Abstract
Background and Objectives:
Prehospital transport practices prevalent among children presenting to the emergency are under-reported. Our objectives were to evaluate the prehospital transport practices prevalent among children presenting to the pediatric emergency and their subsequent clinical course and outcome.
Methods:
In this prospective observational study we enrolled all children ≤17 years of age presenting to the pediatric emergency (from January to June 2013) and recorded their demographic data and variables pertaining to prehospital transport practices. Data was entered into Microsoft Excel and analyzed using Stata 11 (StataCorp, College Station, TX, USA).
Results:
A total of 319 patients presented to the emergency during the study period. Acute gastroenteritis, respiratory tract infection and fever were the most common reasons for presentation to the emergency. Seventy-three (23%) children required admission. Most commonly used public transport was auto-rickshaw (138, 43.5%) and median time taken to reach hospital was 22 min (interquartile range: 5, 720). Twenty-six patients were referred from another health facility. Of these, 25 were transported in ambulance unaccompanied. About 8% (25) of parents reported having difficulties in transporting their child to the hospital and 57% (181) of parents felt fellow passengers and drivers were unhelpful. On post-hoc analysis, only time taken to reach the hospital (30 vs. 20 min; relative risk [95% confidence interval]: 1.02 [1.007, 1.03], P = 0.003) and the illness nature were significant (45% vs. 2.6%; 0.58 [0.50, 0.67], P ≤ 0.0001) on multivariate analysis.
Conclusions:
In relation to prehospital transport among pediatric patients we observed that one-quarter of children presenting to the emergency required admission, the auto-rickshaw was the commonest mode of transport and that there is a lack of prior communication before referring patients for further management.
Keywords: Auto-rickshaw, delay in transport, inter-hospital transport, mode of transport, pediatric emergency, septic shock, transport
Introduction
Despite the advances in pediatrics, transport of sick children is still challenging and children are being transported in a high-risk environment with limited resources and monitoring.[1] Specially trained pediatric transport teams are firmly in place in the developed nations for transporting the critically ill to the hospital,[2,3] but the same is not true for most resource restricted settings. Patients in these settings often utilize locally available means of transportation to reach the nearest health facility. As a result, there is unavoidable delay without any documentation or record of vitals during transport.[4] This jeopardizes the health and thereby the outcomes of these patients. Although well-known, this finding is underreported.
The aim of our study was, therefore, to generate evidence on the prehospital transport practices prevalent among those presenting to our pediatric emergency room (ER) and their subsequent clinical course and outcome.
Methods
Setting and study population
We conducted this prospective observational study in the pediatric ER and Intensive Care Unit (ICU) of a tertiary care centre in New Delhi from January to June 2013. All children ≤17 years of age presenting to pediatric emergency were enrolled in the study after obtaining written informed consent from one of the parents. Children brought dead were excluded. The study protocol was approved by the Institutional Ethics Committee.
Objectives and outcome variables
Our primary objective was to evaluate the prehospital transport practices such as time taken (in minutes) to reach the health facility, distance travelled, mode of transport (type of vehicle used for transport), referral status, demographic profile, duration and nature of presenting illness (septic shock, neurological, cardiac, respiratory, postoperative, poisoning, liver failure, renal failure, and other conditions) presenting to the ER. Our secondary objective was to evaluate the clinical course and outcome of those requiring admission.
Study protocol
The prehospital transport parameters were recorded in a structured proforma in the ER. At admission, the vital parameters such as heart rate, blood pressure, respiratory rate, temperature, saturation, Glasgow Coma Scale and variables of the pediatric index of mortality 2 (PIM2) were also recorded. For the secondary objective we recorded variables such as the need for admission, clinical course, outcome and duration of hospital stay.
Sample size estimation
As our primary objective was to determine the prehospital transport practices prevalent among children presenting to the pediatric ER, we did not use any formal statistical methods to calculate the sample size. The sample was defined in terms of a number of cases recruited during the study period.
Statistical analysis
Data were entered in Epinfo 3.5.1 (CDC, Atlanta, USA) and analysis was done using Stata 11.0 (StataCorp, College Station, TX, USA). Continuous variables are presented as mean (standard deviation), or median (interquartile range [IQR]) as appropriate. Categorical variables are presented as absolute numbers (%). We also performed a univariate logistic regression analysis and stepwise multiple logistic regression by using “status of admission” (admitted or discharged) as the dependent variable and the variables thought to be clinically important as the independent variables.
