Abstract
Objective:
Cadaveric dissection is used as a major tool for anatomy education at the medical school. In this study we aimed to determine how a uro-anatomy cadaveric dissection course would impact urology residents knowledge.
Materials and methods:
A three days course was given to 50 urology residents by experienced trainers in 1–3 June 2012 at Ege University Medical School’s Anatomy Department, İzmir, Turkey. Efficacy of the course was assessed using a multiple choice questionnaire of 20 questions given before and after the course.
Results:
Completed questionnaires before and after the course were available for 25 residents (50%) that were included. Residents answered correctly to 11.7 out of 20 questions (59%) before the course and 13.0 out of 20 (65%) after (p<0.05). In individuals analysis, 16 residents (64%) increased their scores, 4 (16%) had similar scores and 5 (20%) had lower scores. The number of correct answers for 6 out of the 20 questions was lower following the course.
Conclusion:
This cadaveric surgical anatomy course was effective in improving surgical anatomy knowledge for most urology residents but not all and helped to identify ways to improve the course in the future.
Keywords: Anatomy, cadaver, education, training, urology
Introduction
Knowledge in anatomy is essential for a safe and effective medical practice.[1] Training sources available for anatomy education are expanding such as anatomy software, live surgery anatomy or medical imaging, but access to cadaveric anatomy is becoming less common.[2] Cadaveric dissection is used as a major tool in learning anatomy, owing to its perceived effectiveness for understanding classification and inter-relationship of different body parts, integration of theory and practice of anatomy, touch-mediated perception, three-dimensional perspectives of structures, and application of practical skills.[3–10] In addition, surgeons may be exposed to pathological conditions and/or anatomical variations during the dissection process, which enhances their learning experience. Through the use of prosection, cadaveric material can be expertly dissected to show surgeons exactly what is intended for them to see without the risk of it being damaged by inexperienced hands. Moreover team-based learning methods in teaching topographical anatomy by dissection provides better acquisition of such knowledge than the previous methods of anatomy teaching to which students have been exposed. Learning anatomy via a surgical approach provides a relevant, in-depth, purposeful and enjoyable learning experience. This technique also provided a valuable insight into surgery.[1] On the other hand dissection videos did not improve performance on final examination scores; however, students favored their use.[13]
The value of anatomy dissection courses using human cadavers in imparting anatomical knowledge has been clearly established.[14–16] Nonetheless, most studies have shown that this applies to medical student learning anatomy. Residents in surgical specialties are regularly exposed to anatomy through surgery or medical imaging and it is unknown whether they will benefit from anatomy courses based on cadaveric dissection. In this study we aimed to determine how a course using cadaveric dissection would impact on urology residents’ knowledge in kidney, prostate, pelvic and genital organs anatomy.
Material and methods
The study was conducted after the approval of the local ethics committee, among 50 urology residents who undertook a three days surgical and theoretical urological anatomy cadaveric dissection course in 1–3 June 2012 at Ege University Medical School’s Anatomy Department, İzmir, Turkey. Mean age was 29 years (26 to 35). All residents were males. The course was advertised my emailing urologists members of the International Young Urologist Association (IYUA) and through its website (www.iyua.org). The number of places was limited to 50. The subsequent topics of the course on urological anatomy were: (A) kidney, ureter and retroperitoneal region (5 hours); (B) prostate (4 hours); (C) Bladder, urethra and pelvis (4 hours) and (D) penis and scrotum (4 hours). Each topic had a consistent sequence of educational activities including urological interactive lecture (1–1.5 hours), task-driven directed self-study in preparation for a subsequent small group work (1 hours), and practical anatomy course (2–2.5 hours).
A formal 25 minutes examination took place before and after the course. The examination consisted in 20 multiple-choice questions with a maximum of five alternative answers. Section A, B, C and D had 11, 5, 3 and 1 questions respectively. The questions were randomly selected from a bank of multiple-choice questions prepared by the 37 scientists. The same 20 questions were asked to the residents before and after the course.
Statistical Analysis
The main outcome measure was overall examination score. Data was analyzed using the Statistical Package for Social Sciences version 15 (SPSS Inc, Chicago, IL, USA). Significance testing of proportions was appropriate by using Wilcoxon matched pairs test, where p≤0.05 was considered significant.
Results
Completed questionnaires before and after the course were available for 25 residents (50%), 19 refused to participate and 6 were excluded because they did not answer all the questions (Figure 1).
Figure 1.
