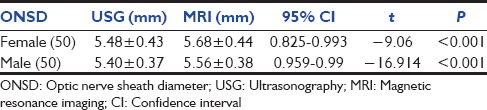
Figure 3.
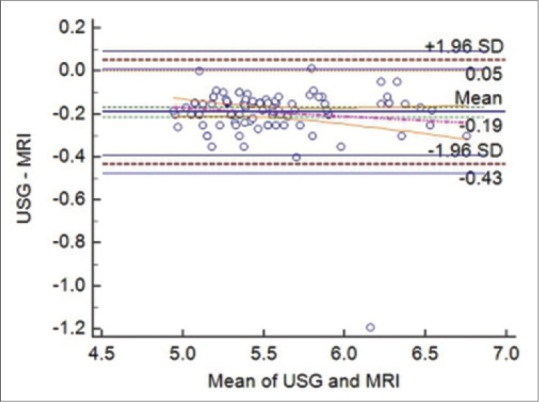
Correlation of optic nerve sheath diameter by transorbital sonography and magnetic resonance imaging using Bland– Altman analysis
Table 3.
Comparison of ONSD by transorbital sonography and MRI

Discussion
Monitoring of ICP is of paramount importance in neuro ICU. Increased ICP causes brain insult that may be associated with increased mortality and poor neurological outcomes.[6,7,13]
Dural covering continues as optic nerve sheath that increases in size, when there is raise in ICP. Edema of the optic disc was earlier considered a sign of raised ICP, but was not shown to be a sensitive marker as it took many days to develop.[14] It was shown that ONSD increases within seconds of raise in ICP which can be detected early with ocular sonography.[5,9] Studies done earlier suggested a good correlation between invasive ICP monitoring and ocular sonography in measuring intracranial hypertension.[15,16] This created much interest among medical fraternity for the use of ultrasound as a means of detecting intracranial hypertension. Ocular sonography for measuring ONSD has been studied in cases of hydrocephalus, hepatic failure, and traumatic brain injury (TBI).[9,17] The ONSD, measured behind the retina at fixed distance has been studied in TBI and intracranial hemorrhage to detect and quantify intracranial hypertension.[2,18] In our previous study, we performed the efficacy of ONSD measurement by USG to predict intracranial hypertension.[19] Using cut-off values of 4.6 mm for females, and 4.8 mm for males, they found a high level of sensitivity and specificity for the diagnosis of intracranial hypertension evident on computed tomography (CT) or MRI.
It was reported earlier that high-resolution MRI had been accurate at measuring ONSD[20,21] as well as detecting raised ICP in cases of idiopathic hydrocephalus and to diagnose a malfunction of shunts.[22,23,24,25]
Steinborn et al. showed good correlation between USG and MRI in measuring ONSD in children with raised ICPs.[26] Studies performed between both modalities to measure ONSD were done in subjects with normal ICP. The reason of selection of MRI of the optic nerve sheath as a reference is due to its high spatial resolution and the clear delineation of orbital structures. We studied the correlation of both modalities in measuring ONSD in meningoencephalitis patients, which were not studied earlier.
Both ONSD-USG and ONSD-MRI were compared at 3 mm depth behind papilla. In female 95% CI was 0.825–0.993, T = −9.06, P < 0.001, whereas in male 95% CI was 0.959–0.99, T = −16.914, P < 0.001. We found a good correlation between ONSD measurements of ocular sonography and MRI. Bland-Altman analysis plot was drawn which also suggested close correlation (r = 0.02; P < 0.001).
Steinborn et al. and few cadaver studies also showed a good correlation between ultrasound and MRI of the ONSD 3 mm behind the papilla in healthy individuals.[27]
A positive correlation was seen between the ONSD and invasive ICP (r = 0.68) in a study performed in TBI patients.[28] Few more noninvasive studies were carried out to correlate ICP with ONSD (transcranial Doppler and Marshall's classification for head CT scan), they also showed similar results. Using a ROC curve the optimum ONSD cut-off value for detection of raised ICP was found to be (5.7 mm). Limitation of our study is the lesser number of subjects we enrolled. A larger number of subjects would be required to be studied to authenticate our conclusions.
Conclusion
ONSD has been established to reflect the raise in ICP. Studies published regarding the accuracy of ultrasound in measuring ONSD have been few. In our trial, we showed that the accuracy of ONSD measured by ocular sonography was similar to ONSD measured by MRI. It further proves the fact that ultrasound as a point of care investigation is reliable and helpful in close monitoring of ICP in neurointensive care requiring patients.
Acknowledgement
We gratefully acknowledge the Department of Neurology, Department of radiology, respiratory technicians and nurses, and management of the hospital for their valuable support. We are thankful to the statistician for a valuable support in analyzing the data. We are also grateful to all the patients and volunteers who were part of this study. It is their contribution that has made this study possible .
