Abstract
Hypertriglyceridemia can cause severe diseases such as acute pancreatitis (AP) and coronary artery disease. The routine management of hypertriglyceridemia is dietary restriction of fat and lipid-lowering medications to manage the secondary or precipitating causes of hypertriglyceridemia. However, in cases of AP with severe hypertriglyceridemia (SHTG) (triglycerides [TG] >1000 mg/dl) rapid reduction of TG levels to well below 1000 mg/dl can improve outcome and prevent further episodes of pancreatitis. Plasmapheresis is a therapeutic option in such medical emergencies. We discussed 2 cases of severe AP with SHTG where we used early plsmapheresis along with other supportive management.
Keywords: Hypertriglyceridemia, plasmaphresis, severe acute pancreatitits
Introduction
Severe hypertriglyceridemia (SHTG) with acute pancreatitis (AP) is a medical emergency. SHTG has been reported to account up to 10% of all episodes of AP.[1] Conventional management of hypertriglyceridemia include dietary restriction of fat and pharmacological treatments. The main pharmacotherapy for high levels of triglycerides (TG) consists of insulin, heparin, omega-3 fatty acids, fibrates, statins, or niacin (nicotinic acid); however, slow mode of action of these agents is a concern in potentially life threatening situation. Plasmapheresis is a therapeutic option in such an emergency in rapidly lowering TG and has been used in studies with varied results.[2,3,4,5,6] We used early plasmapheresis in 2 cases of SHTG induced severe AP (SAP) and found significant rapid reduction of TG and improvement in organ failure.
Case 1
A 34-year-old female uncontrolled type II diabetes mellitus, obese (body mass index [BMI] 39/kg/m2) admitted with pain in epigastric region and vomiting since 3 days. On examination patient had pulse 135/min, respiratory rate (RR) 32/min, blood pressure (BP) 88/46 mm of Hg, with normal respiratory and cardiovascular examination on auscultation, abdominal distention, epigastric tenderness and guarding. She was admitted in intensive care unit (ICU), with APACHE II score 14, started on fluid resuscitation and other supportive management. Her ultrasound abdomen showed diffusely enlarged pancreas with fat stranding. Her arterial blood gas (ABG) showed severe anion gap metabolic acidosis. The blood was highly lipemic and on ultracentrifuge showed TG 9230 mg/dL [Table 1]. She had no history of alcohol use, drug intake, gallstones, and pancreatitis. The patient was managed as SHTG induced SAP and diabetic ketoacidosis with enteral fenofibrate other supportive management. Her condition further deteriorated next day with increasing respiratory distress requirement of vasopressors to maintain BP and she was started on plasmapheresis. Her TG after plasmapheresis decreased to 1620 mg/dL and 435 mg/dl after 1st and 2nd session respectively [Figure 1]. There was improvement in her clinical condition including respiratory failure. She was started on oral diet on subsequent day. Her contrast enhanced computerized topography (CECT) abdomen revealed severe pancreatitis with Balthazar score 7. She was shifted from ICU on day 7 and discharged on day 14 with oral atorvastatin, fenofibrate and insulin. On her follow-up after 1-month her TG were 123 mg/dl.
Table 1.
Initial laboratory investigations
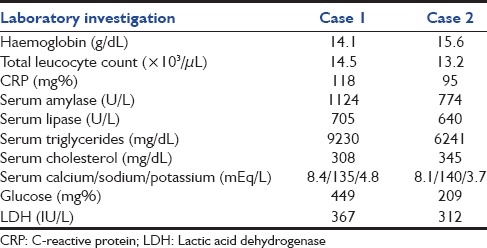
Figure 1.
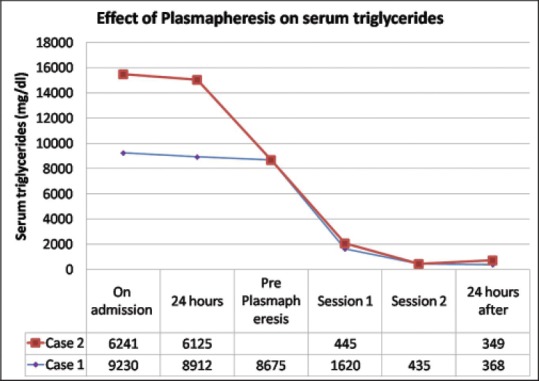
Effect on plasmapheresis on serum triglycerides
Case 2
A 35-year-old male admitted with pain abdomen since 5 days and vomiting since 2 days. On examination his temperature 38.3°C, pulse 124/min, BP 118/46 mm Hg, RR 27/min, BMI 35.7 kg/m 2 and decrease air entry in bases of both lungs with normal cardiovascular examination. He was started on fluid resuscitation and shifted to ICU with APACHE II score 11. His ABG showed metabolic acidosis and on ultrasound abdomen was unremarkable with obscured pancreas due to bowel gas. His noncontrast CT abdomen revealed distorted architecture of pancreas with peripancreatic fat stranding. He had a history of poorly controlled type II diabetes mellitus with hypertriglyceridemia, but he stopped fenofibrate since 6 months. He was nonvegetarian in diet with no history of gallstones or alcohol intake. His blood was lipemic and after ultracentrifuge showed TG 6241 mg/dl [Table 1]. He was taken for urgent plasmapheresis on day 2 in view of deteriorating clinical condition with replacement by thawed fresh frozen plasma [Figure 2]. Postplasmapheresis, his TG decreased to 445 mg/dl and patient showed significant clinical improvement with resolution acidosis and respiratory distress. His CECT abdomen showed pancreatitis with Balthazar score 6. He was started on oral fat-free diet and fenofibrate on day 4 and discharged on day 10. On follow-up after 2 month his TG were 109 mg/dl.
