Abstract
Objective:
To explore the feasibility of laparoscopic trans-rectal Natural Orifice Transluminal Endoscopic Surgery (NOTES) radical prostatectomy in a cadaveric model and to define anatomical landmarks of this surgical route.
Materials and methods:
After the ethical clearance, the study was conducted in Turkish Council of Forensic Medicine. With the cadaver in an exaggerated lithotomy position, a full thickness incision was made on the anterior wall of the rectum. The anteriorly visible Denonvilliers’ fascia was incised sharply, exposing the posterior surface of the prostate. A single-port device (GelPOINT®Path) was inserted transanally passing the incision on the anterior wall of the rectum, into the bluntly created space between rectum and prostate. Three, 10 mm ports were placed through the GelPOINT®Path, at 3, 6, and 9 o’clock positions. A 5 mm, 0° degree lens was introduced at 6 o’clock position; followed by laparoscopic scissors and laparoscopic grasper. Prostatic and periprostatic anatomy was defined as encountered during each step of the procedure.
Results:
Exposure of the posterior surface of the prostate and seminal vesicles was easily achieved. No additional openings of the rectal wall were made. Surgical specimen was extracted keeping its integrity.
Conclusion:
Transrectal radical prostatectomy is technically feasible in the cadaver model, being facilitated by previous experience with perineal surgery. Anatomical observations during the present experimental study suggest that the transrectal NOTES route provides good exposure of the operative field and easy access to the posterior surface of prostate, Future experimental endeavors should focus on reproducibility of this approach and feasibility of lymph node dissection using trans-rectal route.
Keywords: Laparoscopic, radical prostatectomy, single port, transrectal
Introduction
Natural Orifice Transluminal Endoscopic Surgery (NOTES) aims at reproducing minimally invasive surgery with emphasis on diminishing port related complications, reducing pain and maximizing the cosmetic outcomes.[1] NOTES is still in a developmental stage and much work is still needed to refine techniques, verify safety and document efficacy. However, this remains a field of intense clinical and experimental research in various surgical specialties.[2]
A transurethral approach has been previously described for NOTES radical prostatectomy.[3] The transrectal NOTES route has been explored for nephrectomy to date.[4] Given previous experience matured at our center with endoscope-assisted radical perineal prostatectomy (RPP),[5,6] we aimed to explore the technical feasibility of transrectal radical prostatectomy (TRRP) in a cadaveric model and to outline the surgical anatomy of prostate and its surrounding structures when using a transrectal NOTES route.
Material and methods
Once ethical committee of Turkish Council of Forensic Medicine approved the study, they referred an unclaimed 60-year-old male fresh cadaver with no proof of previous prostate surgery. Surgical procedure was applied in the operating room of R.T. Ministry of Justice-Turkish Council of Forensic Medicine. Digital rectal examination showed a very small prostate gland, with apex/anal orifice distance measuring 2.5 cm.
Surgical technique
The cadaver was placed in the exaggerated lithotomy position. A handheld retractor on the posterior rectal wall maintained visualization of the anterior rectal wall adjacent (posterior) to prostate.
A full thickness incision with 3 cm length was made on the anterior wall of the rectum starting from the palpable prostate apex toward prostatic base, proximal to dentate line (Figure 1a). The anteriorly visible Denonvilliers’ fascia was incised sharply, exposing the posterior surface of the prostate. Blunt dissection was performed to create adequate space for insertion of the access port. The single port (GelPOINT® Path Transanal Access Platform, Applied Medical) was inserted trans-anally passing the incision on the anterior wall of the rectum, into the created space between rectum and prostate (Figure 1b). The cavity was insufflated using a thermo-insufflator set at 15mmHg pressure. Three, 10 mm trocars were placed in the single port at 3, 6, and 9 o’clock positions. A 5 mm 0 degree lens was introduced via the 6 o’clock port.
Figure 1. a, b.