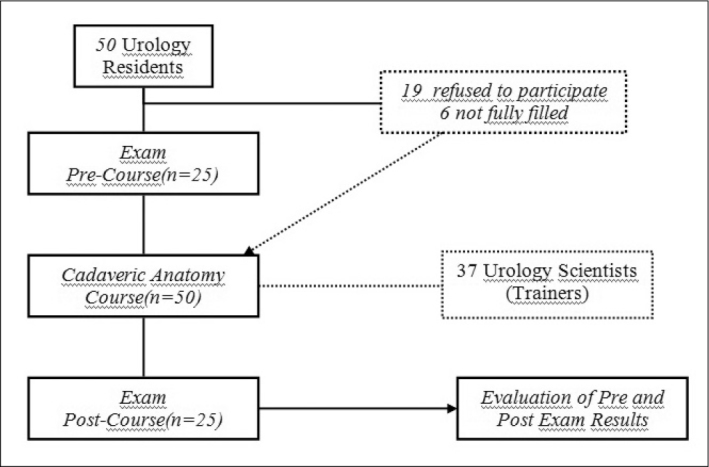
Flow chart of the study
Residents answered correctly to 11.7 out of 20 questions (59%) before the course and 13.0 out of 20 (65%) after (p<0.05).
The detail for each individual is reported in Figure 2. For 13 questions (65%), the number of correct answers was higher following the course (Figure 3). All residents had a pre course score <15, and three had a post course score ≥15. Scores in sub groups questions (A, B, C, D) also increased after the course (p<0.05) (Table 1), In individuals analysis, 16 residents (64%) increased their scores, 4 (16%) had similar score and 5 (20%) had a lower score (Figure 3). No question was answered correctly by all residents in the pre-test, while 3 questions were answered correctly by all residents after the course. These questions were about muscles anatomy. Worse results were observed following the course for 6 questions (30%) mainly about arteries anatomy.
Figure 2.
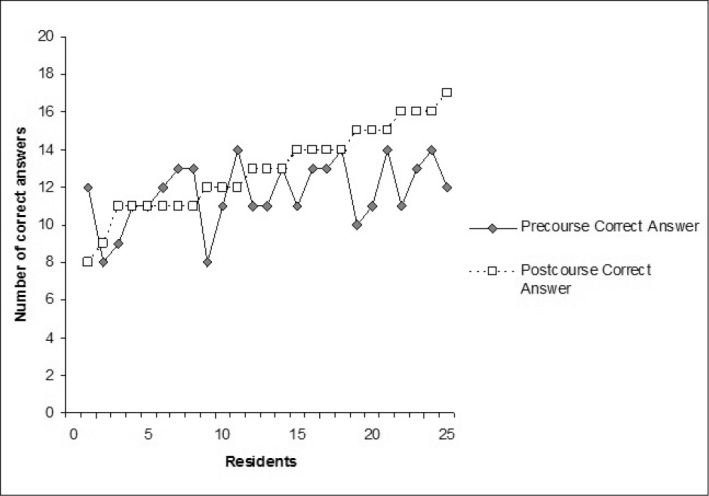
Number of correct answers before and after the course for each resident
Figure 3.
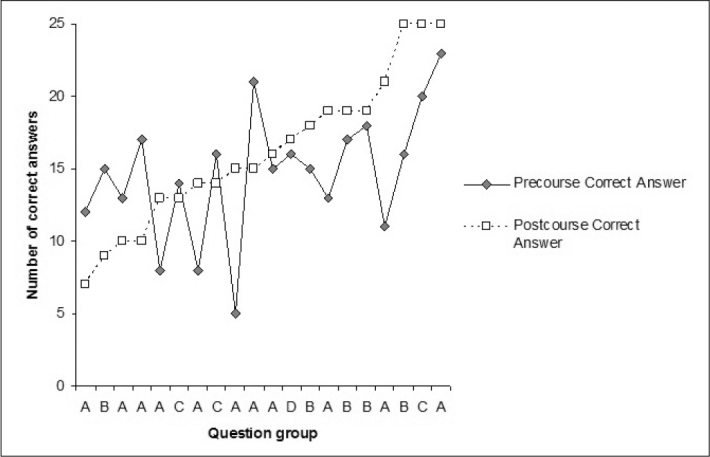
Number of correct answers before and after the courses for each question
Table 1.