Figure 2.

Plasmapheresis showing extracted highly lipemic plasma
Discussion
Severe hypertriglyceridemia with serum triglyceride concentrations >1000 mg/dL is a risk factor for AP.[2] SHTG can also interfere with clinical laboratory tests, making patient diagnosis and management more difficult. In both of our patients due to very high levels of TG, the serum sample so lipemic that no sample testing could be performed initially. Ultracentrifugation can be used for extracting serum for laboratory diagnostic testing. The exact pathophysiology of hypertriglyceridemia induced AP is not clear. A proposed mechanism is hydrolysis of TG by pancreatic lipase, leading to accumulation of high concentrations free fatty acids and chylomicrons which can produce acinar cell injury and capillary plugging causing ischemia and acidosis activating trypsinogen and AP.[7] Conventional management of hypertriglyceridemia dietary fat restriction and pharmacotherapy is time consuming. Also in the patients with SAP urgent lowering of TG is necessary to prevent disease complications and oral pharmacological therapy may not always be feasible.[7,8]
Plasmapheresis is an effective therapeutic option for rapidly lowering TG in such cases. There are few case studies reports published in literature.[2,3,4,5,6,7,8] The indications of plasmapheresis or lipid apheresis in such cases are (a) patient refractory to nutritional and pharmacological approaches, (b) serum TG exceed 1000 mg/dL, (c) serum lipase 3 times the upper limit of normal, (d) severe hypocalcemia, (e) lactic acidosis, and (f) worsening inflammation and organ dysfunction.[9] Our patients in Case 1 had 5 and Case 2 had 4 out of 6 criteria respectively.
The beneficial effect of plasmapheresis is believed to be because of rapid decrease in TG levels, however, removal of excessive proteases from the plasma which are key enzymes in inflammation and replacement of consumed protease inhibitors might be an additionally benefit.[8]
In a recent review on plasmapheresis in hypertriglyceridemia-induced AP, though the triglyceride levels reduced by 46–80%, there was still no benefit in outcome because of insufficient studies.[10] In another observation study, the plasmapheresis effectively reduced TG faster than could be expected with conservative treatment and improve outcome.[8] The timing of initiation of plasmapheresis might be crucial. There are few reports showing that reduction in morbidity and mortality with plasmapheresis can be achieved when apheresis is used early.[4,6,10] We used plasmapheresis in both of our cases within 48 h of diagnosing AP with hypertriglyceridemia. Both the patients not only showed rapid reduction of TG but also improvement in organ failure.
Conclusion
Plasmapheresis is an effective therapeutic option for SHTG induced SAP with rapid reduction of serum TG and can be considered early in the management.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Anderson F, Thomson SR, Clarke DL, Buccimazza I. Dyslipidaemic pancreatitis clinical assessment and analysis of disease severity and outcomes. Pancreatology. 2009;9:252–7. doi: 10.1159/000212091. [DOI] [PubMed] [Google Scholar]
- 2.Ewald N, Kloer HU. Treatment options for severe hypertriglyceridemia (SHTG): The role of apheresis. Clin Res Cardiol Suppl. 2012;7:31–5. doi: 10.1007/s11789-012-0042-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramírez-Bueno A, Salazar-Ramírez C, Cota-Delgado F, de la Torre-Prados MV, Valdivielso P. Plasmapheresis as treatment for hyperlipidemic pancreatitis. Eur J Intern Med. 2014;25:160–3. doi: 10.1016/j.ejim.2013.08.701. [DOI] [PubMed] [Google Scholar]
- 4.Syed H, Bilusic M, Rhondla C, Tavaria A. Plasmapheresis in the treatment of hypertriglyceridemia-induced pancreatitis: A community hospital's experience. J Clin Apher. 2010;25:229–34. doi: 10.1002/jca.20232. [DOI] [PubMed] [Google Scholar]
- 5.Ábel T, Sándor K, Tremmel A, Pénzes I, Gamal EM, Lengyel G, et al. Plasmapheresis in the treatment of hypertriglyceridemia. Orv Hetil. 2014;155:1203–6. doi: 10.1556/OH.2014.29954. [DOI] [PubMed] [Google Scholar]
- 6.Kyriakidis AV, Karydakis P, Neofytou N, Pyrgioti M, Vasilakakis D, Digenis P, et al. Plasmapheresis in the management of acute severe hyperlipidemic pancreatitis: Report of 5 cases. Pancreatology. 2005;5:201–4. doi: 10.1159/000085272. [DOI] [PubMed] [Google Scholar]
- 7.Havel RJ. Pathogenesis, differentiation and management of hypertriglyceridemia. Adv Intern Med. 1969;15:117–54. [PubMed] [Google Scholar]
- 8.Gubensek J, Buturovic-Ponikvar J, Romozi K, Ponikvar R. Factors affecting outcome in acute hypertriglyceridemic pancreatitis treated with plasma exchange: An observational cohort study. PLoS One. 2014;9:e102748. doi: 10.1371/journal.pone.0102748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta N, Ahmed S, Shaffer L, Cavens P, Blankstein J. Severe hypertriglyceridemia induced pancreatitis in pregnancy. Case Rep Obstet Gynecol. 2014;2014:485493. doi: 10.1155/2014/485493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rehmanjan M. Is plasmapheresis the optimal treatment option for acute pancreatitis secondary to hypertriglyceridemia. A systematic review? Aust Med Stud J. 2014;4:19–22. [Google Scholar]