Footnotes
Financial support and sponsorship Nil.
Conflict of Interest: There are no conflicts of interest.
References
- 1.Bäuerle J, Nedelmann M. Sonographic assessment of the optic nerve sheath in idiopathic intracranial hypertension. J Neurol. 2011;258:2014–9. doi: 10.1007/s00415-011-6059-0. [DOI] [PubMed] [Google Scholar]
- 2.Geeraerts T, Merceron S, Benhamou D, Vigué B, Duranteau J. Non-invasive assessment of intracranial pressure using ocular sonography in neurocritical care patients. Intensive Care Med. 2008;34:2062–7. doi: 10.1007/s00134-008-1149-x. [DOI] [PubMed] [Google Scholar]
- 3.Geeraerts T, Newcombe VF, Coles JP, Abate MG, Perkes IE, Hutchinson PJ, et al. Use of T2-weighted magnetic resonance imaging of the optic nerve sheath to detect raised intracranial pressure. Crit Care. 2008;12:R114. doi: 10.1186/cc7006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Killer HE, Jaggi GP, Flammer J, Miller NR, Huber AR, Mironov A. Cerebrospinal fluid dynamics between the intracranial and the subarachnoid space of the optic nerve. Is it always bidirectional? Brain. 2007;130(Pt 2):514–20. doi: 10.1093/brain/awl324. [DOI] [PubMed] [Google Scholar]
- 5.Hansen HC, Helmke K. Validation of the optic nerve sheath response to changing cerebrospinal fluid pressure: Ultrasound findings during intrathecal infusion tests. J Neurosurg. 1997;87:34–40. doi: 10.3171/jns.1997.87.1.0034. [DOI] [PubMed] [Google Scholar]
- 6.Newton CR, Crawley J, Sowumni A, Waruiru C, Mwangi I, English M, et al. Intracranial hypertension in Africans with cerebral malaria. Arch Dis Child. 1997;76:219–26. doi: 10.1136/adc.76.3.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Calvo A, Hernández P, Spagnuolo E, Johnston E. Surgical treatment of intracranial hypertension in encephalic cryptococcosis. Br J Neurosurg. 2003;17:450–5. doi: 10.1080/02688690310001611242. [DOI] [PubMed] [Google Scholar]
- 8.Beckmann U, Gillies DM, Berenholtz SM, Wu AW, Pronovost P. Incidents relating to the intra-hospital transfer of critically ill patients. An analysis of the reports submitted to the Australian Incident Monitoring Study in Intensive Care. Intensive Care Med. 2004;30:1579–85. doi: 10.1007/s00134-004-2177-9. [DOI] [PubMed] [Google Scholar]
- 9.Helmke K, Hansen HC. Fundamentals of transorbital sonographic evaluation of optic nerve sheath expansion under intracranial hypertension II. Patient study. Pediatr Radiol. 1996;26:706–10. doi: 10.1007/BF01383384. [DOI] [PubMed] [Google Scholar]
- 10.Dubourg J, Javouhey E, Geeraerts T, Messerer M, Kassai B. Ultrasonography of optic nerve sheath diameter for detection of raised intracranial pressure: A systematic review and meta-analysis. Intensive Care Med. 2011;37:1059–68. doi: 10.1007/s00134-011-2224-2. [DOI] [PubMed] [Google Scholar]
- 11.Dubost C, Le Gouez A, Jouffroy V, Roger-Christoph S, Benhamou D, Mercier FJ, et al. Optic nerve sheath diameter used as ultrasonographic assessment of the incidence of raised intracranial pressure in preeclampsia: A pilot study. Anesthesiology. 2012;116:1066–71. doi: 10.1097/ALN.0b013e318246ea1a. [DOI] [PubMed] [Google Scholar]
- 12.Rajajee V, Vanaman M, Fletcher JJ, Jacobs TL. Optic nerve ultrasound for the detection of raised intracranial pressure. Neurocrit Care. 2011;15:506–15. doi: 10.1007/s12028-011-9606-8. [DOI] [PubMed] [Google Scholar]
- 13.Gangemi M, Cennamo G, Maiuri F, D’Andrea F. Echographic measurement of the optic nerve in patients with intracranial hypertension. Neurochirurgia (Stuttg) 1987;30:53–5. doi: 10.1055/s-2008-1053656. [DOI] [PubMed] [Google Scholar]
