Abstract
Double-j (DJ) ureteral stenting is a very common procedure performed after various endourological procedures. Although several complications due to DJ stent insertion were revealed, only three cases of renal parenchymal perforation have been reported to date. We present a case of a 35-year-old woman who had perforation of renal parenchyma without perirenal hematoma following insertion of DJ ureteral stent after flexible ureteroscopy for the treatment of an upper ureteral calculi. Non-contrast computed tomography was used for diagnosis. Patient was successfully managed with repositioning of the stent under fluoroscopic guidance on postoperative second day postoperatively.
Keywords: Double-j stent, flexible ureteroscopy, renal parenchymal perforation
Introduction
Ureteral stenting via endoscopic route was firstly reported by Zimskind et al.[1] in 1967. In urology practice frequently observed adverse effects related tu ureteral stenting can be enumerated as urinary system infections, hematuria, irritative ureteral complaints, and flank pain secondary to vesicoureteral reflux. Apart from these adverse effects, intravascular migration of double-J (D-J) catheter, ureteroarterial fistula, hemoperitoneum, and knotted stent have been reported in the literature as very rarely seen complications.[2–5] Perforation of the renal parenchyma associated with perirenal hematoma after ureteral DJ stenting has been reported firstly by Dündar et al.[6] in 2008. We have encountered a total of only 3 cases cited in the literature.[6–8] In one of the cases proper positioning of DJ stent was reported as sufficient to prevent complications[7] while in two cases application of blood transfusion was reported because of associated perirenal hematoma.[6,8]
In this paper we presented a case of perforation of renal parenchyma as a complication of flexible ureteroscopy (FURS) we applied for the management of upper left ureteral stone.
Case presentation
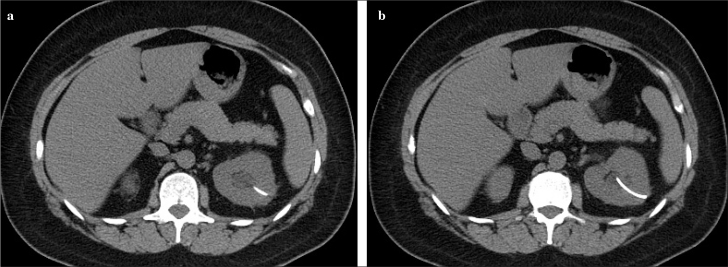
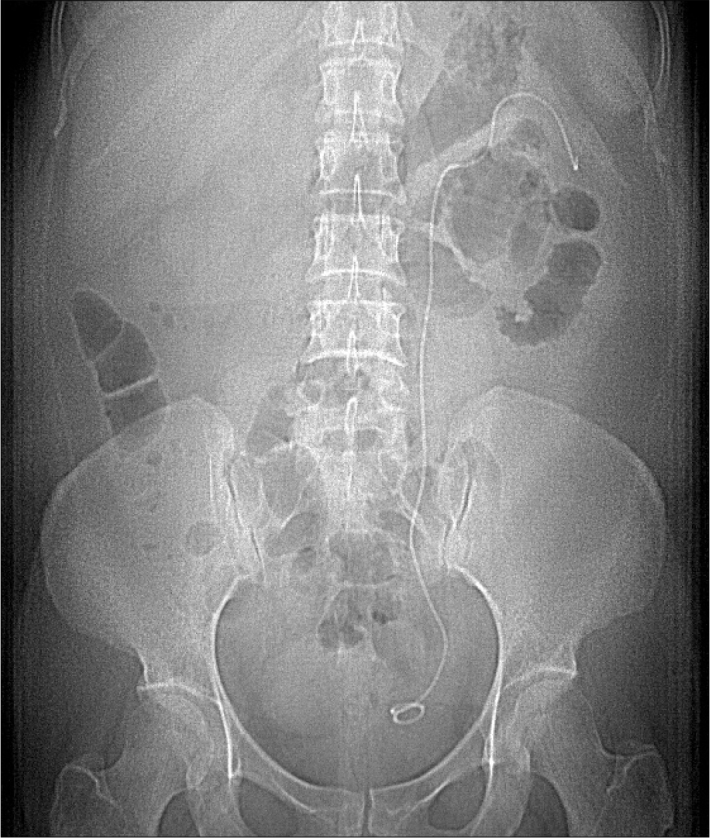
A 35-year-old female patient without any metabolic disease or previously experienced surgery consulted to our urology clinic with complaints of recurrent left renal colic within the last 2 months. The patient had been treated with 4 sessions of failed extracorporal shock-wave lithotripsy (ESWL) one month ago previously for her left proximal ureteral stone. Her physical examination revealed left costovertebral angle tenderness, while microscopic hematuria was noted in her urinalysis. Bacterial growth was not detected in her urine culture. On her urinary system noncontrast computed tomography (CT), upper urinary system stone (9 mm), and grade 2–3 hydro-ureteronephrosis was detected. Ureteroscopic lithotripsy was planned. Under general anesthesia, with semi-rigid ureteroscope, attempts to access to the stone failed, so with a flexible ureteroscope (7.5 F Storz