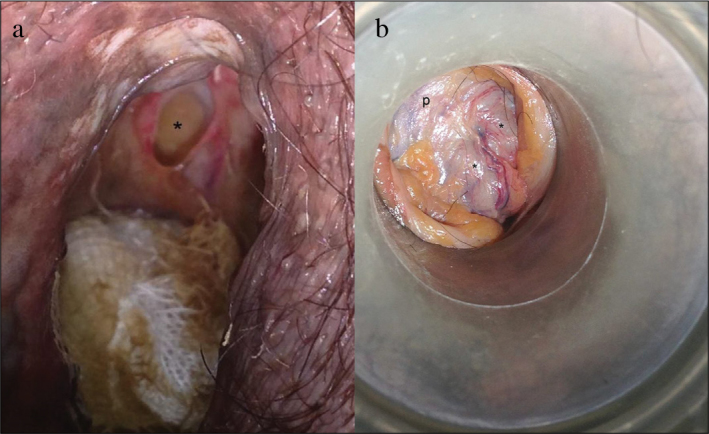
(a) The full thickness incision on the anterior wall of rectum. Incised thin DenonVillier’s fascia appears as a white crescent. The sponge is placed posteriorly in the rectum. The (*) marks the rectoprostatic area behind the DenonVillier’s fascia. (b) Single port view of rectoprostatic area prior to insufflation. p: Prostate. *: Vas deferentia
The bare posterior surface of the prostate and seminal vesicles were seen at the center of the screen with intact endopelvic fascia covering the gland laterally (Figure 2a, 2b). The Denonvilliers’ fascia overlying the seminal vesicles was quite attenuated. Five mm straight laparoscopic scissors were introduced through the 3 o’clock port, followed by a grasper via the 9 o’clock positioned port. The space between lateral lobes of the prostate and endopelvic/periprostatic fascia was further developed with blunt dissection with laparoscopic instruments.
Figure 2. a, b.
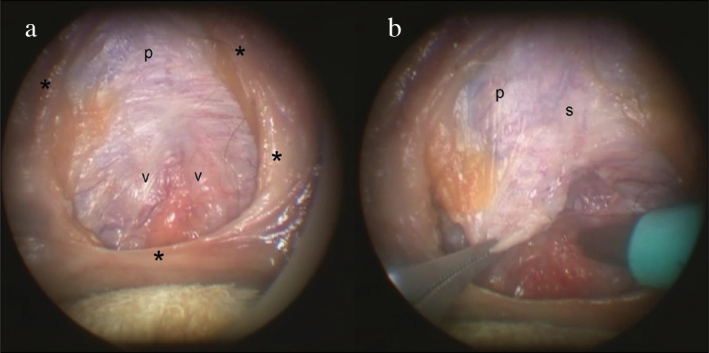
(a) Camera view after insufflation; p: Prostate; v: Vas deferentia; *: marks the borders of anterior rectal wall incision. (b) Endopelvic fascia covering the lateral surface of the prostate is under traction by grasper on the right side; p: Prostate; s: midline prostatic sulcus
The intrafascial dissection ensured the preservation of the neurovascular bundles. Vas deferentia were identified and sharply transected near their entrance into prostate. Relatively atrophic seminal vesicles were bluntly dissected in their entirety. Apical anatomy was further defined by blunt dissection followed by sharp transection of the membranous urethra. The lateral extensions of puboprostatic ligaments and the dorsal vein complex were visualized following this maneuver (Figure 3a, 3b). Dorsal vein and puboprostatic ligaments were spared. Dissection in the space between cephalic surface of the prostate and dorsal venous complex toward prostatic base led to complete mobilization of the prostate. Prostatic pedicles were controlled in the same manner as the perineal radical prostatectomy approach, postero-laterally at the base. The prostate-bladder junction was defined on its entirety.
Figure 3. a, b.