Average number of questions in each subgroup properly answered by the residents
| Question Group | Section A | Section B | Section C | Section D | All |
|---|---|---|---|---|---|
| Number of questions | 11 | 5 | 3 | 1 | 20 |
| Precourse average number well answered (% of all questions) | 5.8 (52.7%) | 3.2 (64%) | 2 (66.7%) | 0.6 (60%) | 11.7 (58.5%) |
| Postcourse average number well answered (% of all questions) | 6.6 (60%) | 3.6 (72%) | 2.1 (70%) | 0.7 (70%) | 13 (65%) |
| Difference | 13.8% | 12.5% | 5% | 16.7% | 11.1% |
We also observed lower score for foreigners (average score on 20 before and after) but this did not appear as statistically significant.
Discussion
Overall, this course on cadaveric surgical anatomy improved residents’ knowledge in uro-anatomy. Nonetheless, the training was not efficient for 36% of the residents who achieved worse or similar post course scores. This highlights the limits of this course and gives suggestions on topics that need to be better detailed in future to improve its educational value. It is also possible that questions with similar or worse post course scores were confusing and need to be rephrased. A validation process of the questions was lacking and will be integrated in future courses. Nonetheless, the examination assessed objectively the impact of the course on residents’ knowledge. Theoretical knowledge was only one part of this training which includes practical aspects of urological anatomy that were not assessed by the questionnaire and are of critical importance for surgical practice. The natural view of anatomical structures is particularly beneficial to the trainees learning process as it relates to texture, color, location, size, and function of the various organs.[17]
Anatomy dissection courses using human cadavers have long been used to impart anatomical knowledge to surgical trainees.[14–16] This process provides a valuable insight into surgery and focus on the anatomy.[1] The design of classic lectures, notes and practical anatomy laboratory lectures empower the residents to direct, evaluate and reflect on their learning. This teaching method based on student-directed fresh tissue anatomy courses is appreciated by students who found objectives were clear, achievable, and taught effectively with relevant clinical correlates.[18]
Another advantage of the laboratory session design is the interaction between educational doctors and trainees which offers an opportunity for professional development and continuous improvement of resident teaching skills. Trainers have been established as an effective teaching resource in several areas of gross anatomy education.[19–21] This study gave also the opportunity for ‘stepped procedure’ learning in surgical education. First residents see the anatomical structure in real body but bloodless and safely. Then they can use the knowledge during surgical procedure of living bodies. During the learning period, using the surgical steps to determine the lack of training could be suggested.[22] Nonetheless, whether this course will impact on surgical training remains to be proven.
The challenge is to find cost-effective models and teaching systems that have a high reproducibility with humans and have a high degree of transferability from the training model to the living human. Traditional model of clinical training is the most common source of training for residents but has various disadvantages. Inefficient and dangerous practices may be perpetuated and inadequate supervision of procedural skills in the operating theatre was reported by advanced surgical trainees.[23–25] Benefits of a competency-based training should include rapid improvements in trainees’ skills that are sustained and transferable to the clinical setting.[23] Live animal models are interesting to learn the principles of surgery but they are not broadly available, of little interest for learning human anatomy, expensive and carry a potential infectious risk. Simulators or dissection videos have also been used but the latest were not improving performance on final examination scores; although students favored their use.[13]
One of the limits of the assessment of the educational value of this training method was the number of residents who refused to complete the questionnaire. This is possibly related to poor anatomy knowledge in this subgroup and it remains unknown whether a minimal background in urological anatomy would be required for optimal course efficacy. Questionnaire assessment of any educational program is of paramount importance for the trainers should they wish to improve the quality of the course in further teaching sessions. Ideally, a salvage session for those having knowledge in some sub topics would warrant the objectives of the course were reached. This study did not assess whether knowledge acquisition also remained or faded quickly with time. In the future, technical training components could be implemented following this course so to favor surgical training efficacy and safety.
Altogether, based on strict objective data this course improved responses rates and probably knowledge in anatomy. Nonetheless this is only part of the benefits expected from such a course. The ability for residents to better recognize anatomical structures in the human body during practical session aims to improve their surgical skills. This was not measured although this is likely to be the main objective for residents. Measuring this would be uneasy, but we plan to add questions for future courses on whether the course might be of any clinical use for their current or future practice and whether future courses should be tailored in a different way to respond such needs.
This study showed that a cadaveric surgical anatomy course is effective in improving surgical anatomy knowledge in most urology residents and helped to identify ways to improve the course in the future. Whether cadaveric surgical anatomy training performs better than other methods would require further studies.