Ureteroscope) passed over 9.5 F access sheath the stone was approached. The stone was pushed into renal pelvis, and then into a lower calyx. Afterwards using 200 µm Holmium laser probe the stone was completely fragmented. Following the procedure which was achieved without any problem, flexible ureteroscope was withdrawn, then through an access sheath a 0.038 inch-soft-tipped hydrophilic guidewire was advanced to the collecting system and over the guidewire a 4.8 F DJ ureteral stent was advanced. All these procedures were performed under fluoroscopic guidance. Curling of both ends of the stent was observed during fluoroscopy which necessitated successful termination of the procedure. Bladder was evacuated with 10F Nelaton catheter, and a Foley catheter was not inserted via transurethral route. On post-operative first day the patient did not require analgesics, and so she was discharged On postoperative second day she presented to the emergency service with severe renal colicky pain. The patient with stable vital findings underwent plain KUB (Figure 1), then noncontrast computed tomograms were obtained when the proximal tip of the stent was suspected to be outside of the collecting system. On CT, we observed that proximal tip perforated the renal parenchyma, and curled in the perirenal area (Figures 2, 3). Perirenal hematoma or urinoma was not observed. Then under local anesthesia, cystoscopy was performed, and stent was grasped from its distal end with a foreign substance forceps under fluoroscopic guidance, and brought back into proximal renal collecting system. The patient was followed up on an ambulatory basis with oral antibiotics, and analgesics Three weeks later her stent was removed. Any additional complication was not observed.
Figure 1.
Postoperative seconday KUB image
KUB: Kidney-ureter- bladder
Figure 2. a, b.
The course of ureteral DJ stent inside the renal parenchyma
DJ: double-j
Figure 3.
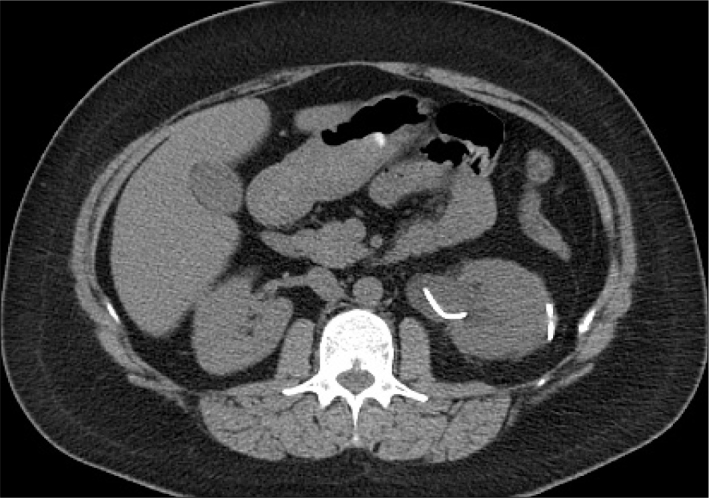
Curling of the ureteral Double-J-stent outside the renal parenchyma
Discussion
As a complication of ureteral double-j stenting renal parenchyma perforation is a quiet rarely encountered condition. In 2 of 3 literature cases we could access, serious perirenal hematoma accompanied parenchymal perforation.[6,8] In this article we presented the second case of parenchymal perforation in the literature not associated with perirenal hematoma.[7] Two cases reported in the literature were complications of DJ stenting applied following rigid ureteroscopic lithotripsy[6,7], while the third case was a ureteral DJ stenting performed for the management of a ureteral stone in a patient with a solitary kidney under the guidance of cystoscope.[8] In our case, this complication developed during laser lithotripsy performed using flexible ureteroscope placed over access sheath after pushing the stone from ureter into the lower calyx group.