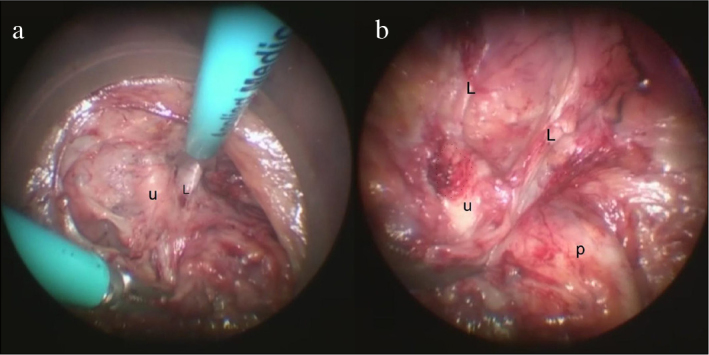
(a) Prostatic apical dissection; u: Urethra; L: Puboprostatic ligaments. (b) Transected urethra and adjacent anatomical structures; u: Proximal urethra; L: Puboprostatic ligaments; p: Prostate.
Bladder neck was opened at six o’clock followed by complete excision of the prostate. The specimen was removed via the single port. Inspection of the specimen revealed an intact small prostate (Figure 4a). On laparoscopic inspection of the bladder interior and trigone, both intact ureteric orifices were identified. A urinary catheter was passed through the membranous urethra into the bladder. With minimal traction of the inflated urethral catheter, the bladder and the membranous urethra were approximated without any tension. After removing of the single port device, the incision in the anterior wall of the rectum was closed using a continuous single layer 3/0 monofilament suture.
Figure 4. a–c.
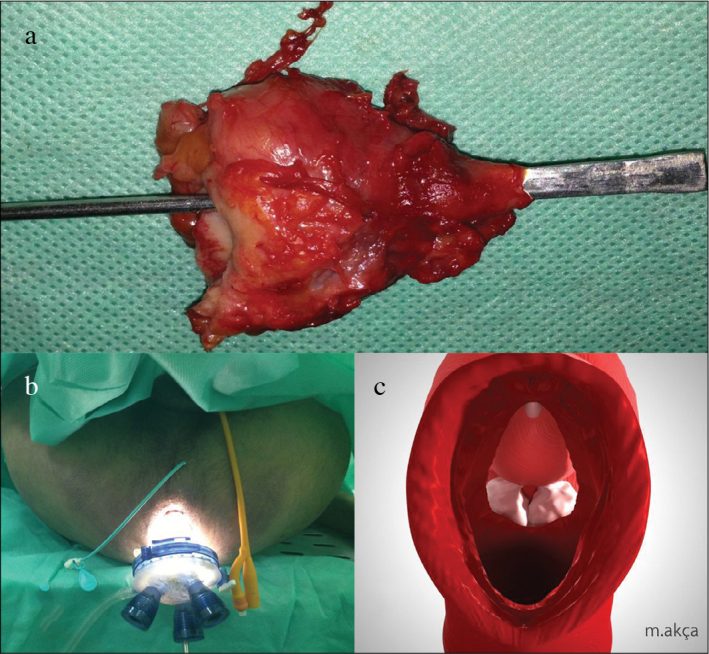
(a) The prostatectomy specimen. (b) External view of single port inserted transanally (urethral catheter and percutaneous drain can be seen in situ). (c) 3-dimensional axial lithotomy view illustrating prostate and its relations via the transrectal route
Statistical analysis
Since the study is describing an innovate operation technique applied on a single cadaver, no statistical analysis was required and used.
Results
Exposure of the posterior surface of the prostate and seminal vesicles was easily achieved. There was no injury to vascular or neural structures since endopelvic fascia and DVC (Dorsal Venous Complex) have never been incised. No additional openings of the rectal wall were made and incised anterior rectal wall was closed easily after the removal of single port. Integrity of the surgical specimen was preserved during surgical procedure and extraction.
Discussion
In this experimental study, the concept of NOTES was applied to the radical prostatectomy procedure with the aim of exploring the surgical anatomy of the prostate gland and its surrounding structures when using a transrectal approach.