Footnotes
Ethics Committee Approval: Ethics committee approval was obtained.
Informed Consent: We didn’t use patients, patients’ names, initials, or hospital numbers, especially in any illustrative materials in this questinnary study. Informed consent forms were not necessary for these reasons.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - S.Ö., E.H.; Design - İ.T.; Supervision - M.S., M.B.; Funding - M.S., M.B.; Materials - İ.T.; Data Collection and/or Processing - S.Ö., E.H.; Analysis and/or Interpretation - Ö.F.Y.; Literature Review - T.K.; Writer - S.Ö., E.H.; Critical Review - S.L., T.K.
Conflict of Interest: The authors declared no conflict of interest.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Nutt J, Mehdian R, Parkin I, Dent J, Kellett C. Cadaveric surgery: a novel approach to teaching clinical anatomy. Clin Teach. 2012;9:148–51. doi: 10.1111/j.1743-498X.2012.00536.x. http://dx.doi.org/10.1111/j.1743-498X.2012.00536.x. [DOI] [PubMed] [Google Scholar]
- 2.McLachlan JC, Bligh J, Bradley P, Searle J. Teaching anatomy without cadavers. Med Educ. 2004;38:418–24. doi: 10.1046/j.1365-2923.2004.01795.x. http://dx.doi.org/10.1046/j.1365-2923.2004.01795.x. [DOI] [PubMed] [Google Scholar]
- 3.Aziz MA, Mckenzie JC, Wilson JS, Cowie RJ, Ayeni SA, Dunn BK. The human cadaver in the age of biomedical informatics. Anat Rec. 2002;269:20–32. doi: 10.1002/ar.10046. http://dx.doi.org/10.1002/ar.10046. [DOI] [PubMed] [Google Scholar]
- 4.Rizzolo LJ. Human dissection: an approach to interweaving the traditional and humanistic goals of medical education. Anat Rec. 2002;269:242–8. doi: 10.1002/ar.10188. http://dx.doi.org/10.1002/ar.10188. [DOI] [PubMed] [Google Scholar]
- 5.Hinduja K, Samuel R, Mitchell S. Problem-based learning: Is anatomy a casualty? Surgeon. 2005;3:84–7. doi: 10.1016/s1479-666x(05)80067-8. http://dx.doi.org/10.1016/S1479-666X(05)80067-8. [DOI] [PubMed] [Google Scholar]
- 6.Lempp HK. Perceptions of dissection by students in one medical school: beyond learning about anatomy. A qualitative study. Med Educ. 2005;39:318–25. doi: 10.1111/j.1365-2929.2005.02095.x. http://dx.doi.org/10.1111/j.1365-2929.2005.02095.x. [DOI] [PubMed] [Google Scholar]
- 7.Lachman N, Pawlina W. Integrating professionalism in early medical education: the theory and application of reflective practice in the anatomy curriculum. Clin Anat. 2006;19:456–60. doi: 10.1002/ca.20344. http://dx.doi.org/10.1002/ca.20344. [DOI] [PubMed] [Google Scholar]
- 8.Azer SA, Eizenberg N. Do we need dissection in an integrated problem-based learning medical course? Perceptions of first- and second-year students. Surg Radiol Anat. 2007;29:173–80. doi: 10.1007/s00276-007-0180-x. http://dx.doi.org/10.1007/s00276-007-0180-x. [DOI] [PubMed] [Google Scholar]
- 9.Gogalniceanu P, Madani H, Paraskeva PA, Darzi A. A minimally invasive approach to undergraduate anatomy teaching. Anat Sci Educ. 2008;1:46–7. doi: 10.1002/ase.9. http://dx.doi.org/10.1002/ase.9. [DOI] [PubMed] [Google Scholar]
- 10.Sugand K, Abrahams P, Khurana A. The anatomy of anatomy: A review for its modernization. Anat Sci Educ. 2010;3:83–93. doi: 10.1002/ase.139. http://dx.doi.org/10.1002/ase.139. [DOI] [PubMed] [Google Scholar]
- 11.Codd AM, Choudhury B. Virtual reality anatomy: is it comparable with traditional methods in the teaching of human forearm musculoskeletal anatomy? Anat Sci Educ. 2011;4:119–25. doi: 10.1002/ase.214. http://dx.doi.org/10.1002/ase.214. [DOI] [PubMed] [Google Scholar]