- 14.Hayreh SS. Pathogenesis of oedema of the optic disc (papilloedema). A preliminary report. Br J Ophthalmol. 1964;48:522–43. doi: 10.1136/bjo.48.10.522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Geeraerts T, Launey Y, Martin L, Pottecher J, Vigué B, Duranteau J, et al. Ultrasonography of the optic nerve sheath may be useful for detecting raised intracranial pressure after severe brain injury. Intensive Care Med. 2007;33:1704–11. doi: 10.1007/s00134-007-0797-6. [DOI] [PubMed] [Google Scholar]
- 16.Kimberly HH, Shah S, Marill K, Noble V. Correlation of optic nerve sheath diameter with direct measurement of intracranial pressure. Acad Emerg Med. 2008;15:201–4. doi: 10.1111/j.1553-2712.2007.00031.x. [DOI] [PubMed] [Google Scholar]
- 17.Hansen HC, Helmke K. The subarachnoid space surrounding the optic nerves. An ultrasound study of the optic nerve sheath. Surg Radiol Anat. 1996;18:323–8. doi: 10.1007/BF01627611. [DOI] [PubMed] [Google Scholar]
- 18.Moretti R, Pizzi B. Optic nerve ultrasound for detection of intracranial hypertension in intracranial hemorrhage patients. Confirmation of previous findings in a different patient population. J Neurosurg Anesthesiol. 2009;21:16–20. doi: 10.1097/ANA.0b013e318185996a. [DOI] [PubMed] [Google Scholar]
- 19.Shirodkar CG, Rao SM, Mutkule DP, Harde YR, Venkategowda PM, Mahesh MU. Optic nerve sheath diameter as a marker for evaluation and prognostication of intracranial pressure in Indian patients: An observational study. Indian J Crit Care Med. 2014;18:728–34. doi: 10.4103/0972-5229.144015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ozgen A, Aydingöz U. Normative measurements of orbital structures using MRI. J Comput Assist Tomogr. 2000;24:493–6. doi: 10.1097/00004728-200005000-00025. [DOI] [PubMed] [Google Scholar]
- 21.Weigel M, Lagrèze WA, Lazzaro A, Hennig J, Bley TA. Fast and quantitative high-resolution magnetic resonance imaging of the optic nerve at 3.0 tesla. Invest Radiol. 2006;41:83–6. doi: 10.1097/01.rli.0000195820.98062.c5. [DOI] [PubMed] [Google Scholar]
- 22.Mashima Y, Oshitari K, Imamura Y, Momoshima S, Shiga H, Oguchi Y. High-resolution magnetic resonance imaging of the intraorbital optic nerve and subarachnoid space in patients with papilledema and optic atrophy. Arch Ophthalmol. 1996;114:1197–203. doi: 10.1001/archopht.1996.01100140397006. [DOI] [PubMed] [Google Scholar]
- 23.Gass A, Barker GJ, Riordan-Eva P, MacManus D, Sanders M, Tofts PS, et al. MRI of the optic nerve in benign intracranial hypertension. Neuroradiology. 1996;38:769–73. doi: 10.1007/s002340050344. [DOI] [PubMed] [Google Scholar]
- 24.Brodsky MC, Vaphiades M. Magnetic resonance imaging in pseudotumor cerebri. Ophthalmology. 1998;105:1686–93. doi: 10.1016/S0161-6420(98)99039-X. [DOI] [PubMed] [Google Scholar]
- 25.Agid R, Farb RI, Willinsky RA, Mikulis DJ, Tomlinson G. Idiopathic intracranial hypertension: The validity of cross-sectional neuroimaging signs. Neuroradiology. 2006;48:521–7. doi: 10.1007/s00234-006-0095-y. [DOI] [PubMed] [Google Scholar]
- 26.Steinborn M, Fiegler J, Ruedisser K, Hapfelmeier A, Denne C, Macdonald E, et al. Measurement of the optic nerve sheath diameter in children: Comparison between transbulbar sonography and magnetic resonance imaging. Ultraschall Med. 2012;33:569–73. doi: 10.1055/s-0031-1273491. [DOI] [PubMed] [Google Scholar]
- 27.Steinborn M, Fiegler J, Kraus V, Denne C, Hapfelmeier A, Wurzinger L, et al. High resolution ultrasound and magnetic resonance imaging of the optic nerve and the optic nerve sheath: Anatomic correlation and clinical importance. Ultraschall Med. 2011;32:608–13. doi: 10.1055/s-0029-1245822. [DOI] [PubMed] [Google Scholar]
- 28.Sekhon MS, McBeth P, Zou J, Qiao L, Kolmodin L, Henderson WR, et al. Association between optic nerve sheath diameter and mortality in patients with severe traumatic brain injury. Neurocrit Care. 2014;21:245–52. doi: 10.1007/s12028-014-0003-y. [DOI] [PubMed] [Google Scholar]