Rectal injuries represent possible but rare events during routine radical prostatectomy, not leading to major complications if timely recognized and repaired.[7,8] Transrectal route for performing nephrectomy has been previously described in cadaveric[9] and animal models.[10]
The presently described technique of TRRP has similarities with the perineal approach. The claimed benefits of perineal approach include maintaining the integrity of endopelvic fascia, minimizing injury to striated urethral sphincter, enhanced visualization of urethro-vesical anastomosis,[11] and suitability for obese patients particularly in the settings of previous abdominal surgery.[12,13]
Intrafascial dissection as a method for nerve preservation during radical prostatectomy has been previously described.[14] With transrectal prostatectomy approach, similar to perineal prostatectomy,[15] intrafascial dissection aids with the preservation of neurovascular bundles during prostatectomy.
Conceptually TRRP approach offers similar advantages with potential additional benefits. In our experiment we noted that exposing the posterior surface of the prostate and seminal vesicles was easily achieved, compared to our perineal experience where this step of the procedure can be more challenging due to the anatomical barriers. For instance, the step of division of rectoprostatic muscle fibers is time consuming due to surgeon’s concern for incidental rectal injury. In contrast if the plane of dissection is too far anteriorly, there is a risk of injury to striated urethral sphincter. TRRP path of dissection mitigates these risks. Although with TRRP rectal incision is mandatory, however given the knowledge of its presence and subsequent meticulous repair makes this less morbid than an inadvertent unrecognized injury.
Excision and subsequent repair of the rectum is an established principle in trans-anal minimally invasive surgery (TAMIS). TAMIS literature has shown that full thickness segments of the rectum can be excised and repaired for treatment of rectal malignancy with minimal complications and without the need for fecal diversion.[16,17]
We could not assess the viability of rectal wall post procedure in a cadaveric model. Prolonged retraction on the rectal wall with the GelPoint and the manipulation during the procedure could have a detrimental effect on the viability of the rectal tissue. However this phenomenon has not been described with previous NOTES in animal model utilizing rectal route[10] or human studies with NOTES.[18]
Another observed improvement compared to the perineal technique was better visualization of surgical field owing to magnification offered by endoscopic equipment. At the same time this improvement in vision along with pneumatic insufflation allowed for easier dissection and better ergonomics. Finally, like any other NOTES procedure TRRP may offer a scarless surgery. This feature can potentially translate into further reduction of surgical invasiveness.
Another advantage of TRRP compare to NOTES transurethral prostatectomy is the integrity of the surgical specimen for pathology assessment and negating the need for making additional skin incisions during extraction. Depending on the technique, NOTES transurethral prostatectomy, either requires morcellation[19] of the specimen or additional skin incision for the specimen extraction.[3] Morcellation is contradictory to oncological principles. On the other hand, creating additional skin incisions moves away from the principle of NOTES and should be considered a hybrid technique.[1]
Few important issues require further consideration. Rectal injury during prostatectomy is a feared complication of the procedure. Although experience from TAMIS with this regard is encouraging but the idea of opening the gastrointestinal system within proximity to the vesico-urethral anastomosis site, demands further contemplation. Potential risk for development of rectourethral fistula cannot be over emphasized and any assessment of this risk without further in vivo experiments is not plausible. Creating a watertight anastomosis and layered rectal closure, along with use of vascularized interposition graft are possible avenues for preventing such a catastrophic complication.
The potential for anal sphincter injury and rectal continence mechanism dysfunction post-procedure is another issue that needs to be considered. The rectal wall incision in this case was proximal to dentate (pectinate) line, which is a safe area in terms of distance from anal sphincter. The deep, superficial and subcutaneous components of external anal sphincter and internal anal sphincter all lie caudal to our incision site.[20,21] Data from TAMIS procedures suggest that the risk of anal sphincter injury and dysfunction is relatively low.[22,23]
Some of the limitations inherent to single port surgery also apply to TRRP. Reduced maneuverability, loss of instrument triangulation and the need for advance laparoscopic suturing skills during the vesico-urethral anastomosis are some of the technical limitations of this approach. Further developments of the TRRP technique should encompass exploration of the utility of robotic platforms[24] to overcome these limitations.