- 12.Burgess AW, Ramsey-Stewart G, May J, Mellis C. Team-based learning methods in teaching topographical anatomy by dissection. ANZ J Surg. 2012;82:457–60. doi: 10.1111/j.1445-2197.2012.06077.x. http://dx.doi.org/10.1111/j.1445-2197.2012.06077.x. [DOI] [PubMed] [Google Scholar]
- 13.Mahmud W, Hyder O, Butt J, Aftab A. Dissection videos do not improve anatomy examination scores. Anat Sci Educ. 2011;4:16–21. doi: 10.1002/ase.194. http://dx.doi.org/10.1002/ase.194. [DOI] [PubMed] [Google Scholar]
- 14.Fahrer M. Art macabre: Is anatomy necessary? ANZ J Surg. 2001;71:783–4. http://dx.doi.org/10.1046/j.1440-1622.2001.02161.x. [PubMed] [Google Scholar]
- 15.Parker LM. Anatomical dissection. Why are we cutting it out? Dissection in undergraduate teaching. ANZ J Surg. 2002;72:910–2. doi: 10.1046/j.1445-2197.2002.02596.x. http://dx.doi.org/10.1046/j.1445-2197.2002.02596.x. [DOI] [PubMed] [Google Scholar]
- 16.Stewart F, West R. Gross topographical anatomy by dissection for basic surgical training candidates: Development and implementation of a course at University of Sydney. ANZ J Surg. 2002;72:98. [Google Scholar]
- 17.Robinson AG, Metten S, Guiton G, Berek J. Using fresh tissue dissection to teach human anatomy in the clinical years. Acad Med. 2004;79:711–16. doi: 10.1097/00001888-200407000-00021. http://dx.doi.org/10.1097/00001888-200407000-00021. [DOI] [PubMed] [Google Scholar]
- 18.McBride JM, Drake RL. Student-directed fresh tissue anatomy course for physician residents. Anat Sci Educ. 2011;4:264–8. doi: 10.1002/ase.233. http://dx.doi.org/10.1002/ase.233. [DOI] [PubMed] [Google Scholar]
- 19.Yeager VL, Young PA. Peer teaching in gross anatomy at St. Louis University. Clin Anat. 1992;5:304–10. http://dx.doi.org/10.1002/ca.980050407. [Google Scholar]
- 20.Brueckner JK, MacPherson BR. Benefits from peer teaching in the dental gross anatomy laboratory. Eur J Dent Educ. 2004;8:72–7. doi: 10.1111/j.1600-0579.2003.00333.x. http://dx.doi.org/10.1111/j.1600-0579.2003.00333.x. [DOI] [PubMed] [Google Scholar]
- 21.Youdas JW, Hoffarth BL, Kohlwey SR, Kramer CM, Petro JL. Peer teaching among physical therapy students during human gross anatomy: perceptions of peer teachers and students. Anat Sci Educ. 2008;1:199–206. doi: 10.1002/ase.44. http://dx.doi.org/10.1002/ase.44. [DOI] [PubMed] [Google Scholar]
- 22.Emre H, Turgay A, Ali A, Murat B, Ozgür Y, Cankon G. ‘Stepped procedure’ in laparoscopic cyst decortication during the learning period of laparoscopic surgery: Detailed evaluation of initial experiences. J Minim Access Surg. 2010;6:37–41. doi: 10.4103/0972-9941.65162. http://dx.doi.org/10.4103/0972-9941.65162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martin M, Vashisht B, Frezza E, Ferone T, Lopez B, Pahuja M, et al. Competency-based instruction in critical invasive skills improves both resident performance and patient safety. Surgery. 1998;124:313–7. http://dx.doi.org/10.1016/S0039-6060(98)70136-9. [PubMed] [Google Scholar]
- 24.Thomson BNJ, Civil ID, Danne PD, Deane SA, McGrath PJ. Trauma training in Australia and New Zealand: results of a survey of advanced surgical trainees. ANZ J Surg. 2001;71:83–8. doi: 10.1046/j.1440-1622.2001.02033.x. http://dx.doi.org/10.1046/j.1440-1622.2001.02033.x. [DOI] [PubMed] [Google Scholar]
- 25.McMahon DJ, Chen S, MacLellan DG. Formal teaching of basic surgical skills. ANZ J Surg. 1995;65:607–9. doi: 10.1111/j.1445-2197.1995.tb01707.x. http://dx.doi.org/10.1111/j.1445-2197.1995.tb01707.x. [DOI] [PubMed] [Google Scholar]