Results
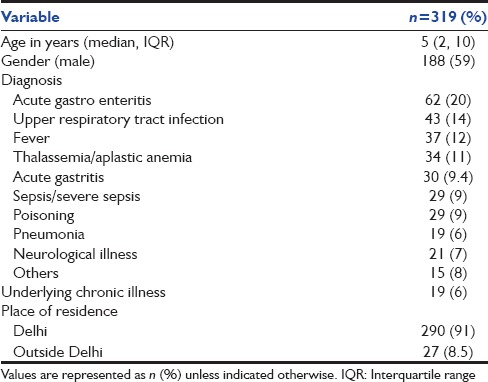
A total of 319 patients presented to the pediatric ER during the study period. The baseline characteristics of all children presenting to the emergency are described in Table 1. Acute gastroenteritis, respiratory tract infection and fever were the most common reasons for presentation to the emergency. The majority (293, 92%) were from Delhi.
Table 1.
Baseline characteristics of the study population
Primary outcomes
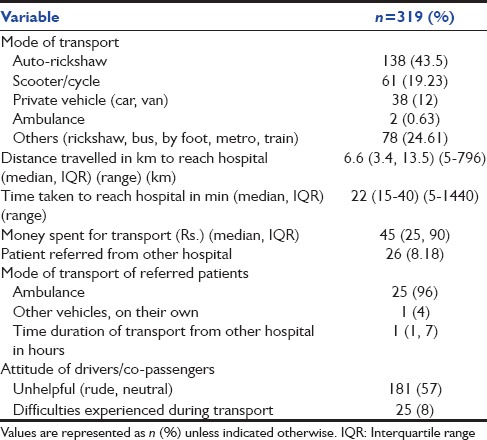
The majority of children were transported by public transport system. Most commonly used public transport was auto-rickshaw (138, 43.5%) and few others used private vehicle [Table 2]. The median time taken to reach the hospital was 22 min (IQR: 15–40). Twenty-six patients were referred from another health facility. Of these, 25 children were transported in ambulance unaccompanied. About 8% (25) of the parents reported having difficulties in transporting their child to the hospital and majority felt that they have received no help from drivers/co-passengers [Table 2].
Table 2.
Primary outcome - prehospital transport variables in children presenting to the emergency room
Secondary outcomes
Almost one quarter of the children (73, 22.8%) required admission. Of these, 54 (17%) required pediatric ICU (PICU) admission and the remaining were admitted to the wards. In those requiring PICU admission, the most common admitting diagnosis was a septic shock (26, 48%), followed by pneumonia (15, 28%) and status epilepticus (8, 15%). The median PIM2 probability was 56%. Ten children (18%) needed mechanical ventilation and 25 (46%) required inotropic support within the first hour of admission. Sixteen children (30%) died and median (IQR) duration of PICU stay was 5 (2–7) days. Twenty six children were referred from another health care facility. Of these 9 were in decompensated shock. None of those referred were transported with a transport team, proper documentation or any prior information.
Nineteen children were admitted to the wards. The admitting diagnoses in these children were acute exacerbation of asthma, pneumonia, acute gastroenteritis with severe dehydration, nephrotic syndrome, and febrile neutropenia among others. Only two children required subsequent ICU transfer and died. The remaining patients were discharged.
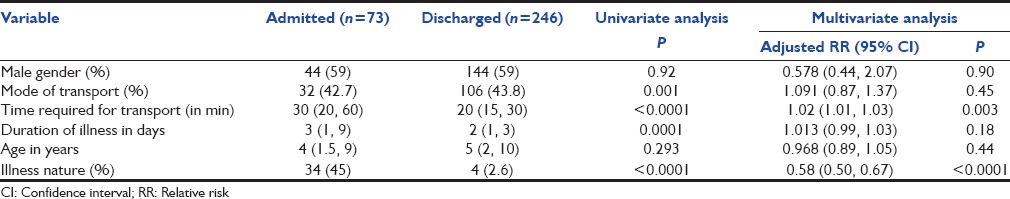
We also carried out a post-hoc analysis to see which prehospital transport factors were associated with the need for emergency admission. We found the mode of transport (auto-rickshaw versus others), the time required to reach the hospital, duration and nature of the illness (septic shock versus others) to be significant [Table 3]. However, on multivariate analysis, only the time required to reach the hospital (30 vs. 20 min; relative risk [RR] [95% confidence interval [CI]: 1.02 [1.007, 1.03], P = 0.003) and the illness nature remained significant (45% vs. 2.6%; RR [95% CI]: 0.58 [0.50, 0.67], P ≤ 0.0001).