We reviewed surgical notes, and videoscopic images so as to analyze possible etiological factors. During laser fragmentation procedure, we determined from surgical notes, and videoscopic images that irrigation fluid drained actively through access sheath, and the procedure lasted within less than 20 minutes under a low intrarenal pressure. Besides videofilms taken during surgery were examined, and it was confirmed that laser energy was directed only at stone without any damage to surrounding tissues which might otherwise cause bleeding or perforation of the collecting system. Calyx which retained the fragmented stone, and location of the perforation was far away from each other. The first thing that came to our mind was that rigid tip of the guide-wire positioned in the access sheath before DJ stenting might stick into collecting system leading to perforation However in that case we thought that advancement of DJ stent through a soft tip will be difficult which could be at a high probability discerned instantaneously during the operation. We couldn’t explain how soft tip of the guidewire perforated renal parenchyma.
If proper curling of the proximal end of the DJ stent as visualized during fluoroscopic images performed at the end of the operation is accepted as the only criterion for correct positioning of the stent, then as was seen in our case, errors can be made.
In conclusion, it should be kept in mind that ‘so-called’ invasive ureteral stenting frequently applied following endourological surgieries though rarely can lead to life-threatening complications ranging from pulmonary embolism to transfusion-requiring perirenal hematoma.
Footnotes
Informed Consent: Written informed consent was obtained from patient who participated in this case.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - B.A.; Design - B.A.; Supervision - B.E.; Funding - V.G.; Data Collection and/or Processing - B.A., M.C.K.; Analysis and/or Interpretation - B.A.; Literature Review -B.A.; Writer - B.A.; Critical Review - B.E.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Zimskind PD, Fetter TR, Wilkerson JL. Clinical use of long-term indwelling silicone rubber ureteral splints inserted cystoscopically. J Urol. 1967;97:840–4. doi: 10.1016/S0022-5347(17)63130-6. [DOI] [PubMed] [Google Scholar]
- 2.Michalopoulos AS, Tzoufi MJ, Theodorakis G, Mentzelopoulos SD. Acute postoperative pulmonary thromboembolism as a result of intravascular migration of a pigtail ureteral stent. Anesth Analg. 2002;95:1185–8. doi: 10.1097/00000539-200211000-00011. http://dx.doi.org/10.1097/00000539-200211000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Gelder MS, Alvarez RD, Partridge EE. Ureteroarterial fistulae in exenteration patients with indwelling ureteral stents. Gynecol Oncol. 1993;50:365–70. doi: 10.1006/gyno.1993.1227. http://dx.doi.org/10.1006/gyno.1993.1227. [DOI] [PubMed] [Google Scholar]
- 4.Chitale SV, Ho ET. Haemoperitoneum secondary to ureteric stenting. Int Urol Nephrol. 2002;34:197–8. doi: 10.1023/a:1023274514526. http://dx.doi.org/10.1023/A:1023274514526. [DOI] [PubMed] [Google Scholar]
- 5.Baldwin DD, Juriansz GJ, Stewart S. Knotted ureteral stent: a minimally invasive technique for removal. J Urol. 1998;159:2065–6. doi: 10.1016/S0022-5347(01)63248-8. http://dx.doi.org/10.1016/S0022-5347(01)63248-8. [DOI] [PubMed] [Google Scholar]
- 6.Dündar M, Çalışkan T, Koçak İ. Unexpected complication: renal parenchymal perforation with double-J ureteral stent. Urol Res. 2008;36:279–81. doi: 10.1007/s00240-008-0150-8. http://dx.doi.org/10.1007/s00240-008-0150-8. [DOI] [PubMed] [Google Scholar]
- 7.Karakose A, Yuksel MB. An extremely rare complication of double-j stenting: renal parenchymal perforation with no hematoma. Curr Urol. 2011;5:165–8. http://dx.doi.org/10.1159/000327472. [Google Scholar]
- 8.Nomikos MS, Chousianitis Z, Georgiou C, Georgellis C, Rikas P, Anagnostou T. Renal parenchyma perforation and hematoma formation following double-j stent ınsertion in a solitary functioning kidney: An unusual complication. Case Rep Urol. 2012;2012:301275. doi: 10.1155/2012/301275. [DOI] [PMC free article] [PubMed] [Google Scholar]