Another challenge with this procedure is the limitation of performing lymph node dissection via the trans-rectal route. While simultaneous lymph node dissection within the perineal prostatectomy has been described[25], its feasibility during the TRRP requires further examination.
In conclusion, transrectal radical prostatectomy is technically feasible in the cadaver model, being facilitated by previous experience with perineal surgery. Anatomical observations during the present experimental study suggest that the transrectal NOTES route provides good exposure of the operative field and easy access to the posterior surface of prostate. Future experimental endeavors should focus on reproducibility of this approach and feasibility of lymph node dissection using trans-rectal route.
Acknowledgments
Ali Simsek for assisting with reviewing the manuscript’s text in English. Muhammet Akca for 3D illustrations. Saglam-Medical Equipments (GIMMI® Laparoscopy system) and Intra-Medical Equipments (Applied Medical GelPOINT®Path and Laparoscopic hand instruments) for their contributions.
Footnotes
Ethics Committee Approval: Ethics committee approval was obtained.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - O.A.; Design - O.A., A.S.G., A.A., S.A.; Supervision - O.A., H.Z., R.A., L.F.B., S.A., R.H.; Materials -A.S.G, A.A.; Data Collection and/or Processing - O.A., A.S.G., A.A.; Analysis and/or Interpretation - O.A., H.Z., R.A., L.F.B., S.A., R.H.; Literature Review - O.A., H.Z., S.A.; Writer - O.A., H.Z., S.A.; Critical Review - O.A., H.Z., R.A., L.F.B., A.S.G., A.A., R.H., S.A.
Conflict of Interest: The authors declared no conflict of interest.
Financial Disclosure: Oktay Akca is funded by TUBITAK.
Consent form for the cadaver study: According to the law has been printed by the date of June 31, 2004 and by the number of 25539 prompting in the ‘c’ section of 10th subject in the Official Gazette of Turkish Republic, Scientific Committee of Turkish Council of Forensic Medicine approved the study.
References
- 1.Gettman MT, Box G, Averch T, Cadeddu JA, Cherullo E, Clayman RV, et al. Consensus statement on natural orifice transluminal endoscopic surgery and single-incision laparoscopic surgery: heralding a new era in urology? Eur Urol. 2008;53:1117–20. doi: 10.1016/j.eururo.2008.02.006. http://dx.doi.org/10.1016/j.eururo.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 2.Autorino R, Yakoubi R, White WM, Gettman M, De Sio M, Quattrone C, et al. Natural orifice transluminal endoscopic surgery (NOTES): where are we going? A bibliometric assessment. BJU Int. 2013;111:11–6. doi: 10.1111/j.1464-410X.2012.11494.x. http://dx.doi.org/10.1111/j.1464-410X.2012.11494.x. [DOI] [PubMed] [Google Scholar]
- 3.Humphreys MR, Sauer JS, Ryan AR, Leslie KO, Castle EP, Lingeman JE, et al. Natural orifice transluminal endoscopic radical prostatectomy: initial perioperative and pathologic results. Urology. 2011;78:1211–7. doi: 10.1016/j.urology.2011.06.056. http://dx.doi.org/10.1016/j.urology.2011.06.056. [DOI] [PubMed] [Google Scholar]