Table 3.
Univariate and multivariate analysis of prehospital factors in children requiring hospital admission
Discussion
In this study, we observed that the profile of patients presenting to our emergency was similar to that of a previous report from South India. The common reasons for presentation and admission were respiratory illness, fever and seizures in that study.[5]
Despite the availability of free ambulance services in and around Delhi (both government and private) only a few arrived in an ambulance.[6,7] The reason for such underutilization might be that most of the parents are not aware of ambulance availability. Ambulance services, although supposed to be helpful, have their own pros and cons in our country. In Delhi, there is the availability of government-sponsored (Centralised Acciedent and Trauma Servies [CATS]) (nonprofit) and public private partnership operated ambulance services. But these services are not linked through one centralized telephone number and often patients during emergency don't know where to call. Ambulances run by the government and nongovernmental organization are not well equipped and most don't follow protocols in terms of equipment or personnel and none of these have coordination with local police. Due to inordinate delays in the arrival of the ambulance, people often prefer a locally available mode of transport like the auto-rickshaw that was the most common mode of transport in our study.
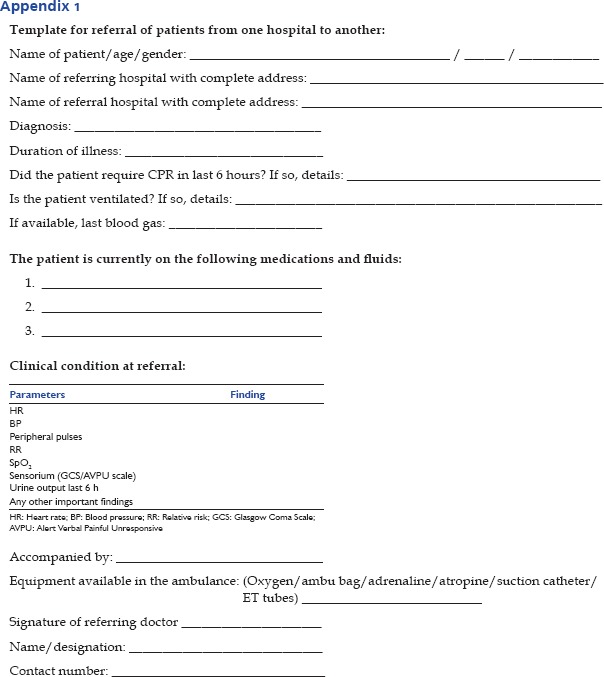
Interhospital transfers and referral of patients is done after prior communication and with a proper transport team as a standard of care.[2,8,9,10] However, we observed that none of the children referred to us from other health care facilities were accompanied by medical or paramedical personnel, or had a proper documentation and were shifted without prior information. Health care personnel need to be sensitive to the needs of sick patients during transport to improve this situation.[2,10] A simple proforma easy to fill and which does not miss out on important information such as that available in our emergency [Appendix 1] could be utilized for referring children.
Although post-hoc, on multivariate analysis of factors associated with emergency admission, we found the time required to reach hospital and illness nature (septic shock) to be significant after adjusting for all other factors. By ensuring optimal and timely transport using trained health care personnel both these factors, that is, delay in reaching the hospital and management of shock could be taken care of. Recognizing and treating septic shock early can prevent progression from compensated to decompensated shock and thereby improve outcomes.[11,12,13] Similarly, children because of their limited physiologic reserves can become critically ill in no time and the importance of ‘golden hour’ can only be overemphasized.[14] Therefore, it was not surprising to find these two factors significant after adjusting for all others.
The strength of our study is, it is the first study to report on the prehospital transport practices prevalent in children in a resource-limited setting. The limitation is, it is a single center study and the transport practices may be different in different settings. Our study therefore, could be considered a pilot study and the same repeated across many different hospitals, preferably in different parts of the country and in different settings (private, government, urban, rural etc.,). The data thus collected would then be robust and could be used to form policies.
Conclusion
Important conclusions from this study are - in relation to prehospital transport among paediatric patients we observed that one-quarter of children presenting to the emergency required admission, the auto-rickshaw was the commonest mode of transport and that there is a lack of prior communication before referring patients for further management.