- 4.Bazzi WM, Stroup SP, Cohen SA, Dotai T, Kopp RP, Colangelo C, et al. Feasibility of transrectal hybrid natural orifice transluminal endoscopic surgery (NOTES) nephrectomy in the cadaveric model. Urology. 2012;80:590–95. doi: 10.1016/j.urology.2012.06.026. http://dx.doi.org/10.1016/j.urology.2012.06.026. [DOI] [PubMed] [Google Scholar]
- 5.Albayrak S, Canguven O, Aydemir H, Goktas C, Cetinel C, Akca O. Endoscope-assisted radical perineal prostatectomy. J Endourol. 2010;24:527–30. doi: 10.1089/end.2009.0398. http://dx.doi.org/10.1089/end.2009.0398. [DOI] [PubMed] [Google Scholar]
- 6.Oktay A, Savas Y, Rahim H, Mustafa B, Alper K, Cihangir C, et al. Enigmatic traces determined on radical perineal prostatectomy specimens: an anatomohistological study. J Clin Anal Med. 2014;5:377–80. [Google Scholar]
- 7.Wedmid A, Mendoza P, Sharma S, Hastings RL, Monahan KP, Walicki M, et al. Rectal injury during robot-assisted radical prostatectomy: incidence and management. J Urol. 2011;186:1928–33. doi: 10.1016/j.juro.2011.07.004. http://dx.doi.org/10.1016/j.juro.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 8.Yıldırım M, Göktaş C, Horuz R, Cetinel CA, Cangüven O, Küçük HF, et al. Rectal injury during radical prostatectomy. Ulus Travma Acil Cerrahi Derg. 2012;18:250–4. doi: 10.5505/tjtes.2012.04379. http://dx.doi.org/10.5505/tjtes.2012.04379. [DOI] [PubMed] [Google Scholar]
- 9.Eyraud R, Laydner H, Autorino R, Hillyer S, Long JA, Panumatrassamee K, et al. Robot-assisted transrectal hybrid natural orifice translumenal endoscopic surgery nephrectomy and adrenalectomy: initial investigation in a cadaver model. Urology. 2013;81:1090–4. doi: 10.1016/j.urology.2012.11.006. http://dx.doi.org/10.1016/j.urology.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 10.Bazzi WM, Stroup SP, Cohen SA, Sisul DM, Liss MA, Masterson JH, et al. Comparison of transrectal and transvaginal hybrid natural orifice transluminal endoscopic surgery partial nephrectomy in the porcine model. Urology. 2013;82:84–9. doi: 10.1016/j.urology.2013.03.007. http://dx.doi.org/10.1016/j.urology.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 11.Harris MJ. The anatomic radical perineal prostatectomy: an outcomes-based evolution. Eur Urol. 2007;52:81–8. doi: 10.1016/j.eururo.2006.10.041. http://dx.doi.org/10.1016/j.eururo.2006.10.041. [DOI] [PubMed] [Google Scholar]
- 12.Yiou R, Salomon L, Colombel M, Patard JJ, Chopin D, Abbou CC. Perineal approach to radical prostatectomy in kidney transplant recipients with localized prostate cancer. Urology. 1999;53:822–4. doi: 10.1016/s0090-4295(98)00365-3. http://dx.doi.org/10.1016/S0090-4295(98)00365-3. [DOI] [PubMed] [Google Scholar]
- 13.Boczko J, Melman A. Radical perineal prostatectomy in obese patients. Urology. 2003;62:467–9. doi: 10.1016/s0090-4295(03)00464-3. http://dx.doi.org/10.1016/S0090-4295(03)00464-3. [DOI] [PubMed] [Google Scholar]
- 14.Stolzenburg JU, Schwalenberg T, Horn LC, Neuhaus J, Constantinides C, Liatsikos EN. Anatomical landmarks of radical prostatecomy. Eur Urol. 2007;51:629–39. doi: 10.1016/j.eururo.2006.11.012. http://dx.doi.org/10.1016/j.eururo.2006.11.012. [DOI] [PubMed] [Google Scholar]
- 15.Weiss JP, Schlecker BA, Wein AJ, Hanno PM. Preservation of periprostatic autonomic nerves during total perineal prostatectomy by intrafascial dissection. Urology. 1985;26:160–3. doi: 10.1016/0090-4295(85)90051-2. http://dx.doi.org/10.1016/0090-4295(85)90051-2. [DOI] [PubMed] [Google Scholar]
- 16.Atallah S, Albert M, Larach S. Transanal minimally invasive surgery: a giant leap forward. Surg Endosc. 2010;24:2200–5. doi: 10.1007/s00464-010-0927-z. http://dx.doi.org/10.1007/s00464-010-0927-z. [DOI] [PubMed] [Google Scholar]
- 17.Atallah SB, Albert MR, deBeche-Adams TH, Larach SW. Robotic TransAnal Minimally Invasive Surgery in a cadaveric model. Tech Coloproctol. 2011;15:461–4. doi: 10.1007/s10151-011-0762-9. http://dx.doi.org/10.1007/s10151-011-0762-9. [DOI] [PubMed] [Google Scholar]
- 18.Kaouk JH, Khalifeh A, Laydner H, Autorino R, Hillyer SP, Panumatrassamee K, et al. Transvaginal hybrid natural orifice transluminal surgery robotic donor nephrectomy: first clinical application. Urology. 2012;80:1171–5. doi: 10.1016/j.urology.2012.08.061. http://dx.doi.org/10.1016/j.urology.2012.08.061. [DOI] [PubMed] [Google Scholar]
- 19.Humphreys MR, Krambeck AE, Andrews PE, Castle EP, Lingeman JE. Natural orifice translumenal endoscopic surgical radical prostatectomy: proof of concept. J Endourol. 2009;23:669–75. doi: 10.1089/end.2008.0670. http://dx.doi.org/10.1089/end.2008.0670. [DOI] [PubMed] [Google Scholar]
- 20.Bai X, Li S, Yu B, Su H, Jin W, Chen G, et al. Sphincter-preserving surgery after preoperative radiochemotherapy for T3 low rectal cancers Oncol lett. 2012;3:1336–40. doi: 10.3892/ol.2012.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tokoro T, Okuno K, Hida J, Ueda K, Yoshifuji T, Daito K, et al. Analysis of the clinical factors associated with anal function after intersphincteric resection for very low rectal cancer. World J Surg Oncol. 2013;11:24. doi: 10.1186/1477-7819-11-24. http://dx.doi.org/10.1186/1477-7819-11-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee TG, Lee SJ. Transanal single-port microsurgery for rectal tumors: minimal invasive surgery under spinal anesthesia. Surg Endosc. 2014;28:271–80. doi: 10.1007/s00464-013-3184-0. http://dx.doi.org/10.1007/s00464-013-3184-0. [DOI] [PubMed] [Google Scholar]
- 23.Albert MR, Atallah SB, deBeche-Adams TC, Izfar S, Larach SW. Transanal minimally invasive surgery (TAMIS) for local excision of benign neoplasms and early-stage rectal cancer: efficacy and outcomes in the first 50 patients. Dis Colon Rectum. 2013;56:301–7. doi: 10.1097/DCR.0b013e31827ca313. http://dx.doi.org/10.1097/DCR.0b013e31827ca313. [DOI] [PubMed] [Google Scholar]
- 24.Haber GP, White MA, Autorino R, Escobar PF, Kroh MD, Chalikonda S, et al. Novel robotic da Vinci instruments for laparoendoscopic single-site surgery. Urology. 2010;76:1279–82. doi: 10.1016/j.urology.2010.06.070. http://dx.doi.org/10.1016/j.urology.2010.06.070. [DOI] [PubMed] [Google Scholar]
- 25.Keller H, Lehmann J, Beier J. Radical perineal prostatectomy and simultaneous extended pelvic lymph node dissection via the same incision. Eur Urol. 2007;52:384–8. doi: 10.1016/j.eururo.2006.09.045. http://dx.doi.org/10.1016/j.eururo.2006.09.045. [DOI] [PubMed] [Google Scholar]