Recommendations
As auto-rickshaw seems to be the most common mode of transport, training of auto-rickshaw drivers in basic life support skills and providing basic equipment to carry out the same in case of emergencies may be a small step towards improving the current situation. Public awareness about the availability of free ambulance services through telephone helpline numbers (toll free number - 102 for CATS) needs to be created and ambulance services should be prompt and easily accessible to those needing such services in emergency. More data on outcomes related to delayed or improper transport needs to be generated so that effective policies could be made for pediatric transport in our country.
Appendix 1: Template for referral of patients from one hospital to another:
Footnotes
Financial support and sponsorship Nil.
Conflict of Interest: There are no conflicts of interest.
References
- 1.Emergency Care for Children: Growing Pains. Washington, DC: National Academies Press; 2007. Institute of Medicine of the National Academies; pp. 2–3. [Google Scholar]
- 2.Orr RA, Felmet KA, Han Y, McCloskey KA, Dragotta MA, Bills DM, et al. Pediatric specialized transport teams are associated with improved outcomes. Pediatrics. 2009;124:40–8. doi: 10.1542/peds.2008-0515. [DOI] [PubMed] [Google Scholar]
- 3.Odetola FO, Rosenberg AL, Davis MM, Clark SJ, Dechert RE, Shanley TP. Do outcomes vary according to the source of admission to the Pediatric Intensive Care Unit? Pediatr Crit Care Med. 2008;9:20–5. doi: 10.1097/01.PCC.0000298642.11872.29. [DOI] [PubMed] [Google Scholar]
- 4.Limprayoon K, Sonjaipanich S, Susiva C. Transportation of critically ill patient to pediatric intensive care unit, Siriraj Hospital. J Med Assoc Thai. 2005;88(Suppl 8):S86–91. [PubMed] [Google Scholar]
- 5.Santhanam I, Pai M, Kasturi K, Radhamani MP. Mortality after admission in the pediatric emergency department: A prospective study from a referral children's hospital in southern India. Pediatr Crit Care Med. 2002;3:358–63. doi: 10.1097/00130478-200210000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Centralized Ambulance Trauma Services Supporting Documents. [Last accessed on 2015 May 12]. Available from: http://www.healthmarketinnovations.org/sites/default/files/Centralized%20Ambulance%20Trauma%20Services%20Supporting%20Document%202.pdf .
- 7.Transport in India. [Last accessed on 2015 Mar 24]. Available from: http://www.en.wikipedia.org/wiki/Transport_in_India .
- 8.Woodward GA, Insoft RM, Pearson-Shaver AL, Jaimovich D, Orr RA, Chambliss R, et al. The state of pediatric interfacility transport: Consensus of the second national pediatric and neonatal interfacility transport medicine leadership conference. Pediatr Emerg Care. 2002;18:38–43. doi: 10.1097/00006565-200202000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Stroud MH, Trautman MS, Meyer K, Moss MM, Schwartz HP, Bigham MT, et al. Pediatric and neonatal interfacility transport: Results from a national consensus conference. Pediatrics. 2013;132:359–66. doi: 10.1542/peds.2013-0529. [DOI] [PubMed] [Google Scholar]
- 10.Karlsen KA, Trautman M, Price-Douglas W, Smith S. National survey of neonatal transport teams in the United States. Pediatrics. 2011;128:685–91. doi: 10.1542/peds.2010-3796. [DOI] [PubMed] [Google Scholar]
- 11.Han YY, Carcillo JA, Dragotta MA, Bills DM, Watson RS, Westerman ME, et al. Early reversal of pediatric-neonatal septic shock by community physicians is associated with improved outcome. Pediatrics. 2003;112:793–9. doi: 10.1542/peds.112.4.793. [DOI] [PubMed] [Google Scholar]
- 12.Gross PA. Hypotension and mortality in septic shock: The “golden hour”. Crit Care Med. 2006;34:1819–20. doi: 10.1097/01.CCM.0000220054.95214.7D. [DOI] [PubMed] [Google Scholar]
- 13.Khilnani P, Singhi S, Lodha R, Santhanam I, Sachdev A, Chugh K, et al. Pediatric sepsis guidelines: Summary for resource-limited countries. Indian J Crit Care Med. 2010;14:41–52. doi: 10.4103/0972-5229.63029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stroud MH, Prodhan P, Moss MM, Anand KJ. Redefining the golden hour in pediatric transport. Pediatr Crit Care Med. 2008;9:435–7. doi: 10.1097/PCC.0b013e318172da62. [DOI] [PubMed] [Google Scholar]


